Abstract
Purpose
Cerebral perfusion territories are known to vary widely among individuals. This may lead to misinterpretation of the symptomatic artery in patients with ischaemic stroke to a wrong assumption of the underlying aetiology being thromboembolic or hypoperfusion. The aim of the present study was to investigate such potential misinterpretation with territorial arterial spin labelling (T-ASL) by correlating infarct location with imaging of the perfusion territory of the carotid arteries or basilar artery.
Materials and methods
223 patients with subacute stroke underwent MRI including structural imaging scans to determine infarct location, time-of-flight MR angiography (MRA) to determine the morphology of the circle of Willis and T-ASL to identify the perfusion territories of the internal carotid arteries, and basilar artery. Infarct location and the perfusion territory of its feeding artery were classified with standard MRI and MRA according to a perfusion atlas, and were compared to the classification made according to T-ASL.
Results
A total of 149 infarctions were detected in 87 of 223 patients. 15 out of 149 (10%) infarcts were erroneously attributed to a single perfusion territory; these infarcts were partly located in the originally determined perfusion territory but proved to be localised in the border zone with the adjacent perfusion territory instead. 12 out of 149 (8%) infarcts were misclassified with standard assessments and were not located in the original perfusion territory.
Conclusions
T-ASL with territorial perfusion imaging may provide important additional information for classifying the symptomatic brain-feeding artery when compared to expert evaluation with MRI and MRA.
Introduction
Diagnosis of the ischaemic stroke mechanism is important for prevention of recurrent stroke in patients with a recent transient ischaemic attack (TIA) or stroke. Differentiation between infarcts caused by emboli, decreased perfusion or local thrombosis depends predominantly on the presence of risk factors, the size of the infarct and the presence of large-vessel occlusions. The location of the infarct in relationship to the perfusion territories of the brain-feeding arteries may be used for confirming the thromboembolic source in patients with symptomatic carotid disease, and also for identifying ‘border zone’ or ‘watershed’ infarcts in patients with compromised cerebral perfusion.1
Standardised perfusion territory atlases of the brain are used to determine the location of the ischaemic lesion. However, studies have shown that there is wide variability in the perfusion territories on the brain-feeding arteries.2–4 This variability is even more pronounced in patients with a pre-existent carotid steno-occlusive disease due to collateral blood flow recruitment.5 6 Owing to this large between-subject variability, standard perfusion territories maps may fall short and lead to misinterpretation of the infarct location or its aetiology with respect to a thromboembolic or haemodynamic origin. Territorial arterial spin labelling (T-ASL) perfusion MRI is a new non-invasive technique that can be used to determine the flow territories of the brain-feeding arteries at the brain tissue level and to detect collateral blood flow patterns through the circle of Willis.
The aim of the current study is to investigate whether assessment of the cerebral perfusion territories with T-ASL may lead to reconsideration of the symptomatic cerebropetal artery related to infarct location and its aetiology, and to determine the prevalence of such misinterpretations in patients with acute and subacute stroke. To achieve this goal, we defined the symptomatic artery by examining the infarct location and the configuration of the circle of Willis, and we assessed cerebral perfusion territories of the brain-feeding arteries with T-ASL perfusion MRI.
Materials and methods
This study was conducted in compliance with medical research protection requirements involving human participants. The institutional review board approved the study and a waiver of informed consent was obtained.
Patients
Over a period of 18 months, patients referred consecutively by a general practitioner or neurologist to our hospital, a tertiary referral centre for stroke, for follow-up after a TIA or non-disabling minor ischaemic stroke (modified Rankin scale score of 1–2) were included in this study.7 As part of the standard clinical work-up for secondary prevention, all patients underwent MRI examination to assess the prior ischaemic damage, cerebrovasculature and rule out potential stroke mimickers. Duplex ultrasonography of the carotid arteries and vertebral arteries was performed to diagnose and grade a potential carotid artery stenosis or occlusion based on peak systolic velocity.8 9 If present, the stenosis or occlusion of the carotid arteries was confirmed with either a recent contrast-enhanced (CE) CT angiography or with CE magnetic resonance angiography (CE MRA) and graded according to the North American Symptomatic Carotid Endarterectomy Trial (NASCET) criteria.10
MRI protocol
MRI was performed on a clinical 3 T MRI scanner (Achieva, Philips Medical Systems, Best, the Netherlands) equipped with an eight-channel coil. A standardised imaging protocol for clinical routine follow-up of cerebral stroke was used, including T1-weighted and T2-weighted imaging, diffusion-weighted imaging (DWI), T2-weighted fluid attenuation inversion recovery (FLAIR) imaging, three-dimensional time-of-flight MRA (3D TOF MRA) of the circle of Willis, T-ASL perfusion imaging and CE T1-weighted imaging using a single dose of gadolinium.
