Abstract
Objective:
Review the clinical skills needed to recognize, diagnose, and manage binge-eating disorder (BED) in a primary care setting.
Data Sources:
A PubMed search of English-language publications (January 1, 2008–December 11, 2014) was conducted using the term binge-eating disorder. Relevant articles known to the authors were also included.
Study Selection/Data Extraction:
Publications focusing on preclinical topics (eg, characterization of receptors and neurotransmitter systems) without discussing clinical relevance were excluded. A total of 101 publications were included in this review.
Results:
Although BED is the most prevalent eating disorder, it is underdiagnosed and undertreated. BED can be associated with medical (eg, type 2 diabetes and metabolic syndrome) and psychiatric (eg, depression and anxiety) comorbidities that, if left untreated, can impair quality of life and functionality. Primary care physicians may find diagnosing and treating BED challenging because of insufficient knowledge of its new diagnostic criteria and available treatment options. Furthermore, individuals with BED may be reluctant to seek treatment because of shame, embarrassment, and a lack of awareness of the disorder. Several short assessment tools are available to screen for BED in primary care settings. Pharmacotherapy and psychotherapy should focus on reducing binge-eating behavior, thereby reducing medical and psychiatric complications.
Conclusions:
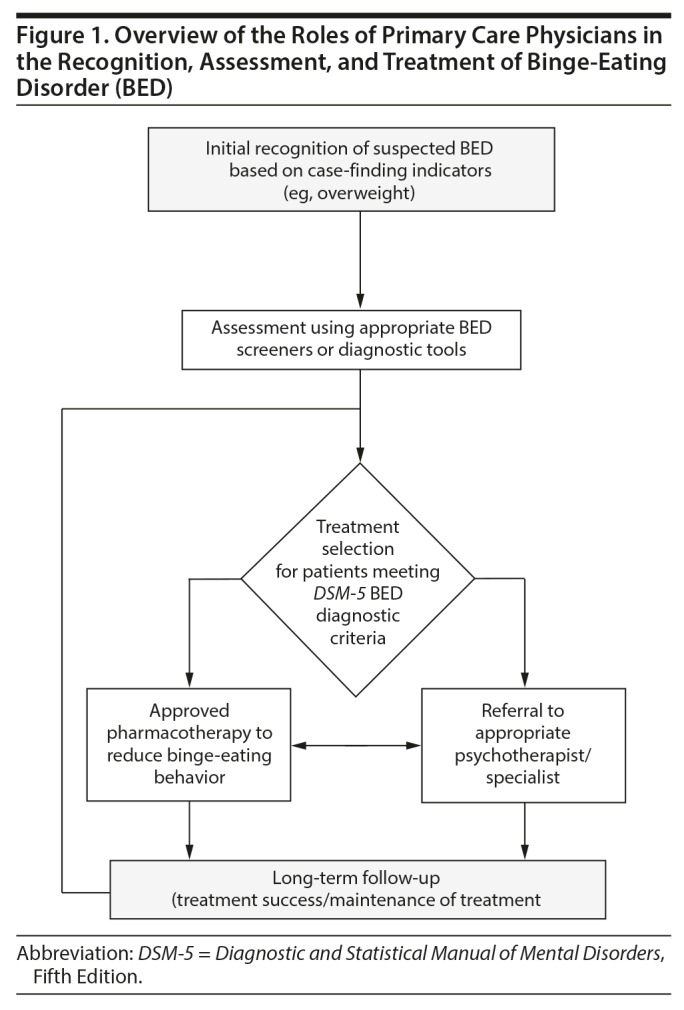
Overcoming primary care physician– and patient-related barriers is critical to accurately diagnose and appropriately treat BED. Primary care physicians should take an active role in the initial recognition and assessment of suspected BED based on case-finding indicators (eg, eating habits and being overweight), the initial treatment selection, and the long-term follow-up of patients who meet DSM-5 BED diagnostic criteria.
Clinical Points
■ Individuals with binge-eating disorder may exhibit medical and psychiatric comorbidities that can impair quality of life and functionality without adequate treatment.
■ Overcoming primary care physician and patient-related barriers is critical to accurately diagnosing and appropriately treating binge-eating disorder.
■ Primary care physicians should take an active role in the initial recognition and assessment of suspected binge-eating disorder, the initial treatment selection, and the long-term follow-up of patients who meet DSM-5 diagnostic criteria.
Binge-eating disorder (BED) received formal recognition as a distinct eating disorder in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).1 To be diagnosed with BED according to DSM-5 criteria (Table 1), there must be recurrent binge-eating episodes, occurring ≥ 1 time per week for ≥ 3 months, that are characterized by the consumption of larger amounts of food in a discrete period than is typical for most people and a lack of control of eating during these episodes. Binge-eating episodes must be associated with at least 3 of the following symptoms: eating more rapidly than normal, eating until feeling uncomfortable, eating large amounts of food when not physically hungry, eating alone because of embarrassment over the amount of food being consumed, or having feelings of disgust, guilt, or depression following a binge-eating episode. There must also be marked distress over the presence of binge eating.1 Unlike with bulimia nervosa (BN) and anorexia nervosa (AN), there are no recurrent inappropriate compensatory behaviors, such as excessive exercise or purging, in BED.1 The binge-eating frequency criterion in the DSM-5 is less stringent (at least once a week for 3 months)1 than that used in the DSM-IV-TR provisional BED diagnostic criterion (at least twice a week for 6 months).2
Table 1.
Summary of the DSM-5 Diagnostic Criteria for Binge-Eating Disordera
| Criterion A. Recurrent episodes of binge eating. An episode of binge eating is characterized by both of the following: |
|
|
| Criterion B. The binge eating episodes are associated with 3 (or more) of the following: |
|
|
|
|
|
| Criterion C. Marked distress regarding binge eating is present |
| Criterion D. The binge eating occurs, on average, at least once a week for 3 months |
| Criterion E. The binge eating is not associated with the recurrent use of inappropriate compensatory behavior as in bulimia nervosa and does not occur exclusively during the course of bulimia nervosa or anorexia nervosa |
Reprinted with permission from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (Copyright ©2013). American Psychiatric Association. All Rights Reserved.
Abbreviation: DSM-5 = Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
BED is more prevalent than AN and BN, with estimates of the lifetime prevalence of BED ranging from 1.9% to 2.8%.3,4 However, BED treatment rates are low. On the basis of data from the World Health Organization (WHO) World Mental Health Survey, < 40% of individuals with a lifetime diagnosis of BED have ever been treated for an eating disorder.4 Treatment rates for BED may be low because many primary care physicians (PCPs) find the diagnosis and treatment of BED challenging, and they have an insufficient knowledge of its new diagnostic criteria and treatment options.5,6 Obesity is common in individuals with BED, with up to 43% of individuals with BED reported to be obese.3,4
Left untreated, BED presents a significant public health concern because the increase in the risk of comorbid medical conditions (eg, metabolic syndrome) is greater than the risk posed by obesity alone7 and because BED is frequently comorbid with psychiatric disorders (eg, mood, anxiety, and substance use disorders).8–11 Thus, it is important for PCPs to recognize the signs of BED and its comorbid disorders and to determine the most appropriate course of treatment.
