Abstract
It has been repeatedly shown that clozapine is more efficacious than other antipsychotics in the management of treatment-resistant schizophrenia. However, clozapine is associated with a number of side effects including weight gain. Antipsychotic-induced weight gain has been linked with a number of untoward events including psychological factors such as stigma and low self-esteem, and physical factors such as metabolic syndromes and untimely death. The mechanism underlying antipsychotic (including clozapine)-induced weight gain is not clearly understood, although it is said to involve several brain areas, several neurotransmitters, neuropeptides and genetic factors. To some individuals however, clozapine use is associated with significant weight loss (13.5–50% of body weight). The observed weight loss in these groups of patients has not been attributed to any underlying diagnosable physical disorders. There have been a handful cases published with this phenomenon, which seems to be contrary to what is expected when clozapine is prescribed. From the currently published cases three groups emerge – those who lost weight simply by taking clozapine, those who lost weight due to improved mental state, engaging in diet and increased exercise, and those for whom weight loss was a sign of a poor response to clozapine. A case of JX who has a diagnosis of schizoaffective disorder is presented. JX lost over 26% of her body weight when she was prescribed clozapine. A detailed review of other published cases is undertaken. The underlying mechanisms involving weight loss are discussed and the implications to clinicians are highlighted. Coordinated studies to examine these groups of patients may provide some insight, not only in the mechanism of clozapine-induced weight loss, but also in the better management of patients with treatment-resistant schizophrenia involving clozapine use.
Keywords: clozapine, treatment-resistant schizophrenia, weight loss
Introduction
Schizophrenia is a chronic debilitating illness with a lifetime prevalence of 0.3–0.66 % [McGrath et al. 2008]. It is estimated that between 20% and 30% of patients with schizophrenia have treatment-resistant illness [Lieberman et al. 2005; Conley and Buchanan, 1997]. Clozapine is the only antipsychotic drug that has been repeatedly shown to be effective in the treatment of treatment-resistant schizophrenia (TRS) [Kane et al. 1988; Lewis et al. 2006; Wahlbeck et al. 1999]. It is estimated that up to 30% of patients with TRS would respond to clozapine in short-term treatment. However, this can increase up to 60% if the treatment period is over 6 months [Kane et al. 1988; Meltzer 1989].
Weight gain is one of the common problems associated with antipsychotic medications. It is estimated that up to a third of those who are started on clozapine are already obese and that women may be more vulnerable [Covell et al. 2004]. A meta-analysis on the metabolic effects of antipsychotics by Rummel-Kluge and colleagues showed that clozapine and olanzapine caused more weight gain than other antipsychotics with rapid weight gain in the first few weeks that plateaued around 42–46 months for clozapine [Rummel-Kluge et al. 2010].
Though clozapine is commonly associated with weight gain, a small number of patients lose weight following its use. Other noted benefits include cognitive improvement. A case is presented where significant weight loss and cognitive improvement followed clozapine use. A summary of previous reported cases is presented and a detailed review of the possible underlying mechanisms is discussed.
Case history
JX is a 51-year-old Afro-Caribbean woman with a diagnosis of schizoaffective disorder from her mid-20s. She has had several lengthy hospital admissions in the past. JX remained in a hospital setting continuously for 5 years. She has had trials of several antipsychotics both first-generation and second-generation including long-acting injections with limited success. She had a trial of clozapine for a few weeks in September 2011, however, it was stopped due to a reluctance to having physical monitoring and blood tests.
JX had no marked negative symptoms of schizophrenia such as social withdrawal, lack of interest, poor social drive or blunting of affect. She related well to staff and her peers. However, JX had positive psychotic symptoms that were resistant to treatment. She experienced a number of psychotic symptoms including delusional beliefs, some somatic symptoms, where she felt someone jumping on her, and auditory hallucinations. JX believed that she had a lover living in her bedroom and would take food in there to feed the imagined man. Left alone she would accumulate food, which would rot in her room. JX heard many voices including the voice of a woman who wanted food from her during meal times. JX believed at times that the woman she heard resided in her body and would eat the food she ate leaving her with faeces. Other times JX felt that she was being strangled or choked by the woman during meal times to stop her from eating. JX talked passionately and openly about her experiences and expressed her disgust about the woman whom she described as being greedy. In the early part of her illness, JX would stop eating for a few days at times as a way of punishing the imagined woman. However, there was no time in her history prior to clozapine use where weight loss was a matter of concern. Despite having these psychotic symptoms over the years, JX ate normally and there were no concerns of her losing significant weight or restricting her diet intake for a prolonged period of time.
