Abstract
Introduction
Melatonin has been studied in headache disorders. Amitriptyline is efficacious for migraine prevention, but its unfavourable side effect profile limits its use.
Methods
A randomised, double-blind, placebo-controlled study was carried out. Men and women, aged 18–65 years, with migraine with or without aura, experiencing 2–8 attacks per month, were enrolled. After a 4-week baseline phase, 196 participants were randomised to placebo, amitriptyline 25 mg or melatonin 3 mg, and 178 took a study medication and were followed for 3 months (12 weeks). The primary outcome was the number of migraine headache days per month at baseline versus last month. Secondary end points were responder rate, migraine intensity, duration and analgesic use. Tolerability was also compared between groups.
Results
Mean headache frequency reduction was 2.7 migraine headache days in the melatonin group, 2.2 for amitriptyline and 1.1 for placebo. Melatonin significantly reduced headache frequency compared with placebo (p=0.009), but not to amitriptyline (p=0.19). Melatonin was superior to amitriptyline in the percentage of patients with a greater than 50% reduction in migraine frequency. Melatonin was better tolerated than amitriptyline. Weight loss was found in the melatonin group, a slight weight gain in placebo and significantly for amitriptyline users.
Conclusions
Melatonin 3 mg is better than placebo for migraine prevention, more tolerable than amitriptyline and as effective as amitriptyline 25 mg.
Keywords: MIGRAINE
Introduction
Migraine is a chronic debilitating neurological condition affecting 12–20% of the population worldwide.1 Preventive treatments are available, decreasing the number and severity of headache attacks, and improving health outcomes and quality of life; half of the patients show 50% reduction in attack frequency.2 Although migraine prophylaxis guidelines from North American, South American and European societies are available, only 3–5% of patients receive adequate preventive therapy.3
Public surveys report that migraineurs are among the most dissatisfied patients.4 5 About half of the patients with migraine stop seeking care for their headaches, partly because of their side effect profile.6 Most guidelines recommend topiramate, divalproex/sodium valproate, propranolol and metoprolol as having the highest level of evidence.7 Newer effective and tolerable options for migraine prophylaxis are necessary to reduce this gap and improve patients' quality of life.
Melatonin use in migraine prevention is supported by several biological effects.8 Melatonin levels are decreased in patients with migraine; it has been studied for migraine prophylaxis with conflicting results.9–11 We aimed to study the effect of melatonin in a double-blind, placebo controlled trial with an active comparator.
Methods
Patients
Patients with migraine were eligible for the study if they met inclusion criteria: age of 18–65 years; migraine with or without aura criteria according to the International Classification of Headache Disorders, third edition, β-version12 for at least 1 year, age of onset before 50 years, at least three migraine headache attacks or four migraine headache days (defined as any occurrence of migraine headache pain of at least 30 min in duration with acute treatment) per month, presents with migraine or non-migraine headache attacks <15 days per month during each of the 3 months prior to the screening visit and the reference period. Migraine diagnosis was performed by a trained neurologist headache specialist. Women were eligible if they were unable to bear children or if they were not pregnant and using adequate contraception.
Patients were excluded if they had a history of psychiatric disorder (in the past or present); ergotamine, triptan, opioid, or combination medication intake for >10 days per month, or simple analgesic intake for >15 days per month for >3 months; in use of preventive medications such as β-blockers, tricyclic antidepressants, calcium channel blockers, antiepileptic drugs, bupropion, serotonergic norepinephrine reuptake inhibitors; and were unable to discontinue the treatment; had previously taken melatonin, amitriptyline or agomelatine; or had uncontrolled hypertension (ie, sitting systolic blood pressure >160 mm Hg or sitting diastolic blood pressure >90 mm Hg) at the screening visit or at randomisation. Data collection was performed after patient compliance and signing of informed consent. Patients were recruited from the general population, primary care, advertising and social media. Those interested in participating in the trial called and were asked screening questions. If inclusion and exclusion criteria were met, they were invited for a screening visit.
Patients’ involvement
Patients/service users/carers/laypeople were not involved in the study design. Outcome measures were defined by scientific criteria, designed to better meet patients' preferences, priorities and experience. Patients were not involved in recruitment and conducting the study. Results will be disseminated to patients/carers/laypeople by publication in the clinicaltrials.org database and to press/social media. Burden of intervention, for example, side effects were assessed. The research question and outcome measures were developed to meet patients' needs.
