Abstract
Introduction
Femoroacetabular impingement (FAI) syndrome is increasingly recognised as a cause of hip pain. As part of the design of a randomised controlled trial (RCT) of arthroscopic surgery for FAI syndrome, we developed a protocol for non-operative care and evaluated its feasibility.
Methods
In phase one, we developed a protocol for non-operative care for FAI in the UK National Health Service (NHS), through a process of systematic review and consensus gathering. In phase two, the protocol was tested in an internal pilot RCT for protocol adherence and adverse events.
Results
The final protocol, called Personalised Hip Therapy (PHT), consists of four core components led by physiotherapists: detailed patient assessment, education and advice, help with pain relief and an exercise-based programme that is individualised, supervised and progressed over time. PHT is delivered over 12–26 weeks in 6–10 physiotherapist-patient contacts, supplemented by a home exercise programme. In the pilot RCT, 42 patients were recruited and 21 randomised to PHT. Review of treatment case report forms, completed by physiotherapists, showed that 13 patients (62%) received treatment that had closely followed the PHT protocol. 13 patients reported some muscle soreness at 6 weeks, but there were no serious adverse events.
Conclusion
PHT provides a structure for the non-operative care of FAI and offers guidance to clinicians and researchers in an evolving area with limited evidence. PHT was deliverable within the National Health Service, is safe, and now forms the comparator to arthroscopic surgery in the UK FASHIoN trial (ISRCTN64081839).
Trial registration number
ISRCTN 09754699.
Keywords: Hip, Exercise rehabilitation, Physiotherapy, Orthopaedics
Introduction
Femoroacetabular impingement (FAI) syndrome is a motion-related clinical hip disorder with a triad of symptoms, clinical signs and imaging findings.1 It represents a symptomatic premature contact between the proximal femur and the acetabulum.1–4 Typically, the morphology of the hip exhibits shapes that predispose to impingement, often described with the terms cam and pincer morphology.2 3 5 The epidemiology of cam and pincer morphology is not well defined but may be present in 30% of the general population.5 Not all patients with cam and/or pincer morphology develop FAI syndrome,6 but the treatment of those who do is controversial. Over the past 10 years, increasing numbers of patients have been treated for FAI syndrome with shape changing surgery, most frequently through hip arthroscopy.7 8 Surgery has been shown to provide improvements in patient symptoms,9 although patient expectations are not always met.10
It has been suggested that clinicians should be cautious in the use of surgery for FAI syndrome and that non-operative approaches should be considered.11–13 Patients with FAI syndrome have altered hip muscle strength, range of motion (ROM) and gait biomechanics, and these offer potential targets for treatment through physiotherapy.14–17 While many authors recognise the likely value of non-operative or conservative care, there is very little published guidance and evidence on how this care should be delivered.12 13
Given the uncertainty and lack of evidence about treatment for FAI syndrome, a randomised controlled trial (RCT) comparing hip arthroscopy and conservative care was proposed to guide future practice.11 18 In 2012, the UK National Institute of Health Research (UK NIHR) Health Technology Assessment programme (HTA) commissioned us to perform a feasibility and pilot study for an RCT to compare hip arthroscopy with ‘best conservative care’ for patients with FAI syndrome (FASHIoN HTA10/41/02).19 At the time, there was no established ‘best conservative care’,12 and we are not aware of any that has been published since. To design this trial, we needed to develop a suitable conservative care protocol.
The aim of this study was to develop an agreed conservative treatment protocol for patients with FAI syndrome that was deliverable within the UK National Health Service (NHS), was safe, and that could be used in the planned RCT.