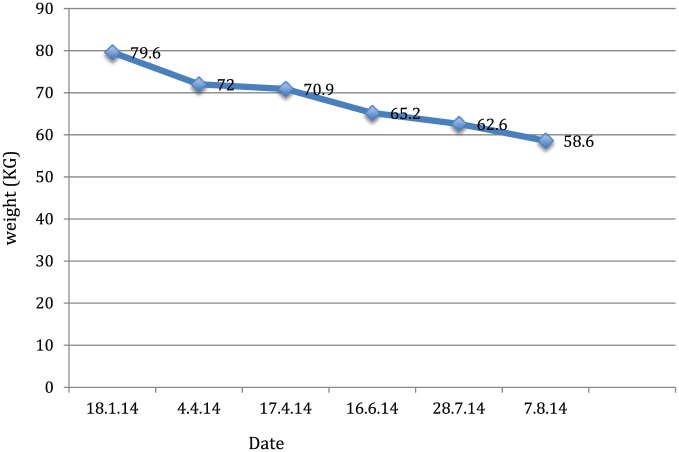
JX was started on clozapine in March 2014. At the start of treatment, JX weighed 79.6 kg, height 158 cm, with a body mass index (BMI) of 31.84. Despite receiving a good dose of clozapine (500 mg, clozapine serum level 581 µg/L, norclozapine 307 µg/L), JX continued to experience positive psychotic symptoms and started to restrict her diet intake. Her weight dropped gradually over the following several months (see Figure 1). Her BMI dropped from 31.8 to 23.4. She lost over 26% of her body weight following the commencement of clozapine. Her weight loss was not attributable to a diagnosable physical illness. Her physical evaluations, including blood tests, were all within normal limits.
Figure 1.
Weight loss chart.
Discussion
There have been a handful of cases reported in peer-reviewed journals where significant weight loss followed clozapine use (Table 1). The explanation given as to the cause of weight loss varied between cases. In three cases [Lally and McDonald, 2011; Appiani et al, 2011; Webster and Ingram, 2013], weight loss was as a result of improved mental state, better side-effect management and engagement in diet and exercise. In the three cases reported by Hanwella and colleagues, weight loss was attributable purely to taking clozapine [Hanwella et al. 2010]. The authors proposed that there might be some underlying genetic cause to the observed changes. Thomas and colleagues however, noted that weight loss early on following clozapine use was associated with a poor response to treatment [Thomas et al. 2009]. JX’s response to clozapine follows the pattern observed by Thomas and colleagues [Thomas et al. 2009].
Table 1.
Demographic characteristics and reasons for weight loss.
