Abstract
Objective
To investigate the distribution of antibiotic prescriptions in primary health care among children aged 0–6 years and its association with socioeconomic factors.
Design
A cross-sectional study describing antibiotic prescriptions and socioeconomic factors, using different population-based registers from Statistics Denmark.
Setting
Antibiotic prescriptions in 2012 from primary health care in the Capital Region of Denmark.
Subjects
The population of children aged 0–6 years (n = 139,398) in the Capital Region of Denmark.
Main outcome measures
High use of antibiotics identified by number of antibiotic prescriptions (≥ 3 prescriptions per year) and defined daily doses (DDD). A multinomial logistic regression analysis estimating the association between high antibiotic use and parents’ education, employment status, income, child’s sex, and ethnic background.
Results
Ten percent of children accounted for 25% of the total use DDD. There was a clear tendency that the risk for high antibiotic use increased as parental educational level decreased. The risk for high use was the highest among children of mothers and fathers with basic schooling ≤10 years (OR 1.60, 95% CI 1.29–1.98, and OR 1.60, 95% CI 1.34–1.91, respectively). Low income and unemployment were not associated with high antibiotic use.
Conclusion
Socioeconomic factors can only partially explain differences in antibiotic use. Further research is needed to clarify the unequal distribution of antibiotic prescribing and the association between high antibiotic use and low educational level. This would provide valuable information in the planning of strategies to promote rational use of antibiotics among children.
Key Points
The Capital Region of Denmark has the highest rate of antibiotic prescribing in Denmark.
Preschool children are among the age groups with the highest use.
Ten percent of the children accounted for 25% of the total antibiotic use.
Low parental educational level was associated with increased antibiotic use.
Parents’ income or employment status was not found to be associated with high antibiotic use.
Keywords: Antibiotics, children, Denmark, general practice, infection, primary health care
Introduction
According to WHO, one of the most serious public health problems is the rapidly increasing occurrence of resistant bacteria worldwide.[1] Antimicrobial resistance is directly related to the use of antibiotics.[2] Most antibiotics are prescribed for respiratory tract infections,[3] but the majority of respiratory infections are caused by virus. Accordingly, antibiotics have no beneficial effect and may lead to harmful adverse reactions [4] and therefore, a more appropriate level of antibiotic prescribing is needed.[5] In Denmark, 90% of all antibiotics are prescribed in primary care,[6] and the highest rate of antibiotic prescribing is observed in the Capital Region.[7]
In Denmark and in most countries infants and preschool children are among the age group with highest use.[7–9] The majority (about 70%) of antibiotics prescribed to preschool children are for respiratory tract infections.[10]
Socioeconomic factors have been shown to have an impact on antibiotic prescribing patterns among children.[11–15] However, the literature is scarce and lacks large studies based on data at an individual level. Moreover, the results are inconclusive, as employment status, income, and educational level have been found to be related to both high and low antibiotic use among children.[11–18]
To reduce inappropriate antibiotic prescribing among preschool children, it is important to get more knowledge about the distribution of antibiotics and the socioeconomic mechanisms that could influence the antibiotic prescribing pattern. Therefore, this study aims to investigate whether there is an equal distribution of antibiotic use among children aged 0–6 years and to what extent parents’ socioeconomic factors are associated with high use of antibiotics in the Capital Region of Denmark.
Material and methods
Setting
The study was a population-based retrospective register-based study combining data from Statistics Denmark and the Danish National Prescription Database.
The study population was children aged 0–6 years old living in the Capital Region in 2012. The Capital Region is one of five regions in Denmark and consists of 29 municipalities with 1 749,405 inhabitants (1 January 2014) corresponding to 31% of the entire Danish population. All children born between 2006 and 2012 were included in the study (n = 139,398). Children aged 0 years were born during the study period year 2012.