METHODS
In this review, the clinical skills necessary to recognize and diagnose BED, the management of BED, and the evaluation of comorbid conditions are discussed. The review is based on a comprehensive search of PubMed, which included publications from January 1, 2008, to December 11, 2014. The search was restricted to the titles and abstracts of English-language articles and used the term binge-eating disorder. Publications focusing solely on preclinical topics (eg, characterization of receptors, transmitters, and central nervous system pathways) without discussing the clinical relevance of the reported findings were excluded. Additional articles were also included on the basis of the authors’ knowledge. A total of 101 publications were included in this review.3,4,7–105
RESULTS
Symptoms, Characteristics, and Timecourse of BED
Diagnostic criteria for BED are based on eating behaviors and characteristics and do not exclude individuals on the basis of body weight (ie, normal-weight individuals can meet diagnostic criteria for BED).1 In brief, BED is characterized by recurrent binge-eating episodes that occur during a discrete period of time, consist of the consumption of more food than is typical of most people under similar circumstances, and are associated with feelings of loss of control over eating and marked distress.1 To be diagnosed with BED, binge-eating episodes must occur at least once a week for a minimum of 3 months.1 One study12 in individuals diagnosed with BED characterized binge-eating episodes as being, on average, 42 minutes in duration and occurring approximately 9 times each week.
Defining characteristics of BED include a sense of lack of control13 during binge-eating episodes and marked distress14 over binge eating. Compared with obese individuals without BED, obese individuals with BED express greater feelings of loss of control during eating episodes, even after controlling for negative affect and total calories consumed.13 Individuals with BED who exhibit marked distress over binge-eating behavior show increased eating disorder pathology compared to individuals who meet all BED diagnostic criteria except marked distress.14 In addition, increased reward sensitivity to food-related stimuli has been reported in obese women with BED compared with both normal-weight controls and obese women without BED15; similarly, impulsivity in response to food-related stimuli is elevated in obese individuals with BED compared with normal-weight controls.16 Obese individuals with BED also report higher scores for disorder-specific shame and guilt than obese individuals without BED.17 Although overvaluation of shape and weight is not included among the DSM-5 diagnostic criteria for BED, unlike in AN and BN, it has been demonstrated that overvaluation of shape and weight is reliably associated with the severity of eating pathology and has negative prognostic significance.18
Diagnostic crossover between BED and BN has been reported to occur in some individuals, with roughly comparable percentages of individuals crossing over to BN from BED (20%) and to BED from BN (23%).19 However, crossover between BED and AN is unusual, with the same study reporting no crossover to AN from BED or to BED from AN.19 One distinguishing characteristic of BED compared with AN and BN is the lack of recurrent inappropriate compensatory behaviors (eg, purging, laxative use, excessive exercise) in response to binge eating.1 However, individuals with BED also demonstrate a number of other distinguishing characteristics. For instance, a 2013 review20 noted that when individuals with BED were asked to consume an amount of food with which they were comfortable and did not consider a binge, those with BED still ate more than controls, whereas those with BN ate less than controls, which suggests that BED may be associated with more overeating in general. Furthermore, obese women with BED (but not nonobese women with BED) have been reported to express less “drive for thinness” compared with individuals with BN.21 However, given the lack of a significant difference between nonobese women with BED and women with BN regarding a drive for thinness, an influence of obesity on the reported difference between obese women with BED and women with BN cannot be excluded. In general, the prognosis for BED has been reported to be better than for BN, with higher percentages of individuals with BED no longer meeting diagnostic criteria at 15-, 30-, 45-, and 60-month follow-ups than individuals with BN, despite the fact that more individuals with BN sought treatment for their eating disorder.22 BED also differs from BN in regard to its later age at onset and lower persistence.4
BED is not a subtype of obesity. Although BED is strongly associated with obesity, it is found across body mass index categories.3,4 BED has been reported to cluster in families independent of the presence of obesity, and individuals with family histories of BED are at greater risk of obesity in adulthood than those with family histories of obesity and no BED.23 Individuals with BED have also been shown to differ from obese individuals without BED in regard to the quantity of food consumed outside of binges and in the motivation to eat under stressful conditions.24–26 Furthermore, individuals with BED who are obese exhibit more severe psychopathology than do obese individuals without BED,27 but psychopathology does not differ between obese and nonobese individuals with BED.28
The symptoms of BED typically begin during adolescence or young adulthood,1,4 with 1%–2% of adolescents experiencing BED.29 On the basis of epidemiologic data from the WHO Mental Health Survey, the mean (median) age at onset for BED is 23.3 (19.3) years4; the age at onset of eating disorder symptoms has been reported to be older in BED than in BN or AN.30,31 In the elderly, the characteristics of BED have been reported to be similar to those seen in younger adults. However, in elderly individuals, a later onset and a longer duration of illness has been reported.32
Across racial and ethnic groups, the lifetime prevalence of BED and the frequency of binge-eating episodes do not appear to differ substantially.33,34 However, lifetime 12-month prevalence rates of BED have been reported to be higher in women than in men, although the gender ratio is more balanced compared to other eating disorders.3,4 Hormonal fluctuations could be a factor influencing the higher BED prevalence rate in women. In a small study of unmedicated women with bipolar disorder who also met DSM-IV-TR criteria for BED, binge-eating episode frequency and severity increased the week before menses, and 80% of participants reported weight gain during menses.35 However, it is unclear if these findings would generalize to women with BED who do not have comorbid bipolar disorder.
Medical Comorbidities Associated With BED
In addition to its core eating disorder psychopathology, BED is associated with general medical and psychiatric comorbidities and with increased mortality relative to individuals who do not have eating disorders.7,36–38 Individuals with BED are at an increased lifetime risk for developing type 2 diabetes and hypertension compared with individuals without eating disorders.39,40 The risk of type 2 diabetes in individuals with BED was found to be elevated in males and in African Americans on the basis of multivariate regression analyses that included factors such as weight and age.36 Among individuals at risk for developing components of metabolic syndrome, individuals with BED reported higher 5-year rates of hypertension, dyslipidemia, type 2 diabetes, any metabolic syndrome component, and 2 or more metabolic syndrome components than individuals without BED.7 Although data related to sleep in a general population of individuals with BED are not available, sleep has been reported to be disturbed in women with BED, in whom a higher frequency of sleep problems before and during pregnancy and for 18 months after childbirth is observed relative to women who do not exhibit BED symptoms.37
Psychiatric Comorbidities and Psychological Aspects Associated With BED
Psychiatric comorbidities are also associated with BED. In a systematic review,41 10 of 14 studies reviewed noted an association between depression and BED. Across studies,8,9,11,42–44 approximately 30%–80% of individuals with BED have lifetime comorbid mood or anxiety disorders. Other psychiatric comorbidities and personality disorders reported in individuals with BED or eating disorders include gambling problems, bipolar disorder, and substance abuse, as well as avoidant, obsessive-compulsive, and borderline personality disorders.11,45–49
Compared with healthy individuals without an eating disorder, individuals with BED also show impairment in aspects of psychological well-being, including autonomy, environmental mastery, self-acceptance,50 and emotional regulation.51 In addition, though not a diagnostic criteria, overvaluation of shape and weight is reliably associated with eating pathology severity, psychological distress, and negative prognostic significance in individuals with BED.18
Impaired mental health in individuals with BED may also have direct consequences on suicidal behavior. In 1 study,52 women with BED and comorbid depression had higher rates of suicide attempts and completion than individuals with BED but without major depression. In another study,53 nearly 30% of individuals with BED reported suicidal ideation, especially those with alexithymia and depressive symptoms.