Methods
Study design
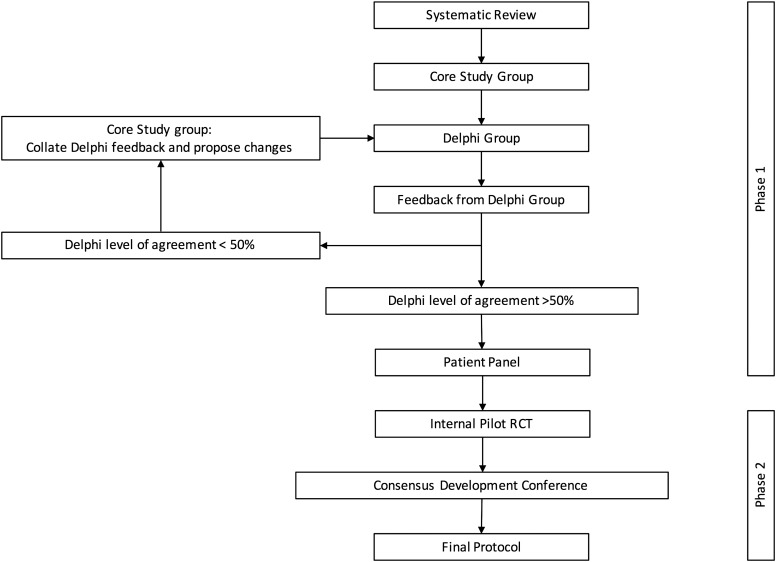
Research ethical approval was granted for this study (NHSREC11/WM/0389). In phase one, a non-operative treatment protocol for FAI syndrome was developed using established consensus methodology, guided by the principles described by the Medical Research Council for development of complex interventions.20 21 In phase two, the protocol was tested in an internal pilot RCT comparing conservative care versus arthroscopic hip surgery for FAI.22 Figure 1 presents a flow diagram of the protocol development process. This study formed part of the FASHIoN feasibility trial whose results, including aspects of this study, have been published.23
Figure 1.
Study flow diagram. RCT, randomised controlled trial.
Phase 1: consensus development
Given the lack of an agreed conservative care treatment protocol for FAI syndrome,12 we formed core and Delphi study groups in order to develop and agree on the treatment protocol.20 The core study group comprised two extended scope practitioner musculoskeletal physiotherapists with an interest in managing FAI syndrome (DR and IH), a senior academic research physiotherapist with expertise in musculoskeletal pain research (NEF) and an academic orthopaedic surgeon (PDHW). The core study group oversaw protocol development and provided the input required for consensus by nominal group technique.20 The use of this consensus methodology is reasonable given the lack of an established conservative care protocol.20 21
To form the Delphi study group, we took a targeted approach to sampling, using networks of physiotherapists most likely to be involved in the management of FAI syndrome. National advertisements were placed in the orthopaedic, rheumatology, pain and manual therapy electronic networks of the Chartered Society of Physiotherapy (iCSP) and in the magazine of the Chartered Society of Physiotherapists, Frontline. The advertisements invited physiotherapists to help develop a consensus for a conservative care protocol for FAI syndrome. Electronic invitations were also sent to physiotherapists in the USA and Australia known to the authors through previous collaborative work on FAI syndrome. To encourage a process of ‘snowball sampling’, physiotherapists were encouraged to invite colleagues with experience and interest in managing FAI syndrome to join the consensus development process.
A systematic review was conducted to identify any previously published protocols for conservative treatment of FAI syndrome.12 The first protocol was drafted using evidence gathered from this systematic review and was circulated via email to the Delphi study group. They completed a questionnaire asking whether they agreed or disagreed with the proposed protocol, and where appropriate provide comments and suggestions for improvement. Additional comments and treatment strategies were grouped into themes and tabulated. An agreement level of 50% for this Delphi consensus technique was used. If no consensus was evident, the core study group refined the protocol in the light of the feedback using a nominal group technique. The refined protocol was then recirculated to the Delphi group and the cycle repeated until a consensus of at least 50% was achieved.
Phase 1: patient panel
As part of the FASHIoN feasibility trial, a qualitative research study among an expert patient panel was undertaken to guide many aspects of the development of the RCT.23 One task for the panel was to name the conservative treatment arm of the RCT. Previous qualitative research has highlighted the importance of naming treatments in order to improve uptake and adherence with treatment, in particular within the context of RCTs.24 Further details of this qualitative research can be found in Griffin et al.23
Phase 2: protocol testing and refinement
Once adequate consensus on the conservative care protocol was reached, the protocol was implemented within a multicentre internal pilot RCT comparing arthroscopic surgery versus conservative care (FASHIoN feasibility study ISRCTN09754699). Since the pilot RCT was designed to be internal to a full RCT, there was no interim analysis of outcomes; the outcomes will be reported as part of the full RCT.22 25 The eligibility criteria for the RCT are listed in box 1.
Box 1. Eligibility criteria for a pilot randomised controlled trial.
Inclusion criteria
Aged ≥16; (no upper age limit)
Symptoms of hip pain - patients may also have symptoms of clicking, catching or giving way;
- Radiographic evidence of pincer- and/ or cam-type FAI on plain radiographs and cross-sectional imaging, defined as;
-
–Cam – an alpha angle >55°
-
–Pincer morphology – a lateral centre edge angle of >40° or a cross over sign on the anteroposterior radiograph of the pelvis
-
–
The treating surgeon believes that they would benefit from arthroscopic FAI surgery;
Able to give written informed consent and participate fully in the interventions.