Data and variables
Population and socioeconomic statistics were obtained from Statistics Denmark. Information on antibiotic prescriptions in 2012 was extracted from the Danish National Prescription Database, which contains complete information on prescriptions according to the Anatomical Therapeutic Chemical Classification System (ATC).[19]
From Statistics Denmark’s register on population and education, information on socioeconomic factors of the parents was obtained regarding income, education, and employment status; and information regarding the ethnic background of the children. The rate of antibiotic prescribing for children aged 0–6 years was extracted from the Danish National Prescription Database. This register contains complete information on all prescriptions redeemed in Denmark at outpatient pharmacies and has a high validity.[20]
Variables
Outcome variable: The study applied two measures of antibiotic use: number of prescriptions issued per year and defined daily doses (DDD). Antibiotic use by number of prescriptions was divided into three groups depending on the number of prescriptions: 0 prescription (low use), 1–2 prescriptions (median use) or ≥3 prescriptions (high use). All prescriptions were identified through the National Health Service and linked to the child population. In Denmark, antibiotics are purchased on prescription only and only sold through pharmacies, which have the exclusive rights to sell prescription-only medicine to consumers.
Covariates: Education: mothers’ and fathers’ highest completed educational level was obtained and divided into eight groups in ascending order in relation to number of years of education: basic schooling, secondary education, vocational education, short higher education, medium higher education, graduate, longer higher education, and researcher (reference group). In Denmark, it is mandatory to receive education corresponding to the basic school curriculum until the 10th year of school education. Secondary education or vocational education is normally after basic schooling and may be followed by further or higher education. Employment status was obtained for the mother and father and divided into four groups: self-employed (reference group), employee, unemployed, and others. The group “others” consists of parents assisting spouses, students, or those on leave.
Income was defined by the total household income in Danish kroner (DKK) and divided into five groups: ≤ 299,999; 300,000–499,999; 500,000–799,999; 800,000–999,999; and ≥1,000,000–(reference group). Here, one Euro corresponds to DKK 7.44.
Ethnic background was divided into three groups and defined as children with a Danish background (Danish), and Danish-born children with one or both parents born in a country other than Denmark (descendants), and children born in a country other than Denmark (immigrants) (reference group).
Statistics
Statistical analyses were done using SAS 9.3. A Lorenz curve was used to describe the unequal distribution of antibiotic use among children. The Lorenz curve has been applied to the use of medicines to highlight the unequal distribution of drugs in the population,[21] and recently also in a study of antibiotic consumption.[22] In the Lorenz curve, the x-axis represents the accumulated percentage of drug users and the y-axis the accumulated percentage of the total consumption DDD per year. In this study, we included the number of prescriptions in the Lorenz curve as a proxy for the number of treatment episodes per year. This modification was proposed as a supplement by Malo et al.[22] The selected socioeconomic variables (independent variables) were categorized and examined for their associations with antibiotic use. A multinomial logistic regression analysis was conducted to estimate the association between socioeconomic factors and number of antibiotic prescriptions in 2012.
Firstly, each independent variable was analyzed separately in univariate analyses, and we analyzed potential associations with antibiotic exposure. Secondly, an analysis including all the independent variables was done in a multivariate analysis in order to estimate the adjusted odds ratios.
Results
The average number of prescriptions per 1000 children aged 0–6 years was 739 per year. Of all children aged 0–6 years in the Capital Region, 34.4% had received at least one antibiotic prescription in 2012. Among the children exposed to antibiotics, 56% had received one prescription, 24% two, and 10% three or more (results not shown). The highest rate of antibiotic use was found in one-year-olds, of whom 54% were prescribed at least one antibiotic in 2012. The prescription rate declined with increasing age and among children aged 6 years, the prescription rate was 26.1% (Figure 1).
Figure 1.
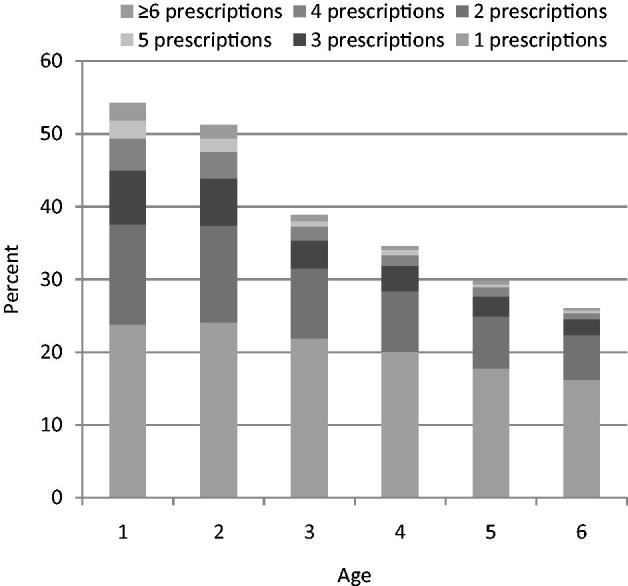
Number of prescriptions redeemed per child by age.