Quality of Life and Functional Impairments Associated With BED
Quality of life (QoL) is impaired in individuals with BED.54–56 In 1 study,54 patients with BED reported lower scores on multiple components of the Medical Outcomes Study Short Form 36-item Health Survey compared with a normative US sample and with obese individuals without BED. Additionally, obese individuals meeting criteria for BED have demonstrated significant reductions in QoL in areas of physical and mental health, cognitive function, and social interaction compared with obese individuals without BED and nonobese individuals with or without BED.55
Consistent with reported reductions in QoL, multiple studies10,54,55,57–61 have shown that functional impairment is observed in BED. In 1 study,60 impaired mental QoL was related to depressive symptoms and impaired physical QoL was related to walking ability. In another study,61 overall impairment in general functioning in individuals with BED was correlated with poor body image attitudes and a lack of physical activity. On the basis of data from the large WHO Mental Health Survey,4 46.7% of individuals with BED reported “any role impairment” and 13.2% reported “severe role impairment” on the Sheehan Disability Scale. Similarly, data from the same WHO survey indicated that early onset BED was associated with reduced odds of marriage among women (but not among men) and reduced odds of employment among men (but not among women).62
Risk Factors and Case-Finding Indicators Associated With BED
Although evidence suggests that BED has a strong genetic component,23 both genetic and environmental risk factors contribute to the development of BED. In a study of twins,23 59% of the variance in the core DSM-IV features of BED (ie, binge eating in the absence of compensatory behavior and diagnosis of AN or BN) were accounted for by environmental factors.
It is important for PCPs to consider these indicators when identifying suspected cases of BED in their practice. BED often co-occurs with obesity and type 2 diabetes,7 with binge-eating severity being one of the predictors for comorbidity.36 Given the poor prognosis for individuals with comorbid diabetes and eating disorders, it is recommended that individuals with diabetes be routinely assessed for an eating disorder.63 Table 2 lists case-finding indicators for BED.
Table 2.
Case-Finding Indicators for Binge-Eating Disorder in Primary Care Practices
| Individual/physical |
| Psychological |
|
|
|
| Family/relationships |
|
|
|
|
Other specific indicators for BED include childhood obesity and familial eating problems23,69 and having a parent with a mood disorder or substance use disorder69; a parental history of substance use disorder is associated with an earlier age at onset of BED.71 Exposure to traumatic life events or life stressors (eg, death of or separation from a friend or family member, termination of a relationship, history of physical abuse, accident) also increases the risk of BED and is likely to have occurred prior to the onset of symptoms.67,68 Histories of family discord, high parental demands or parental perfectionism, and parental separation are also reported to increase the risk of BED.69 In a Norwegian study,70 the stress of pregnancy was associated with increased BED risk, with factors such as worrying about and overevaluation of pregnancy-related weight gain increasing the risk of BED. The consequences of BED in pregnant women are important. Pregnant women meeting criteria for BED have been reported to consume more calories but fewer nutrients (including vitamin C and folic acid) and to gain weight faster during pregnancy than pregnant women not meeting criteria for BED,72,73 possibly negatively affecting fetal development.
The PCP’s Role in Recognizing and Diagnosing BED
Patients who are not obese3,4 may engage in bingeing and qualify for the diagnosis of BED, but binge eating disorder is prevalent among individuals seeking weight loss treatment.43 Individuals with BED often gain weight (≥ 5% of their body weight) in the year before seeking treatment.64,65 In addition, in a survey66 of individuals who were either diagnosed with BED or undiagnosed despite meeting DSM-5 criteria for BED, a majority of survey respondents reported seeing a general physician for their binge-eating–related symptoms. Therefore, PCPs, who often provide weight management care, are well positioned to identify patients with BED. Unfortunately, obese individuals with BED seeking medical attention from PCPs may focus on weight management rather than on their binge-eating behaviors.
While the effectiveness of screening all patients in primary care settings has not been evaluated, case finding among those at increased risk (Table 2) is a reasonable strategy. PCPs should consider their patients’ clinical history, including dietary and weight issues, to determine if risk factors for BED are present. As is true for other eating disorders, the most productive habit a PCP can adopt is to routinely ask about eating habits (Table 3) and to monitor changes in body weight as a part of a complete patient history (for instance, during the review of systems).
Table 3.
Suggested Diagnostic Questions to Identify Binge-Eating Disorder
| Do you think you eat more food than the average person your age? How much do you typically eat during the average day? |
| Do you experience feelings of loss of control over your eating and marked distress when you think about your eating habits? |
| How often (ie, times per week) do you binge eat? |
| Do you experience guilt or shame during or after an episode of binge eating? |
| Do any other members of your family have eating problems? |
Identification of BED is hindered by a general lack of assessment of weight and body mass index (BMI) by PCPs during routine visits. A survey of PCPs suggested that BMI was calculated rarely or never by 40% of PCPs; 42% of PCPs have never assessed their patients for BED.74 Assessing weight, BMI, and weight gain, however, is not sufficient to lead to the recognition of BED. Because shame and guilt are frequently observed in individuals with BED and can act as barriers to communicating about binge-eating symptoms,17,66 a reluctance to discuss eating habits may be a red flag for BED. Furthermore, many patients may not present with the chief complaint of an eating disorder or with signs of an eating disorder upon physical examination.75 Those individuals who do seek treatment for an eating disorder are often prompted by increased symptom severity, psychological distress including a sense of lack of control, interference with daily life, comorbid health conditions, and a desire to “get better.”76 However, these patients may focus on the BED-associated comorbidities as opposed to problematic eating behaviors76; therefore, the PCP needs to uncover the course of the patient’s issues to discern the antecedent condition.
Case-Finding Assessment Tools
Of the validated diagnostic and case-finding tools, the Eating Disorders Examination–Questionnaire77 and the Questionnaire of Eating and Weight Patterns–Revised,78 are 2 self-report instruments that may be used in primary care settings to assess eating disorders.79 It has also been reported that, in instances where a face-to-face clinical interview is not possible, the Eating Disorder Questionnaire–Online version may be an acceptable alternative.80 Although there are multiple diagnostic tools that can be used to assess BED, many are unlikely to be used in clinical settings because they are cumbersome. To that end, several short assessment tools (ie, the Eating Disorder Screen for Primary care,81 the 7-item Binge Eating Disorder Screener [BEDS-7],82 and the Eating Disorder Assessment for the DSM-5,83) have been developed that may be of more utility in primary care settings. However, only the BEDS-782 is specific for BED.
Available tools are based on interviews and subject reports, which can be time consuming to implement. The limited time available to PCPs during routine office visits may diminish the ability to utilize these tools for case finding. The early recognition and identification of a potential BED diagnosis is important because it may mitigate the long-term impact of BED in the patient. As such, eating disorder specialists need to consider developing time-efficient assessment tools that PCPs can use to effectively identify BED. If PCPs are unable or lack confidence in their ability to make a definitive diagnosis, the patient should be referred to a mental health specialist with experience in diagnosing and treating eating disorders.