Exclusion criteria:
Evidence of pre-existing osteoarthritis, defined as Tonnis grade >1, or more than 2 mm loss of superior joint space width on anteroposterior pelvic radiograph;
Previous significant hip pathology such as Perthes’ disease, slipped upper femoral epiphysis or avascular necrosis;
Previous hip injury such as acetabular fracture, hip dislocation or femoral neck fracture;
Previous shape change (open or arthroscopic) in the hip being considered for treatment.
FAI, femoroacetabular impingement.
All physiotherapists delivering the conservative care protocol were asked to complete a case report form (CRF) for each patient treated, which included details about the number, nature and duration of the patient contacts, the exercises prescribed and other treatments provided. Given that this was an internal pilot trial, all patients recruited were followed up for 1 year. Any adverse events (AEs) were collated from CRFs, hospital records and follow-up questionnaires. AEs were defined as any untoward medical occurrence in the RCT.
Phase 2: consensus development conference
After treating patients in the internal pilot RCT, physiotherapists delivering the protocol were invited to a consensus development conference chaired by NF to share their experiences of delivering the protocol and make suggestions for further amendments prior to the full RCT.
Results
Thirty-six physiotherapists responded and agreed to take part in the Delphi consensus process, 24 from the UK, 10 from the USA and 2 from Australia. All 36 had previously managed patients with FAI syndrome and included physiotherapists from the military, primary and secondary care, tertiary hip preservation services, extended scope practitioners, private practice and elite sport.
Phase 1: consensus development
The first protocol proposed and circulated to physiotherapists is summarised in online supplementary file A. The level of agreement with the first protocol among the 36 physiotherapists was below the 50% threshold. Details of the degree of consensus reached and a summary of the feedback from the first round of the Delphi exercise are summarised in online supplementary file B.
bjsports-2016-096368supp_A.pdf (37KB, pdf)
bjsports-2016-096368supp_B.pdf (61.3KB, pdf)
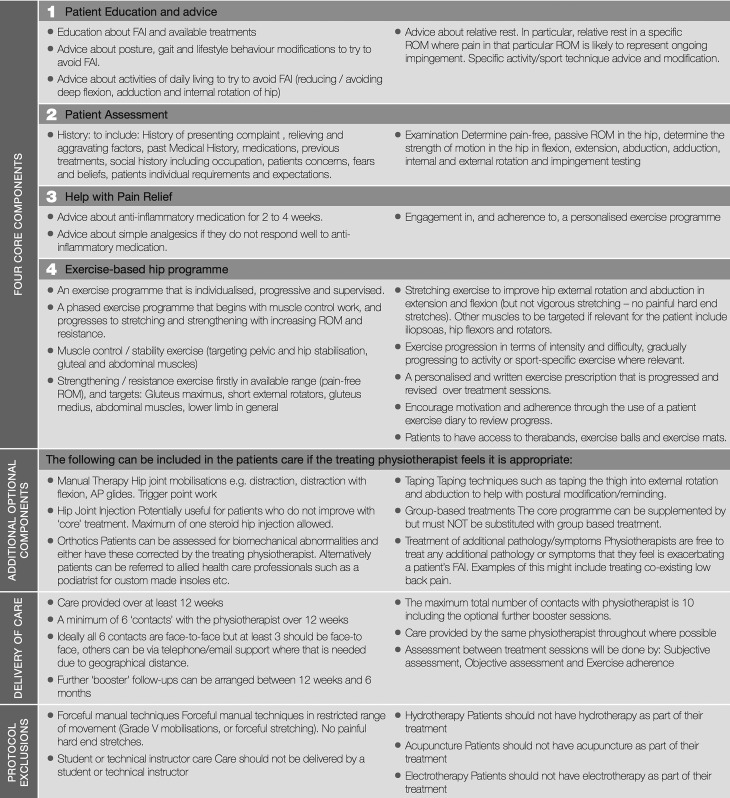
Using the additional comments made by the Delphi group, and drawing on available evidence and underpinning theory, the core study group derived a second protocol. This had four core components and four optional components, which are described in table 1.
Table 1.
Protocol components
| Core 1 | Patient assessment |
|
|
| Core 2 | Patient education and advice |
|
|
| Core 3 | Help with pain relief |
|
|
| Core 4 | Exercise-based hip programme |
|
|
| Optional 1 | Treat coexisting symptoms |
|
|
| Optional 2 | Orthotics |
|
|
| Optional 3 | Corticosteroid hip joint injection |
|
|
| Optional 4 | Manual Therapy |
|
FAI, femoroacetabular impingement; PHT, Personalised Hip Therapy; ROM, range of motion.