Figure 2 shows the distribution of antibiotic use in the different age groups by the two measures applied among children with ≥3 prescriptions. The prescription rate declined with increasing age – from 4.1 prescriptions on average among 1-year-olds to 3.7 prescriptions on average among 6-year-olds. DDD increased – as expected – with increasing age – from children aged 1 year (16.3 DDD) to children aged 6 years (17.5 DDD). Results on high antibiotic use among children may depend on if the outcome measure is prescriptions or DDD.
Figure 2.
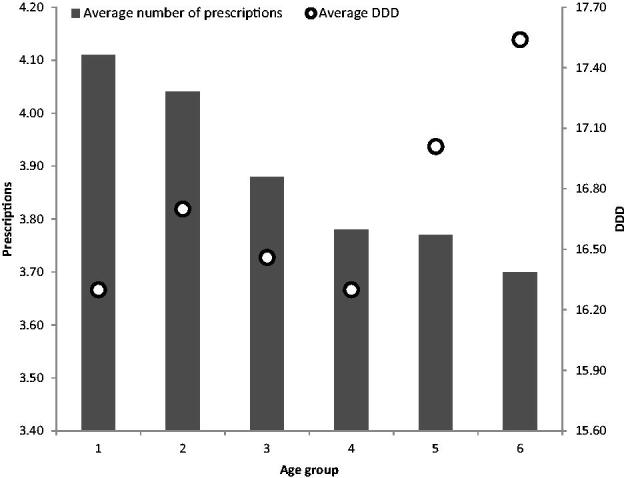
Average number of prescriptions and average of DDD among children with ≥ 3 prescriptions.
The results in this study demonstrate an unequal use of antibiotics. Approximately 10% of the children accounted for about 25% of the total antibiotic use. High antibiotic use, defined as having ≥3 prescriptions per year, corresponding to 20% of the children, accounted for 41% of the total antibiotic use (Figure 3).
Figure 3.
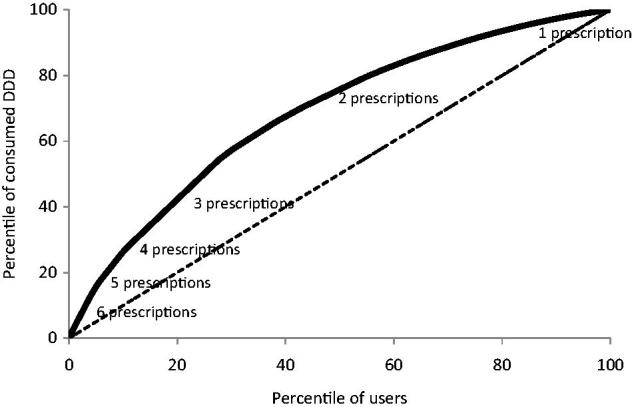
Lorenz curve of antibiotic use.
Table 1 shows the distribution of socioeconomic factors according to antibiotic use in 2012. High use of antibiotics (≥ 3 prescriptions per year) varied significantly in each socioeconomic category (all p values <0.01). The results were verified when multinomial regression analyses were later done.
Table 1.
Socioeconomic factors by number of antibiotic prescriptions among children aged 0–6 years old in the Capital Region 2012.