Study design
The study was conducted in a randomised, multicentre, parallel-group design. Melatonin 3 mg was compared with amitriptyline 25 mg and placebo. Randomisation was performed centrally with the use of randomisation lists with randomly permuted block lengths stratified according to centre. Patients, treating clinicians and the outcome assessor were blinded. Study medications were also blinded and delivered to the investigators by the pharmacy which prepared the three study medications equally in design, shape, and colour.
The trial conformed to the Declaration of Helsinki, Good Clinical Practice guidelines and the International Organization for Standardization standards and was approved by the ethics committee for each participating centre. The trial was funded by FAPESP, Fundação de Amparo a Pesquisa de São Paulo, a Brazilian governmental funding agency without any role in manuscript preparation. The trial was registered at ClinicalTrials.gov number NCT01357031.
Procedures
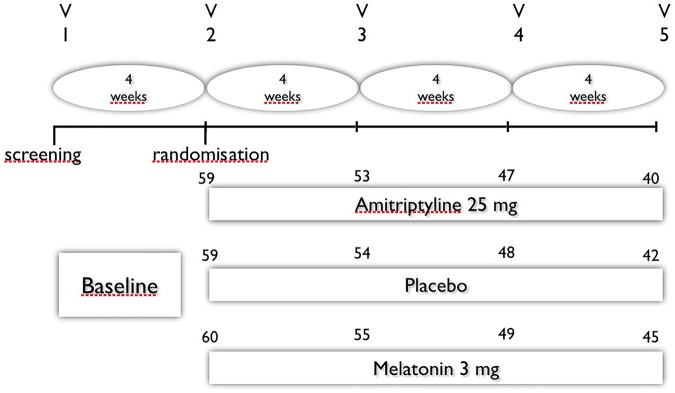
The study consisted of a 4-week period to established baseline measures followed by a 12-week treatment period. After eligibility had been determined, patients were randomised to treatment groups (figure 1).
Figure 1.
Study design.
Patients meeting eligibility criteria were randomised 1:1:1 to one of the three groups: placebo, melatonin 3 mg or amitriptyline 25 mg, all taken at bedtime. Use of acute migraine medication was permitted for breakthrough migraine attacks. Patients recorded information about migraine or non-migraine headache occurrence, mean migraine headache attack intensity, duration, analgesics taken, (type of medication, number of days of medication use, number of doses) and associated symptoms in a paper-based diary. Trained neurologists in headache abstracted the information, which was double-checked by another investigator and uploaded into a spreadsheet. Any migraine headache during at least 30 min was defined as a migraine headache day. The variables were collected from the diaries and defined at the end of the baseline period, and at the first (weeks 1–4), second (weeks 5–8) and third (weeks 9–12) months after treatment.
Outcome measures
Efficacy
The primary efficacy outcome measure was frequency in number of migraine headache days per month comparing baseline with the past 4 weeks of treatment. Secondary end points included reduction in migraine intensity, attack duration, number of analgesics used and percentages of patients with greater than 50% reductions in migraine headache days.
Tolerability and safety
Patients were monitored by adverse events and vital signs to determined tolerability and safety. An adverse event was defined as any medical occurrence reported by a patient or noted by a clinician during the study, regardless of its suspected cause. It was recorded if it was considered to be related to study medication. Tolerability measures included the incidences of adverse events, including those that led to the premature withdrawal of the study and serious adverse events (defined as death, disability or incapacity; were life-threatening; or required hospitalisation). Adverse events data were summarised for the safety population, defined as randomised patients who were administered at least one dose of the study medication.
Statistical analysis
Sample size calculation was based on previous trials. A 20% difference between active drug and placebo response was assumed. The randomisation ratio of 1:1:1 for placebo, and the two treatment groups, 59 participants in each groups were determined to provide 80% power to detect a significant difference in the primary endpoint.
This estimate was based on a two-sided analysis of variance (ANOVA), an α level of 0.05 and an SD of 4.0. Efficacy data were analysed for the intention-to-treat population, defined as randomised patients who received at least one dose of the study medication and provided at least one postbaseline efficacy assessment. No interim analysis was planned. Missing data were analysed by three methods. The first method extended the calendar earlier into the treatment period until 28 days of non-missing data contributed to the count of migraine headache days. The second method proportionately adjusted the number of migraine headache days (multiplied by 28 and divided by the number of non-missing days). The third method treated all missing days as non-migraine headache days (used for the primary end point). An analysis of covariance (ANCOVA) model was used to test the null hypothesis of no difference between placebo and the average of the values for the three groups. Results were summarised using the adjusted mean and SE for each treatment group, a 95% CI for the change from baseline for each treatment group, a model estimate of the difference between each active treatment group and placebo, a 95% CI for the difference, and an associated p value and adjusted p value for the difference. Analysis of the primary end point was carried out using a combination of a sequential method and a Hochberg procedure to maintain the experiment-wise α level of 0.05.