The initial round of responses suggested that patients should be seen over a longer period (the first draft protocol suggested 2–3 weeks26) and more frequently in order to optimise patient outcomes. Within the NHS, the typical number of treatment sessions given by physiotherapists to patients with musculoskeletal pain is three or four. Evidence suggests that better outcomes are achieved from exercise-based regimes when they are supervised and the contact between the supervisor and patient is increased.27 28 In order to allow more contact between physiotherapists and their patients, without increasing the burden of travel to clinic appointments, telephone and email contacts were also allowed to progress the exercise programme and to support patient adherence. The core study group decided that the protocol could be delivered over a 12-week period and a minimum of six treatment sessions, of which at least three should be face to face. The treatment sessions with physiotherapists were to be supplemented by patients continuing their individualised exercise programme at home. The duration of care was in keeping with established theory that suggests that physiological changes in muscle occur after a 12-week programme of exercise.29
The core study group agreed on the following protocol exclusions:
Painful hard end stretches. Although only mentioned by two physiotherapists in the initial questionnaire responses, there is some evidence to suggest that painful hard end stretches and forceful manual techniques in a restricted range of movement may be harmful.4
Group-based treatment was excluded to ensure that care was individualised.
Treatment by a technical or student instructor was excluded to ensure that care was delivered by qualified physiotherapists who had received training in the protocol.
In total, 30 (83%) of the original 36 physiotherapists responded and agreed with the second protocol and provided no additional suggestions for change. One did not respond and five disagreed with the second protocol and made further suggestions for change. These points were discussed among the core study group and the following further changes were made:
Allowing treatment to be delivered over 6 months. This was in response to concerns that the initial 12-week programme might be insufficient to correct what is likely to be a significant chronic biomechanical dysfunction. Further treatment sessions were also felt to help with patient adherence to the programme.27 28
The addition of taping techniques to help with postural modification and to remind patients of desired positions. Although only mentioned by one physiotherapist, it was noted that taping was a feature of the published literature.12 No specific protocol for taping was included; this was left to the discretion of the treating physiotherapist.
Inclusion of an exercise diary to help patients self-monitor their home exercise programme and provide feedback to physiotherapists to guide future exercise progression.
Given the level of agreement (83%), the core study group decided to use the second protocol with the modifications discussed above for implementation in the pilot RCT.
Phase 1: patient panel
Eighteen UK patients (8 female and 10 male) with FAI syndrome took part in the qualitative study to derive a name for the conservative care protocol, of whom 5 had been treated with conservative care and 13 with arthroscopy.23 They were asked to choose between four potential names which had been suggested by the core study group, with the option to suggest a different name if they wished.
Personalised Hip Therapy (HIP) appealed to and conveyed a positive message to patients. This combination emphasises that the protocol is an active intervention that differs from other conservative care regimes that patients may have previously tried.
Phase 2: testing and refinement
Forty-two patients were recruited to the internal pilot RCT across eight NHS hospitals. The baseline patient data are displayed in table 2. Twelve experienced musculoskeletal physiotherapists delivered PHT. Two physiotherapists were Band 6, six Band 7, and two Band 8; NHS bands reflect seniority, ranging from a newly qualified physiotherapist at Band 5 to the most senior and experienced physiotherapist at Band 8. They had previously treated a mean of 30 (range 3–90) patients with FAI syndrome. Of the 42 patients recruited in the pilot RCT, 21 were allocated to PHT. On average, PHT started 38 (range 12–76) days after randomisation, reflecting physiotherapy service waiting times in the NHS. Patients attended a mean of six sessions (SD 2.3). Treatment was judged to have been delivered in line with the PHT protocol in 13 (62%) patients. Reasons for deviation from the protocol included immediate postrandomisation crossover (n=1), patient decided they no longer required treatment (n=1), no CRF received (n=2) and insufficient number of treatment sessions (n=5). Clinical outcomes are not reported from this internal pilot RCT due to the ongoing nature of the full RCT where pilot data will be included in the main analysis (FASHION ISCTRN64081839). The only AE reported was muscle soreness at 6 weeks by 13 (62%) patients.
Table 2.