| Author | Sex | Age | Length of illness (years) | Diagnosis | Length of follow up (years) | Initial weight (kg) (BMI) | Weight at end (kg) (BMI) | Weight lost (kg) (%) | Dietary changes | Reason attributed to weight loss | Response to clozapine | Clozapine dose |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Thomas et al. 2009 | F | 34 | 10 | Schizophrenia | – | – | – | 8 kg | – | Sign of poor response | Partial/poor | 400 mg |
| M | 36 | 5 | Schizophrenia | – | – | – | 6 kg | – | Sign of poor response | Partial/poor | 400 mg | |
| F | 32 | 10 | Schizophrenia | – | – | – | 13 kg | – | Sign of poor response | Partial/poor | 500 mg | |
| M | 35 | – | Schizophrenia | – | – | – | 10 kg | – | Sign of poor response | Partial/poor | 500 mg | |
| M | 46 | 24 | Schizophrenia | – | – | – | 4 kg | – | Sign of poor response | Partial/poor | 500 mg | |
| Hanwella et al. 2010 | F | 34 | 20 | Schizophrenia | 3 years | 67 | 34 | 33 kg (49.3%) | None | Clozapine and genetic? | Good | 800 mg |
| M | 41 | 15 | Schizophrenia | 18 weeks | 98 | 80 | 18 kg (18.4%) | None | Clozapine and genetic? | Good | 400 mg | |
| F | 33 | 7 | Schizophrenia | 21 weeks | 66.4 | 52 | 14.4 kg (21.7%) | None | Clozapine and genetic? | Good | 450 mg | |
| Lally and McDonald, 2011 | M | 44 | 20 | Schizophrenia | 3 years | 127 kg (41.5%) | 76 kg (24.8%) | 51 kg (40%) | YES | Improved psychotic symptoms. Motivated to engage in diet and exercise | Good | 500 mg |
| Appiani et al. 2011 | – | 32 | ? | Schizophrenia | 1 year | 104 kg | 90 kg | 14 kg (13.5%) | YES | Improved negative symptoms. Motivated to engage in diet and exercise |
Good | 300 mg |
| Webster and Ingram, 2013 | – | 56 | Schizophrenia | 6 months | 93 | 63 | 30 kg (32.1%) | Better management of side effects | Good | 300 mg | ||
| Tungaraza 2015 (present study) | F | 51 | 20 | Schizoaffective | 7 months | 79.6 kg (31.8%) | 58.6kg (23.4%) | 21 kg (26.4%) | YES | Poor response and diet restriction due to psychotic beliefs | Partial /poor | 500 mg |
From the cases published so far it can be seen that as far as weight loss is concerned, three groups emerge. Those who lose weight simply by taking clozapine, those who lose weight by engaging in diet and increased physical activities, and those in whom weight loss indicated poor or partial response to clozapine. A large case-controlled study coupled with genetic evaluation is needed to provide clarity on these observations.
The case of JX and the observation by Thomas and colleagues suggests that for some patients with TRS, weight loss following clozapine use indicates poor response to treatment [Thomas et al. 2009]. It is of interest to note that a number of studies in the past have associated weight gain and a good response to clozapine [Stanton, 1995; Czobor et al. 2002]. It was thought that weight gain was due to an increase in triglycerides, which has been shown to predict good response to clozapine, with poor responders having low triglyceride changes [Procyshyn et al. 2007]. A study by Hermes and colleagues confirmed the association of weight gain and good response to antipsychotics, however, no association with increased triglycerides was observed [Hermes et al. 2011]. Is weight gain an unavoidable consequence of getting better on clozapine? The significance of this remains unsolved.
In the case of JX, the use of clozapine was associated with other benefits including cognitive functions. Clozapine and other atypical antipsychotics have been shown to improve cognitive functions in schizophrenia independent of psychotic symptoms in areas of attention, verbal fluency, working memory, speed of processing, conceptual organization and general intelligence [Meltzer and McGurk, 1999; Weickert et al. 2003]. The use of clozapine has been associated with over 0.5 standard deviation improvements in letter fluency that predicted employment outcome [Sumiyoshi et al. 2013]. It is of interest to note that JX had the same psychotic symptoms over the years before starting clozapine but she never restricted her diet for a prolonged period of time as a way of punishing the imagined woman. This happened only after clozapine was started. Though no specific cognitive ability was carried out on her prior to treatment with clozapine, it can be hypothesized that following clozapine initiation, her cognitive ability improved even though she was still experiencing the same psychotic symptoms. The improved cognitive ability afforded her the planning and execution ability she needed to act on her belief, restricting her diet intake resulting in significant weight loss. Other aspects of her life also improved. For the first time in many years, JX was able to go out alone and explore areas further away from the unit, again supporting the view that her cognitive ability had improved. JX’s psychotic symptoms improved further following augmentation with amisulpiride. The ongoing active intervention to manage her diet stopped further weight loss.