Results
Patients
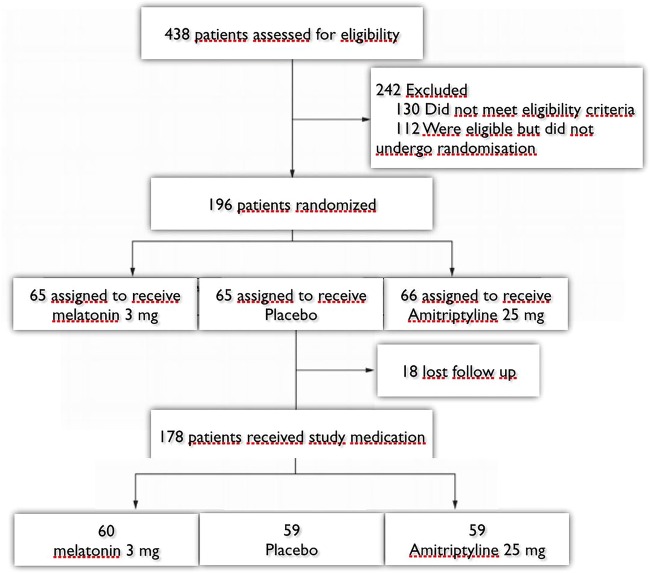
The number of patients randomised to treatment was 196 after 438 were recruited and assessed for eligibility. Eighteen randomised patients were excluded from the study, the analysis was performed in the remaining completed cases, 178 patients (59 placebo, 60 melatonin and 59 amitriptyline. Between 69% and 75% of patients completed the study in the treatment groups. Adverse events occurrence was the most common reason for premature withdrawal for all randomised patients (figure 2).
Figure 2.
Study enrolment and randomisation.
Treatment groups presented with similar demographics and baseline clinical characteristics (table 1). There were no significant differences in all variables.
Table 1.
Characteristics of study patients at baseline and of completers at the end of the trial
| Characteristic | Placebo (n=59) | Amitriptyline (n=59) | Melatonin (n=60) |
|---|---|---|---|
| Age—year (SD) baseline/end of trial | 36.6 (13.7)/36.1 (13.2) | 37.2 (11.2)/36.9 (13) | 36.9 (10.1) 36.5 (12.1) |
| Sex—N (%) women baseline/end of trial | 45 (76.3)/32 (76.2) | 44 (74.6)/30 (75) | 44 (73.3)/33 (73.3) |
| BMI baseline/end of trial, kg/m2 | 24.6 (4.0)/24.9 (3.8) | 23.9 (4.3)/24.3 (4.1) | 24.3 (4.9)/24.1 (4.7) |
| History of migraine—years (SD) baseline/end of trial | 20.2 (10.6)/21.1 (9.6) | 24.1 (9.1)/23.6 (9.5) | 23.2 (11.0)/21 (9.8) |
| Headache frequency (number of headache days)* | 7.3 (3.1) | 7.2 (2.5) | 7.3 (2.8) |
| Mean attack duration*—hours (SD) | 18.7 (17.3) | 16.7 (12.0) | 18.1 (13.8) |
| Mean headache intensity (0–10)* | 6.6 (1.4) | 7.0 (2.1) | 7.1 (1.9) |
| Aura—N (%) baseline/end of trial | 9 (15.2)/7 (17.5) | 10 (16.9)/7 (16.6) | 13 (21.7)/8 (17.7) |
| Number of analgesic doses taken per week* | 4.2 (1.3) | 4.6 (1.7) | 4.5 (1.9) |
*At baseline (4 weeks before start of study medication).
BMI, body mass index.