Baseline patient characteristics
| Characteristics | Summary data |
|---|---|
| Age (years)* | 33.4 (6.4) |
| Sex female: male | 6: 15 (29%) |
| Duration of symptoms (months)* | 30.9 (24.4) |
| UCLA score* | 3.6 (2.7) |
| iHOT33 score* | 31.4 (15.2) |
| SF12 PCS* | 31.1 (14.8) |
| SF12 MCS* | 46.4 (15.0) |
| EQ5D* | 0.58 (0.23) |
*mean (SD).
EQ5D, EuroQol 5 dimension questionnaire; iHOT33, internal hip outcome tool; MCS, mental component score; PCS, physical component score; SF12, short form 12; UCLA, University of California, Los Angeles activity score.
Phase 2: consensus development conference
A consensus development conference was held at the University of Warwick in May 2013 after 21 patients randomised to PHT were treated. Eight physiotherapists from eight sites attended and provided feedback and discussion about the PHT protocol, content and delivery. Collectively, these 8 physiotherapists treated 18 patients within the pilot RCT. The physiotherapists agreed that the PHT protocol worked well, but that they would like to change the number of treatment contacts and the overall duration of the protocol. As a result, the protocol was amended to include a minimum of 6 and a maximum of 10 contacts over a total period of 6 months. In addition, 3 further exercises were recommended and were added to the original selection of 21 exercises within the exercise template (see online supplementary file C).
An overview of the final agreed protocol is shown in figure 2 with the exercise template provided in online supplementary file C. The full PHT manual, used as a training aid for trial physiotherapists, is available in online supplementary file D.
Figure 2.
Personalised hip therapy summary. FAI, femoroacetabular impingement.
bjsports-2016-096368supp_C.pdf (678.8KB, pdf)
bjsports-2016-096368supp_D.pdf (411.2KB, pdf)
Discussion
We aimed to develop and undertake initial testing of a physiotherapist-led non-operative treatment protocol for patients with FAI syndrome that could be compared with arthroscopic surgery in a large pragmatic RCT. We combined results from a systematic review, two rounds of Delphi consensus, relevant literature and the experiences of physiotherapists treating patients with FAI syndrome within the internal pilot RCT, in order to develop the agreed treatment protocol, referred to as Personalised Hip Therapy.30 31 This PHT protocol provides guidance to clinicians and researchers in an area where evidence is limited.8 12 18
Exercise is an effective treatment for many types of musculoskeletal pain.32 33 PHT has many similarities to other non-operative treatment regimens including the EULAR and OARSI guidelines on hip and knee osteoarthritis. These also recommend a comprehensive assessment, education, lifestyle modification and exercise-based programme.34 35 However, these guidelines were unable to make specific exercise recommendations for hip OA due to a lack of evidence, although a mixed regime (quadriceps strengthening, aerobic capacity and flexibility training) was recommended in knee osteoarthritis by EULAR.34
As well as including aspects in common with other non-operative care protocols of hip disorders, PHT includes an exercise-based programme that aims to improve deficiencies in hip function (including muscle weaknesses and ROM) that have been highlighted in FAI syndrome.14 17 Through an individualised exercise-based programme, physiotherapists using PHT are able to target these deficiencies. A recent editorial highlighted what might be included in a non-operative care protocol for FAI syndrome.17 PHT includes all of these points, including hip-specific function and lower limb strengthening, core stability and postural balance exercises.
During the pilot RCT, only 62% of PHT treatments were judged to closely follow the protocol. This raises questions about the deliverability of PHT in the ‘real world’. However, some of the reasons for deviation were teething problems to be expected in a pilot trial. These included an immediate postrandomisation crossover (n=1), no completed CRF available (n=2) and an insufficient number of treatment sessions (n=5); in some circumstances, this may reflect patient improvement, resulting in discharge prior to receiving six sessions. Compliance with home exercises can be problematic;36 but physiotherapists were able to use an exercise diary to monitor patient adherence to the exercise programme at home and did not report any concerns. Muscle soreness was reported in 62% of patients, 6 weeks into the PHT programme. This is to be expected as part of an exercise-based regime as the muscles adapt to the increased demand. Reassuringly, this had resolved in all cases by 3 months follow-up. This is in keeping with similar exercise-based interventions used in RCTs for other musculoskeletal conditions.37–39 On balance, we believe that the results from the pilot RCT show that PHT is safe and deliverable in the ‘real world’ of the NHS. The overall fidelity of PHT is similar to other conservative care protocols used in RCTs,40 so it is also suitable for use in the planned pragmatic RCT.
Limitations of the PHT protocol include that it was developed based on the experiences of clinicians treating patients with FAI syndrome and not by targeting the deficiencies, observed in patients with FAI syndrome, reported in the literature.
