Abstract
The Government of Malawi has signed contracts called service level agreements (SLAs) with mission health facilities in order to exempt their catchment populations from paying user fees. Government in turn reimburses the facilities for the services that they provide. SLAs started in 2006 with 28 out of 165 mission health facilities and increased to 74 in 2015. Most SLAs cover only maternal, neonatal and in some cases child health services due to limited resources. This study evaluated the effect of user fee exemption on the utilization of maternal health services. The difference-in-differences approach was combined with propensity score matching to evaluate the causal effect of user fee exemption. The gradual uptake of the policy provided a natural experiment with treated and control health facilities. A second control group, patients seeking non-maternal health care at CHAM health facilities with SLAs, was used to check the robustness of the results obtained using the primary control group. Health facility level panel data for 142 mission health facilities from 2003 to 2010 were used. User fee exemption led to a 15% (P < 0.01) increase in the mean proportion of women who made at least one antenatal care (ANC) visit during pregnancy, a 12% (P < 0.05) increase in average ANC visits and an 11% (P < 0.05) increase in the mean proportion of pregnant women who delivered at the facilities. No effects were found for the proportion of pregnant women who made the first ANC visit in the first trimester and the proportion of women who made postpartum care visits. We conclude that user fee exemption is an important policy for increasing maternal health care utilization. For certain maternal services, however, other determinants may be more important.
Keywords: Antental care, maternity services, user fees, utilization
Key Messages
User fee exemption at mission health facilities in Malawi led to increases in the percentage of pregnant women who made at least one antenatal care visit during pregnancy, average antenatal care visits and facility deliveries. No effects were found for first antenatal care visits in the first trimester and postpartum care visits.
User fee exemption is important for increasing maternal health care utilization but may not have the same importance for different maternal health services. For maternal health services for which utilization was not responsive to the price change, other determinants may need to be examined.
Introduction
Since the late 1990s, many low and middle countries have abolished user fees for health care or put in place exemption mechanisms in order to expand access to health care. In Malawi, the Government has intervened to exempt catchment populations of mission health facilities from paying user fees since 2006. User fee exemption is implemented through contracts between Government and Christian Health Association of Malawi (CHAM) health facilities. These contracts are called service level agreements (SLAs). Through SLAs, CHAM health facilities exempt their catchment populations from paying user fees and Government in turn reimburses them for the services that they provide. The aim of SLAs is to expand access to a basic package of health services known as the Essential Health Package (EHP). The EHP consists of cost-effective interventions targeting a limited number of diseases and conditions that rank highly in terms of burden of disease (Ministry of Health 2002). The first SLA was piloted in 2005. In 2006, SLAs were rolled out to 28 out of 165 CHAM health facilities and increased to 74 in 2015. Most SLAs only cover maternal and neonatal services. Therefore, pregnant women and neonates in the catchment areas of CHAM health facilities with SLAs are exempted from paying user fees. This article asks whether user fee exemption at CHAM health facilities with SLAs has led to increased utilization of antenatal, delivery and postpartum care at these facilities.
Research on the effects of user fee exemption on maternal health care utilization has mostly demonstrated positive effects. User fee removal has been shown to increase the use of maternal health care in Uganda, Sierra Leone, Senegal, Kenya, Ghana, Burkina Faso, Burundi and Nepal (Burnham et al. 2004; Deininger and Mpuga 2005; Penfold et al. 2007; Witter et al. 2010; De Allegri et al. 2011; Meessen et al. 2011; Ridde and Morestin 2011; UNICEF, 2011; Witter et al. 2011; World Health Organization, 2011; Powell-Jackson and Hanson, 2012; Chama-Chiliba and Koch, 2014; McKinnon et al. 2015). There are exceptions, however. In Afghanistan, there was an increase in antenatal care (ANC) visits immediately after user fee abolition but it was not sustained. There was no effect on deliveries (Steinhardt et al. 2011). In South Africa, user fee abolition was associated with a decline in ANC attendances and new ANC registrations (Wilkinson et al. 2001).
The limitation of most of these studies is that they did not estimate causal effects. This was either because nationwide implementation of user fee removal provided no scope for controls (e.g. Burnham et al. 2004; Deininger and Mpuga 2005; Steinhardt et al. 2011) or, in the case of user fee exemptions, opportunities for creating control groups were not exploited (e.g. Wilkinson et al. 2001; UNICEF 2011). So, in addition to the evidence not being unequivocal, there is a limitation that the reported effects on utilization cannot solely be attributed to user fee removal (Deininger and Mpuga 2005; Ministry of Health, 2010a; Khandker et al. 2010). Further, many of the studies have reported increases in total attendances or total new visits but have not controlled for population which may have confounded the reported effects.
This article contributes to the literature on user fee removal as follows. First, it evaluates the causal effect of a user fee exemption policy implemented within the context of a pre-existing public-private partnership between Government and CHAM. Government and CHAM have had a mutually beneficial relationship where Government relies on CHAM to provide health services in areas where there are no Government health facilities and CHAM depends on Government to provide personnel emoluments for its human resources. About 80% of CHAM health facilities are located in rural areas where the majority of the poor live (Aukerman 2006). Government and CHAM also have a policy where Government cannot build a health facility in the catchment area of a CHAM facility and CHAM has to inform Government when taking on board a new facility (Banda and Simukonda 1994). In all the countries studied in this article, user fee removal was introduced in the public sector except in Burundi where the policy was extended to faith-based providers but failed within a year due to late reimbursement of providers by the Government (Nimpagaritse and Bertone 2011). Second, this paper evaluates the effect of user fee exemption on the proportion of women who used particular maternal health services, hence controlling for any changes in utilization that were due to population changes.
Background
Malawi is classified as a less developed country (World Bank 2015). Typically, it has low Gross Domestic Product (GDP) per capita. It was estimated at US$274 in 2014 in constant 2005 US dollars translating into US$0.75 to spend per day for the average individual (World Bank 2015). An ANC visit at US$6 and a normal delivery at US$11 in the same year show the opportunity cost of using maternal health care in terms of forgone consumption of other goods and services (GIZ Health 2011).