The structural and anatomical images were acquired with the vendor's standard available sequences. DWI and FLAIR images were acquired for detecting areas of tissue infarction. The FLAIR sequence parameters were as follows: repetition time/echo time (TR/TE), 11 000/125 ms; inversion time (IR), 2800 ms; field of view (FOV), 220×220 mm2; matrix size, 512×512; slices, 26; slice thickness, 4 mm with 1 mm gap; and scan time, 4 min. The DWI sequence parameters were as follows: TR/TE, 3055/62 ms; FOV, 220×220 mm2; matrix size, 512×512; slices, 26; slice thickness, 4 mm with 1 mm gap; and scan time, 2 min.
A 3D TOF MRA of the circle of Willis was acquired with subsequent maximal intensity projection reconstruction using the following parameters: TR/TE, 30/6.9 ms; flip angle, 20°; 2 dynamics; FOV, 100×100 mm2; matrix, 256×256; slices, 50; slice thickness, 1.2 mm with 0.6 mm overlap; and scan time, 3 min.
Perfusion territory imaging
The T-ASL perfusion images were acquired with a planning-free vessel-encoded (VE) pseudo-continuous ASL (p-CASL) sequence, as outlined in a previous study.11 This technique used radiofrequency pulses to magnetically label the blood. Selective labelling was accomplished through manipulating the spatial labelling efficiency. This was achieved by applying additional gradients between the labelling pulses in sets of five variations: no label (control), full non-selective label (global perfusion), right-to-left encoded label (with 50 mm between full label and control) and two anterior-to-posterior encoded label variations (with 18 mm between full label and control, each shifted 9 mm from each other).
Image processing was performed in MATLAB (MathWorks, Natick, Massachusetts, USA). The perfusion territories of right and left internal carotid arteries (RICA and LICA) and the basilar artery (BA) in the VE p-CASL images were identified with k-means clustering, as described in detail in a previous study.11 To identify the perfusion territories, first the images with the same spatial ASL encoding were averaged and subsequent subtraction of label and control pairs resulted in four perfusion-weighted images. According to the spatial ASL encoding, there was one global (non-selective) perfusion image and three (spatially encoded) selective perfusion images. Relative labelling efficiencies were calculated by normalising the signal intensities of each (spatially encoded) selective perfusion image with the signal intensity of the global perfusion image. This yielded three relative labelling efficiency maps, which were used with the k-means clustering algorithm to segment the perfusion territories into three or two territories depending on the presence of an ICA occlusion.12–14 To improve the outcome of the k-means clustering algorithm, the x, y and z coordinates of each voxel (normalised by half the FOV in that direction) were also included as features in the clustering.12 15 16
Evaluation of cerebral infarct location and perfusion territory
Two board-certified neuroradiologists (JH and LJLDC) evaluated the DWI, T2-weighted and FLAIR images for acute and subacute cerebral infarcts. In each patient, the location of an infarct was determined in two ways: (1) according to a standardised perfusion territory atlas supplemented with MR angiographic information and (2) according to the acquired T-ASL perfusion maps. Both reads were done randomly in a separate session. The readers were blinded to the patient's identity, clinical information and diagnosis. Discrepancies were resolved in a consensus meeting.
The location of a cerebral infarct was categorised with both methods to be in the perfusion territory of the right ICA, left ICA, BA or in a border zone area between two perfusion territories of the anterior cerebral artery (ACA), middle cerebral artery (MCA) or posterior cerebral artery (PCA). Infarcts that affected more than two lobes or that comprised a cortical and subcortical area were considered large infarcts. Cortical areas were restricted to one lobe and were defined as follows: frontal lobe, parietal lobe, temporal lobe, occipital lobe and the insula. Subcortical areas were defined as follows: corpus callosum, the caudate or lentiform nucleus either in isolation or in combination (corpus striatum), thalamus, internal and external capsule, and the remaining deep white matter including corona radiate and semioval centre. Cerebellar infarcts were not included in this study.
For the reads based on a standardised template,17 it was assumed that in a normal configuration of the circle of Willis, the ACA and MCA were supplied by their ipsilateral ICA, and the PCA was supplied by the BA. In case of a missing A1 segment, it was assumed that the ACA was supplied by the contralateral ICA. In case of a fetal-type circle of Willis, it was assumed the PCA was supplied by the ipsilateral ICA. In case of ICA occlusion, it was assumed the ipsilateral ACA and MCA were supplied by a collateral route through the circle of Willis with a preference for the contralateral ICA and BA, respectively. For the subcortical areas, it was assumed the corpus striatum was supplied by the medial and lateral lenticulostriate arteries originating from the ACA and MCA, respectively, even though variations in the blood supply of the caudate nucleus are known to exist.18 The thalamus was assumed to be supplied by branches originating from the PCA, even though many variations in the blood supply of the thalamus are also known to exist.19
The territorial classifications of cerebral infarcts with the standard perfusion territory atlas complemented with MRA were compared with the perfusion territory as determined with T-ASL. Two types of mismatch were considered. We defined two different types of mismatch. The first was partial mismatch, where an infarct was classified to a specific territory, but was actually found to located on the border zone with an adjacent territory on T-ASL, or vice versa. The second was a complete mismatch, where an infarct was classified in a complete other territory than determined on T-ASL.