Where conservative treatment of FAI syndrome is advocated, PHT gives clinicians a protocol for content and delivery. We do not yet know how effective PHT will be—only that it is based on the published literature, represents a consensus among experienced physiotherapists on ‘best conservative care’, and that it has at least been tested in a pilot trial and found to be deliverable and safe. Following this successful pilot RCT, the effectiveness of PHT versus arthroscopic surgery is being tested in the full UK FASHIoN trial (ISCTRN64081839), where the outcome measures are hip-related quality of life (iHOT33), general health (SF12 and EQ5D) and health economics.
Key messages .
Femoroacetabular impingement syndrome is increasingly recognised as a source of hip pain, especially in young adults.
A period of non-operative care is recommended, although this is poorly defined.
A protocol for a physiotherapy-led package of education, exercise and pain relieving techniques for femoroacetabular impingement syndrome called Personalised Hip Therapy is described for use in an RCT.
The package of care is deliverable within the UK National Health Service, is safe, and is acceptable to patients.
Acknowledgments
The FASHIoN feasibility trial, which was published in the Health Technology Assessment Journal (Griffin DR, Wall PD, Realpe A, et al. UK FASHIoN: Feasibility study of a randomised controlled trial of arthroscopic surgery for hip impingement compared with best conservative care in Health Technology Assessment 2016;20(32)), includes details of the Personalised Hip Therapy protocol reported in this study. The authors wish to acknowledge funding for this study from NIHR HTA, support from hospital Trusts, CLRNs and collaborating surgeons, physiotherapists and research associates, and the work of Ceri Jones, R&D manager at the lead site, University Hospital of Coventry and Warwickshire NHS Trust. Finally, the authors thank the patients who gave so generously of their time in the expert patient panel, and those who agreed to participate in the pilot RCT.
Footnotes
Contributors: PDHW, NEF and DRG contributed to the conception, design, analysis and interpretation of the work. EJD, IH, AR, RH and DR contributed to the acquisition, analysis and interpretation of the data. All authors contributed to the drafting of the manuscript and approved the final version.
Funding: This work was funded as part of the FASHIoN trial (UK NIHR HTA 10/41/02), for which DRG is the Chief Investigator. NEF, an NIHR Senior Investigator, was supported through an NIHR Research Professorship (NIHR-RP-011-015). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: NHS REC 11/WM/0389.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Griffin DR, Dickenson EJ, O'Donnell J, et al. . The 2016 Warwick Agreement on Femoroacetabular Impingement. Br J Sports Med 2016;50:1179. [DOI] [PubMed] [Google Scholar]
- 2.Beck M, Kalhor M, Leunig M, et al. . Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br 2005;87:1012–18. 10.1302/0301-620X.87B7.15203 [DOI] [PubMed] [Google Scholar]
- 3.Ganz R, Parvizi J, Beck M, et al. . Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 2003:112–20. 10.1097/01.blo.0000096804.78689.c2 [DOI] [PubMed] [Google Scholar]
- 4.Lavigne M, Parvizi J, Beck M, et al. . Anterior femoroacetabular impingement: part I. Techniques of joint preserving surgery. Clin Orthop Relat Res 2004;418:61–6. 10.1097/00003086-200401000-00011 [DOI] [PubMed] [Google Scholar]
- 5.Dickenson E, Wall PD, Robinson B, et al. . Prevalence of cam hip shape morphology: a systematic review. Osteoarthr Cartil 2016;24:949–61. 10.1016/j.joca.2015.12.020 [DOI] [PubMed] [Google Scholar]
- 6.Urwin M, Symmons D, Allison T, et al. . Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Dis 1998;57:649–55. 10.1136/ard.57.11.649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Montgomery SR, Ngo SS, Hobson T, et al. . Trends and demographics in hip arthroscopy in the United States. Arthroscopy 2013;29:661–5. 10.1016/j.arthro.2012.11.005 [DOI] [PubMed] [Google Scholar]
- 8.Reiman MP, Thorborg K. Femoroacetabular impingement surgery: are we moving too fast and too far beyond the evidence? Br J Sports Med 2015;49:782–4. 10.1136/bjsports-2014-093821 [DOI] [PubMed] [Google Scholar]