The Malawi health care system consists of public, private-for-profit and private not-for-profit providers. Health services in the public sector are provided free-of-charge at the point of use while private-for-profit and private not-for-profit providers charge user fees. CHAM is a major not-for-profit provider, an umbrella organization of mission health care providers. In 2015, CHAM facilities had a total catchment population of about 3.5 million out of a total national population of 16.3 million. It is estimated that CHAM provides approximately up to 29% of all health care in Malawi (Ministry of Health and ICF International 2014).
Government observed that user fees at CHAM health facilities posed a barrier to accessing the EHP for a significant proportion of the population. Therefore, the Ministry of Health in its Program of Work (2004–10) introduced a policy of free access to the EHP by every Malawian at the point of delivery. SLAs were an operationalization of this policy in catchment areas of CHAM facilities. In order to sign an SLA, a District Health Office (DHO) conducts a needs assessment and then negotiates with the concerned CHAM health facility services to be covered by the SLA and their prices. Once the contract is signed, the DHO makes a publicity campaign to make the catchment population of the CHAM health facility aware of the free health services that become available under the SLA. The health facility retrospectively bills the DHO on a monthly basis based on the total quantity of health services utilized. The total bill is the quantity of health services provided in a month multiplied by fixed reimbursement rates agreed in the contract. SLAs are renewable yearly.
The causal effect of user fee exemption on maternal health care utilization at CHAM health facilities is not known Ministry of Health (2010a,b). SLAs were rolled out based on the results of a before and after comparison of utilization for the pilot SLA which showed increased utilization. As was pointed out earlier, results from before and after studies are unreliable. It is not possible to disentangle the effects of user fee exemption from the effects of external factors using this evaluation method (Deininger and Mpuga 2005; Xu et al. 2006; Ministry of Health 2010a). For example, there may be an improvement in the economic conditions of households at the same time that the policy is implemented. So the increase in utilization may be due to both the exemption policy and the increased ability to pay for health care by households (Khandker et al., 2010). Before and after studies report the sum of both effects. Lack of evidence on the impact of user fee exemption implies that the Ministry of Health has no objective basis for expanding SLAs to more CHAM health facilities. This study addresses this evidence gap. Since user fee exemption is equivalent to a reduction in price, we hypothesize that it will lead to increased utilization of maternal health services.
Methods
Ideally, the effect of user fee exemption on health care utilization should be the difference between the level of utilization at a health facility in the presence of user fee exemption and the level of utilization in the absence of user exemption. If is a measure of utilization, superscript 1 denotes treatment (user fee exemption) and superscript 0 denotes no treatment (no user fee exemption), then the effect of user fee exemption for health facility at time can be measured as . The average impact of the policy for health facilities implementing user fee exemption will be
| (1) |
where denotes health facility with user fee exemption and denotes health facility with no user fee exemption. The problem, however, is that is never observed because the health facility can only be in one state at a time. Different evaluation methods implicitly provide alternatives to estimating the counterfactual, (Blundell and Costa Dias 2000). This study uses the difference-in-differences (DiD) method which estimates the counterfactual outcome as the sum of the mean of the outcome for the treatment group before the policy and the mean gain in the outcome for the control group before and after treatment. is therefore expressed as follows where before the policy and after the policy (Blundell and Costa Dias 2007)
| (2) |
A key DiD assumption is that outcomes in both the treatment and control groups have a parallel trend in the absence of the policy (Blundell and Macurdy 1999; Chaudhury and Parajuli 2010). We tested this assumption in two ways. First, we visually inspected utilization trends for SLA and non-SLA health facilities. Second, we followed an approach by Autor (2003) which involves estimating regressions with interacted terms of treatment and time variables before and after treatment. The pre-treatment interactions are then tested for statistical significance. If they are not significant, then the null hypothesis of no difference in the trends for the treatment and control groups cannot be rejected. We also used a second control group, patients seeking all other non-maternal health care at SLA CHAM health facilities, to check the robustness of the results obtained using the first control group. The second control group and treatment group would experience the same shocks for coming from the same catchment area, thus nullifying the need to invoke the common trends assumption. Using the second control group also helped circumvent the potential problem of endogeneity i.e. correlation of the policy variable with the error term which arises as a result of the policy targeting health facilities with low utilization and leads to inconsistent estimates (Wooldridge 2010).
To ensure that the treatment and control groups were comparable in terms of initial characteristics, treatment and control health facilities were matched on their propensity scores and then DiD estimation was conducted. Propensity score matching was only implemented for the models which used the first control group because the second group shared the same characteristics with the treatment group, the data being at facility level. Propensity scores were obtained by estimating the following probit equation for each year of the data
| (3) |
Equation (3) estimates the probability of health facility i participating in an SLA as a function of a vector of health facility types (‘hcf’) (i.e. whether it was a health centre, a community hospital or a secondary hospital), the number of health workers at the health facility (‘hw’) and catchment population (‘cpopn’). is the cumulative normal density function. From equation (3), the propensity scores of participating in an SLA, , were estimated for each health facility for every year. Balancing tests were conducted until there were no statistically significant differences in the means of the explanatory variables between the treatment and control groups. DiD was combined with propensity score matching by weighting regressions with weights obtained from the propensity scores. The caliper technique was used to estimate the weights (Khandker et al. 2010). For treated units the weight was 1 while for control units the weight was expressed as (Khandker et al. 2010). The following unobserved effects regression model was used
| (4) |
In equation (4), is the natural log of a measure of utilization for health facility in year . is a vector of all year dummy variables included to fully control for time trends. is the policy dummy variable, which took the value of 1 if health facility had user fee exemption in year and 0 otherwise. is the coefficient of the policy dummy and estimates the average treatment effect on the treated as expressed in equation (2). It is the mean difference in between the treatment and control groups before and after the introduction of user fee exemption. is a time invariant health facility unobserved effect. It may capture management quality or any other facility or catchment area characteristics that affect the provision of health services but remain constant over time (Wooldridge 2010). is an idiosyncratic error term. Only observations that were in the region of common support in the propensity score matching were used in the estimation of equation (4).