Treatment and Long-Term Management of BED
Many patients with BED remain undiagnosed and, if managed at all, have received delayed treatment or inadequate treatment.84 Whatever strategy the PCP uses to recognize and diagnose BED, taking care to convey a nonjudgmental interest in helping the patient, communicating that eating disorders (including BED) are of medical concern and amenable to treatment, and using motivational interviewing principles to establish agreed-upon treatment goals and gain adherence with care are likely to be helpful. The PCP is ideally positioned to integrate treatment of BED with that of obesity and other conditions such as diabetes or depression. The main goal of BED treatment should be to reduce binge-eating behavior, not to promote weight management or weight loss, and thereby reduce the risk of medical and psychiatric complications.
After confirming a diagnosis of BED, the PCP should play an active role in the initial treatment selection, including prescribing approved pharmacotherapy and referring patients to an appropriate specialist who can provide psychotherapy. The PCP should also be the primary treatment coordinator, manage medical complications, and help determine the need for inpatient hospitalization for potential comorbidities or suicidality. Although PCPs with adequate training can initiate and manage the treatment of BED without a referral, because of the high incidence of comorbid psychiatric disorders in individuals with BED, referral to a mental health professional should be considered for a thorough evaluation and the subsequent management of comorbidities. Lastly, PCPs should take a leading role in the long-term follow-up of their patients with BED, including assessment of initial treatment success and the maintenance of treatment.
There are several treatment options that have been studied in adults with BED; however, there is a general lack of treatment and intervention studies in adolescent and young adult populations.85 Psychotherapy has demonstrated benefit in the treatment of BED. In general, cognitive-behavioral therapy (CBT), interpersonal therapy, and dialectic therapy reduce binge-eating behavior, associated eating disorder psychopathology, and depressive symptoms without producing clinically meaningful weight loss.86–89 At least 1 study90 reported that the frequency of binge eating in individuals provided with a self-help version of CBT in combination with usual care was not significantly different compared to those provided usual care alone. In another study,31 CBT resulted in a higher remission rate from eating disorder symptoms in individuals with BED compared with individuals with BN despite the fact that individuals with BED had a higher rate of treatment discontinuation. Overall, a meta-analysis91 of clinical trials of psychotherapy (a majority of which were CBT trials) and structured self-help in adults with BED reported statistically significant effect sizes (95% CI) for reductions in binge-eating frequency versus controls (psychotherapy: 0.82 [0.41–1.22], structured self-help: 0.84 [0.37–1.30]) and versus pretreatment values (psychotherapy: 1.46 [1.12–1.80], structured self-help: 1.09 [0.67–1.50]) but not for reductions in body weight. Lisdexamfetamine dimesylate is currently the only pharmacotherapy approved by the US Food and Drug Administration for the treatment of BED; it is approved for the treatment of adults with mild to moderate BED.92 In a phase 2, randomized, placebo-controlled study, significantly greater reductions in binge-eating days per week were observed with lisdexamfetamine dimesylate than with placebo.93 In 2 large, identically designed, phase 3 registration trials, dose-optimized lisdexamfetamine dimesylate produced clinically meaningful and statistically superior reductions in binge-eating days per week compared with placebo (the primary efficacy endpoint) in adults with protocol-defined moderate to severe BED.94 In the phase 3 studies,94 lisdexamfetamine dimesylate treatment also resulted in statistically greater response than placebo on outcomes of global improvement in BED pathology on the Clinical Global Impressions–Improvement scale, on 4-week cessation of binge eating, on BED-related obsessive and compulsive psychopathology as measured on the Yale-Brown Obsessive Compulsive Scale Modified for Binge Eating, on the percent weight reduction from baseline, and on fasting triglycerides.
Several other pharmacotherapies have been investigated for the treatment of BED.95 Antidepressants, including selective serotonin reuptake inhibitors and serotonin-norepinephrine reuptake inhibitors, have been examined in several randomized controlled clinical trials32,87,96–99 with varied success. In a meta-analysis of placebo-controlled trials, the antidepressants citalopram, fluoxetine, fluvoxamine, imipramine, and sertraline produced greater remission rates than placebo, but there was substantial variability across studies, and consistent reductions in binge frequency or weight loss compared with placebo were not reliably observed.100 The anticonvulsant topiramate significantly reduced binge frequency and weight compared with placebo in 2 randomized, placebo-controlled studies.101,102 The weight loss drug orlistat produced significantly greater weight loss and produced greater reductions in some aspects of eating pathology than did placebo in obese individuals with BED.103 Treatment with the anorexiant sibutramine significantly reduced binge-eating days per week and produced greater weight loss than placebo in individuals with BED,104 but this agent has been withdrawn from the market as a result of increased cardiovascular risk in individuals with preexisting cardiovascular conditions.105
CONCLUSION
Although BED is the most common eating disorder,3 it often goes unrecognized, undiagnosed, and untreated. This may be because it only recently received official designation as an eating disorder in the DSM-5. Left untreated, BED may negatively impact QoL and functionality. BED is also associated with a number of physical and mental comorbidities. Therefore, despite limitations of time, it is important for PCPs to be aware of risk factors that increase the likelihood of BED; take thorough patient histories, which include assessments of eating habits and changes in body weight; and pursue further case finding among those at increased risk for BED. Despite showing similar psychopathology, nonobese individuals with BED tend to be younger and more reluctant to seek treatment; in these individuals, early recognition is particularly important. To aid in diagnosis, time-efficient case-finding tools can be utilized by PCPs.
Figure 1 provides a schematic overview of the roles of PCPs in the initial recognition and assessment of suspected BED symptoms based on case-finding indicators (eg, eating habits and being overweight, see Table 2) and the initial treatment selection and long-term follow-up for those patients who meet DSM-5 diagnostic criteria. In brief, if BED is suspected, diagnostic evaluations should assess the presence of BED symptoms and also medical or psychiatric comorbidities. The PCP should also be aware of traumatic life events or the presence of life stressors and evaluate how the patient is handling these life stressors. After considering initial treatment options, referral to the appropriate mental health professionals or multidisciplinary management with these specialists is recommended as necessary. The management of BED should focus on reducing binge behavior through a multidimensional treatment plan, which potentially includes the use of approved pharmacotherapy and the appropriate psychotherapy. Regardless of treatment selection, PCPs should take a lead role in the long-term follow-up to assess treatment success and maintenance.
Figure 1.
Overview of the Roles of Primary Care Physicians in the Recognition, Assessment, and Treatment of Binge-Eating Disorder (BED)
Drug names:
citalopram (Celexa and others), fluoxetine (Prozac and others), fluvoxamine (Luvox and others), imipramine (Tofranil and others), lisdexamfetamine (Vyvanse), orlistat (Xenical), sertraline (Zoloft and others), topiramate (Topamax and others).
No trade:
sibutramine.