| Overall number(n = 139,398) | Low use (no prescriptions)n = 90,046 | High use (≥ 3 prescription)n = 107,43 | |
|---|---|---|---|
| Gender | |||
| Girl | 71,590 | 63.8 | 8.3 |
| Boy | 67,808 | 65.5 | 7.1 |
| Mother’s employment status | |||
| Independent | 4030 | 68.9 | 6.1 |
| Employee | 102,009 | 64.7 | 7.7 |
| Unemployed | 18,086 | 61.5 | 9.2 |
| Others | 15,273 | 66.8 | 6.5 |
| Father’s employment status | |||
| Independent | 9885 | 65.5 | 6.9 |
| Employee | 105,053 | 64.6 | 7.8 |
| Unemployed | 9497 | 62.3 | 8.6 |
| Others | 14,934 | 65.6 | 7.3 |
| Missing | 29 | – | – |
| Household income | |||
| <299,999 | 9932 | 66.8 | 6.8 |
| 300,000–499,999 | 24,150 | 62.8 | 8.6 |
| 500,000–799,999 | 52,326 | 63.0 | 8.2 |
| 800,000–999,999 | 25,418 | 65.7 | 7.3 |
| >1,000,000 | 27,572 | 67.3 | 6.6 |
| Mother’s highest completed education | |||
| Basic schooling (≤ 10 years) | 16,474 | 60.1 | 9.9 |
| Secondary education (11–13 years) | 7948 | 64.5 | 7.3 |
| Vocational education (10.5–15.5 years) | 27,872 | 61.1 | 9.1 |
| Short higher education (13–16 years) | 6987 | 64.0 | 8.1 |
| Medium higher education (14–17.5 years) | 29,183 | 64.3 | 7.7 |
| Graduate (14–17 years) | 5681 | 67.6 | 6.4 |
| Long higher education (16–19 years) | 32,390 | 68.6 | 6.0 |
| Researcher education (18.5–22 years) | 1905 | 69.5 | 6.0 |
| Others | 2111 | 66.0 | 7.0 |
| Missing | 8847 | – | – |
| Father’s highest completed education | |||
| Basic schooling (≤ 10 years) | 19,117 | 60.6 | 9.3 |
| Secondary education (11–13 years) | 8382 | 64.8 | 7.3 |
| Vocational education (10.5–15.5 years) | 35,700 | 61.6 | 8.9 |
| Short higher education (13–16 years) | 9200 | 64.1 | 7.5 |
| Medium higher education (14–17.5 years) | 17,198 | 65.9 | 6.9 |
| Graduate (14–17 years) | 31,131 | 68.9 | 6.5 |
| Long higher education (16–19 years) | 4405 | 67.8 | 5.8 |
| Researcher education (18.5–22 years) | 3086 | 71.5 | 5.2 |
| Others | 2986 | 64.1 | 8.8 |
| Missing | 8193 | – | – |
| Ethical background | |||
| Danish | 121,163 | 65,0 | 7.6 |
| Immigrant | 2278 | 73.2 | 3.9 |
| Descendant | 15,957 | 61.1 | 9.0 |
The crude odds ratios for high antibiotic use in the univariate analysis are shown in Table 2 (results for medium use are not shown). Results from the adjusted model show that high use was more pronounced among boys than among girls (20%, 95% CI 1.15–1.25). Children with unemployed mothers and employed mothers, respectively, had the highest risk for high antibiotic use (41%, 95% CI 1.21–1.64 and 33%, 95% CI 1.16–1.54) compared with children with self-employed mothers. The employment status of the father did not follow the same pattern as that of the mother. Children of unemployed fathers did not have a significantly higher risk for high antibiotic use compared with children with self-employed fathers.
Table 2.
Associations between high antibiotic use (≥ 3 prescriptions) and socioeconomic factors.