The fixed effects model was used to estimate equation (4). It eliminates the unobserved effect and hence produces consistent estimates even when the unobserved effect is arbitrarily correlated with explanatory variables (Heckman et al. 1999; Todd 2007; Wooldridge 2010). We used a fully robust variance-covariance matrix estimator to produce consistent estimates in light of potential serial correlation (Wooldridge 2010). Estimation was conducted using Stata 12 and the program psmatch2 by Leuven and Sianesi (2003) was used for propensity score matching.
Data
Yearly panel data on maternal health care utilization at CHAM health facilities were used. They were obtained from the health management information system (HMIS) of the Ministry of Health. The data covered an 8-year period, 2003–10, for up to 142 CHAM health facilities per year. The number of SLA and non-SLA facilities by facility type and year are shown in Table 1. The intention was to use data for the total number of CHAM health facilities in every year, 161 in 2003 increasing to 172 in 2010 (JICA 2003; CHAM 2014). However, not all health facilities reported data every year. This is shown in Table 1 by the fluctuation in the total number of health facilities in the sample over time.
Table 1.
Number of mission health facilities in the sample by SLA status, facility type and year
| Year |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Whether facility has SLA | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | |
| No | Health Centre | 96 | 87 | 96 | 88 | 73 | 67 | 67 | 64 |
| Community Hospital | 27 | 25 | 27 | 19 | 16 | 14 | 13 | 10 | |
| Hospital | 14 | 15 | 15 | 4 | 3 | 2 | 1 | 1 | |
| Sub-total | 137 | 127 | 138 | 111 | 92 | 83 | 81 | 75 | |
| Yes | Health Centre | 9 | 25 | 31 | 32 | 35 | |||
| Community Hospital | 8 | 12 | 14 | 15 | 18 | ||||
| Hospital | 11 | 12 | 14 | 14 | 14 | ||||
| Sub-total | 28 | 49 | 59 | 61 | 67 | ||||
| Grand total | 137 | 127 | 138 | 139 | 141 | 142 | 142 | 142 | |
In addition to the health facilities not reporting their data for all years, not every health facility reported data for all 12 months of the year. The average number of months reported per year though was 11 for all variables for the whole sample. In fact, at least 65% of observations for all utilization variables were based on 12 months’ reporting and at least 80% on not <9 months’ reporting for the whole sample. SLA facilities had a higher mean reporting rate in months per year than non-SLA facilities by about a month. This is shown in Table A.1 in Supplementary Appendix A. It is possible that the requirement to send monthly bills to the DHO with sufficient evidence of services provided positively influenced reporting of HMIS data to the Ministry of Health headquarters. Summary statistics for all variables used in this study are provided in Table 2, disaggregated by SLA status. The maternal health care utilization variables in Table 2 are defined as follows:
Proportion of pregnant women who made the first ANC visit in first trimester: yearly total of pregnant women who made their first antenatal visit at a health facility within the first 3 months of pregnancy divided by the estimated number of pregnant women in the catchment area of the facility.
Proportion of pregnant women who made at least one ANC visit during pregnancy: yearly total number of pregnant women who made at least one ANC visit at a health facility during pregnancy divided by the estimated number of pregnant women in the catchment area.
Average ANC visits: the total number of ANC visits at a health facility in a year divided by the estimated population of pregnant women in the catchment area.
Proportion of health facility deliveries: the total number of deliveries at a health facility in a year divided by the estimated number of pregnant women in the catchment area.
Proportion of women who made postpartum care visits 2 weeks after delivery: the yearly total number of women who made at least one postpartum care visit 2 weeks after delivery at a health facility divided by the estimated number of pregnant women in the catchment area. The two week period is recommended by the Ministry of Health (Ministry of Health 2003).
Table 2.
Summary statistics by SLA status for the period 2003–10
| SLA |
No SLA |
Difference |
||||||
|---|---|---|---|---|---|---|---|---|
| N | Mean | SD | N | Mean | SD | Mean | p-value | |
| Proportion of pregnant women who made: | ||||||||
| First ANC visits in first trimester | 262 | 0.08 | 0.10 | 795 | 0.07 | 0.10 | 0.01* | 0.059 |
| At least one ANC visit during pregnancy | 264 | 0.96 | 0.54 | 805 | 0.82 | 0.59 | 0.14*** | 0.001 |
| Facility deliveries | 264 | 0.62 | 0.35 | 788 | 0.44 | 0.30 | 0.18*** | 0.000 |
| Postpartum care visits | 252 | 0.28 | 0.22 | 518 | 0.26 | 0.21 | 0.02 | 0.246 |
| Average ANC visits | 264 | 2.34 | 1.38 | 807 | 2.25 | 1.54 | 0.09 | 0.357 |
| Health workers per facility | 261 | 23.5 | 26.2 | 772 | 7.8 | 12.7 | 15.7*** | 0.000 |
| Facility catchment population | 264 | 37993 | 34688 | 844 | 20462 | 18347 | 17531*** | 0.000 |
| Health facility type | ||||||||
| Health centre | 264 | 0.50 | 0.50 | 844 | 0.76 | 0.43 | 0.26*** | 0.000 |
| Community hospital | 264 | 0.25 | 0.44 | 844 | 0.18 | 0.38 | 0.07** | 0.013 |
| Secondary hospital | 264 | 0.25 | 0.43 | 844 | 0.07 | 0.25 | 0.18*** | 0.000 |
*P < 0.10; ** P < 0.05; ***P < 0.01.
N represents the total number of observations for all health facility panels. SD, standard deviation.
The five variables capture different dimensions of the maternal health care process. The proportion of women who made the first ANC visit in the first trimester measures the extent of early ANC seeking. The proportion of women who made at least one ANC visit during pregnancy is self-explanatory. Average ANC visits portray the extent to which pregnant women are followed up during pregnancy, holding other factors constant. ANC visits are expected to culminate in facility deliveries and the maternal health care process is completed by postpartum care. The ANC variables are also performance indicators for the focussed ANC (FANC) approach (see Villar et al. 2001). The FANC approach recommends that pregnant women who have no complications make four ANC visits at specific times during pregnancy. The first visit should ideally occur before 12 weeks (first trimester) but not later than 16 weeks of pregnancy. More visits are recommended for women who have complications or special needs (Ministry of Health 2003; National Statistical Office and ICF Macro 2011).