Results
Two hundred and twenty-three symptomatic patients were included consecutively in this study over a period of 18 months. Table 1 outlines the demographic and clinical patient characteristics. A total of 149 infarctions were detected in 87 of the 223 patients, as outlined in table 2. A total of 28 out of 87 patients (32%) with detected infarctions had an infarction that showed restricted diffusion on DWI. Thirty-nine patients had more than one infarction. One infarct was located in the brainstem. A total of 52 of the remaining 148 infarcts were located cortically and 72 infarcts were located subcortically. Twenty-four infarcts were located in the cortical and subcortical regions, or in more than one lobe. Figures 1–4 show representative case examples.
Table 1.
Demographic and clinical patient characteristics
| Number | 223 |
|---|---|
| Age, mean years±SD | 64±12 |
| Men, n (%) | 141 (59%) |
| Reason for presentation, n | |
| Minor ischaemic stroke | 110 |
| Transient ischaemic attack | 113 |
| Symptom onset to imaging time, median days (IQR) | 6 (2–19) |
| Comorbidity, n | |
| Antithrombotic drugs | 223 |
| Antihypertensive drugs | 43 |
| Lipid-lowering drugs | 39 |
| Diabetes | 21 |
| Previous myocardial infarction | 10 |
| Previous cardiac bypass surgery | 9 |
| Peripheral artery disease | 6 |
| Current or recently stopped smoker | 33 |
| Degree of ICA stenosis, n | |
| 0–50% | 97 |
| 50–70% | 19 |
| 70–99% | 58 |
| Occlusion | 49 |
| Degree of contralateral ICA stenosis, n | |
| 0–50% | 156 |
| 50–70% | 25 |
| 70–99% | 35 |
| Occlusion | 7 |
| Degree of BA stenosis, * n | |
| 0–50% | 208 |
| 50–99% unilateral | 9 |
| 50–99% bilateral | 4 |
| Occlusion unilateral | 2 |
*Based on peak systolic velocity criteria for duplex ultrasound.
BA, basilar artery; ICA, internal carotid artery.
Table 2.
Correct classification of infarcts per anatomical area
| Anatomical location | Correctly classified (n) | Misclassified | (n, %) |
|---|---|---|---|
| Brainstem | 1 | 0 | 0 |
| Large | 18 | 6 | 25 |
| Cortex | |||
| Insula | 2 | 1 | 33 |
| Frontal lobe | 16 | 4 | 20 |
| Parietal lobe | 11 | 6 | 35 |
| Parieto-occipital lobe | 2 | 0 | 0 |
| Parietotemporal lobe | 1 | 0 | 0 |
| Temporal lobe | 2 | 0 | 0 |
| Temporo-occipital lobe | 3 | 0 | 0 |
| Occipital lobe | 3 | 1 | 25 |
| Subcortical | |||
| Corpus callosum | 2 | 0 | 0 |
| Corpus striatum | 11 | 2 | 15 |
| Caudate nucleus | 15 | 3 | 17 |
| Lentiform nucleus | 11 | 0 | 0 |
| Internal capsule | 2 | 0 | 0 |
| Thalamus | 16 | 6 | 27 |
| Corona radiate | 4 | 0 | 0 |
| Total | 120 | 29 | 19 |
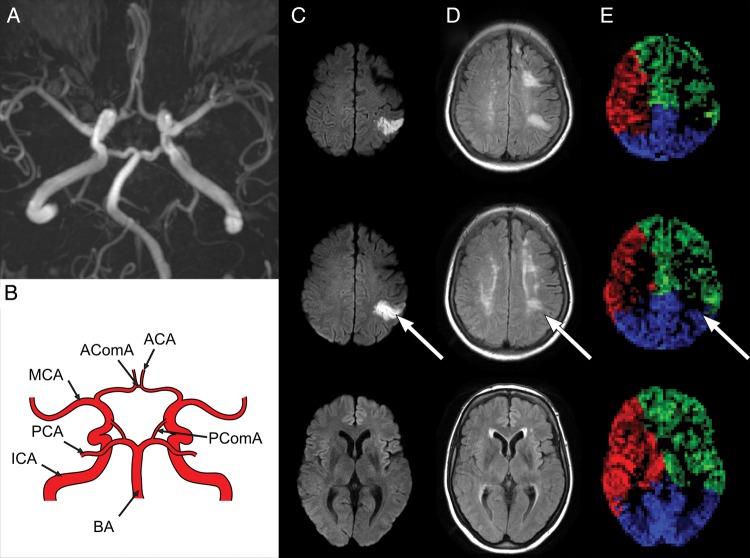
Figure 1.
