Abstract
AIM
To evaluate use of palliative care services in patients with end-stage liver disease who do not have access to liver transplant.
METHODS
Evaluated were end-stage liver disease patients who were removed from the liver transplant wait-list or died prior to transplant at a single transplant center over a 2-year period. Those who were removed due to noncompliance or ultimately transplanted elsewhere were excluded from this study. Patient characteristics associated with palliative care consultation were assessed using logistic regression analysis.
RESULTS
Six hundred and eighty-three patients were listed for liver transplant in 2013-2014 with 107 (16%) dying (n = 62) or removed for clinical decompensation prior to liver transplant (n = 45): Median age was 58 years, and the majority were male (66%), Caucasian (53%), had Child C cirrhosis (61%) or hepatocellular carcinoma (52%). The palliative care team was consulted in only 18 of the 107 patients (17%) who died or were removed, 89% of which occurred as inpatients. Half of these consultations occurred within 72 h of death. In univariable analysis, patients of younger age, white race, and higher end-stage liver disease scores at time of listing and delisting were more likely to receive palliative care services. Only younger age [Odds ratio (OR) = 0.92; P = 0.02] and Caucasian race (OR = 4.90; P = 0.02) were still associated with integration of palliative care services through multivariable analysis.
CONCLUSION
Palliative care services are grossly underutilized in older, non-white patients with cirrhosis on the liver transplant wait-list. We encourage early integration of these services into clinical decision-making in the transplant population, with further studies aimed at understanding barriers to consultation.
Keywords: Cirrhosis, Hospice, End of life, Symptom management, Palliative care
Core tip: Without liver transplant, patients with cirrhosis have 50% mortality at 5 years; these patients represent a population that would benefit from palliative care services. Palliative care services are grossly underutilized in older, non-white patients with cirrhosis on the liver transplant wait-list. We encourage early integration of these services into clinical decision-making in the transplant population, with further studies aimed at understanding barriers to consultation.
INTRODUCTION
Decompensated cirrhosis is characterized by ascites, hepatic encephalopathy, and variceal bleeding. Mortality is high with 50% death rate due to complications of cirrhosis within five years[1,2]. In addition to these medical complications, patients with decompensated cirrhosis experience a large symptomatic burden including debilitating fatigue, muscle wasting, anorexia, and intractable pruritus. Self-reported quality of life is poor in cirrhotics; in one study, 38% of elderly patients with cirrhosis had difficulty in independently completing at least one daily living activity including dressing, walking few steps, or bathing while 10% had impaired integral activities of daily living (i.e., managing money, cooking, grocery shopping)[3-5]. Their physical symptoms, inability to independently care for themselves, and knowledge of their terminal disease often erodes their emotional and psychological well-being.
While it is clear that liver transplantation is essentially the only known cure for complications of end-stage liver disease, the ability to receive a transplant can be unpredictable: One in five individuals awaiting liver transplantation will die on the waitlist[6]. While the process of listing individuals for liver transplantation is highly structured through formal medical, surgical, social, and psychological evaluations, there is no standard of care for the process to transition those who are deemed too sick for liver transplantation to comfort care. We aimed to evaluate current utilization of palliative care services in liver transplant candidates who did not survive to liver transplant and understand which patient characteristics are associated with palliative care consultation in this population.
MATERIALS AND METHODS
All adult cirrhotic patients who were newly listed for liver transplant at a single, large volume United States liver transplant center from January 1, 2013 to December 31, 2014 and died prior to transplant or were delisted for being too ill for transplant were included in this study. We excluded patients delisted due to inadequate social support, medical non-adherence, active substance abuse, or those who were transplanted at another center.
Patient demographics (age, gender, ethnicity, language spoken), etiology of liver disease, Model for End-Stage Liver Disease (MELD) score at time of transplant listing, and education level were received from the United Network for Organ Sharing and Organ Procurement and Transplantation Network registries. Patients’ MELD at delisting or death, Child Pugh Score at time of removal, presence of hepatocellular cancer (HCC), and insurance type were collected through review of the electronic health record. Details on the palliative care consultations were also manually reviewed from the electronic medical records.
Descriptive statistics were computed for all continuous variables (age at listing, candidate MELD lab score when being listed for transplant) including means, medians, and interquartile ranges. The rank sum test was used for these continuous variables. Pearson’s χ2 testing was used for the categorical values (candidate gender, ethnicity, highest education level, and diagnosis) to further compare the baseline characteristics of patients removed from the waiting list vs those who remained active. We employed univariable logistic regression to identify factors associated with palliative care consultation with a P value cut-off of 0.10. These factors were then evaluated for inclusion in the final multivariable logistic regression model using backwards step-wise elimination, using a P value cut-off of 0.05.