Potential conflicts of interest:
Dr Kornstein holds research grants from Forest, Palatin Technologies, and Takeda; is a consultant and/or serves on advisory boards for Allergan, Forest, Naurex, Eli Lilly, Pfizer, Shire, and Takeda; and receives royalties from Guilford Press. Dr Kunovac is the founder of Altea Research Institute; a cofounder of Excell Research, Inc; and a consultant and/or serves on advisory boards for AstraZeneca, Bristol-Myers Squibb, Pfizer, Janssen, Novartis, and Sunovion. Dr Herman is an employee of Shire and holds stock and stock options in Shire Development LLC. Dr Culpepper serves as an advisor or consultant for AstraZeneca, Forest, Merck, Shire PLC, Lundbeck A/S, Sunovion, and Takeda; owns stock in M3 (My Mood Monitor); and receives royalties from UpToDate and the Oxford University Press. Dr Culpepper is the journal’s editor-in-chief; he was not involved in the editorial review or decision to publish this article.
Funding/support:
Shire Development LLC provided funding to Complete Healthcare Communications, Inc (Chadds Ford, Pennsylvania) for support in writing and editing this manuscript.
Role of the sponsor:
The sponsor supported writing and editing of this manuscript. The content of this manuscript, the ultimate interpretation, and the decision to submit it for publication in The Primary Care Companion for CNS Disorders was made by the authors independently.
Acknowledgments:
Under the direction of the authors, writing assistance was provided by Stefan Kolata, PhD, and Craig Slawecki, PhD (employees of Complete Healthcare Communications, Inc). Editorial assistance in the form of proofreading, copy editing, and fact checking was also provided by Complete Healthcare Communications, Inc. Drs Kolata and Slawecki report no other conflicts of interest realted to the subject of this article.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fifth Edition. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 3.Hudson JI, Hiripi E, Pope HG, Jr, et al. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61(3):348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kessler RC, Berglund PA, Chiu WT, et al. The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biol Psychiatry. 2013;73(9):904–914. doi: 10.1016/j.biopsych.2012.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Currin L, Waller G, Schmidt U. Primary care physicians’ knowledge of and attitudes toward the eating disorders: do they affect clinical actions? Int J Eat Disord. 2009;42(5):453–458. doi: 10.1002/eat.20636. [DOI] [PubMed] [Google Scholar]
- 6.Allen KL, Fursland A, Watson H, et al. Eating disorder diagnoses in general practice settings: comparison with structured clinical interview and self-report questionnaires. J Ment Health. 2011;20(3):270–280. doi: 10.3109/09638237.2011.562259. [DOI] [PubMed] [Google Scholar]
- 7.Hudson JI, Lalonde JK, Coit CE, et al. Longitudinal study of the diagnosis of components of the metabolic syndrome in individuals with binge-eating disorder. Am J Clin Nutr. 2010;91(6):1568–1573. doi: 10.3945/ajcn.2010.29203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guerdjikova AI, McElroy SL, Kotwal R, et al. Comparison of obese men and women with binge eating disorder seeking weight management. Eat Weight Disord. 2007;12(1):e19–e23. doi: 10.1007/BF03327777. [DOI] [PubMed] [Google Scholar]
- 9.Grilo CM, White MA, Barnes RD, et al. Psychiatric disorder comorbidity and correlates in an ethnically diverse sample of obese patients with binge eating disorder in primary care settings. Compr Psychiatry. 2013;54(3):209–216. doi: 10.1016/j.comppsych.2012.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grucza RA, Przybeck TR, Cloninger CR. Prevalence and correlates of binge eating disorder in a community sample. Compr Psychiatry. 2007;48(2):124–131. doi: 10.1016/j.comppsych.2006.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Javaras KN, Pope HG, Lalonde JK, et al. Co-occurrence of binge-eating disorder with psychiatric and medical disorders. J Clin Psychiatry. 2008;69(2):266–273. doi: 10.4088/jcp.v69n0213. [DOI] [PubMed] [Google Scholar]
- 12.Schreiber-Gregory DN, Lavender JM, Engel SG, et al. Examining duration of binge eating episodes in binge eating disorder. Int J Eat Disord. 2013;46(8):810–814. doi: 10.1002/eat.22164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pollert GA, Engel SG, Schreiber-Gregory DN, et al. The role of eating and emotion in binge eating disorder and loss of control eating. Int J Eat Disord. 2013;46(3):233–238. doi: 10.1002/eat.22061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grilo CM, White MA. A controlled evaluation of the distress criterion for binge eating disorder. J Consult Clin Psychol. 2011;79(4):509–514. doi: 10.1037/a0024259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schag K, Schönleber J, Teufel M, et al. Food-related impulsivity in obesity and binge eating disorder—a systematic review. Obes Rev. 2013;14(6):477–495. doi: 10.1111/obr.12017. [DOI] [PubMed] [Google Scholar]
- 16.Schag K, Teufel M, Junne F, et al. Impulsivity in binge eating disorder: food cues elicit increased reward responses and disinhibition. PLoS ONE. 2013;8(10):e76542. doi: 10.1371/journal.pone.0076542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Albohn-Kühne C, Rief W. Shame, guilt and social anxiety in obesity with binge-eating disorder. Psychother Psychosom Med Psychol. 2011;61(9–10):412–417. doi: 10.1055/s-0031-1284334. [DOI] [PubMed] [Google Scholar]
- 18.Grilo CM. Why no cognitive body image feature such as overvaluation of shape/weight in the binge eating disorder diagnosis? Int J Eat Disord. 2013;46(3):208–211. doi: 10.1002/eat.22082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stice E, Marti CN, Rohde P. Prevalence, incidence, impairment, and course of the proposed DSM-5 eating disorder diagnoses in an 8-year prospective community study of young women. J Abnorm Psychol. 2013;122(2):445–457. doi: 10.1037/a0030679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Heaner MK, Walsh BT. A history of the identification of the characteristic eating disturbances of bulimia nervosa, binge eating disorder and anorexia nervosa. Appetite. 2013;65:185–188. doi: 10.1016/j.appet.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 21.Barry DT, Grilo CM, Masheb RM. Comparison of patients with bulimia nervosa, obese patients with binge eating disorder, and nonobese patients with binge eating disorder. J Nerv Ment Dis. 2003;191(9):589–594. doi: 10.1097/01.nmd.0000087185.95446.65. [DOI] [PubMed] [Google Scholar]
- 22.Fairburn CG, Cooper Z, Doll HA, et al. The natural course of bulimia nervosa and binge eating disorder in young women. Arch Gen Psychiatry. 2000;57(7):659–665. doi: 10.1001/archpsyc.57.7.659. [DOI] [PubMed] [Google Scholar]