Example of a 53-year-old female with left internal carotid artery (ICA) stenosis >70%. Time-of-flight magnetic resonance angiography (MRA) image (A) shows a complete circle of Willis as illustrated in the schematic drawing (B). Diffusion-weighted imaging (DWI) (C) and fluid attenuation inversion recovery (FLAIR) images (D) and corresponding territorial arterial spin labelling (T-ASL) perfusion maps (E) from caudal (left) to cranial (right). A recent parietal cortical ischaemic infarct showing diffusion restriction (C, arrow) may be appreciated on the FLAIR images (D, arrow). Using the standard perfusion territory atlas, the infarct was assumed to be within the middle cerebral artery (MCA) perfusion territory of the left ICA. T-ASL perfusion maps (E) show the perfusion territories of the right ICA (red), left ICA (green) and the basilar artery (BA) (blue), and locate the infarct on the border zone of the MCA and posterior cerebral artery (PCA) perfusion territories.
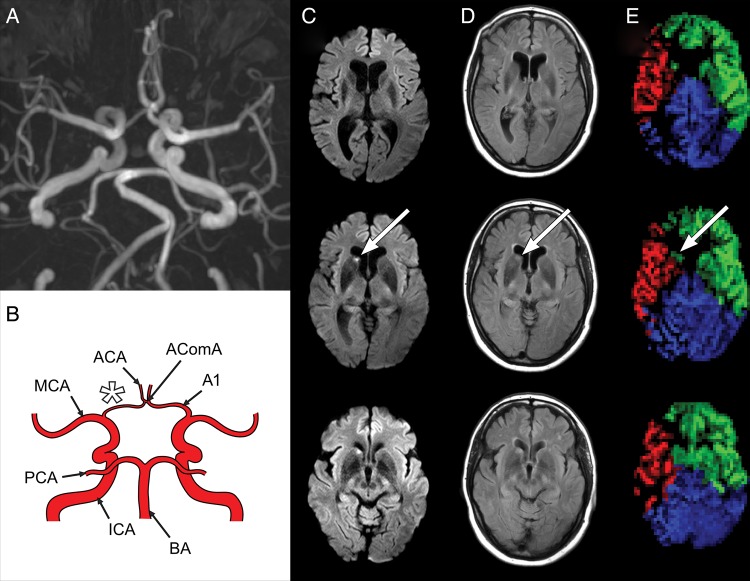
Figure 2.
Example of a 50-year-old female with right internal carotid artery (ICA) stenosis >70%. Time-of-flight magnetic resonance angiography (MRA) image (A) shows a hypoplastic A1 segment (A, B, star) as illustrated in the schematic drawing (B). Diffusion-weighted imaging (DWI) (C) and fluid attenuation inversion recovery (FLAIR) images (D) and territorial arterial spin labelling (T-ASL) perfusion maps (E) are presented identically to figure 1. A recent lacunar infarct in the caudate nucleus showing diffusion restriction (C, arrow) may be appreciated on the FLAIR images (D, arrow). Using the standard perfusion territory atlas, the infarct was assumed to be within the territory of the right ICA. T-ASL perfusion maps show however the infarct is located in the perfusion territory of the (contralateral) left ICA (E, arrow). PCA, posterior cerebral artery.
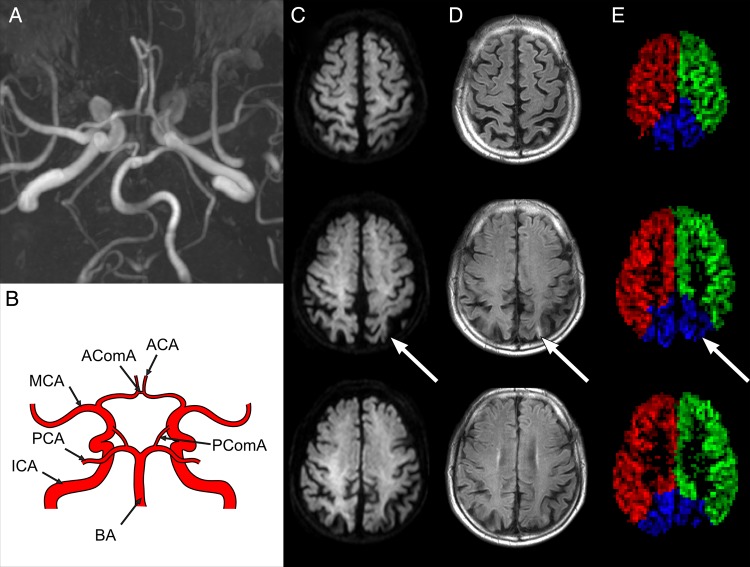
Figure 3.
Example of a 71-year-old male with a left-sided internal carotid artery (ICA) stenosis 50%. Time-of-flight magnetic resonance angiography (MRA) image (A) shows a complete circle of Willis as illustrated in the schematic drawing (B). Diffusion-weighted imaging (DWI) (C) and fluid attenuation inversion recovery (FLAIR) images (D) and territorial arterial spin labelling (T-ASL) perfusion maps (E) are presented identically to figure 1. A chronic occipital cortical ischaemic infarct can be appreciated on the FLAIR images (D, arrow). By applying the standard perfusion territory atlas, it was determined the infarct was located in the border zone of the middle cerebral artery (MCA) and posterior cerebral artery (PCA). The T-ASL perfusion maps show that the ischaemic lesion is within the perfusion territory of the basilar artery (BA) (E, arrow) instead.