Could the observed weight loss be attributable to improvement in her negative symptoms? That was less likely for the following reasons. First, negative symptoms were not a prominent feature of JX’s presentation. Depending on the definition used, the prevalence of persistent negative symptoms in patients with chronic schizophrenia varies between 20% and 58% [Sarkar et al. 2015; Chue and Lalonde, 2014]. The symptoms tend to persist longer, are more difficult to treat than the positive symptoms and predict poor social function [Sarkar et al. 2015; Chue and Lalonde, 2014]. No specific treatment exists today though there is limited evidence that some second-generation antipsychotics, antidepressants and N-methyl-D-aspartate receptor enhancers may reduce the severity of negative symptoms [Chue and Lalonde, 2014]. Second, the specific symptoms related to food were positive symptoms in the form of auditory hallucinations and the associated delusion about a woman who wanted food. These symptoms were markedly present as JX gradually lost weight. Finally, one would have expected JX to engage in diet and increased physical activities with staff to manage her weight. However, that was not the case. Instead, it was noted that JX actively restricted her diet intake. She would decline to eat during mealtimes or would take her leave shortly before meals were served. She became secretive as far as her dietary intake was concerned and continued to have the same positive symptoms.
Mechanisms of antipsychotic-induced weight loss
Clozapine, a second-generation antipsychotic, has affinity on many receptors including dopamine (DA), serotonin (5HT), muscarinic (M), histamine (H), adrenergic, GABAergic and glutamatergic receptors to mention a few. This poly-receptor profile activity is believed to account not only for its unique efficacy but also for the side effects including weight gain and weight loss [De Berardis et al. 2012; Wenthur and Lindsley, 2013; Valpato et al. 2013; Werneke et al. 2013].
It is known that antipsychotics that have strong antagonistic activity on DA2, 5HT2c, M3 and H1 receptor subtypes are associated with a propensity to cause weight gain, while antipsychotics that have less affinity to or have agonist activity are associated with less weight gain. Clozapine has strong antagonist activity at M3, H1 and 5HT2c subtypes and is associated with significant weight gain [De Berardis et al. 2012; Wenthur and Lindsley, 2013; Valpato et al. 2013].
The mechanisms underlying the propensity to induce weight loss are complex. It is likely that environmental and genetic factors, a complex series of neurotransmitters and neuropeptides, and a number of brain areas are involved [Fiedorowicz et al. 2012; Zhang and Malhotra, 2013]. It has been repeatedly shown that agonists or having a weak antagonist activity at 5HT2c subtype receptors is associated with less weight gain. Typical examples here are aripiprazole and ziprasidone. It is thought that the anorexigenic effect of leptin (from white adipose tissue), melanocortin and proopiomelanocortin, are also mediated through 5HT2c [Lee and Bishop, 2011; Wallace et al. 2011]. Evidence also shows that having a certain genetic type of 5HT2c (−759 C/T, T allele rather than C allele) protects against antipsychotic-induced weight gain [Wallace et al. 2011; Reynolds, 2012].
Histamine receptors are involved in a number of physiological responses including eating behaviour. Centrally, H1 receptors are exclusively found at the tuberomamillary nucleus of the posterior hypothalamus. Agonists at H1 receptors significantly decrease food intake [Valpato et al. 2013]. Histamine can suppress the mesolimbic DA pathway involved in controlling palatable food. Leptin, another anorexigenic hormone, is said to exert its effect via histamine. It can therefore be seen that histamine antagonists, of which clozapine has strong affinity, will disrupt the system resulting in weight gain, whereas agonists at H1 have been associated with weight loss [Teff and Kim, 2011; Valpato et al. 2013].