This study was approved by the Institutional Review Board of UCSF. Stata, version 12 (Stata Corp., College Station, TX) was used for statistical analyses.
RESULTS
There were 683 patients placed on the liver transplant list in 2013-2014, of which 107 (16%) ultimately dying (n = 62) or removed for clinical decompensation prior to liver transplant (n = 45). Median age was 58 years and majority (66%) was male. Majority of the patients who died or were de-listed were white (53.3%), followed by Hispanic (22.4%), Asian (12.1%), Black (9.3%), and other (2.8%). The etiology of cirrhosis was alcohol (11%), hepatitis C (41%), alcohol and hepatitis C (20%), and various other etiologies (30%). Majority of these patients had Child-Pugh Class C cirrhosis (60.7%) while 52% of these patients had HCC. In terms of education level, 93.5% had a college degree or less (Table 1).
Table 1.
Baseline characteristics of 107 patients who died or were delisted for being too sick for transplant
| n = 107 | |
| Age at listing, yr | 58 (53-63) |
| Male sex | 71 (66%) |
| Ethnicity | |
| White | 57 (53.3%) |
| Hispanic | 24 (22.4%) |
| Asian | 13 (12.1%) |
| Black | 10 (9.3%) |
| Other | 3 (2.8%) |
| MELD at time of listing | 16 (12-23) |
| Etiology of cirrhosis | |
| Alcohol related | 12 (11%) |
| Hepatitis C | 44 (41%) |
| Alcohol + hepatitis C | 21 (20%) |
| Other | 30 (28%) |
| Child-pugh score at de-listing | |
| A | 16 (15%) |
| B | 26 (24.3%) |
| C | 65 (60.7%) |
| HCC | 56 (52%) |
| Education level | |
| College degree or less | 100 (93.5%) |
| Graduate level degree | 7 (6.5%) |
MELD: Model for end-stage liver disease; HCC: Hepatocellular cancer.
Of these 107 patients who were delisted or died while awaiting transplant, 18 (17%) received a palliative care consult in the 2-year period, of which 89% occurred as inpatients. The median number of days (interquartile range) from palliative care consultation to death was 4 (1-11) d; half of these consultations occurred within 72 h of death and 17% on the same day as death (Figure 1). Reasons for palliative care consultation included aiding in transitioning to hospice in 78% of patients, goals of care without transition to comfort care in 11%, and symptom management including refractory ascites, pruritus, and pain in the remaining 11%. Even from the 26 patients with ESLD who were delisted for advanced HCC, just 12% had palliative care consultation.
Figure 1.
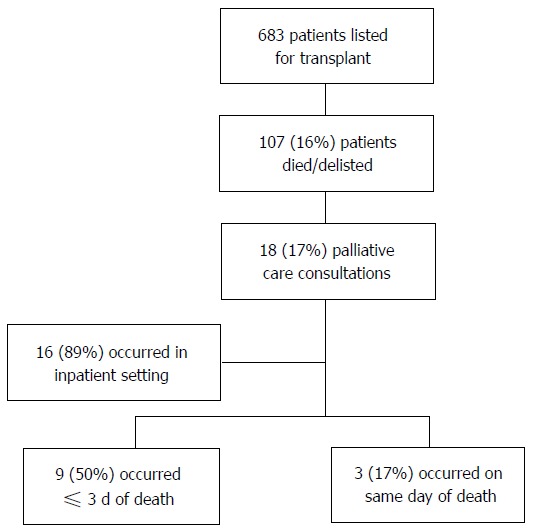
Palliative care consultations in patients who died or were delisted over a 24-mo period.
Patient characteristics associated with palliative care consultation in univariate analysis included younger age (OR = 0.92; P < 0.01), white race (OR = 3.74; P = 0.03), and higher MELD at listing (OR = 1.06; P = 0.02) and at delisting (OR = 1.05; P = 0.01). Subsequent multivariable analysis revealed only younger age (OR = 0.92; P = 0.02) and white race (OR = 4.90; P = 0.02) remained associated with utilization of palliative care services (Table 2).
Table 2.