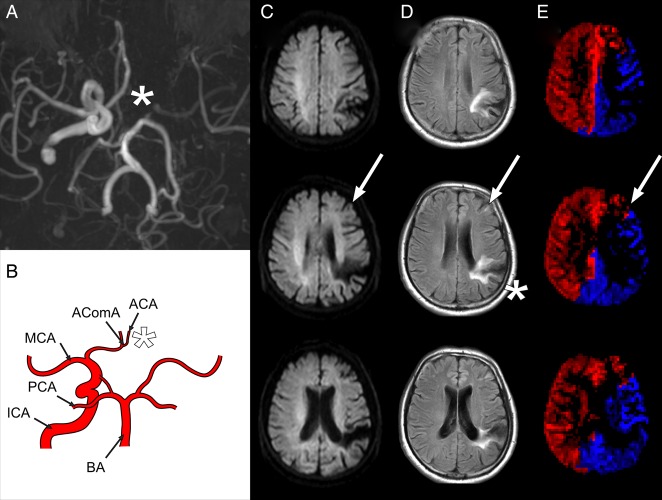
Figure 4.
Example of a 60-year-old male with a left-sided internal carotid artery (ICA) occlusion. Time-of-flight magnetic resonance angiography (MRA) image (A) shows an absent A1 segment (A, B, asterisk) as illustrated in the schematic drawing (B), with collateral flow to the anterior carotid artery (ACA) via the AcomA and collateral flow to the middle carotid artery (MCA) via the PcomA. Diffusion-weighted imaging (DWI) (C) and fluid attenuation inversion recovery (FLAIR) images (D) and territorial arterial spin labelling (T-ASL) perfusion maps (E) are presented identically to figure 1. A small frontal infarct (D, arrow) and a large chronic parietal infarct (D, star) can be appreciated in the FLAIR images. The small frontal infarct is of a recent date, even though it does not show diffusion restriction (C, arrow), since it was not visible on earlier imaging. By applying the standard perfusion territory atlas, it was determined the infarct was located within the MCA territory, currently supplied by the basilar artery (BA). The T-ASL perfusion maps show the small recent frontal infarct is not located within the MCA territory but is actually located on the border zone of the ACA and MCA (E, arrow), and is thus currently supplied by the right (contralateral) ICA as well as the BA. PCA, posterior cerebral artery.
Table 3 shows the territorial classification of cerebral infarcts with the standard perfusion territory atlas and as assessed with T-ASL. There was a mismatch between the expected infarction location in 29 of the 149 (19%) infarcts. On the basis of the territorial perfusion maps, the perfusion territory altered in between the expected infarction location in 12 of the 52 (23%) cortical infarcts, in 11 of the 72 (15%) subcortical infarcts and in 6 of the 24 (25%) large infarcts.
Table 3.
Infarct location classification by applying a perfusion territory atlas complemented by MRA clues as opposed to using T-ASL perfusion map
| T-ASL perfusion map | |||||
|---|---|---|---|---|---|
| Perfusion territory atlas+MRA clues | Ipsilateral ICA | BDZ ipsilateral ICA+BA | Contralateral ICA | BDZ contralateral ICA+BA | BA |
| Ipsilateral ICA | 64 | 2 | 1 | 0 | 0 |
| BDZ ipsilateral ICA+BA | 1 | 5 | 0 | 0 | 1 |
| Contralateral ICA | 0 | 0 | 19 | 10 | 4 |
| BDZ contralateral ICA+BA | 0 | 0 | 0 | 7 | 0 |
| BA | 4 | 2 | 3 | 1 | 25 |
BDZ indicates border zone between the stated vascular territories of the ipsilateral or contralateral ICA or BA. BA, basilar artery; ICA, internal carotid artery; MRA, magnetic resonance angiography; T-ASL, territorial arterial spin labelling.
A total of 15 out of 149 (10%) infarcts were wrongly attributed to a single perfusion territory, while on the basis of the perfusion maps, these infarcts were localised in the adjacent border zone (partial mismatch). In total, 27 of 149 (18%) infarcts were border zone infarcts as determined by T-ASL. In 12 out of 149 (8%) infarcts, the localisation was completely in a different perfusion territory (complete mismatch). Seven (5%) of the infarcts that were misclassified showed restricted diffusion on DWI. All of these patients had an ICA stenosis on the side of the infarct; one a stenosis of 50% and six a stenosis >70%. One infarct was actually located in the contralateral ICA, four infarcts were wrongly attributed to the BA territory, two infarcts were wrongly attributed to the border zone of the ipsilateral ICA and BA, while one was actually located in the ipsilateral ICA territory and one was located in the BA territory instead.
Discussion
To the best of our knowledge, this is the first study that shows the cross-sectional relation between cerebral infarct location and territories with perfusion disorders in vivo. The study shows that traditional perfusion territory maps are unreliable when trying to use the brain tissue-feeding artery to differentiate a territorial from a watershed infarct. This means that in a large proportion of patients with stroke with a steno-occlusive lesion in the carotid artery, with traditional MR assessments, it is difficult to distinguish a thromboembolic from a hypoperfusion origin of the infarct.