Table 2 shows that the means of the utilization variables were lower in the control group and their differences between the SLA and non-SLA groups were statistically significant except for average ANC visits and the proportion of women who made postpartum care visits. The mean values of the number of health workers per health facility and catchment population were higher in the SLA group because it had more community and secondary hospitals.
Results
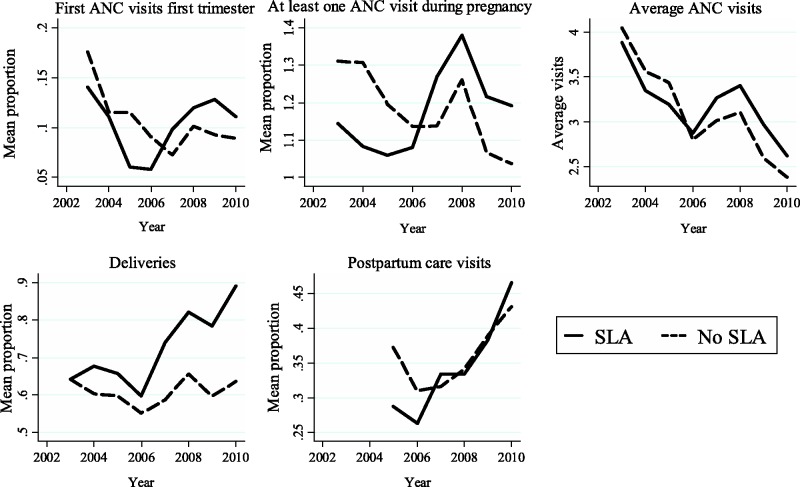
Utilization trends by SLA status are shown in Figure 1. The trends were generally parallel up to 2006. This was confirmed by significance tests of coefficients of pre-policy treatment and time interactions. The tests failed to reject the null hypothesis of no difference in the trends for all variables except ln(Prop. Postpartum care visits). The test was not conducted for the variable ln(Prop. Postpartum care visits) because it did not have adequate pre-policy data. The results are reported in Supplementary Appendix B. We therefore concluded that the common trends assumption was satisfied.
Figure 1:
Utilization trends by SLA status.
Propensity score matching eliminated bias in all the variables except one category of the health facility type variable i.e. there were no statistically significant differences in the means of the variables by SLA status after matching except for the one category of the facility type variable. We were satisfied with the matching results and did not want to pursue achieving balance for the one health facility type category at the expense of the sample in the region of common support. The results are reported in Supplementary Appendix C. We then estimated equation (4) for all five maternal health care utilization variables, applying weights derived from the matching results. Two sets of results are presented. The primary set of results relates to models in which the control group was pregnant women at CHAM health facilities with no SLAs. The second set of results relates to models in which patients who used non-maternal health care at CHAM health facilities with SLAs were the control group. Because the dependent variables were log-transformed, the formula is used to interpret the coefficient of the SLA dummy variable in relation to the dependent variable [ is the percentage change in the dependent variable, denotes exponent, is the estimated coefficient and is the change in the regressor (Wooldridge 2009)].
Control group is pregnant women at non-SLA CHAM health facilities
Table 3 shows results for all the five utilization variables when pregnant women at non-SLA CHAM health facilities were the control group. Data for postpartum care visits were only available from 2005. In model (i), user fee exemption had no effect on the proportion of pregnant women who made first ANC visit in the first trimester. In model (ii), the coefficient on the SLA dummy shows that the mean proportion of women who made at least one ANC visits during pregnancy increased by 15% (95% CI: 8%, 24%) (P < 0.01) due to user fee exemption. The baseline mean proportion of women who made at least one ANC visit during pregnancy for SLA CHAM health facilities before user fee exemption started was estimated to be 0.729. Therefore, the 15% increase means this proportion rose to 0.838 due to user fee exemption. In model (iii), the coefficient on the SLA dummy shows that user fee exemption led to a 12% (95% CI: 0.70%, 25%) (P < 0.05) increase in average ANC visits. The baseline number of average ANC visits was 2.31 for SLA CHAM health facilities. A 12% increase means that average visits rose to 2.59 due to user fee exemption. In model (iv), user fee exemption led to an 11% (95% CI: 1%, 21%) (P < 0.05) increase in the mean proportion of facility deliveries. The pre-policy mean utilization rate for deliveries was 0.44. The 11% increase therefore implies that the mean proportion of facility deliveries rose from 0.44 to 0.49 due to user fee exemption. Finally, in model (v), user fee exemption had no effect on the proportion of women who made postpartum care visits 2 weeks after delivery.
Table 3.
. Fixed effects regressions when the control group was pregnant women at mission health facilities without SLAs
| (i) | (ii) | (iii) | (iv) | (v) | |
|---|---|---|---|---|---|
| ln(Prop. First ANC visits in first trimester) | ln(Prop. at least one ANC visit during pregnancy) | ln(Average ANC visits) | ln(Prop. deliveries) | ln(Prop. Postpartum care visits) | |
| SLA | 0.074 (0.088) | 0.149*** (0.035) | 0.116** (0.055) | 0.105** (0.044) | 0.004 (0.094) |
| Year (Base = 2003) | |||||
| 2004 | 0.460** (0.184) | 0.597*** (0.063) | 0.839*** (0.076) | 0.630*** (0.068) | |
| 2005 | 0.064 (0.229) | 0.176*** (0.055) | 0.374*** (0.087) | 0.127* (0.075) | (Base = 2005) |
| 2006 | 0.283 (0.201) | 0.096 (0.078) | 0.527*** (0.086) | 0.165** (0.072) | 0.423*** (0.108) |
| 2007 | 0.402*** (0.088) | 0.154** (0.061) | 0.480*** (0.072) | 0.071 (0.072) | 0.255*** (0.077) |
| 2008 | 0.044 (0.079) | 0.143** (0.056) | 0.481*** (0.065) | 0.070 (0.068) | 0.035 (0.161) |
| 2009 | 0.125 (0.110) | 0.205** (0.081) | 0.527*** (0.118) | 0.146 (0.103) | 0.091 (0.146) |
| 2010 | 0.042 (0.114) | 0.194*** (0.070) | 0.656*** (0.114) | 0.024 (0.078) | 0.113 (0.106) |
| Constant | 0.264*** (0.056) | 0.189*** (0.054) | 0.490*** (0.058) | 0.155*** (0.054) | 0.188*** (0.065) |
| N | 748 | 758 | 760 | 744 | 533 |
| Adjusted R2 | 0.076 | 0.238 | 0.213 | 0.282 | 0.085 |
Standard errors in parentheses.