Factors associated with palliative care consultation, univariable and multivariable logistic regression analysis
| Factor |
Univariable analysis |
Multivariable analysis |
||
| OR (95%CI) | P value | OR (95%CI) | P value | |
| Age, per year | 0.92 (0.87-0.98) | < 0.01 | 0.92 (0.87-0.98) | 0.02 |
| Male sex | 0.76 (0.27-2.16) | 0.61 | - | - |
| White race | 3.74 (1.14-12.26) | 0.03 | 4.90 (1.30-18.30) | 0.02 |
| MELD at listing | 1.06 (1.01-1.12) | 0.02 | 1.00 (0.97-1.10) | 0.39 |
| MELD at delisting | 1.05 (1.00-1.10) | 0.01 | 1.00 (0.97-1.10) | 0.34 |
| Etiology of liver disease | ||||
| Alcohol related | Reference | Reference | ||
| Hepatitis C | 0.95 (0.17-5.28) | 0.95 | - | - |
| Alcohol + hepatitis C | 1.56 (0.25-9.65) | 0.63 | ||
| Other | 0.77 (0.12-4.88) | 0.78 | ||
| Child-pugh score at delisting | ||||
| A | Reference | Reference | ||
| B | 0.60 (0.03-10.30) | 0.73 | - | - |
| C | 4.90 (0.60-40.10) | 0.14 | ||
| HCC | 0.89 (0.32-2.46) | 0.83 | - | - |
| College or lower level of education (vs graduate level) | 1.23 (0.14-10.9) | 0.85 | - | - |
| Private insurance (vs government) | 0.70 (0.25-1.97) | 0.50 | - | - |
| English language | 0.93 (0.24-3.65) | 0.92 | - | - |
MELD: Model for end-stage liver disease; HCC: Hepatocellular cancer.
DISCUSSION
According to the World Health Organization, palliative care “improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial, and spiritual”[7]. For patients with end-stage liver disease, early integration of palliative care into their routine medical care is particularly crucial to understanding patients’ preferences for the end of life, as progressive hepatic encephalopathy often leads to impaired decision-making. Those on the liver transplant list, however, represent a unique sub-group of patients with a “terminal” condition - by virtue of having end-stage liver disease - but await the promise of a cure through liver transplantation. In this setting, palliative care, which traditionally has been considered only for those “at the end of life”, may be perceived - by both the patient and providers alike - as unnecessary and unwelcome[8-11].
Indeed, we observed very low utilization of palliative care services among liver transplant candidates who ultimately died or were delisted for being too sick for liver transplant. Among the 17% of these patients who received palliative care services, half of the consultations occurred within 72 h of death and one in five occurred on the day of death, hardly enough time to develop rapport and aid both patients and their caregivers in the transition to supportive care at the end of life[12,13]. Importantly, we identified two factors - younger age and non-Hispanic white race - that were associated with palliative care consultation. This finding confirms a prior study evaluating barriers to palliative care among older adults that demonstrated that a terminal diagnosis in an elderly patient often is considered an “expectation” rather than a shock compared to that in a younger patient; it is also possible that younger patients at the end of life have more support networks/caretakers at this stage that advocate for improved quality of life[14,15]. Cultural and language barriers likely contribute to underutilization of palliative care services in the non-white population.
In addition, we find it interesting that more than three-fourths of palliative care consultations in our population were to assist with transition to comfort care and just 11% were for aid in symptom management. This depicts how transplant clinicians view palliative care, as a mode to help make patients comfortable at the end of life, but not to facilitate goals of care discussions or to help relieve pain and suffering in a patient population with a terminal condition without transplantation. We recognize the need for integration of palliative care and transplant hepatology teams in efforts to provide comprehensive care for our patients to meet their physical and psychosocial needs even when actively listed for liver transplantation.
We acknowledge that this study is limited by a relatively small sample size; however, it represents the entire eligible population at our liver transplant center during the study period, so is an unselected group. Another limitation is that we only evaluated those who died or were delisted rather than all patients on the liver transplant list. This was intentional, as we first wanted to evaluate the uptake of palliative care among those for whom death was certain.
Despite these limitations, this study represents one of the largest to date to evaluate palliative care consultation in the liver transplant population. Poonja et al[16] reported their experience in the liver transplant population at the University of Alberta and noted that of the 102 patients removed from the waitlist or declined over a 5 year period, only 10% were referred to palliative care despite high levels of pain, nausea, and depression. As patients with ESLD have high burden of symptoms, we advocate for increased utilization of palliative care services - for both symptom management and discussions regarding goals of care - and integration of such services early in the liver transplant listing process. Baumann et al[17] confirmed that early palliative care utilization in patients listed for transplantation led to improved symptom management and well-being in this population.