European guidelines for the management of ischaemic stroke and the management of symptomatic carotid artery stenosis currently recommend that patients with recent symptomatic carotid artery stenosis should undergo revascularisation within 2 weeks of symptoms.20 21 For this reason, the correct identification of the symptomatic perfusion territory may be important before revascularisation is planned. With the direct cross-sectional visualisation of perfusion territories by means of T-ASL MRI, the territorial classification in 19% of the cerebral infarcts changed, 5% of which were acute or subacute lesions. A partial mismatch between the assumed and measured perfusion territory was more frequent than a complete mismatch. As ischaemia in the border zone may be caused by hypoperfusion or thromboemboli, reclassification of a cerebral infarct usually lacks clinical consequences. However, it may potentially impact clinical care in those with complete mismatch. For instance, in patients with an infarct in the basal ganglia, the primary blood supply may originate from the contralateral hemisphere through crossflow via the anterior communicating artery or recurrent artery of Heubner (figure 2). Territorial perfusion imaging can potentially also be useful to determine the location of an ischaemic lesion in patients where there is a shift in the flow distribution through the circle of Willis (figure 4). While reclassification of a cerebral infarct to a border zone infarct usually lacks clinical consequences, as ischaemia in these locations may be caused by hypoperfusion possibly in combination with thromboembolic phenomena, in the current study, the therapeutic management of 7 patients (8% of 87 patients with an infarct) with territorial misinterpretation of cerebral infarcts should be reappraised based on imaging findings.20 For instance, it may be necessary to treat a carotid stenosis that was initially considered asymptomatic because the infarct was incorrectly localised in the perfusion territory of the BA. Thus, territorial perfusion imaging can provide important information when determining individualised treatment.
Based on autopsy studies, the prevalence of border zone infarcts was previously reported around 10%.22–24 In this study, 18% of the infarcts were ultimately classified as border zone infarcts, while only 8% were initially classified as border zone infarct when only using standardised templates. Based on our findings, we suspect border zone infarcts may be even more prevalent than previously reported. Alternatively, the large amount of patients with steno-occlusive disease of the large brain-feeding arteries might have accounted for the larger amount of border zone infarcts in the current study. Border zone ischaemia may occur due to hypoperfusion, either due to reduced cardiac output or decreased cerebral perfusion pressure in patients with an obstructive carotid artery lesion and poor collaterals. However, ischaemia may also occur to thromboemboli, especially as these areas of relatively lower perfusion are more susceptible to ischaemia after thromboembolic attacks due to decreased washout.25 In a previous study on patients with stroke presenting in the emergency room, a perfusion territory mismatch between the assumed and measured perfusion territory of cerebral infarcts was observed in only 11% of the patients, as compared with the 19% seen in the present study.26 We hypothesise that in the current patient group with a large percentage of patients with steno-occlusive disease of the large brain-feeding arteries, the presence of collateral flow resulted in a larger percentage of changes in perfusion territories.
Cerebral infarct location with respect to cerebral perfusion territory is currently assessed in clinical practice by combining all available MRI information, including MRA. MRA can provide important clues for determining the perfusion territories of the brain-feeding arteries. When an ICA occlusion is, for instance, seen on the MRA and is accompanied by only a small infarct distal to this occlusion, the presence of collateral perfusion from the contralateral ICA and BA can be anticipated. The presence of this collateral flow via primary collateral pathways (ie, the circle of Willis) can be further strengthened by the presence and diameter of the anterior collateral flow route (A1 segments and the anterior communicating artery) and the posterior collateral flow route (ipsilateral P1 segment and the posterior communicating artery). External carotid artery and leptomeningeal collateral flow contributions are however difficult to assess based on MRA images alone.
In addition to the assessment of potential collateral flow, anatomical variants of the circle of Willis can also be determined with MRA. For a subgroup of infarcts, the presence of anatomical variants of the circle of Willis will have a direct effect on the perfusion territory of a cerebral infarct; for instance, in case of a PCA infarct in a patient with a fetal-type configuration, or in case of an ACA infarct in a patient with an absent A1 segment. Angiography however depicts the presence of vasculature and does not provide information on flow direction or perfusion at the brain tissue level. Our study shows that by extracting information from the anatomical and angiographic imaging exclusively, still 19% of infarcts were misclassified. Changes in assumed and measured perfusion territories of cerebral infarcts were observed for cortical, subcortical and larger (subcortical+cortical) infarcts. Although other causes for subcortical infarcts (eg, small vessel disease) cannot be ruled out, no specific subgroup of infarct locations was found to have a high prevalence of change in the attributed perfusion territories.