- 23.Hudson JI, Lalonde JK, Berry JM, et al. Binge-eating disorder as a distinct familial phenotype in obese individuals. Arch Gen Psychiatry. 2006;63(3):313–319. doi: 10.1001/archpsyc.63.3.313. [DOI] [PubMed] [Google Scholar]
- 24.Guss JL, Kissileff HR, Devlin MJ, et al. Binge size increases with body mass index in women with binge-eating disorder. Obes Res. 2002;10(10):1021–1029. doi: 10.1038/oby.2002.139. [DOI] [PubMed] [Google Scholar]
- 25.Yanovski SZ, Leet M, Yanovski JA, et al. Food selection and intake of obese women with binge-eating disorder. Am J Clin Nutr. 1992;56(6):975–980. doi: 10.1093/ajcn/56.6.975. [DOI] [PubMed] [Google Scholar]
- 26.Schulz S, Laessle RG. Stress-induced laboratory eating behavior in obese women with binge eating disorder. Appetite. 2012;58(2):457–461. doi: 10.1016/j.appet.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 27.Fandiño J, Moreira RO, Preissler C, et al. Impact of binge eating disorder in the psychopathological profile of obese women. Compr Psychiatry. 2010;51(2):110–114. doi: 10.1016/j.comppsych.2009.03.011. [DOI] [PubMed] [Google Scholar]
- 28.Dingemans AE, van Furth EF. Binge eating disorder psychopathology in normal weight and obese individuals. Int J Eat Disord. 2012;45(1):135–138. doi: 10.1002/eat.20905. [DOI] [PubMed] [Google Scholar]
- 29.Schneider M. Bulimia nervosa and binge-eating disorder in adolescents. Adolesc Med. 2003;14(1):119–131. [PubMed] [Google Scholar]
- 30.Baiano M, Salvo P, Righetti P, et al. Exploring health-related quality of life in eating disorders by a cross-sectional study and a comprehensive review. BMC Psychiatry. 2014;14(1):165. doi: 10.1186/1471-244X-14-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Agüera Z, Riesco N, Jiménez-Murcia S, et al. Cognitive behaviour therapy response and dropout rate across purging and nonpurging bulimia nervosa and binge eating disorder: DSM-5 implications. BMC Psychiatry. 2013;13(1):285. doi: 10.1186/1471-244X-13-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guerdjikova AI, McElroy SL, Winstanley EL, et al. Duloxetine in the treatment of binge eating disorder with depressive disorders: a placebo-controlled trial. Int J Eat Disord. 2012;45(2):281–289. doi: 10.1002/eat.20946. [DOI] [PubMed] [Google Scholar]
- 33.Franko DL, Thompson-Brenner H, Thompson DR, et al. Racial/ethnic differences in adults in randomized clinical trials of binge eating disorder. J Consult Clin Psychol. 2012;80(2):186–195. doi: 10.1037/a0026700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Marques L, Alegria M, Becker AE, et al. Comparative prevalence, correlates of impairment, and service utilization for eating disorders across US ethnic groups: implications for reducing ethnic disparities in health care access for eating disorders. Int J Eat Disord. 2011;44(5):412–420. doi: 10.1002/eat.20787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schoofs N, Chen F, Bräunig P, et al. Binge eating disorder and menstrual cycle in unmedicated women with bipolar disorder. J Affect Disord. 2011;129(1–3):75–78. doi: 10.1016/j.jad.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 36.Webb JB, Applegate KL, Grant JP. A comparative analysis of type 2 diabetes and binge eating disorder in a bariatric sample. Eat Behav. 2011;12(3):175–181. doi: 10.1016/j.eatbeh.2011.04.007. [DOI] [PubMed] [Google Scholar]
- 37.Ulman TF, Von Holle A, Torgersen L, et al. Sleep disturbances and binge eating disorder symptoms during and after pregnancy. Sleep. 2012;35(10):1403–1411. doi: 10.5665/sleep.2124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Suokas JT, Suvisaari JM, Gissler M, et al. Mortality in eating disorders: a follow-up study of adult eating disorder patients treated in tertiary care, 1995–2010. Psychiatry Res. 2013;210(3):1101–1106. doi: 10.1016/j.psychres.2013.07.042. [DOI] [PubMed] [Google Scholar]
- 39.Raevuori A, Suokas J, Haukka J, et al. Highly increased risk of type 2 diabetes in patients with binge eating disorder and bulimia nervosa. Int J Eat Disord. 2015;48(6):555–562. doi: 10.1002/eat.22334. [DOI] [PubMed] [Google Scholar]
- 40.Stein DJ, Aguilar-Gaxiola S, Alonso J, et al. Associations between mental disorders and subsequent onset of hypertension. Gen Hosp Psychiatry. 2014;36(2):142–149. doi: 10.1016/j.genhosppsych.2013.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Araujo DM, Santos GF, Nardi AE. Binge eating disorder and depression: a systematic review. World J Biol Psychiatry. 2010;11(2 pt 2):199–207. doi: 10.3109/15622970802563171. [DOI] [PubMed] [Google Scholar]
- 42.Grilo CM, White MA, Masheb RM. DSM-IV psychiatric disorder comorbidity and its correlates in binge eating disorder. Int J Eat Disord. 2009;42(3):228–234. doi: 10.1002/eat.20599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jones-Corneille LR, Wadden TA, Sarwer DB, et al. Axis I psychopathology in bariatric surgery candidates with and without binge eating disorder: results of structured clinical interviews. Obes Surg. 2012;22(3):389–397. doi: 10.1007/s11695-010-0322-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schulz S, Laessle RG. Associations of negative affect and eating behavior in obese women with and without binge eating disorder. Eat Weight Disord. 2010;15(4):e287–e293. doi: 10.1007/BF03325311. [DOI] [PubMed] [Google Scholar]
- 45.Yip SW, White MA, Grilo CM, et al. An exploratory study of clinical measures associated with subsyndromal pathological gambling in patients with binge eating disorder. J Gambl Stud. 2011;27(2):257–270. doi: 10.1007/s10899-010-9207-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ramacciotti CE, Paoli RA, Marcacci G, et al. Relationship between bipolar illness and binge-eating disorders. Psychiatry Res. 2005;135(2):165–170. doi: 10.1016/j.psychres.2004.04.014. [DOI] [PubMed] [Google Scholar]
- 47.Gearhardt AN, White MA, Masheb RM, et al. An examination of food addiction in a racially diverse sample of obese patients with binge eating disorder in primary care settings. Compr Psychiatry. 2013;54(5):500–505. doi: 10.1016/j.comppsych.2012.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gearhardt AN, White MA, Masheb RM, et al. An examination of the food addiction construct in obese patients with binge eating disorder. Int J Eat Disord. 2012;45(5):657–663. doi: 10.1002/eat.20957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Friborg O, Martinussen M, Kaiser S, et al. Personality disorders in eating disorder not otherwise specified and binge eating disorder: a meta-analysis of comorbidity studies. J Nerv Ment Dis. 2014;202(2):119–125. doi: 10.1097/NMD.0000000000000080. [DOI] [PubMed] [Google Scholar]
- 50.Tomba E, Offidani E, Tecuta L, et al. Psychological well-being in out-patients with eating disorders: a controlled study. Int J Eat Disord. 2014;47(3):252–258. doi: 10.1002/eat.22197. [DOI] [PubMed] [Google Scholar]