While this study represents a critical first step towards developing interdisciplinary programs directed at providing palliative care to liver transplant candidates, future studies should focus on understanding barriers to early integration of palliative care in the liver transplant population among all ages and ethnicities, in both the inpatient and outpatient setting. In addition, in a prospective study, patient-centered outcomes can be obtained in efforts to show the direct impact of palliative care involvement on the physical and psychosocial well being of these patients. Ultimately the goal should be to facilitate collaboration and, perhaps, even co-management between transplant and palliative care providers for the care of these complex patients - even when the intention to treat is curative - to improve the quality of care and quality of life for patients with cirrhosis awaiting liver transplantation.
COMMENTS
Background
Patients with end stage liver disease have 50% 5-year mortality due to complications of cirrhosis and experience a large symptomatic burden including debilitating fatigue, muscle wasting, anorexia, and intractable pruritus. While it is clear that liver transplantation is essentially the only known cure for complications of end-stage liver disease, the ability to receive a transplant can be unpredictable. In patients who do not have access to liver transplant, palliative care services may aid in quality of life of patients and caretakers alike.
Research frontiers
Though the process of listing individuals for liver transplantation is highly structured, there is no standard of care for the process to transition those who are deemed too sick for liver transplantation to comfort care. Current utilization of palliative care services in liver transplant candidates who did not survive to liver transplant is not largely understood.
Innovations and breakthroughs
Authors aimed to understand the use of palliative care services in patients with end-stage liver disease who do not have access to liver transplant over a 2-year period and a large volume center. Palliative care services were consulted in less than 20% of patients who were died or removed from the transplant list, majority of which occurred while patients were already hospitalized. In univariable analysis, patients of younger age, white race, and higher model for end-stage liver disease (MELD) scores at time of listing and delisting were more likely to receive palliative care services. Only younger age and Caucasian race were still associated with integration of palliative care services through multivariable analysis. The authors recognize that palliative care services are grossly underutilized in patients who are not deemed transplant candidates.
Applications
While this study represents a critical first step towards developing interdisciplinary programs directed at providing palliative care to liver transplant candidates, future studies should focus on understanding barriers to early integration of palliative care in the liver transplant population. In addition, in a prospective study, patient-centered outcomes can be obtained to show the direct impact of palliative care involvement on the physical and psychosocial well being of these patients. Ultimately the goal should be to facilitate collaboration and, perhaps, even co-management between transplant and palliative care providers for the care of these complex patients - even when the intention to treat is curative - to improve the quality of care and quality of life for patients with cirrhosis awaiting liver transplantation.
Terminology
Palliative care services encompass more than aiding in transitioning to comfort care and assisting in goals of care discussions, and can be particularly helpful in symptom management, even in patients who are not terminally ill. The laboratory based MELD score accounts for patients’ bilirubin, international normalized ratio (INR), and creatinine levels and was calculated both at time of transplant listing and delisting. The child pugh score entails a combination of laboratory (bilirubin, albumin, INR) and clinical (presence of ascites, encephalopathy) factors; though it was originally used to predict mortality in cirrhotics at the time of surgery, if can also aid in understanding the severity of liver disease.
Peer-review
This is an integral single center retrospective study that aims to shed light on the need for integration of palliative care into the liver transplant population, even when the intent to treat is curative, in efforts to improve their quality of life.
Footnotes
Institutional review board statement: This study was reviewed and approved by the UCSF Institutional Review Board.
Informed consent statement: This study was reviewed and approved by the UCSF Institutional Review Board.
Conflict-of-interest statement: There are no disclosures or conflicts-of-interest involving any of the study authors.