| Unadjusted high use(≥3 prescriptions) OR (95% CI) | Adjusteda high use(≥3 prescriptions) OR (95% CI) | |
|---|---|---|
| Gender | ||
| Girl | – | – |
| Boy | 1.21 (1.16–1.26) | 1.20 (1.15–1.25) |
| Mother’s employment status | ||
| Independent | – | – |
| Employee | 1.34 (1.16–1.53) | 1.33 (1.16–1.54) |
| Unemployed | 1.70 (1.48–1.95) | 1.41 (1.21–1.64) |
| Others | 1.10 (0.95–1.27) | 1.18 (1.01–1.38) |
| Father’s employment status | ||
| Independent | – | – |
| Employee | 1.14 (1.05–1.24) | 1.18 (1.08–1.28) |
| Unemployed | 1.32 (1.18–1.47) | 1.05 (0.93–1.19) |
| Others | 1.05 (0.95–1.16) | 1.11 (1.00–1.24) |
| Household income | ||
| <299.999 | 1.04 (0.95–1.14) | 0.91 (0.80–1.04) |
| 300,000–499,999 | 1.40 (1.31–1.50) | 1.02 (0.93–1.12) |
| 500,000–799,999 | 1.32 (1.25–1.40) | 1.04 (0.98–1.11) |
| 800,000–999,999 | 1.13 (1.06–1.21) | 1.02 (0.95–1.10) |
| >1,000,000 | – | – |
| Mother’s highest completed education | ||
| Basic schooling (≤ 10 years) | 1.92 (1.57–2.34) | 1.60 (1.29–1.98) |
| Secondary education (11–13 years) | 1.30 (1.06–2.34) | 1.41 (1.10–1.83) |
| Vocational education (10.5–15.5 years) | 1.64 (1.28–2.10) | 1.46 (1.18–1.79) |
| Short higher education (13–16 years) | 1.47 (1.19–1.81) | 1.33 (1.06–1.65) |
| Medium higher education (14–17.5 years) | 1.39 (1.14–1.69) | 1.28 (1.04–1.57) |
| Graduate (14–17 years) | 1.10 (0.88–1.37) | 1.10 (0.87–1.38) |
| Long higher education (16–19 years) | 1.02 (0.84–1.24) | 1.01 (0.82–1.24) |
| Researcher education (18.5–22 years) | – | – |
| Father’s highest completed education | ||
| Basic schooling (≤ 10 years) | 2.11 (1.79–2.50) | 1.60 (1.34–1.91) |
| Secondary education (11–13 years) | 1.56 (1.30–1.87) | 1.58 (1.28–1.96) |
| Vocational education (10.5–15.5 years) | 1.89 (1.53–2.32) | 1.56 (1.31–1.86) |
| Short higher education (13–16 years) | 1.61 (1.35–1.93) | 1.37 (1.13–1.64) |
| Medium higher education (14–17.5 years) | 1.43 (1.21–1.70) | 1.25 (1.05–1.50) |
| Graduate (14–17 years) | 1.16 (0.94–1.42) | 1.08 (0.87–1.34) |
| Long higher education (16–19 years) | 1.32 (1.12–1.56) | 1.28 (1.08–1.52) |
| Researcher education (18.5–22 years) | – | – |
| Ethical background | ||
| Danish | 2.19 (1.77–2.72) | 2.91 (1.07–7.90) |
| Immigrant | – | – |
| Descendant | 2.77 (2.23–3.45) | 3.40 (1.25–9.25) |
Adjusted for gender, mothers’, and fathers’ employment and highest completed education, household income, ethical background.
The different categories of household income showed no significant association with high antibiotic use. Children who were descendants or with Danish background showed higher antibiotic use compared with immigrant children. .
The odds of high antibiotic use increased as mothers’ educational level decreased: there was a significantly higher risk for high use among children with mothers of all educational levels compared with children of mothers with researcher education, apart from graduate and longer higher education. The risk for high use was the highest for children of mothers with basic schooling only (60%, 95% CI 1.29–1.98) compared with children of mothers with researcher education. The odds of high antibiotic use also increased as father’s educational level decreased apart from graduate education. The risk was the highest among children of fathers with basic schooling only (60%, 95% CI 1.34–1.91). The pattern was almost the same for the mothers’ and the fathers’ education.
The results did not change when it was tested for the robustness of the categories (0, 1–2, ≥ 3 prescriptions) in a couple of sensitivity analyses. The first analysis (0, 1–2, 3–4, ≥5 prescriptions) showed a minimal increase in OR but with larger confidence intervals. The second analysis (0, 1, 2, ≥3 prescriptions) barely changed the OR.
Discussion
Statement of principal findings
Our findings showed that approximately one third of all preschool children in the Capital Region of Denmark received at least one antibiotic prescription in one year (2012). There was a considerable difference in the use of antibiotics as 10% used 25% of the total consumption. The average prescribing rate was 739 prescriptions per 1000 children per year. There was no association between household income and antibiotic prescribing. The odds ratios were significantly increased by having parents with low educational level.
Strengths and weaknesses of the study
The strength of this study is the full coverage of the entire population of children aged 0–6 years in the Capital Region of Denmark. Individual information about socioeconomic factors and antibiotic prescribing covering about one third of all preschool children in a country has only rarely been achieved by other studies, as most countries do not have access to link prescription data with other public registers. Antibiotics are available only on prescription in Denmark; accordingly, we could account for all users, apart from the small proportion of patients admitted to hospital.