- 51.Brockmeyer T, Skunde M, Wu M, et al. Difficulties in emotion regulation across the spectrum of eating disorders. Compr Psychiatry. 2014;55(3):565–571. doi: 10.1016/j.comppsych.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 52.Pisetsky EM, Thornton LM, Lichtenstein P, et al. Suicide attempts in women with eating disorders. J Abnorm Psychol. 2013;122(4):1042–1056. doi: 10.1037/a0034902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Carano A, De Berardis D, Campanella D, et al. Alexithymia and suicide ideation in a sample of patients with binge eating disorder. J Psychiatr Pract. 2012;18(1):5–11. doi: 10.1097/01.pra.0000410982.08229.99. [DOI] [PubMed] [Google Scholar]
- 54.Masheb RM, Grilo CM. Quality of life in patients with binge eating disorder. Eat Weight Disord. 2004;9(3):194–199. doi: 10.1007/BF03325066. [DOI] [PubMed] [Google Scholar]
- 55.Perez M, Warren CS. The relationship between quality of life, binge-eating disorder, and obesity status in an ethnically diverse sample. Obesity (Silver Spring) 2012;20(4):879–885. doi: 10.1038/oby.2011.89. [DOI] [PubMed] [Google Scholar]
- 56.Winkler LA, Christiansen E, Lichtenstein MB, et al. Quality of life in eating disorders: a meta-analysis. Psychiatry Res. 2014;219(1):1–9. doi: 10.1016/j.psychres.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 57.Folope V, Chapelle C, Grigioni S, et al. Impact of eating disorders and psychological distress on the quality of life of obese people. Nutrition. 2012;28(7–8):e7–e13. doi: 10.1016/j.nut.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 58.Sandberg RM, Dahl JK, Vedul-Kjelsås E, et al. Health-related quality of life in obese presurgery patients with and without binge eating disorder, and subdiagnostic binge eating disorders. J Obes. 2013;2013:878310. doi: 10.1155/2013/878310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kolotkin RL, Westman EC, Østbye T, et al. Does binge eating disorder impact weight-related quality of life? Obes Res. 2004;12(6):999–1005. doi: 10.1038/oby.2004.122. [DOI] [PubMed] [Google Scholar]
- 60.Vancampfort D, De Herdt A, Vanderlinden J, et al. Health related quality of life, physical fitness and physical activity participation in treatment-seeking obese persons with and without binge eating disorder. Psychiatry Res. 2014;216(1):97–102. doi: 10.1016/j.psychres.2014.01.015. [DOI] [PubMed] [Google Scholar]
- 61.Vancampfort D, Probst M, Adriaens A, et al. Clinical correlates of global functioning in obese treatment seeking persons with binge eating disorder. Psychiatr Danub. 2014;26(3):256–260. [PubMed] [Google Scholar]
- 62.Kessler RC, Shahly V, Hudson JI, et al. A comparative analysis of role attainment and impairment in binge-eating disorder and bulimia nervosa: results from the WHO World Mental Health Surveys. Epidemiol Psychiatr Sci. 2014;23(1):27–41. doi: 10.1017/S2045796013000516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gagnon C, Aimé A, Bélanger C, et al. Comorbid diabetes and eating disorders in adult patients: assessment and considerations for treatment. Diabetes Educ. 2012;38(4):537–542. doi: 10.1177/0145721712446203. [DOI] [PubMed] [Google Scholar]
- 64.Masheb RM, White MA, Grilo CM. Substantial weight gains are common prior to treatment-seeking in obese patients with binge eating disorder. Compr Psychiatry. 2013;54(7):880–884. doi: 10.1016/j.comppsych.2013.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ivezaj V, Kalebjian R, Grilo CM, et al. Comparing weight gain in the year prior to treatment for overweight and obese patients with and without binge eating disorder in primary care. J Psychosom Res. 2014;77(2):151–154. doi: 10.1016/j.jpsychores.2014.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Herman BK, Safikhani S, Hengerer D, et al. The patient experience with DSM-5–defined binge eating disorder: characteristics, barriers to treatment, and implications for primary care physicians. Postgrad Med. 2014;126(5):52–63. doi: 10.3810/pgm.2014.09.2800. [DOI] [PubMed] [Google Scholar]
- 67.Pike KM, Wilfley D, Hilbert A, et al. Antecedent life events of binge-eating disorder. Psychiatry Res. 2006;142(1):19–29. doi: 10.1016/j.psychres.2005.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Degortes D, Santonastaso P, Zanetti T, et al. Stressful life events and binge eating disorder. Eur Eat Disord Rev. 2014;22(5):378–382. doi: 10.1002/erv.2308. [DOI] [PubMed] [Google Scholar]
- 69.Striegel-Moore RH, Dohm FA, Kraemer HC, et al. Health services use in women with a history of bulimia nervosa or binge eating disorder. Int J Eat Disord. 2005;37(1):11–18. doi: 10.1002/eat.20090. [DOI] [PubMed] [Google Scholar]
- 70.Knoph Berg C, Torgersen L, Von Holle A, et al. Factors associated with binge eating disorder in pregnancy. Int J Eat Disord. 2011;44(2):124–133. doi: 10.1002/eat.20797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Blomquist KK, Masheb RM, White MA, et al. Parental substance use history of overweight men and women with binge eating disorder is associated with distinct developmental trajectories and comorbid mood disorder. Compr Psychiatry. 2011;52(6):693–700. doi: 10.1016/j.comppsych.2010.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Siega-Riz AM, Haugen M, Meltzer HM, et al. Nutrient and food group intakes of women with and without bulimia nervosa and binge eating disorder during pregnancy. Am J Clin Nutr. 2008;87(5):1346–1355. doi: 10.1093/ajcn/87.5.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zerwas SC, Von Holle A, Perrin EM, et al. Gestational and postpartum weight change patterns in mothers with eating disorders. Eur Eat Disord Rev. 2014;22(6):397–404. doi: 10.1002/erv.2314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Crow SJ, Peterson CB, Levine AS, et al. A survey of binge eating and obesity treatment practices among primary care providers. Int J Eat Disord. 2004;35(3):348–353. doi: 10.1002/eat.10266. [DOI] [PubMed] [Google Scholar]
- 75.Williams PM, Goodie J, Motsinger CD. Treating eating disorders in primary care. Am Fam Physician. 2008;77(2):187–195. [PubMed] [Google Scholar]
- 76.Hepworth N, Paxton SJ. Pathways to help-seeking in bulimia nervosa and binge eating problems: a concept mapping approach. Int J Eat Disord. 2007;40(6):493–504. doi: 10.1002/eat.20402. [DOI] [PubMed] [Google Scholar]
- 77.Fairburn CG, Beglin SJ. Assessment of eating disorders: interview or self-report questionnaire? Int J Eat Disord. 1994;16(4):363–370. [PubMed] [Google Scholar]
- 78.Spitzer RL, Yanovski S, Wadden T, et al. Binge eating disorder: its further validation in a multisite study. Int J Eat Disord. 1993;13(2):137–153. [PubMed] [Google Scholar]
- 79.Barnes RD, Masheb RM, White MA, et al. Comparison of methods for identifying and assessing obese patients with binge eating disorder in primary care settings. Int J Eat Disord. 2011;44(2):157–163. doi: 10.1002/eat.20802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.ter Huurne ED, de Haan HA, ten Napel-Schutz MC, et al. Is the Eating Disorder Questionnaire-Online (EDQ-O) a valid diagnostic instrument for the DSM-IV-TR classification of eating disorders? Compr Psychiatry. 2015;57:167–176. doi: 10.1016/j.comppsych.2014.10.019. [DOI] [PubMed] [Google Scholar]