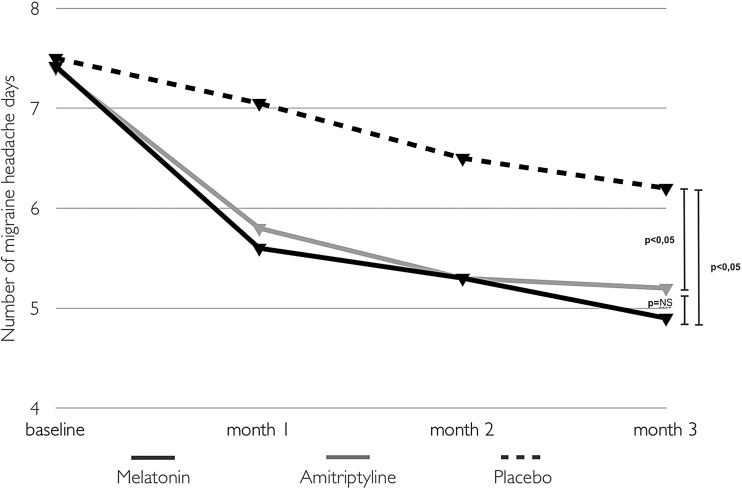
The primary efficacy end point was frequency in number of migraine headache days per month. Melatonin 3 mg and amitriptyline 25 mg efficiencies were superior to placebo (p<0.05) when comparing baseline with the last month of observation (table 2 and figure 3).
Table 2.
Observed means and differences (SD), effect sizes and CI for primary and secondary outcomes in baseline versus months 1, 2 and 3
| Placebo (n=59) | Amitriptyline (n=59) | Difference amitriptyline 25 mg vs placebo (95% CI) | Melatonin (n=60) | Difference melatonin 3 mg vs placebo (95% CI) | |
|---|---|---|---|---|---|
| Mean (SD)/difference from baseline | Mean (SD)/difference from baseline | RR (95% CI) | Mean (SD)/difference from baseline | RR (95% CI) | |
| Primary efficacy measure | |||||
| Number of migraine headache days | |||||
| Baseline | 7.3 (3.1) | 7.2 (2.5) | 7.3 (2.8) | ||
| Weeks 1–4 | 7.0 (2.9)/−0.3 | 5.8 (2.1)/−1.4 | −1.1 (−1.7 to −0.6) | 5.6 (2.0)/−1.7 | −1.4 (−2.1 to −0.8) |
| Weeks 5–8 | 6.6 (2.6)/−0.7 | 5.3 (2.4)/−1.9 | −1.2 (−1.6 to −0.8) | 5.3 (2.1)/−2.0 | −1.3 (−1.7 to −0.8) |
| Weeks 9–12 | 6.2 (2.5)/−1.1 | 5.0 (2.5)/−2.2 | −1.1 (−1.5 to −0.7)* | 4.6 (2.3)/−2.7 | −1.6 (−2.4 to −0.9)* |
| Secondary efficacy measures | |||||
| Mean headache intensity (0–10) | |||||
| Baseline | 6.6 (1.4) | 7.0 (2.1) | 7.1 (1.9) | ||
| Weeks 1–4 | 5.7 (3.2)/−0,9 | 5.2 (3.1)/−1.8 | −0.5 (−0.9 to −0.1) | 5.0 (2.8)/−2.1 | −0.7 (−1.2 to −0.2) |
| Weeks 5–8 | 5.4 (3.6)/−1.2 | 4.2 (3.4)/−2.8 | −1.2 (−1.5 to −0.9) | 4.3 (2.4)/−2.8 | −1.1 (−1.5 to −0.7) |
| Weeks 9–12 | 4.8 (3.3)/−1.8 | 3.5 (3.5)/−3.5 | −1.3 (−1.7 to −0.9)* | 3.6 (3.5)/−3.5 | −1.2 (−1.6 to −0.8)* |
| Number of analgesics | |||||
| Baseline | 4.2 (1.3) | 4.6 (1.7) | 4.5 (1.9) | ||
| Weeks 1–4 | 3.9 (1.4)/−0.3 | 4.1 (2.1)/−0.5 | −0.2 (−0.7 to 0.2) | 3.4 (2.0)/−1.1 | −0.8 (−1.1 to −0.5) |
| Weeks 5–8 | 3.8 (1.4)/−0.4 | 3.3 (1.9)/−1.3 | −0.9 (−1.4 to −0.4) | 3.2 (1.9)/−1.3 | −0.9 (−1.3 to −0.5) |
| Weeks 9–12 | 3.6 (1.2)/−0.6 | 3.2 (2.0)/−1.4 | −1.0 (−1.5 to −0.5)* | 2.9 (1.7)/−1.6 | −1.0 (−1.4 to −0.6)* |
| Mean attack duration (hours) | |||||
| Baseline | 18.7 (17.3) | 16.7 (12.0) | 18.1 (13.8) | ||
| Weeks 1–4 | 17.7 (16.2)/−1.0 | 13.2 (12.1)/−3.5 | −2.5 (−3.2 to −1.8) | 13.5 (12.4)/−4.6 | −3.6 (−4.7 to −2.5) |
| Weeks 5–8 | 16.8 (15.7)/−1.9 | 10.7 (9.7)/−6.0 | −4.1 (−4.6 to −3.6) | 12.2 (11.0)/−5.9 | −4.0 (−4.9 to −3.1) |
| Weeks 9–12 | 16.2 (15.3)/−2.5 | 9.8 (10.5)/−6.9 | −4.4 (−5.1 to −3.9)* | 10.9 (9.5)/−7.2 | −4.8 (−5.7 to −3.9)* |
*p<0.05.