To evaluate antibiotic prescribing, we calculated the number of prescriptions per year because we believe it reflects the number of episodes of infections. According to the European Centre for Disease Prevention, this is a more realistic way to evaluate antibiotic prescribing than the traditional measure calculated as number of DDD per 1000 inhabitants per day since dosing depends on a patient’s body weight.[23] The results of this study confirm that using DDD instead of number of prescriptions may underestimate antibiotic consumption among children aged 1–4 years. Overall, there were barely any differences in the Lorenz curve regarding whether number of prescriptions or DDD was used. Using DDD in the Lorenz curve showed that 27.1% of children accounted for 53.5% of the antibiotic use. When using prescriptions, the Lorenz curve showed 28.4% of children accounted for 53.6% of the antibiotic use. Both measures seem to be suitable for this age group. For study populations including both children and adults, Malo et al., 2014 recommend number of prescriptions to calculate the distribution in a Lorenz curve.[22]
The study is cross-sectional, which cannot lead to any conclusion on causality of high antibiotic use. Nevertheless, most socioeconomic factors have probably been established before the children’s antibiotic use. Due to the unique possibility of linking individual socioeconomic data to antibiotic prescriptions for a large group of children, only very, few international studies, mostly from Sweden, were available for comparison.
It is unknown whether high antibiotic use among children with lower educated parents is simply a picture of unequal distribution of infections in society. Studies about socioeconomic factors and infections are dominated by studies from developing countries. However, a few studies among British and US children have found that children from lower social classes are more at risk of infection,[24] but this has not been investigated in a Danish setting.
It was not possible to obtain data on indications for antibiotic prescribing. Knowing the reasons why antibiotics were prescribed to the child would allow a more valid evaluation of the appropriateness of the treatment. Another limitation of the present analysis is the absence of morbidity data and, hence, our inability to adjust for possible differences in morbidity in relation to antibiotic use. Finally, prescriptions may be affected by general practitioners’ prescription behavior, but the study lacks data on which children are seen by which general practitioners.
Findings in relation to other studies and interpretation
Compared with equivalent children in Sweden in 2012, there is a substantially higher prescription rate in Denmark – 57%. The average prescription rate in Sweden in 2012 was about 470 prescriptions per 1000 children, and the Swedish region Skaane, bordering the Capital Region of Denmark, had an antibiotic prescribing rate of about 550 prescriptions per 1000 children per year.[25] Despite the higher antibiotic use in Denmark among children compared with that in Sweden, prescription rates in Denmark are still among the lowest in Europe.[26]
Antibiotic prescribing was more frequent among boys than among girls, which is in accordance with a newly published Danish study on drug utilization.[7] This may partly be explained by the fact that acute otitis media is more frequent among young boys.[27]
A study by Hjern et al. (2000) showed no association between children who had consumed antibiotics at least once during the previous 12 months and unemployed parents.[15] Compared to the employment status independent, our study found that children with employed and unemployed mothers had a higher risk for increased antibiotic use, whereas children with unemployed fathers did not have an increased risk. It can be concluded that associations between employment status and antibiotic use is unclear and needs further research. This study found no association between household income and antibiotic prescribing, whereas other studies have found a significant association between antibiotic use and household income.[12,13,15,18]
The longer the education, the lower the odds ratios for high antibiotic use. That is more or less the picture of the results in this study. These results are in line with a Danish study from 2003 finding that children aged 0–2 years of mothers with low educational level had a slightly higher risk of high antibiotic use (> 4 antibiotic courses) during the first 2 years of life. Two Swedish studies did not find similar associations: Hjern et al. (2000) found that children aged 6–15 years consumed fewer antibiotics during the previous 12 months if their parents had low levels of education (less than 10 years);[15] Hedin et al. (2006) found no association between antibiotic treatment for 18-month-old children and parents’ education.[16] Although Denmark and Sweden are neighboring countries, there seems to be differences in antibiotic prescribing behavior.