M receptors blockade, especially M3 subtypes, have been associated with weight gain and insulin resistance [Teff and Kim, 2011; Valpato et al. 2013]. Antagonist activity at M3 has been noted to be the strongest predictor of type II diabetes for patients on antipsychotics, of which clozapine is a leading offender [Valpato et al. 2013]. A number of neuropeptides are involved in reducing food intake such as α-melanocyte-stimulating hormone from the hypothalamus, leptin, insulin and glucagon [Werneke et al. 2013]. The endocannabinoid system (CB) is involved in appetite, reward, hunger and satiety [Loh and Kew, 2008; Tiwari et al. 2010]. Centrally CB1 increases appetite and also interacts with DA to promote food searching and is said to regulate glucose metabolism and lipogenesis [Loh and Kew, 2008; Tiwari et al. 2010]. However, a CB1 antagonist such as rimonabant has been associated with significant weight loss [Loh and Kew, 2008].
Based on the current known clozapine receptor profile, it is not apparent how it can cause weight loss without other factors such as genetic variations coming into play. It has been observed however, that blocking DA2 receptors can create an anhedonic effect triggering compulsive eating and possibly weight gain [Werneke et al. 2013]. However, not all overeat or gain weight suggesting that due to having certain genetic variation some are able to suppress overeating and avoid weight gain [Werneke et al. 2013]. JX did not have overeating or compulsive eating behaviour; instead she restricted her diet intake following the introduction of clozapine. A detailed study of patients who experience this phenomenon may provide some needed breakthrough.
Weight management
Managing weight is paramount for patients on antipsychotic medications. Being overweight has been associated with a number of untoward events such metabolic syndrome, type II diabetes, hypertension, stroke and untimely death. There are also psychological factors such stigma, low confidence, poor image and low self-esteem [Lee and Bishop, 2011; Raja, 2011; Werneke et al. 2013].
Management of antipsychotic-induced weight needs to include a number of strands such as lifestyle changes, cognitive behavioural therapy, change to antipsychotics that are less likely to cause weight gain and adding compounds known to induce weight loss [Kwon et al. 2006; Khazaal et al. 2007; Raja, 2011; Werneke et al. 2013]. Lifestyle modification was possible in two cases [Lally and McDonald. 2011; Appiani, 2011]. In the case of clozapine, adding compounds that are known to induce weight loss such as topiramate, aripiprazole and metformin [Karunakaran et al. 2007; Fiedorowicz et al. 2012], are options that can be considered if switching to other antipsychotics is not possible. Aripiprazole has agonist effect on 5HT2C resulting in reduced appetite. Topiramate inhibits lipogenesis peripherally. Centrally it increases satiety and hence reduces appetite [Fiedorowicz et al. 2012]. Metformin is an antidiabetic drug that in addition to improving glycaemic control is thought to reduce appetite by causing taste disturbance, nausea and by increasing the anorexic glucagon-like peptide-1 [Fiedorowicz et al. 2012]. Effective antipsychotics with negligible effect on weight are still being sought. Better ways of managing antipsychotic-induced weight gain are still being explored. Interestingly, how clozapine induces weight loss in some individuals remains unknown half a century after it was manufactured. Its pharmacodynamics profiles continue to be of interest to both researchers and clinicians.
Conclusion
Though commonly associated with weight gain, clinicians need to be aware that some patients with TRS may lose significant weight following clozapine use. Three groups appear to emerge at present. However, in all published cases, weight loss was not attributable to diagnosable physical illnesses. Physical evaluation is indicated to exclude any underlying treatable conditions. In some however, weight loss may be the early visible sign of a poor response to clozapine. The mechanisms involving clozapine induced weight loss and a poor response to clozapine are not yet fully understood.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest statement: The author declares that there is no conflict of interest.