*P < 0.10; **P < 0.05; ***P < 0.01.
Control group is patients seeking non-maternal health care at CHAM health facilities with SLAs
Table 4 shows the results of the DiD analysis that used patients who sought non-maternal health care at CHAM health facilities with SLAs as the control group. Data for postpartum care visits were only available from 2004. User fee exemption had no effect on the proportion of women who made first ANC visits in the first trimester just as in Table 3. In model (ii), user fee exemption led to a 15% (95% CI: 4%, 28%) (P < 0.01) increase in the mean proportion of women who made at least one ANC visit during pregnancy. In model (iii), user fee exemption led to an 11% (95% CI: 0.30%, 25%) (P < 0.10) increase in average ANC visits. The mean proportion of women who delivered at CHAM health facilities with SLAs increased by 15% (95% CI: 4%, 26%) (P < 0.01) in model (iv). In model (v), user fee exemption had no effect on the proportion of women who made postpartum care visits 2 weeks after delivery. The results in Table 4 were consistent with those in Table 3. The same utilization variables had statistically significant coefficients for the SLA variable in both tables and the point estimates and CIs were similar.
Table 4.
. Fixed effects regressions when the control group was patients seeking non-maternal health care at mission health facilities with SLAs
| (i) | (ii) | (iii) | (iv) | (v) | |
|---|---|---|---|---|---|
| ln(Prop. First ANC visits in first trimester) | ln(Prop. at least one ANC visit during pregnancy) | ln(Average ANC visits) | ln(Prop. Deliveries) | ln(Prop. Postpartum care visits) | |
| SLA | 0.091 (0.104) | 0.142*** (0.053) | 0.108* (0.056) | 0.136*** (0.050) | 0.045 (0.099) |
| Year (Base = 2003) | |||||
| 2004 | 0.738*** (0.129) | 0.500*** (0.124) | 0.684*** (0.130) | 0.487*** (0.061) | (Base = 2004) |
| 2005 | 0.330** (0.145) | 0.029 (0.119) | 0.187 (0.124) | 0.040 (0.050) | 0.603*** (0.096) |
| 2006 | 0.237 (0.152) | 0.082 (0.116) | 0.139 (0.124) | 0.071 (0.056) | 0.661*** (0.108) |
| 2007 | 0.314* (0.178) | 0.128 (0.122) | 0.356*** (0.131) | 0.112 (0.069) | 0.529*** (0.118) |
| 2008 | 0.143 (0.183) | 0.160 (0.121) | 0.062 (0.128) | 0.191*** (0.068) | 0.777*** 0.125) |
| 2009 | 0.261 (0.181) | 0.166 (0.124) | 0.097 0.140) | 0.237*** (0.073) | 0.937*** (0.138) |
| 2010 | 0.206 (0.197) | 0.130 (0.129) | 0.199 (0.145) | 0.279*** (0.081) | 1.039*** (0.138) |
| Constant | 3.869*** (0.127) | 2.425*** (0.106) | 1.674*** (0.115) | 2.711*** (0.045) | 3.560*** (0.085) |
| N | 973 | 981 | 981 | 980 | 840 |
| Adjusted R2 | 0.204 | 0.235 | 0.150 | 0.324 | 0.144 |
Standard errors in parentheses.
*P < 0.10; **P < 0.05;*** P < 0.01.
Discussion
The results reported here support the hypothesis that user fee exemption will lead to increased utilization of maternal health care. They also corroborate findings of the majority of evaluations that have shown increased utilization of health care after user fee removal (see Lagarde and Palmer 2011; Dzakpasu et al. 2014). They underscore the importance of user fee exemption as a strategy for universal health coverage. An important implication of the results is that user fee exemption may not have the same importance for different types of maternal health services. This is inferred from the lack of significant effects for some variables and the significant positive effects for the other variables. The fact that the signs and statistical significance of the SLA coefficients were the same for corresponding utilization variables in the two sets of results shows the robustness of the primary set of results. This section discusses the results for each of the utilization variables starting with the ones that had statistically significant effects.
The percentage of pregnant women who make at least one ANC visit during pregnancy has been high in Malawi. The Malawi Demographic and Health Survey (MDHS) (2004) showed that it was 95% nationally while the MDHS (2010) showed that it rose to 99% (National Statistical Office and ORC Macro, 2005; National Statistical Office and ICF Macro 2011). The data used in this study showed that, for CHAM health facilities with user fee exemption, it was 73% between 2003 and 2005 (before user fee exemption was introduced) and increased to 84% due to user fee exemption. However, despite the effect of user fee exemption it still fell below the national average. For average ANC visits, the increase due to user fee exemption means that pregnant women were modestly better followed up at CHAM health facilities with SLAs, holding other factors constant. Nevertheless, even after user fee exemption, the average number of ANC visits was lower than the four visits recommended in the FANC approach. This could partially be attributed to what has been referred to as confidence selection where women who have had previous uneventful pregnancies consider themselves to be at low risk of complications and make fewer visits despite removal of the financial barrier (Grossman and Joyce 1990).