RR; relative risk.
Figure 3.
Primary end point number of migraine headache days at baseline and at months 1, 2 and 3. NS, not significant.
For the secondary end points, melatonin and amitriptyline were more effective to placebo reducing the number of analgesics taken, migraine headache attacks duration and intensity. Melatonin and amitriptyline were equally effective for the primary end point, but for the secondary end point number of responders (patients with a higher than 50% improvement in headache frequency) melatonin was superior to amitriptyline (p<0.05) and placebo (p<0.01) (table 2 and figure 4). Outcomes were not related to duration of illness.
Figure 4.
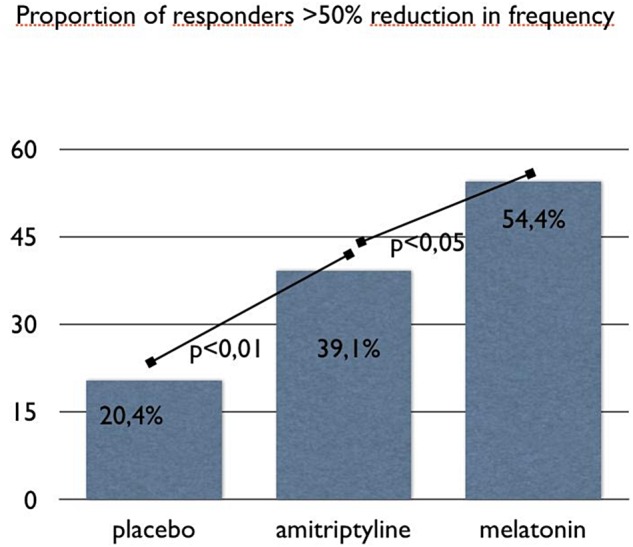
Proportion of responders (patients with a higher than 50% improvement in headache frequency, number of migraine headache days) comparing baseline vs last month of treatment.
Tolerability
Over the 3-month course of treatment, 77 adverse events were reported by 60 participants, 46 reports in the amitriptyline group, 16 in the melatonin group and 17 in the placebo group. No serious adverse events were observed. The majority of adverse events were either mild or moderate in intensity and occurred more commonly in the amitriptyline group compared with melatonin and placebo (p<0.03), whereas the melatonin and placebo groups had similar numbers (p value=not significant). The most common adverse events were daytime sleepiness, dry mouth, epigastralgia, weight gain and constipation (table 3). Blood pressure levels have not changed among groups. Patients were asked specifically about and reported no hypoglycaemic symptoms.
Table 3.
Number of patients reporting side effects in melatonin, amitriptyline and placebo groups
| Side effect | Melatonin (n=60) | Amitriptyline (n=59) | Placebo (n=59) |
|---|---|---|---|
| Sleepiness | 11 | 24 | 7 |
| Pruritus | 1 | 0 | 0 |
| Dizziness | 0 | 3 | 1 |
| Epigastralgia | 2 | 5 | 0 |
| Weight gain | 0 | 3 | 1 |
| Dry mouth | 1 | 6 | 1 |
| Insomnia | 0 | 1 | 0 |
| Constipation | 1 | 4 | 4 |
| Worsening headache | 0 | 0 | 3 |
We also evaluated weight variation in all groups. Surprisingly, patients taking melatonin had on average a weight reduction (mean 0.140±0.156 kg), whereas those taking placebo and amitriptyline had a weight gain (mean 0.432±0.247 kg, and 0.971±0.359 kg), respectively. Weight differences among groups were significantly different (figure 5).
Figure 5.