The current study population represents patients referred to a tertiary hospital for further follow-up and secondary prevention after a TIA or non-disabling minor ischaemic stroke. As such the study population is a heterogeneous group, which is reflected in the demographic and clinical patient characteristics. Most patients were referred and underwent MRI within 2 days of symptom onset. Many patients were evaluated in the same week. Some patients were only referred after several weeks and few after months. This large span in the time of presentation to imaging in combination with the clinical setting as tertiary referral centre for stroke might account in part for the diversity of the study population. Furthermore, there are a relatively large number of patients with a carotid artery stenosis or occlusion. The current results therefore might not be directly applicable to the general public. At the same time, the currently employed method using T-ASL MRI readily provides perfusion territory information and may contribute to further personalised treatment of patients not necessarily referred to a specialised centre.
A limitation of the current study is that we did not compare our T-ASL findings with catheter angiography studies. Yet, a previous study showed that T-ASL measurements of (collateral) perfusion are in good agreement with the catheter angiography-based collateral perfusion measurements.27 The employed planning-free VE p-CASL sequence is furthermore reported to be robust and accurate.11 12 Although most MR vendors are currently implanting ASL perfusion imaging for clinical use, T-ASL is still not widely available. The T-ASL MR images were acquired only at a single time point. We cannot exclude that some of the infarcts were pre-existent. We cannot exclude that the perfusion territories have changed over time in patients with large artery disease of the brain-feeding arteries, such as at the time of ischaemic onset preceding the infarction, which might potentially affect the territorial classification of an individual infarct. In the current study, we did not determine the stroke aetiology or investigate whether our imaging findings could potentially help establish the aetiological classification. Nevertheless, the imaging set-up employed in this study, with a combination of anatomical, angiographic and T-ASL MRI, provides a valuable tool for determining symptomatic brain-feeding arteries in patients with ischaemic stroke and warrants further investigation in a longitudinal setting to determine if it can influence the determination of stroke aetiology and clinical treatment.
In conclusion, territorial perfusion imaging provides important additional information for classifying the symptomatic brain-feeding artery in patients with cerebral ischaemia and steno-occlusive lesions in the brain-feeding arteries when compared with expert evaluation of standard MRI and MRA.
Footnotes
Contributors: All authors contributed in writing the work. JH and LJLDC collected and scored the data. NSH performed the analysis.
Funding: This work was supported by the Dutch Heart Foundation under grant number 2013T047 (RB). JH received support from the Netherlands Organization for Scientific Research (NWO) under grant n°91712322, the European Research Council under grant agreement n°637024 and the Dutch Heart Foundation under grant number 2010B274. N.S. Hartkamp received support from the Dutch Heart Foundation under grant number 2010B274.
Competing interests: None declared.
Ethics approval: UMC Utrecht Institutional Review Board.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: All data including territorial perfusion maps are available to interested third parties upon request per email to the corresponding author.
References
- 1.Hendrikse J, Petersen ET, van Laar PJ, et al. . Cerebral border zones between distal end branches of intracranial arteries: MR imaging. Radiology 2008;246:572–80. 10.1148/radiol.2461062100 [DOI] [PubMed] [Google Scholar]
- 2.Krabbe-Hartkamp MJ, van der Grond J, de Leeuw FE, et al. . Circle of Willis: morphologic variation on three-dimensional time-of-flight MR angiograms. Radiology 1998;207:103–11. 10.1148/radiology.207.1.9530305 [DOI] [PubMed] [Google Scholar]
- 3.Hendrikse J, van Raamt AF, van der Graaf Y, et al. . Distribution of cerebral blood flow in the circle of Willis. Radiology 2005;235:184–9. 10.1148/radiol.2351031799 [DOI] [PubMed] [Google Scholar]
- 4.Hendrikse J, Petersen ET, Chng SM, et al. . Distribution of cerebral blood flow in the nucleus caudatus, nucleus lentiformis, and thalamus: a study of territorial arterial spin-labeling MR imaging. Radiology 2010;254:867–75. 10.1148/radiol.09090284 [DOI] [PubMed] [Google Scholar]
- 5.van Laar PJ, Hendrikse J, Klijn CJM, et al. . Symptomatic carotid artery occlusion: flow territories of major brain-feeding arteries. Radiology 2007;242:526–34. 10.1148/radiol.2422060179 [DOI] [PubMed] [Google Scholar]