- 9.Philippon MJ, Briggs KK, Yen YM, et al. . Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: MINIMUM TWO-YEAR FOLLOW-UP. J Bone Joint Surg 2009;91:16–23. 10.1302/0301-620X.91B1.21329 [DOI] [PubMed] [Google Scholar]
- 10.Mannion AF, Impellizzeri FM, Naal FD, et al. . Fulfilment of patient-rated expectations predicts the outcome of surgery for femoroacetabular impingement. Osteoarthr Cartil 2013;21:44–50. 10.1016/j.joca.2012.09.013 [DOI] [PubMed] [Google Scholar]
- 11.Kemp JL, Crossley KM, Roos EM, et al. . What fooled us in the knee may trip us up in the hip: lessons from arthroscopy. Br J Sports Med 2014;48:1200–1. 10.1136/bjsports-2014-093831 [DOI] [PubMed] [Google Scholar]
- 12.Wall PD, Fernandez M, Griffin DR, et al. . Nonoperative treatment for femoroacetabular impingement: a systematic review of the literature. PM R 2013;5:418–26. 10.1016/j.pmrj.2013.02.005 [DOI] [PubMed] [Google Scholar]
- 13.Excellence NIoHaC. Arthroscopic femoro–acetabular surgery for hip impingement syndrome. NICE Guideline (IPG408), 2011. [Google Scholar]
- 14.Diamond LE, Dobson FL, Bennell KL, et al. . Physical impairments and activity limitations in people with femoroacetabular impingement: a systematic review. Br J Sports Med 2015;49:230–42. 10.1136/bjsports-2013-093340 [DOI] [PubMed] [Google Scholar]
- 15.Casartelli NC, Maffiuletti NA, Item-Glatthorn JF, et al. . Hip muscle weakness in patients with symptomatic femoroacetabular impingement. Osteoarthritis Cartilage 2011;19:816–21. 10.1016/j.joca.2011.04.001 [DOI] [PubMed] [Google Scholar]
- 16.Kennedy MJ, Lamontagne M, Beaulé PE. Femoroacetabular impingement alters hip and pelvic biomechanics during gait walking biomechanics of FAI. Gait Posture 2009;30:41–4. 10.1016/j.gaitpost.2009.02.008 [DOI] [PubMed] [Google Scholar]
- 17.Casartelli NC, Maffiuletti NA, Bizzini M, et al. . The management of symptomatic femoroacetabular impingement: what is the rationale for non-surgical treatment? Br J Sports Med 2016;50:511–12. 10.1136/bjsports-2015-095722 [DOI] [PubMed] [Google Scholar]
- 18.Wall PD, Brown JS, Parsons N, et al. . Surgery for treating hip impingement (femoroacetabular impingement). Cochrane Database Syst Rev 2014;(9):CD010796 10.1002/14651858.CD010796.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Programme HTA. HTA—10/41/02: UK FASHIoN: feasibility study of a randomised controlled trial of arthroscopic surgery for hip impingement compared with best conservative care. Secondary HTA—10/41/02: UK FASHIoN: feasibility study of a randomised controlled trial of arthroscopic surgery for hip impingement compared with best conservative care 2012. http://www.nets.nihr.ac.uk/projects/hta/104102
- 20.Murphy MK, Black NA, Lamping DL, et al. . Consensus development methods, and their use in clinical guideline development. Health Technol Assess 1998;2:i–iv, 1–88. [PubMed] [Google Scholar]
- 21.Craig P, Dieppe P, Macintyre S, et al. . Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337:a1655 10.1136/bmj.a1655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lancaster GA, Dodd S, Williamson PR. Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Pract 2004;10:307–12. 10.1111/j.2002.384.doc.x [DOI] [PubMed] [Google Scholar]
- 23.Griffin D, Wall P, Realpe A, et al. . UK FASHIoN: feasibility study of a randomised controlled trial of arthroscopic surgery for hip impingement compared with best conservative care. Health Technol Assess 2016;20:1–172. 10.3310/hta20320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Featherston K, Donovan JL. Random allocation or allocation at random? Patients’ perspectives of participation in a randomised controlled trial. BMJ 1998;317:1177–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Griffin DR, Dickenson EJ, Wall PD, et al. . Protocol for a multi-centre, parallel-arm, 12-month, randomised controlled trial of arthroscopic surgery versus conservative care for femoroacetabular impingement syndrome (FASHIoN). BMJ Open 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Emara K, Samir W, Motasem el E, et al. . Conservative treatment for mild femoroacetabular impingement. J Orthop Surg (Hong Kong) 2011;19:41–5. [DOI] [PubMed] [Google Scholar]
- 27.Fransen M, McConnell S. Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev 2008;(4):CD004376 10.1002/14651858.CD004376.pub2 [DOI] [PubMed] [Google Scholar]