Increase in the proportion of health facility deliveries due to user fee exemption was an important achievement in a context where delivery at a health facility is a prerequisite for skilled birth attendance. Skilled birth attendance is regarded as an important strategy for reducing maternal mortality and morbidity (AbouZahr 1998; Ronsmans and Graham 2006). The increase would be expected to lead to a decline in the use of substitute providers such as traditional birth attendants and private clinics. Due to data limitations, we could not test this hypothesis. Other studies, though, support this prediction. Ansah et al. (2009) using a randomized controlled trial design and Powell-Jackson and Hanson (2012) using matching methods showed how user fee exemption caused patients to shift from alternative, mostly informal, health care providers to health facilities that had removed user fees in Ghana and Nepal respectively. In Kenya, Mwabu et al. (1995) showed that user fee exemption in the public health sector was associated with a decrease in the use of private care. On the contrary, Xu et al. (2006) found that after user fee abolition in Uganda, health care utilization increased at both public and private health facilities for both the rich and poor. They did not estimate causal effects, however.
A possible explanation why user fee exemption had no effect on first ANC visits in the first trimester may be inferred from the national percentage of pregnant women who make the first ANC visit in the first trimester. Demographic and Health Surveys for the years 2000, 2004 and 2010 found that only 7, 8 and 12.4% of pregnant women, respectively, had a first ANC visit in the first trimester (National Statistical Office and ORC Macro 2001, 2005; National Statistical Office and ICF Macro 2011). A study conducted in the catchment area of a Government health centre showed that only 11% of pregnant women registered for their first visit in the first trimester despite services being free (Mvula-Mgawadere 2009). It can be concluded therefore that this maternal health service was not responsive to price change. The implication of this is that there are other perhaps more important determinants of first ANC visits in the first trimester than price. In the African context, these determinants include cultural norms, quality of care and health worker attitudes (Myer and Harrison 2003; Mvula-Mgawadere 2009; Ndidi and Oseremen 2010; Gross et al. 2012). Cultural beliefs are especially important for first ANC visits in the first trimester. Studies have shown that there is a common cultural belief of disclosing pregnancy late, which has a negative effect on the timing of the first ANC visit (Myer and Harrison 2003; Gross et al. 2012). Increasing first ANC visits in the first trimester may therefore require addressing such determinants in addition to user fee exemption.
A possible reason user fee exemption had no statistically significant effect on postpartum care could be that women who delivered without complications were less likely to return for check-up. The 2009/10 HMIS report showed that only 28% of women who delivered at Government and CHAM health facilities returned for a postpartum check-up 2 weeks after delivery. The percentage of pregnancies that had complications at these health facilities during the same period was 15% (Ministry of Health 2010b). Assuming that each woman who had a complication made one postpartum care visit, then the percentage of women who had no complications but made a postpartum visit 2 weeks after delivery declines significantly. This implies that in order to make an impact on postpartum visits 2 weeks after delivery, there is need to focus more on other determinants.
It would be expected that the estimates of the effects of user fee exemption in the second set of results, where patients who sought non-maternal health care at CHAM health facilities with SLAs were the control group, would be smaller than those in the first set. Income effects working at household level would diminish the gain in the treatment group over the control group. This is because user fee exemption increases the income available to households to spend on other goods and services including non-maternal health care. This argument, though, relies on the assumption that income in the household is pooled and distributed to all members (see Samuelson 1956). Alternatively, there may be positive spill-over effects if other household members see the benefits of health care through the exempted groups or seize the opportunity of taking pregnant mothers or neonates to health facilities to seek health care themselves (Lagarde et al. 2012). The closeness of the estimates in the two sets of results probably indicates that the extra income afforded by user fee exemption was either not pooled and distributed or household members allocated it to other goods and services than health care and there were negligible or no spill-over effects.
Although this study was not an evaluation of the implementation process of user fee exemption, it is worth bearing in mind SLA implementation challenges in the interpretation of the results. An assessment of SLA implementation by the Ministry of Health in 2009 found that there were delays in payments by DHOs which affected implementation of the user fee exemption policy, inadequate staffing levels and equipment at CHAM health facilities which rationed demand and allegations that CHAM facilities were upcoding or inflating utilization in order to fraudulently gain additional revenue (Ministry of Health 2009; Bradley et al. 2015).
Based on the results of this article, it is recommended that measures be put in place to ensure that free maternal health care and indeed the entire EHP is available to all populations that face user fees. This would be consistent with broader Government policy of free health care at the point of use for all Malawians. It is also important to heighten focus on non-price determinants of maternal health care use (Mazalale et al. 2015). This article acknowledges the efforts that the Ministry of Health and other agents have taken through the road map for accelerating the reduction of maternal mortality and morbidity.
The study had limitations. First, data were limited in terms of both quality and variables. Data recording and reporting problems are still inevitable in the Malawi health care system and perhaps more so at CHAM health facilities. Despite the general reporting challenges at CHAM health facilities, SLA facilities had slightly better reporting than non-SLA facilities and this could have biased the reported effects. We also could not model the influence of important demand factors such as socioeconomic status and education on utilization because the HMIS does not collect individual level data. This too could have affected the results. Second, the DiD approach does not control for time-variant unobserved characteristics. If there were any such health facility characteristics which affected utilization, these may have biased the results. Third, this study did not model supply side capacity constraints at CHAM health facilities which may have affected utilization. Fourth, it is likely that increased utilization of maternal health care compromised quality. This study did not explore that dimension.
Conclusion
User fee exemption at CHAM health facilities with SLAs led to an increase in the proportion of pregnant women who made at least one ANC visit during pregnancy, average ANC visits and deliveries while it had no effect on first ANC visits in the first trimester and postpartum care visits. This implies that, while user fee exemption is an important strategy for increasing maternal health care utilization, it may not have the same importance for different maternal health services. We therefore recommend that user fee exemption be expanded to more eligible CHAM health facilities to increase utilization of the price-elastic services while the effects of other determinants such as cultural norms, risk attitudes, quality of maternal health care and health worker attitudes should be evaluated for the services for which utilization was not responsive to price change.
Supplementary Material
Acknowledgements
This article was based on the first author’s PhD which was financed by the Malawi Health Research Capacity Strengthening Initiative. We thank Mr Patrick Naphini formerly of the Ministry of Health and Mrs Mafase Sesani at CHAM Secretariat for helping with the data. We also thank Mr Jacob Mazalale for useful comments on the article.