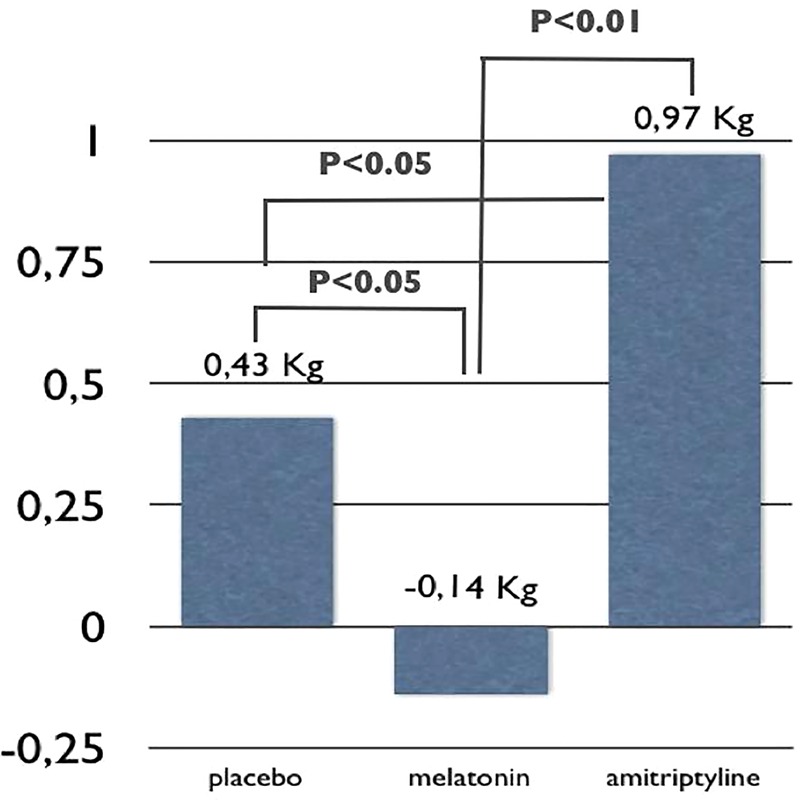
Mean weight variation comparing baseline with past 4 weeks of treatment in all groups.
Discussion
The results from this study support the efficacy and tolerability of melatonin 3 mg as a preventive therapy for migraine. Melatonin was more effective than placebo in the primary end point and all other end points studied. Although melatonin was as effective as amitriptyline 25 mg in the primary end point, in the secondary end point, proportion of patients who improved >50% in headache frequency, melatonin was superior to both placebo and amitriptyline. The placebo rate in our study was 20.4%, similar to the rates reported in the meta-analysis of pharmacological migraine prevention studies 22% (0.17% to 0.28%).
A pilot open-label study was published in 2004,9 showing efficacy and good tolerability of the same melatonin dose as was studied in this trial. A placebo controlled study comparing a different melatonin compound and dose (extended-release melatonin 2.0 mg, Circadin (Neurim Pharmaceuticals, Tel-Aviv, Israel)) with placebo showed negative results.10 Several methodological issues including the short trial length (only 8 weeks), high placebo response rate and low melatonin dosage and patient population limit this trial interpretation. Nevertheless, in this trial, the melatonin response rate was 44%, similar to several other positive migraine prophylaxis trials. The mean decrease in headache frequency was also similar to the most recent and well-designed preventive trials.11
We designed the study according to the International Headache Society guidelines for clinical trials,13 including an active comparator, in order to warrant a better blinding of treatment groups. Patients taking placebo not having sleepiness would probably guess their group to be placebo. Amitriptyline 25 mg is a lower than usually prescribed dose in the USA and studied in trials, but the usual dose in many countries, including Brazil. One study showed that topiramate and amitriptyline were equally effective with a mean daily dose of 74.8 and 76.5 mg, respectively; the amitriptyline group reported an unacceptable side effect profile, at least in our culture, for our patient population profile: dry mouth (35.5%), fatigue (24.3%), somnolence (17.8%), weight increase (13.6%) and dizziness (10.7%). Higher doses of amitriptyline could give better results but certainly a lot higher dropout rates in our population.14 Although our focus was to study melatonin efficacy, and the study was not designed for non-inferiority, this trial also gives support for the use of amitriptyline in lower doses for migraine prophylaxis.