References
- Appiani F., Carroll B., Muñoz C., Trecco J. (2011) Clozapine-induced weight loss? Ann Clin Psychiatry 23: 225. [PubMed] [Google Scholar]
- Chue P., Lalonde J. (2014) Addressing the unmet needs of patients with persistent negative symptoms of schizophrenia: emerging pharmacological treatment options. Neuropsychiatr Dis Treat 10: 777–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conley R., Buchanan R. (1997) Evaluation of treatment-resistant schizophrenia. Schizophr Bull 23: 663–674. [DOI] [PubMed] [Google Scholar]
- Covell N., Weissman E., Essock S. (2004) Weight gain with clozapine compared to first generation antipsychotic medications. Schizophr Bull 30: 229–240. [DOI] [PubMed] [Google Scholar]
- Czobor P., Volavka J., Sheitman B., Lindenmayer J., Citrome L., McEvoy J., et al. (2002) Antipsychotic-induced weight gain and therapeutic response: a differential association. J Clin Psychopharmacol 22: 244–251. [DOI] [PubMed] [Google Scholar]
- De Berardis D., Serroni N., Campanella D., Olivieri L., Ferri F., Carano A., et al. (2012) Update on the adverse effects of clozapine: focus on myocarditis. Curr Drug Saf 7: 55–62. [DOI] [PubMed] [Google Scholar]
- Fiedorowicz J., Miller D., Bishop J., Calarge C., Ellingrod V., Haynes W. (2012) Systematic review and meta-analysis of pharmacological interventions for weight gain from antipsychotics and mood stabilizers. Curr Psychiatry Rev 8: 25–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanwella R., de Silva V., Wijeratne C., Ketharanathan T., de Silva J. (2010) Clozapine-associated weight loss. J Psychopharmacol 24: 1127–1129. [DOI] [PubMed] [Google Scholar]
- Hermes E., Nasrallah H., Davis V., Meyer J., McEvoy J., Goff D., et al. (2011) The association between weight change and symptom reduction in the CATIE schizophrenia trial. Schizophr Res 128: 166–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane J., Honigfeld G., Singer J., Meltzer H. (1988) Clozapine for the treatment-resistant schizophrenic: a double-blind comparison with chlorpromazine. Arch Gen Psychiatry 45: 789–796. [DOI] [PubMed] [Google Scholar]
- Karunakaran K., Tungaraza T., Harbone G. (2007) Is clozapine-aripiprazole combination a useful regime in the management of treatment-resistant schizophrenia? J Psychopharmacol 21: 453–456. [DOI] [PubMed] [Google Scholar]
- Khazaal Y., Fresard E., Rabia S., Chatton A., Rothen S., Pomini V., et al. (2007) Cognitive behavioural therapy for weight gain associated with antipsychotic drugs. Schizophr Res 91: 169–177. [DOI] [PubMed] [Google Scholar]
- Kwon J., Choi J., Bahk W., Yoon Kim C., Hyung Kim C., Chul Shin Y., et al. (2006) Weight management program for treatment-emergent weight gain in olanzapine-treated patients with schizophrenia or schizoaffective disorder: a 12-week randomized controlled clinical trial. J Clin Psychiatry 67: 547–553. [DOI] [PubMed] [Google Scholar]
- Lally J., McDonald C. (2011) Dramatic weight loss associated with commencing clozapine. BMJ Case Rep: doi:.1136/bcr.09.2011.4790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee K., Bishop J. (2011) Pharmacogenetics of leptin in antipsychotic-associated weight gain and obesity-related complications. Pharmacogenomics 12: 999–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis S., Barnes T., Davies L., Murray R., Dunn G., Hayhurst K., et al. (2006) Randomized controlled trial of effect of prescription of clozapine versus other second-generation antipsychotic drugs in resistant schizophrenia. Schizophr Bull 32: 715–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberman J., Stroup T., McEvoy J., Swartz M., Rosenheck R., Perkins D., et al. (2005) Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 353: 1209–1223. [DOI] [PubMed] [Google Scholar]
- Loh K., Kew S. (2008) Endocannabinoid system and cardio-metabolic risk. Med J Malaysia 63: 348–530. [PubMed] [Google Scholar]
- McGrath J., Saha S., Chant D., Welham J. (2008) Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiol Rev 30: 67–76. [DOI] [PubMed] [Google Scholar]
- Meltzer H.Y. (1989) Duration of a clozapine trial in neuroleptic-resistant schizophrenia. Arch Gen Psychiatry 46: 672. [DOI] [PubMed] [Google Scholar]