This study found a higher risk of high antibiotic use among children who were descendants or with a Danish background compared with immigrant children. Immigrant children as well as their parents are not born in Denmark nor do they have Danish citizenship. It could therefore be hypothesized that immigrant children have parents who lack Danish language skills as well as knowledge about the Danish healthcare system. This might reduce contact to a general practitioner and thereby also reduce the risk of being exposed to antibiotics. Children who were descendants of immigrants had a higher odds ratio of high antibiotic use compared with children with a Danish background, but large confidence intervals influence the accuracy of the estimates. Other studies have found no such associations between ethnic background and antibiotic use.[15,16]
Meaning of the study: implications
We found that high antibiotic use is present to a greater degree among children with parents with low education. It could be hypothesized that parents with low educational level lack knowledge about the potentially harmful effects of antibiotics and this could interact with a higher risk for infections among children from lower social classes.[28] Future studies should investigate this. This background knowledge would help general practitioners cope with children at risk of high use.
Conclusion
Socioeconomic factors can only partially explain the differences in high use of antibiotics. Employment status and income were not associated with a high prescription rate. A positive relationship was found between parents’ educational level and prescription rate: the lower the number of years of education, the higher the prescription rate. Further research should clarify the unequal distribution of antibiotic prescribing and explain the association between high antibiotic use and low educational level. This would provide valuable information in the planning of strategies to promote rational use of antibiotics among children.
Ethics approval
No approval from the Ethics committee was needed according to Danish law.
Acknowledgments
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- 1.World Health Organization. Antimicrobial Resistance WHO Global Report on surveillance; France: WHO; Jun 2014. [Internet]. Available from: http://apps.who.int/iris/bitstream/10665/112642/1/9789241564748_eng.pdf. [Google Scholar]
- 2.Bell BG, Schellevis F, Stobberingh E, et al. A systematic review and meta-analysis of the effects of antibiotic consumption on antibiotic resistance . BMC Infect Dis. 2014;14:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Petersen I, Hayward AC.. Antibacterial prescribing in primary care . J Antimicrob Chemother. 2007;60:i43–i47. [DOI] [PubMed] [Google Scholar]
- 4.Smith SM, Fahey T, Smucny J, et al. Antibiotics for acute bronchitis. Cochrane Database Syst Rev. 2014;3:CD000245. [DOI] [PubMed] [Google Scholar]
- 5.Mölstad S. Reduction in antibiotic prescribing for respiratory tract infections is needed! Scand J Prim Health Care. 2003;21:196–198. [DOI] [PubMed] [Google Scholar]
- 6.Statens Serum Institut, National Veterinary Institute, Technical University of Denmark, National Food Institute, Technical University of Denmark. DANMAP 2011 - Use of antimicrobial agents and occurrence of antimicrobial resistance in bacteria from food in animals, food and humans in Denmark; Copenhagen; 2012. Report No.: 1600–2032 [Internet]. Available from: www.danmap.org [Google Scholar]
- 7.Pottegard A, Broe A, Aabenhus R, et al. Use of antibiotics in children: a Danish nationwide drug utilization study. Pediatr Infect Dis J. 2014;34:e16–e22. [DOI] [PubMed] [Google Scholar]
- 8.Huibers L, Moth G, Christensen MB, et al. Antibiotic prescribing patterns in out-of-hours primary care: a population-based descriptive study. Scand J Prim Health Care. 2014;32:200–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clavenna A, Bonati M.. Drug prescriptions to outpatient children: a review of the literature . Eur J Clin Pharmacol. 2009;65:749–755. [DOI] [PubMed] [Google Scholar]