Manuscript source: Unsolicited manuscript
Specialty type: Transplantation
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
Peer-review started: March 23, 2016
First decision: May 13, 2016
Article in press: July 18, 2016
P- Reviewer: Marino IR, Srivastava M S- Editor: Qiu S L- Editor: A E- Editor: Wu HL
References
- 1.Fattovich G, Giustina G, Degos F, Tremolada F, Diodati G, Almasio P, Nevens F, Solinas A, Mura D, Brouwer JT, et al. Morbidity and mortality in compensated cirrhosis type C: a retrospective follow-up study of 384 patients. Gastroenterology. 1997;112:463–472. doi: 10.1053/gast.1997.v112.pm9024300. [DOI] [PubMed] [Google Scholar]
- 2.Lim YS, Kim WR. The global impact of hepatic fibrosis and end-stage liver disease. Clin Liver Dis. 2008;12:733–746, vii. doi: 10.1016/j.cld.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 3.Valery PC, Powell E, Moses N, Volk ML, McPhail SM, Clark PJ, Martin J. Systematic review: unmet supportive care needs in people diagnosed with chronic liver disease. BMJ Open. 2015;5:e007451. doi: 10.1136/bmjopen-2014-007451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rakoski MO, McCammon RJ, Piette JD, Iwashyna TJ, Marrero JA, Lok AS, Langa KM, Volk ML. Burden of cirrhosis on older Americans and their families: analysis of the health and retirement study. Hepatology. 2012;55:184–191. doi: 10.1002/hep.24616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rakoski M, Volk M. Palliative Care for Patients with End-Stage Liver Disease: An Overview. Clinical Liver Disease. 2015;6:19–21. doi: 10.1002/cld.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim WR, Lake JR, Smith JM, Skeans MA, Schladt DP, Edwards EB, Harper AM, Wainright JL, Snyder JJ, Israni AK, et al. OPTN/SRTR 2013 Annual Data Report: liver. Am J Transplant. 2015;15 Suppl 2:1–28. doi: 10.1111/ajt.13197. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. WHO Definition of Palliative Care, 2015. Available from: http://www.who.int/cancer/palliative/definition/en/
- 8.Walling AM, Schreibeis-Baum H, Pimstone N, Asch SM, Robinson L, Korlekar S, Lorenz K, Nwajuaku T, Rosenfeld K. Proactive case finding to improve concurrently curative and palliative care in patients with end-stage liver disease. J Palliat Med. 2015;18:378–381. doi: 10.1089/jpm.2014.0265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Walling AM, Asch SM, Lorenz KA, Wenger NS. Impact of consideration of transplantation on end-of-life care for patients during a terminal hospitalization. Transplantation. 2013;95:641–646. doi: 10.1097/TP.0b013e318277f238. [DOI] [PubMed] [Google Scholar]
- 10.Chochinov HM. Dignity-conserving care--a new model for palliative care: helping the patient feel valued. JAMA. 2002;287:2253–2260. doi: 10.1001/jama.287.17.2253. [DOI] [PubMed] [Google Scholar]
- 11.Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, McIntyre L, Tulsky JA. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA. 2000;284:2476–2482. doi: 10.1001/jama.284.19.2476. [DOI] [PubMed] [Google Scholar]
- 12.QOPI 2015 QCDR Measures. American Society of Clinical Oncology, the Quality Oncology Practice Initiative, 2015. Available from: http://www.instituteforquality.org/sites/instituteforquality.org/files/QOPI%202015%20QCDR%20Measures%20-%20Narrative_0.pdf.
- 13.Morrison RS, Penrod JD, Cassel JB, Caust-Ellenbogen M, Litke A, Spragens L, Meier DE. Cost savings associated with US hospital palliative care consultation programs. Arch Intern Med. 2008;168:1783–1790. doi: 10.1001/archinte.168.16.1783. [DOI] [PubMed] [Google Scholar]
- 14.Gardiner C, Cobb M, Gott M, Ingleton C. Barriers to providing palliative care for older people in acute hospitals. Age Ageing. 2011;40:233–238. doi: 10.1093/ageing/afq172. [DOI] [PubMed] [Google Scholar]
- 15.Hansen L, Press N, Rosenkranz SJ, Baggs JG, Kendall J, Kerber A, Williamson A, Chesnutt MS. Life-sustaining treatment decisions in the ICU for patients with ESLD: a prospective investigation. Res Nurs Health. 2012;35:518–532. doi: 10.1002/nur.21488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Poonja Z, Brisebois A, van Zanten SV, Tandon P, Meeberg G, Karvellas CJ. Patients with cirrhosis and denied liver transplants rarely receive adequate palliative care or appropriate management. Clin Gastroenterol Hepatol. 2014;12:692–698. doi: 10.1016/j.cgh.2013.08.027. [DOI] [PubMed] [Google Scholar]
- 17.Baumann AJ, Wheeler DS, James M, Turner R, Siegel A, Navarro VJ. Benefit of Early Palliative Care Intervention in End-Stage Liver Disease Patients Awaiting Liver Transplantation. J Pain Symptom Manage. 2015;50:882–6.e2. doi: 10.1016/j.jpainsymman.2015.07.014. [DOI] [PubMed] [Google Scholar]