- 28.Hayden JA, van Tulder MW, Malmivaara AV, et al. . Meta-analysis: exercise therapy for nonspecific low back pain. Ann Intern Med 2005;142:765–75. 10.7326/0003-4819-142-9-200505030-00013 [DOI] [PubMed] [Google Scholar]
- 29.Holm L, Reitelseder S, Pedersen TG, et al. . Changes in muscle size and MHC composition in response to resistance exercise with heavy and light loading intensity. J Appl Physiol 2008;105:1454–61. 10.1152/japplphysiol.90538.2008 [DOI] [PubMed] [Google Scholar]
- 30.Fairbank J, Frost H, Wilson-MacDonald J, et al. . Randomised controlled trial to compare surgical stabilisation of the lumbar spine with an intensive rehabilitation programme for patients with chronic low back pain: the MRC spine stabilisation trial. BMJ 2005;330:1233 10.1136/bmj.38441.620417.8F [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Frost H, Lamb SE, Robertson S. A randomized controlled trial of exercise to improve mobility and function after elective knee arthroplasty. Feasibility, results and methodological difficulties. Clin Rehabil 2002;16:200–9. [DOI] [PubMed] [Google Scholar]
- 32.Excellence NIoHaC. Osteoarthritis: care and management. NICE guidelines [CG177], 2014. [Google Scholar]
- 33.Excellence NIfHaC. Low back pain in adults: early management. NICE Guideline (CG88), 2009. [Google Scholar]
- 34.Fernandes L, Hagen KB, Bijlsma JW, et al. . EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann Rheum Dis 2013;72:1125–35. 10.1136/annrheumdis-2012-202745 [DOI] [PubMed] [Google Scholar]
- 35.Zhang W, Moskowitz RW, Nuki G, et al. . OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage 2008;16:137–62. 10.1016/j.joca.2007.12.013 [DOI] [PubMed] [Google Scholar]
- 36.Campbell R, Evans M, Tucker M, et al. . Why Don't patients do their exercises? Understanding non-compliance with physiotherapy in patients with osteoarthritis of the knee. J Epidemiol Community Health 2001;55:132–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van Baar M, Dekker J, Oostendorp RA, et al. . Effectiveness of exercise in patients with osteoarthritis of hip or knee: nine months’ follow-up. Ann Rheum Dis 2001;60:1123–30. 10.1136/ard.60.12.1123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Foley A, Halbert J, Hewitt T, et al. . Does hydrotherapy improve strength and physical function in patients with osteoarthritis—a randomised controlled trial comparing a gym based and a hydrotherapy based strengthening programme. Ann Rheum Dis 2003;62:1162–7. 10.1136/ard.2002.005272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fransen M, Nairn L, Winstanley J, et al. . Physical activity for osteoarthritis management: a randomized controlled clinical trial evaluating hydrotherapy or Tai Chi classes. Arthritis Res 2007;57:407–14. 10.1002/art.22621 [DOI] [PubMed] [Google Scholar]
- 40.French HP, Cusack T, Brennan A, et al. . Exercise and manual physiotherapy arthritis research trial (EMPART) for osteoarthritis of the hip: a multicenter randomized controlled trial. Arch Phys Med Rehabil 2013;94: 302–14. 10.1016/j.apmr.2012.09.030 [DOI] [PubMed] [Google Scholar]
- 41.Hunt D, Prather H, Hayes MH, et al. . Clinical outcomes analysis of conservative and surgical treatment of patients with clinical indications of prearthritic, intra-articular hip disorders. PM R 2012;4:479–87. 10.1016/j.pmrj.2012.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ganz R, Leunig M, Leunig-Ganz K, et al. . The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res 2008;466:264–72. 10.1007/s11999-007-0060-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Moulin DE. Systemic drug treatment for chronic musculoskeletal pain. Clin J Pain 2001;17:S86–93. 10.1097/00002508-200112001-00017 [DOI] [PubMed] [Google Scholar]
- 44.Bergman S. Management of musculoskeletal pain. Best Pract Res Clin Rheumatol 2007;21:153–66. 10.1016/j.berh.2006.10.001 [DOI] [PubMed] [Google Scholar]
- 45.Feeley BT, Powell JW, Muller MS, et al. . Hip injuries and labral tears in the national football league. Am J Sports Med 2008;36:2187–95. 10.1177/0363546508319898 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bjsports-2016-096368supp_A.pdf (37KB, pdf)
bjsports-2016-096368supp_B.pdf (61.3KB, pdf)
bjsports-2016-096368supp_C.pdf (678.8KB, pdf)
bjsports-2016-096368supp_D.pdf (411.2KB, pdf)