- 6.Wolf RL, Detre JA. Clinical neuroimaging using arterial spin-labeled perfusion magnetic resonance imaging. Neurotherapeutics 2007;4:346–59. 10.1016/j.nurt.2007.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van Swieten JC, Koudstaal PJ, Visser MC, et al. . Interobserver agreement for the assessment of handicap in stroke patients. Stroke 1988;19:604–7. 10.1161/01.STR.19.5.604 [DOI] [PubMed] [Google Scholar]
- 8.Nederkoorn PJ, Mali WPTM, Eikelboom BC, et al. . Preoperative diagnosis of carotid artery stenosis: accuracy of noninvasive testing. Stroke 2002;33:2003–8. 10.1161/01.STR.0000021900.58396.44 [DOI] [PubMed] [Google Scholar]
- 9.Buckenham TM, Wright IA. Ultrasound of the extracranial vertebral artery. Br J Radiol 2004;77:15–20. 10.1259/bjr/70447093 [DOI] [PubMed] [Google Scholar]
- 10.Barnett HJ, Taylor DW, Eliasziw M, et al. . Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 1998;339:1415–25. 10.1056/NEJM199811123392002 [DOI] [PubMed] [Google Scholar]
- 11.Hartkamp NS, Helle M, Chappell MA, et al. . Validation of planning-free vessel-encoded pseudo-continuous arterial spin labeling MR imaging as territorial-ASL strategy by comparison to super-selective p-CASL MRI. Magn Reson Med 2014;71:2059–70. 10.1002/mrm.24872 [DOI] [PubMed] [Google Scholar]
- 12.Gevers S, Bokkers RP, Hendrikse J, et al. . Robustness and reproducibility of flow territories defined by planning-free vessel-encoded pseudocontinuous arterial spin-labeling. AJNR Am J Neuroradiol 2012;33:E21–5. 10.3174/ajnr.A2410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kansagra AP, Wong EC. Automated segmentation of multiple vascular territories from vessel encoded pseudo-continuous arterial spin labeling MRI data . Proceedings of the 17th Annual Meeting ISMRM Honolulu, USA, 2009;3652. [Google Scholar]
- 14.Wong EC, Kansagra AP. Mapping middle cerebral artery branch territories with vessel encoded pseudo-continuous ASL: sine/cosine tag modulation and data clustering in tagging efficiency space. Proceedings of the 16th Annual Meeting ISMRM Toronto, Canada, 2008;182. [Google Scholar]
- 15.Kansagra AP, Wong EC. Improved estimation of cerebral artery branch territories using cluster-based segmentation of vessel-encoded pseudocontinuous ASL data. Proceedings of the 20th Annual Meeting ISMRM Melbourne, Australia, 2012;0583. [Google Scholar]
- 16.Anbeek P, Vincken KL, van Osch MJP, et al. . Probabilistic segmentation of White matter lesions in MR imaging. Neuroimage 2004;21:1037–44. 10.1016/j.neuroimage.2003.10.012 [DOI] [PubMed] [Google Scholar]
- 17.Tatu L, Moulin T, Bogousslavsky J, et al. . Arterial territories of the human brain: cerebral hemispheres. Neurology 1998;50:1699–708. 10.1212/WNL.50.6.1699 [DOI] [PubMed] [Google Scholar]
- 18.Boongird A, Duangtongphon P. Variation of the recurrent artery of Heubner in human cadavers. J Med Assoc Thai 2009;92:643–7. [PubMed] [Google Scholar]
- 19.Cosson A, Tatu L, Vuillier F, et al. . Arterial vascularization of the human thalamus: extra-parenchymal arterial groups. Surg Radiol Anat 2003;25:408–15. 10.1007/s00276-003-0153-7 [DOI] [PubMed] [Google Scholar]
- 20.Rothwell PM, Eliasziw M, Gutnikov SA, et al. . Endarterectomy for symptomatic carotid stenosis in relation to clinical subgroups and timing of surgery. Lancet 2004;363:915–24. 10.1016/S0140-6736(04)15785-1 [DOI] [PubMed] [Google Scholar]
- 21.den Hartog AG, Moll FL, van der Worp HB, et al. . Delay to carotid endarterectomy in patients with symptomatic carotid artery stenosis. Eur J Vasc Endovasc Surg 2014;47:233–9. 10.1016/j.ejvs.2013.12.013 [DOI] [PubMed] [Google Scholar]
- 22.Jorgensen L, Torvik A. Ischaemic cerebrovascular diseases in an autopsy series. 2. Prevalence, location, pathogenesis, and clinical course of cerebral infarcts. J Neurol Sci 1969;9:285–320. [DOI] [PubMed] [Google Scholar]
- 23.Momjian-Mayor I, Baron JC. The pathophysiology of watershed infarction in internal carotid artery disease: review of cerebral perfusion studies. Stroke 2005;36:567–77. 10.1161/01.STR.0000155727.82242.e1 [DOI] [PubMed] [Google Scholar]
- 24.Mangla R, Kolar B, Almast J, et al. . Border zone infarcts: pathophysiologic and imaging characteristics. Radiographics 2011;31:1201–14. 10.1148/rg.315105014 [DOI] [PubMed] [Google Scholar]
- 25.Riba-Llena I, Koek M, Verhaaren BF, et al. . Small cortical infarcts: prevalence, determinants, and cognitive correlates in the general population. Int J Stroke 2015;10(Suppl A100):18–24. 10.1111/ijs.12543 [DOI] [PubMed] [Google Scholar]
- 26.Hendrikse J, Petersen ET, Chèze A, et al. . Relation between cerebral perfusion territories and location of cerebral infarcts. Stroke 2009;40:1617–22. 10.1161/STROKEAHA.108.539866 [DOI] [PubMed] [Google Scholar]
- 27.Chng SM, Petersen ET, Zimine I, et al. . Territorial arterial spin labeling in the assessment of collateral circulation: comparison with digital subtraction angiography. Stroke 2008;39:3248–54. 10.1161/STROKEAHA.108.520593 [DOI] [PubMed] [Google Scholar]