- 10.Finkelstein JA, Metlay JP, Davis RL, et al. Antimicrobial use in defined populations of infants and young children. Arch Pediatr Adolesc Med. 2000;154:395–400. [DOI] [PubMed] [Google Scholar]
- 11.Nilsson P, Laurell MH. Impact of socioeconomic factors and antibiotic prescribing on penicillin- non-susceptible Streptococcus pneumoniae in the city of Malmö. Scand J Infect Dis. 2005;37:436–441. [DOI] [PubMed] [Google Scholar]
- 12.Kozyrskyj AL, Dahl ME, Chateau DG, et al. Evidence-based prescribing of antibiotics for children: role of socioeconomic status and physician characteristics. CMAJ. 2004;171:139–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thrane N, Olesen C, Schonheyder HC, et al. Socioeconomic factors and prescription of antibiotics in 0- to 2-year-old Danish children . J Antimicrob Chemother. 2003;51:683–689. [DOI] [PubMed] [Google Scholar]
- 14.Melander E, Nissen A, Henricson K, et al. Utilisation of antibiotics in young children: opposite relationships to adult educational levels in Danish and Swedish counties . Eur J Clin Pharmacol. 2003;59:331–335. [DOI] [PubMed] [Google Scholar]
- 15.Hjern A, Haglund B, Rasmussen F, et al. Socio-economic differences in daycare arrangements and use of medical care and antibiotics in Swedish preschool children. Acta Paediatr. 2000;89:1250–1256. [DOI] [PubMed] [Google Scholar]
- 16.Hedin K, Andre M, Hakansson A, et al. A population-based study of different antibiotic prescribing in different areas. Br J Gen Pract. 2006;56:680–685. [PMC free article] [PubMed] [Google Scholar]
- 17.Hjern A, Haglund B, Rosen M.. Socioeconomic differences in use of medical care and antibiotics among schoolchildren in Sweden. Eur J Public Health. 2001;11:280–283. [DOI] [PubMed] [Google Scholar]
- 18.Henricson K, Melander E, Molstad S, et al. Intra-urban variation of antibiotic utilization in children: influence of socio-economic factors . Eur J Clin Pharmacol. 1998;54:653–657. [DOI] [PubMed] [Google Scholar]
- 19.WHO: WHO Collaborating Centre for Drug Statistics Methodology , Guidelines for ATC classification and DDD assignment 2013. Oslo: 2012. WHO; 2012 [Internet]; [cited 2015 Nov 26]. Available from: http://www.whocc.no/filearchive/publications/1_2013guidelines.pdf. [Google Scholar]
- 20.Kildemoes HW, Sorensen HT, Hallas J.. The Danish National Prescription Registry. Scand J Public Health. 2011;39:38–41. [DOI] [PubMed] [Google Scholar]
- 21.Hallas J, Støvring H.. Templates for analysis of individual-level prescription data. Basic Clin Pharmacol Toxicol. 2006;98:260–265. [DOI] [PubMed] [Google Scholar]
- 22.Malo S, José Rabanaque M, Feja C, et al. High antibiotic consumption: a characterization of heavy users in Spain. Basic Clin Pharmacol Toxicol. 2014;115:231–236. [DOI] [PubMed] [Google Scholar]
- 23.European Centre for Disease Prevention Summary of the latest data on antibiotic consumption in the European Union. Stockholm; 2014. [Internet]. Available from: _http://ecdc.europa.eu/en/eaad/Documents/antibiotic-consumptio-ESAC-Net-2014-EAAD.pdf. [Google Scholar]
- 24.Cohen S. Social status and susceptibility to respiratory infections. Ann N Y Acad Sci. 1999;896:246–253. [DOI] [PubMed] [Google Scholar]
- 25.Folkhelsomyndigheten Antibiotikastatistik-kvartalsrapport 4 2013. Sverige: Folkhelsomyndigheten; 2014. [Internet]. Available from: http://www.folkhalsomyndigheten.se/documents/statistik-uppfoljning/antibiotikastatistik/kvartalsrapporter/2013-antibiotikastatistik-kvartalsrapporter/Antibiotikastatistik-kvartalsrapport-4-2013.pdf [Google Scholar]
- 26.Holstiege J, Schink T, Molokhia M, et al. Systemic antibiotic prescribing to paediatric outpatients in 5 European countries: a population-based cohort study. BMC Pediatr. 2014;14:174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Plasschaert AI, Rovers MM, Schilder AG, et al. Trends in doctor consultations, antibiotic prescription, and specialist referrals for otitis media in children: 1995–2003. Pediatrics. 2006;117:1879–1886. [DOI] [PubMed] [Google Scholar]
- 28.Finkelstein JA, Dutta-Linn M, Meyer R, et al. Childhood infections, antibiotics, and resistance: what are parents saying now? Clin Pediatr (Phila). 2014;53:145–150. [DOI] [PMC free article] [PubMed] [Google Scholar]