Conflict of interest statement. None declared.
Supplementary Data
Supplementary data are available at HEAPOL online
References
- AbouZahr C. 1998. Antepartum and postpartum haemorrhage In: Murray CJL, Lopez AD. (eds). Health Dimensions of Sex and Reproduction. Global Burden of Disease and Injury Series. Volume III . Geneva: World Health Organization, 165–190. [Google Scholar]
- Ansah EK, Narh-Bana S, Asiamah S. et al. 2009. Effect of removing direct payment for health care on utilisation and health outcomes in Ghanaian children: a randomised controlled trial. PLoS Medicine 6: 0048–0058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aukerman D. 2006. Human Resources for Health Workforce: A “Promising Practices” Study. Lilongwe: USAID Global Health. [Google Scholar]
- Autor DH. 2003. Outsourcing at will: the contribution of unjust dismissal doctrine to the growth of employment outsourcing. Journal of Labor Economics 21: 1–42. [Google Scholar]
- Banda EEN, Simukonda HP. 1994. The public/private mix in the health care system in Malawi. Health Policy and Planning 9: 63–71. [Google Scholar]
- Blundell R, Costa Dias M. 2000. Evaluation methods for non-experimental data. Fiscal Studies 21: 427–468. [Google Scholar]
- Blundell R, Costa Dias M. 2007. Alternative Approaches to Evaluation in Empirical Microeconomics. London: Institute for Fiscal Studies. [Google Scholar]
- Blundell R, Macurdy T. 1999. Chapter 27 Labor supply: a review of alternative approaches In: Ashenfelter O, Card D. (eds). Handbook of Labor Economics. Amsterdam: Elsevier, 1559–1695. [Google Scholar]
- Bradley S, Kamwendo F, Chipeta E. et al. 2015. Too few staff, too many patients: a qualitative study of the impact on obstetric care providers and on quality of care in Malawi. BMC Pregnancy and Childbirth 15: 65.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnham GM, Pariyo G, Galiwango E, Wabwire-Mangen F. 2004. Discontinuation of cost sharing in Uganda. Bulletin of the World Health Organization 82: 187–195. [PMC free article] [PubMed] [Google Scholar]
- CHAM. 2014. CHAM Strategic Plan 2010-2014. Lilongwe: CHAM Secretariat. [Google Scholar]
- Chama-Chiliba CM, Koch SF. 2014. Assessing Regional Variations in the Effect of the Removal of User Fees on Institutional Deliveries in Rural Zambia. Pretoria: University of Pretoria, Department of Economics. [Google Scholar]
- Chaudhury N, Parajuli D. 2010. Conditional cash transfers and female schooling: the impact of the female school stipend programme on public school enrolments in Punjab, Pakistan. Applied Economics 42(28): 3565–3583. [Google Scholar]
- De Allegri M, Ridde V, Louis VR. et al. 2011. Determinants of utilisation of maternal care services after the reduction of user fees: a case study from rural Burkina Faso. Health Policy 99: 210–218. [DOI] [PubMed] [Google Scholar]
- Deininger K, Mpuga P. 2005. Economic and welfare impact of the abolition of health user fees: Evidence from Uganda. Journal of African Economies 14: 55–91. [Google Scholar]
- Dzakpasu S, Powell-Jackson T, Campbell OMR. 2014. Impact of user fees on maternal health service utilization and related health outcomes: a systematic review. Health Policy and Planning 29: 137–150. [DOI] [PubMed] [Google Scholar]
- GIZ Health M. 2011. Sustainable Structures for the Health Sector in Malawi: Cost Study of Service Level Agreement (SLA) Covered Services. Lilongwe: GIZ Health, Malawi. [Google Scholar]
- Gross K, Alba S, Glass T, Schellenberg J, Obrist B. 2012. Timing of antenatal care for adolescent and adult pregnant women in south-eastern Tanzania. BMC Pregnancy and Childbirth 12: 16.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman M, Joyce TJ. 1990. Unobservables, pregnancy resolutions, and birth weight production functions in New York city. Journal of Political Economy 98: 983–1007. [Google Scholar]
- Heckman JJ, Lalonde RJ, Smith JA. 1999. Chapter 31. The economics and econometrics of active labor market programs In: Ashenfelter O, Card D. (eds). Handbook of Labor Economics. Amsterdam: Elsevier, 1865–2097. [Google Scholar]
- JICA. 2003. Malawi Health Facilities Inventory Survey,Lilongwe: JICA. [Google Scholar]
- Khandker SR, Koolwal GB, Samad HA. 2010. Handbook on Impact Evaluation: Quantitative Methods and Practices. Washington, DC: World Bank. [Google Scholar]
- Lagarde M, Palmer N. 2011. The impact of user fees on access to health services in low- and middle-income countries. Cochrane Database of Systematic Reviews [Online], 4, (17 November 2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagarde M, Barroy H, Palmer N. 2012. Assessing the effects of removing user fees in Zambia and Niger. Journal of Health Services Research and Policy 17: 30–36. [DOI] [PubMed] [Google Scholar]
- Leuven E, Sianesi B. 2003. PSMATCH2: Stata Module to Perform Full Mahalanobis and Propensity Score Matching, Common Support Graphing, and Covariate Imbalance Testing. Chestnut Hill: Boston College, Department of Economics. [Google Scholar]
- Mazalale J, Kambala C, Brenner S. et al. 2015. Factors associated with delivery outside a health facility: cross-sectional study in rural Malawi. Tropical Medicine and International Health 20: 617–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinnon B, Harper S, Kaufman JS, Bergevin Y. 2015. Removing user fees for facility-based delivery services: a difference-in-differences evaluation from ten sub-Saharan African countries. Health Policy and Planning 30: 432–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meessen B, Hercot D, Noirhomme M. et al. 2011. Removing user fees in the health sector: a review of policy processes in six sub-Saharan African countries. Health Policy and Planning 26: ii16–ii29. [DOI] [PubMed] [Google Scholar]