- Meltzer H., McGurk S. (1999) The effects of clozapine, risperidone, and olanzapine on cognitive function in schizophrenia. Schizophr Bull 25: 233–255. [DOI] [PubMed] [Google Scholar]
- Procyshyn R., Wasan K., Thornton A., Barr A., Chen E., Pomarol-Clotet E., et al. ; Clozapine and Risperidone Enhancement Study Group (2007) Changes in serum lipids, independent of weight, are associated with changes in symptoms during long-term clozapine treatment. J Psychiatry Neurosci 32: 331–338. [PMC free article] [PubMed] [Google Scholar]
- Raja M. (2011) Clozapine safety, 35 years later. Curr Drug Saf 6: 164–184. [DOI] [PubMed] [Google Scholar]
- Reynolds G. (2012) Pharmacogenetic aspects of antipsychotic drug-induced weight gain – a critical review. Clin Psychopharmacol Neurosci 10: 71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rummel-Kluge C., Komossa K., Schwarz S., Hunger H., Schmid F., Lobos C., et al. (2010) Head-to-head comparisons of metabolic side effects of second generation antipsychotics in the treatment of schizophrenia: a systematic review and meta-analysis. Schizophr Res 123: 225–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkar S., Hillner K., Velligan D. (2015) Conceptualization and treatment of negative symptoms in schizophrenia. World J Psychiatry 5: 352–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanton J. (1995) Weight gain associated with neuroleptic medication: a review. Schizophr Bull 21: 463–472. [DOI] [PubMed] [Google Scholar]
- Sumiyoshi T., Higuchi Y., Uehara T. (2013) Neural basis for the ability of atypical antipsychotic drugs to improve cognition in schizophrenia. Front Behav Neurosci 7: 140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teff K., Kim S. (2011) Atypical antipsychotics and the neural regulation of food intake and peripheral metabolism. Physiol Behav 104: 590–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas N., Ravan J., Jebaraj P., Braganza D. (2009) Clozapine producing weight loss: a case series with possible clinical implications – a hypothesis. J Postgrad Med 55: 317. [DOI] [PubMed] [Google Scholar]
- Tiwari A., Zai C., Likhodi O., Lisker A., Singh D., Souza R., et al. (2010) A common polymorphism in the cannabinoid receptor 1 (CNR1) gene is associated with antipsychotic induced weight gain in schizophrenia. Neuropsychopharmacology 35: 1315–1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valpato A., Zugno A., Quevedo J. (2013) Recent evidence and potential mechanisms underlying weight gain and insulin resistance due to atypical antipsychotics. Rev Bras Psiquiatr 35: 295–304. [DOI] [PubMed] [Google Scholar]
- Wahlbeck K., Cheine M., Essali A., Adams C. (1999) Evidence of clozapine’s effectiveness in schizophrenia: a systematic review and meta-analysis of randomized trials. Am J Psychiatry 156: 990–999. [DOI] [PubMed] [Google Scholar]
- Wallace T., Zai C., Brandl E., Müller D. (2011) Role of 5-HT(2C) receptor gene variants in antipsychotic-induced weight gain. Pharmgenomics Pers Med 4: 83–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster A., Ingram L. (2013) A weight off the mind: clozapine and profound weight loss. Aust NZ J Psychiatry 47: 1212–1213. [DOI] [PubMed] [Google Scholar]
- Weickert T., Goldberg T., Marenco S., Bigelow L., Egan M., Weinberger D. (2003) Comparison of cognitive performances during a placebo period and an atypical antipsychotic treatment period in schizophrenia: critical examination of confounds. Neuropsychopharmacology 28: 1491–1500. [DOI] [PubMed] [Google Scholar]
- Wenthur C., Lindsley C. (2013) Classics in chemical neuroscience: clozapine. ACS Chem Neurosci 4: 1018–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werneke U., Taylor D., Sanders T. (2013) Behavioral interventions for antipsychotic induced appetite changes. Curr Psychiatry Rep 15: 347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Malhotra A. (2013) Pharmacogenetics of antipsychotics: recent progress and methodological issues. Expert Opin Drug Metab Toxicol 9: 183–191. [DOI] [PMC free article] [PubMed] [Google Scholar]