- 81.Cotton MA, Ball C, Robinson P. Four simple questions can help screen for eating disorders. J Gen Intern Med. 2003;18(1):53–56. doi: 10.1046/j.1525-1497.2003.20374.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Herman BK, Deal L, DiBenedetti DB, et al. Development of the 7-Item Binge-Eating Disorder Screener (BEDS-7) Prim Care Companion CNS Disorder. In press doi: 10.4088/PCC.15m01896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sysko R, Glasofer DR, Hildebrandt T, et al. The Eating Disorder Assessment for DSM-5 (EDA-5): development and validation of a structured interview for feeding and eating disorders. Int J Eat Disord. 2015;48(5):452–463. doi: 10.1002/eat.22388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.de Zwaan M, Herpertz S, Zipfel S, et al. INTERBED: Internet-based guided self-help for overweight and obese patients with full or subsyndromal binge eating disorder. A multicenter randomized controlled trial. Trials. 2012;13(1):220. doi: 10.1186/1745-6215-13-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bailey AP, Parker AG, Colautti LA, et al. Mapping the evidence for the prevention and treatment of eating disorders in young people. J Eat Disord. 2014;2:5. doi: 10.1186/2050-2974-2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.McElroy SL, Guerdjikova AI, Mori N, et al. Pharmacological management of binge eating disorder: current and emerging treatment options. Ther Clin Risk Manag. 2012;8:219–241. doi: 10.2147/TCRM.S25574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Grilo CM, Masheb RM, Wilson GT. Efficacy of cognitive behavioral therapy and fluoxetine for the treatment of binge eating disorder: a randomized double-blind placebo-controlled comparison. Biol Psychiatry. 2005;57(3):301–309. doi: 10.1016/j.biopsych.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 88.Fischer S, Meyer AH, Dremmel D, et al. Short-term cognitive-behavioral therapy for binge eating disorder: long-term efficacy and predictors of long-term treatment success. Behav Res Ther. 2014;58:36–42. doi: 10.1016/j.brat.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 89.Grilo CM, Masheb RM. A randomized controlled comparison of guided self-help cognitive behavioral therapy and behavioral weight loss for binge eating disorder. Behav Res Ther. 2005;43(11):1509–1525. doi: 10.1016/j.brat.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 90.Grilo CM, Masheb RM, White MA, et al. Treatment of binge eating disorder in racially and ethnically diverse obese patients in primary care: randomized placebo-controlled clinical trial of self-help and medication. Behav Res Ther. 2014;58:1–9. doi: 10.1016/j.brat.2014.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Vocks S, Tuschen-Caffier B, Pietrowsky R, et al. Meta-analysis of the effectiveness of psychological and pharmacological treatments for binge eating disorder. Int J Eat Disord. 2010;43(3):205–217. doi: 10.1002/eat.20696. [DOI] [PubMed] [Google Scholar]
- 92.Vyvanse (lisdexamfetamine dimesylate) [package insert] Wayne, PA: Full Prescribing Information, Shire US Inc; 2015. [Google Scholar]
- 93.McElroy SL, Hudson JI, Mitchell JE, et al. Efficacy and safety of lisdexamfetamine for treatment of adults with moderate to severe binge-eating disorder: a randomized clinical trial. JAMA Psychiatry. 2015;72(3):235–246. doi: 10.1001/jamapsychiatry.2014.2162. [DOI] [PubMed] [Google Scholar]
- 94.McElroy SL, Hudson J, Ferreira-Cornwell MC, et al. Lisdexamfetamine dimesylate for adults with moderate to severe binge eating disorder: results of two pivotal phase 3 randomized controlled trials. Neuropsychopharmacology. 2016;41(5):1251–1260. doi: 10.1038/npp.2015.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Reas DL, Grilo CM. Current and emerging drug treatments for binge eating disorder. Expert Opin Emerg Drugs. 2014;19(1):99–142. doi: 10.1517/14728214.2014.879291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Pearlstein T, Spurell E, Hohlstein LA, et al. A double-blind, placebo-controlled trial of fluvoxamine in binge eating disorder: a high placebo response. Arch Womens Ment Health. 2003;6(2):147–151. doi: 10.1007/s00737-003-0172-8. [DOI] [PubMed] [Google Scholar]
- 97.Guerdjikova AI, McElroy SL, Kotwal R, et al. High-dose escitalopram in the treatment of binge-eating disorder with obesity: a placebo-controlled monotherapy trial. Hum Psychopharmacol. 2008;23(1):1–11. doi: 10.1002/hup.899. [DOI] [PubMed] [Google Scholar]
- 98.Devlin MJ, Goldfein JA, Petkova E, et al. Cognitive behavioral therapy and fluoxetine as adjuncts to group behavioral therapy for binge eating disorder. Obes Res. 2005;13(6):1077–1088. doi: 10.1038/oby.2005.126. http://dx.doi.org/10.1038/oby.2005.126 doi:10.1038/oby.2005.126 [DOI] [PubMed] [Google Scholar]
- 99.McElroy SL, Hudson JI, Malhotra S, et al. Citalopram in the treatment of binge-eating disorder: a placebo-controlled trial. J Clin Psychiatry. 2003;64(7):807–813. doi: 10.4088/jcp.v64n0711. doi:10.4088/JCP.v64n0711 [DOI] [PubMed] [Google Scholar]
- 100.Stefano SC, Bacaltchuk J, Blay SL, et al. Antidepressants in short-term treatment of binge eating disorder: systematic review and meta-analysis. Eat Behav. 2008;9(2):129–136. doi: 10.1016/j.eatbeh.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 101.McElroy SL, Arnold LM, Shapira NA, et al. Topiramate in the treatment of binge eating disorder associated with obesity: a randomized, placebo-controlled trial. Am J Psychiatry. 2003;160(2):255–261. doi: 10.1176/appi.ajp.160.2.255. [DOI] [PubMed] [Google Scholar]
- 102.McElroy SL, Hudson JI, Capece JA, et al. Topiramate Binge Eating Disorder Research Group. Topiramate for the treatment of binge eating disorder associated with obesity: a placebo-controlled study. Biol Psychiatry. 2007;61(9):1039–1048. doi: 10.1016/j.biopsych.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 103.Golay A, Laurent-Jaccard A, Habicht F, et al. Effect of orlistat in obese patients with binge eating disorder. Obes Res. 2005;13(10):1701–1708. doi: 10.1038/oby.2005.208. [DOI] [PubMed] [Google Scholar]
- 104.Appolinario JC, Bacaltchuk J, Sichieri R, et al. A randomized, double-blind, placebo-controlled study of sibutramine in the treatment of binge-eating disorder. Arch Gen Psychiatry. 2003;60(11):1109–1116. doi: 10.1001/archpsyc.60.11.1109. [DOI] [PubMed] [Google Scholar]
- 105.James WP, Caterson ID, Coutinho W, et al. SCOUT Investigators. Effect of sibutramine on cardiovascular outcomes in overweight and obese subjects. N Engl J Med. 2010;363(10):905–917. doi: 10.1056/NEJMoa1003114. [DOI] [PubMed] [Google Scholar]