Melatonin was more tolerable than amitriptyline and as tolerable as placebo. Weight loss was found in the melatonin group as opposed to a slight weight gain in placebo and a significant one in amitriptyline group. This is a very important and original finding that deserves special discussion. There is substantial experimental evidence in the literature indicating the role of melatonin in the control of food intake, energy balance and body weight. An inhibitory action of melatonin in preadipocytes differentiation into adipocytes, reducing the number of cells in the visceral adipose tissue has been demonstrated.15 Melatonin treatment reduced body weight gain, visceral adiposity, blood triglycerides and insulin resistance in a model of high-calorie diet-induced metabolic syndrome.16 Likewise, a single daily administration of melatonin decreased visceral fat in middle-aged mice,17 and after melatonin treatment aged rats showed weight reduction, preceded by an increase in insulin signalling in the central nervous system (CNS) and peripheral tissues.18 In addition, melatonin might have a direct anorexigenic action regulating hypothalamic pro-opiomelanocortin (POMC) gene expression.19 In ageing animals, melatonin and moderate exercise training induced a reduction in food intake associated with a reduction in body weight and amount of visceral adipose tissue depot.20 Melatonin should be considered as regulating the other side of energy balance increasing the energy expenditure by its ability to convert white adipose tissue into brown adipose tissue increasing its metabolic rate.21 The reduction in body weight of patients in the melatonin treated group is, to the best of our knowledge, the first demonstration of the putative effect of melatonin in body weight reduction in humans.
Melatonin mechanism of action in migraine prevention could be due to one of its several effects, including: membrane stabilisation, anti-inflammatory properties, inhibition of dopamine release, modulation of serotonin, gamma amino butyric acid (GAMA) and glutamate neurotransmission, scavenging toxic-free radicals and cerebrovascular regulation.22 Melatonin also potentiates opioid analgesia; therefore, it should be used with caution in patients taking and/or overusing opioids.23 Patients with diabetes and hypertensive patients should be monitored since melatonin may decrease blood pressure24 and glucose levels.25
Owing to its favourable side effect profile and efficacy, melatonin could be an option for patients sensitive to other drugs or with a preference for natural products. With the same efficacy level compared with other treatments and a low cost, melatonin should be a cost-effective treatment.
Different melatonin doses (lower and higher) should be studied, as well as its effect in other migraine types and comorbidities. The use of other chronobiotic agents, including melatonin analogues, could be tested in migraine prevention. Other trials in different populations and other latitudes should be conducted in the future.
Conclusion
Melatonin 3 mg is effective and better than placebo for migraine prevention. Melatonin is as effective as amitriptyline 25 mg in the primary end point, but better than amitriptyline in the secondary end point (50% responder rate). It is more tolerable than amitriptyline 25 mg.
Footnotes
Funding: Fundação de Amparo à Pesquisa do Estado de São Paulo (grant number 0854258-0 and 2014/50457-0).
Competing interests: None declared.
Ethics approval: CEP, CONEP.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Buse DC, Manack A, Serrano D, et al. Sociodemographic and comorbidity profiles of chronic migraine and episodic migraine sufferers. J Neurol Neurosurg Psychiatr 2010;81:428–32. 10.1136/jnnp.2009.192492 [DOI] [PubMed] [Google Scholar]
- 2.Silberstein SD, Holland S, Freitag F, et al. Evidence based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology 2012;78:1337–45. 10.1212/WNL.0b013e3182535d20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stewart WF, Shechter A, Lipton RB. Migraine heterogeneity. Disability, pain intensity, and attack frequency and duration. Neurology 1994;44(6 Suppl 4):S24–39. [PubMed] [Google Scholar]
- 4.Pascual J, Sanchez del Rio M, Jimenez MD, et al. [Satisfaction of the migraine patient attending neurology clinics: results of CIEN-mig project (II)]. Rev Neurol 2010;50:641–5. [PubMed] [Google Scholar]
- 5.Davies GM, Santanello N, Lipton R. Determinants of patient satisfaction with migraine therapy. Cephalalgia 2000;20:554–60. 10.1046/j.1468-2982.2000.00082.x [DOI] [PubMed] [Google Scholar]