- Ministry of Health. 2010a. Final Evaluation of the Health Sector Programme of Work (2004-2010). Lilongwe: Ministry of Health. [Google Scholar]
- Ministry of Health. 2010b. Health Management Information Bulletin. Annual Report, July 2009-June 2010. Lilongwe: Ministry of Health. [Google Scholar]
- Ministry of Health. 2009. Report on the Assessment of Service Level Agreements. Lilongwe: Ministry of Health. [Google Scholar]
- Ministry of Health. 2003. Measuring Health Sector Performance: A Handbook of Indicators. Lilongwe: Ministry of Health. [Google Scholar]
- Ministry of Health. 2002. Essential Health Package: Revised Contents and Costing. Lilongwe: Ministry of Health. [Google Scholar]
- Ministry of Health and ICF International. 2014. Malawi Service Provision Assessment (MSPA) 2013-14. Lilongwe, Malawi, and Rockville, MD, USA: MoH and ICF International. [Google Scholar]
- Mvula-Mgawadere F. 2009. Assessing the Quality of Antenatal Care at Lungwena Health Centre in Rural Malawi. Masters Degree in Public Health Blantyre: University of Malawi, College of Medicine. [Google Scholar]
- Mwabu G, Mwanzia J, Liambila W. 1995. User charges in government health facilities in Kenya: effect on attendance and revenue. Health Policy and Planning. 10: 164–170. [DOI] [PubMed] [Google Scholar]
- Myer L, Harrison A. 2003. Why do women seek antenatal care late? Perspectives from rural South Africa. The Journal of Midwifery and Women’s Health 48: 268–272. [DOI] [PubMed] [Google Scholar]
- National Statistical Office and ICF Macro. 2011. Malawi Demographic and Health Survey 2010. Zomba, Malawi and Calverton, MD, USA: NSO and ICF Macro. [Google Scholar]
- National Statistical Office and ORC Macro. 2005. Malawi Demographic and Health Survey 2004. Calverton, MD: NSO and ORC Macro. [Google Scholar]
- National Statistical Office and ORC Macro. 2001. Malawi Demographic and Health Survey 2000. Zomba, Malawi and Calverton, MD, USA: National Statistical Office and ORC Macro. [Google Scholar]
- Ndidi EP, Oseremen IG. 2010. Reasons given by pregnant women for late initiation of Antenatal care in the Niger delta, Nigeria. Ghana Medical Journal 44: 47–51. [PMC free article] [PubMed] [Google Scholar]
- Nimpagaritse M, Bertone MP. 2011. The sudden removal of user fees: the perspective of a frontline manager in Burundi. Health Policy and Planning 26: ii63–ii71. [DOI] [PubMed] [Google Scholar]
- Penfold S, Harrison E, Bell J, Fitzmaurice A. 2007. Evaluation of the delivery fee exemption policy in Ghana: population estimates of changes in delivery service utilization in two regions. Ghana Medical Journal 41: 100–108. [PMC free article] [PubMed] [Google Scholar]
- Powell-Jackson T, Hanson K. 2012. Financial incentives for maternal health: impact of a national programme in Nepal. Journal of Health Economics 31: 271–284. [DOI] [PubMed] [Google Scholar]
- Ridde V, Morestin F. 2011. A scoping review of the literature on the abolition of user fees in health care services in Africa. Health Policy and Planning 26: 1–11. p [DOI] [PubMed] [Google Scholar]
- Ronsmans C, Graham WJ. 2006. Maternal mortality: who, when, where, and why. The Lancet 368: 1189–1200. [DOI] [PubMed] [Google Scholar]
- Samuelson PA. 1956. Social Indifference Curves. The Quarterly Journal of Economics 70: 1–22. [Google Scholar]
- Steinhardt LC, Aman I, Pakzad I, et al. 2011. Removing user fees for basic health services: a pilot study and national roll-out in Afghanistan. Health Policy and Planning 26: ii92–ii103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Todd PE. 2007. Chapter 60. Evaluating social programs with endogenous program placement and selection of the treated In: Schultz TP, Strauss JA. (eds). Handbook of Development Economics. Amsterdam: Elsevier, 3847–3894. [Google Scholar]
- UNICEF. 2011. Case Study on Narrowing the Gaps for Equity, Sierra Leone: Removing Health Care User Fees to Improve Prospects for Mothers and Children. Freetown: UNICEF. [Google Scholar]
- Villar J, Ba’aqeel H, Piaggio G. et al. 2001. WHO antenatal care randomised trial for the evaluation of a new model of routine antenatal care. The Lancet 357: 1551–1564. [DOI] [PubMed] [Google Scholar]
- Wilkinson D, Gouws E, Sach M, Abdool Karim SS. 2001. Effect of removing user fees on attendance for curative and preventive primary health care services in rural South Africa. Bulletin of the World Health Organization 79: 665–671. [PMC free article] [PubMed] [Google Scholar]
- Witter S, Khadka S, Nath H, Tiwari S. 2011. The national free delivery policy in Nepal: early evidence of its effects on health facilities. Health Policy and Planning 26: ii84–ii91. [DOI] [PubMed] [Google Scholar]
- Witter S, Dieng T, Mbengue D, Moreira I, De Brouwere V. 2010. The national free delivery and caesarean policy in Senegal: evaluating process and outcomes. Health Policy and Planning 25: 384–392. [DOI] [PubMed] [Google Scholar]
- Wooldridge JM. 2010. Econometric Analysis of Cross Section and Panel Data, 2nd edn. Cambridge, MA: MIT Press. [Google Scholar]
- Wooldridge JM. 2009. Introductory Econometrics: A Modern Approach, 4th edn. Canada: South-Western. [Google Scholar]
- World Bank. 2015. World Development Indicators [Online]. http://data.worldbank.org/country/malawi, Accessed 9 November 2015.
- World Health Organization. 2011. Burundi’s Adoption of Performance-Based-Finance to Fund Fee Exempt Health Services. Geneva: World Health Organization. [Google Scholar]
- Xu K, Evans DB, Kadama P. et al. 2006. Understanding the impact of eliminating user fees: Utilization and catastrophic health expenditures in Uganda. Social Science and Medicine 62: 866–876. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.