- 6.Lipton RB, Stewart WF, Simon D. Medical consultation for migraine: results from the American Migraine Study. Headache 1998;38:87–96. 10.1046/j.1526-4610.1998.3802087.x [DOI] [PubMed] [Google Scholar]
- 7.Loder E, Burch R, Rizzoli P. The 2012 AHS/AAN guidelines for prevention of episodic migraine: a summary and comparison with other recent clinical practice guidelines. Headache 2012;52:930–45. 10.1111/j.1526-4610.2012.02185.x [DOI] [PubMed] [Google Scholar]
- 8.Peres MF, Masruha MR, Zukerman E, et al. Potential therapeutic use of melatonin in migraine and other headache disorders. Expert Opin Investig Drugs 2006;15:367–75. 10.1517/13543784.15.4.367 [DOI] [PubMed] [Google Scholar]
- 9.Peres MF, Zukerman E, da Cunha Tanuri F, et al. Melatonin, 3 mg, is effective for migraine prevention. Neurology 2004;63:757 10.1212/01.WNL.0000134653.35587.24 [DOI] [PubMed] [Google Scholar]
- 10.Alstadhaug KB, Odeh F, Salvesen R, et al. Prophylaxis of migraine with melatonin: a randomized controlled trial. Neurology 2010;75:1527–32. 10.1212/WNL.0b013e3181f9618c [DOI] [PubMed] [Google Scholar]
- 11.Peres MF. Melatonin for migraine prevention. Curr Pain Headache Rep 2011;15:334–5. 10.1007/s11916-011-0219-x [DOI] [PubMed] [Google Scholar]
- 12.Headache Classification Committee of the International Headache S. The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 2013;33:629–808. 10.1177/0333102413485658 [DOI] [PubMed] [Google Scholar]
- 13.Tfelt-Hansen P, Block G, Dahlof C, et al. Guidelines for controlled trials of drugs in migraine: second edition. Cephalalgia 2000;20:765–86. 10.1046/j.1468-2982.2000.00117.x [DOI] [PubMed] [Google Scholar]
- 14.Dodick DW, Freitag F, Banks J, et al. Topiramate versus amitriptyline in migraine prevention: a 26-week, multicenter, randomized, double-blind, double-dummy, parallel-group noninferiority trial in adult migraineurs. Clin Ther 2009;31:542–59. 10.1016/j.clinthera.2009.03.020 [DOI] [PubMed] [Google Scholar]
- 15.Alonso-Vale MI, Peres SB, Vernochet C, et al. Adipocyte differentiation is inhibited by melatonin through the regulation of C/EBPbeta transcriptional activity. J Pineal Res 2009;47:221–7. 10.1111/j.1600-079X.2009.00705.x [DOI] [PubMed] [Google Scholar]
- 16.Nduhirabandi F, Du Toit EF, Blackhurst D, et al. Chronic melatonin consumption prevents obesity-related metabolic abnormalities and protects the heart against myocardial ischemia and reperfusion injury in a prediabetic model of diet-induced obesity. J Pineal Res 2011;50:171–82. 10.1111/j.1600-079X.2010.00826.x [DOI] [PubMed] [Google Scholar]
- 17.Rasmussen DD, Boldt BM, Wilkinson CW, et al. Daily melatonin administration at middle age suppresses male rat visceral fat, plasma leptin, and plasma insulin to youthful levels. Endocrinology 1999;140:1009–12. [DOI] [PubMed] [Google Scholar]
- 18.Zanuto R, Siqueira-Filho MA, Caperuto LC, et al. Melatonin improves insulin sensitivity independently of weight loss in old obese rats. J Pineal Res 2013;55:156–65. 10.1111/jpi.12056 [DOI] [PubMed] [Google Scholar]
- 19.Puchalski SS, Green JN, Rasmussen DD. Melatonin effect on rat body weight regulation in response to high-fat diet at middle age. Endocrine 2003;21:163–7. [DOI] [PubMed] [Google Scholar]
- 20.Mendes C, Lopes AM, do Amaral FG, et al. Adaptations of the aging animal to exercise: role of daily supplementation with melatonin. J Pineal Res 2013;55:229–39. 10.1111/jpi.12065 [DOI] [PubMed] [Google Scholar]
- 21.Tan DX, Manchester LC, Fuentes-Broto L, et al. Significance and application of melatonin in the regulation of brown adipose tissue metabolism: relation to human obesity. Obes Rev 2011;12:167–88. 10.1111/j.1467-789X.2010.00756.x [DOI] [PubMed] [Google Scholar]
- 22.Peres MF. Melatonin, the pineal gland and their implications for headache disorders. Cephalalgia 2005;25:403–11. 10.1111/j.1468-2982.2005.00889.x [DOI] [PubMed] [Google Scholar]
- 23.Li SR, Wang T, Wang R, et al. Melatonin enhances antinociceptive effects of delta-, but not mu-opioid agonist in mice. Brain Res 2005;1043:132–8. 10.1016/j.brainres.2005.02.067 [DOI] [PubMed] [Google Scholar]
- 24.Grossman E, Laudon M, Yalcin R, et al. Melatonin reduces night blood pressure in patients with nocturnal hypertension. Am J Med 2006;119:898–902. 10.1016/j.amjmed.2006.02.002 [DOI] [PubMed] [Google Scholar]
- 25.Espino J, Pariente JA, Rodriguez AB. Role of melatonin on diabetes-related metabolic disorders. World J Diab 2011;2:82–91. 10.4239/wjd.v2.i6.82 [DOI] [PMC free article] [PubMed] [Google Scholar]