Abstract
Background:
Food aid programs are strategies that aim to improve nutritional status and to tackle food insecurity. This study aimed to evaluate the effect of a National Food Supplementary Program for Children on households’ food security.
Methods:
The study sample included 359 mothers of children aged 6–72 months under the coverage of the program in two provinces of Iran. Demographic and socioeconomic characteristics of the households and percentage of supplementary food items consumed by target child were assessed by a questionnaire and checklist. Data on household food security were collected by locally adapted Household Food Insecurity Access Scale at the baseline of the study and 6 months thereafter.
Results:
At the baseline, only 4.7% of families were food secure, while 43.5% were severely food insecure, and these proportions were changed to 7.9% and 38%, respectively (P < 0.001), at the end of the study. Odds of having worse food insecurity in households with medium and high wealth index was 65% and 87% lower than those with low wealth index, respectively (odds ratio [OR] = 0.35, 95% confidence interval [CI]: 0.2–0.61, and OR = 0.23, 95% CI: 0.12–0.43). Food sharing was common among more than 95% of the studied households. Mean maternal body mass index (BMI) increased significantly after 6 months (P < 0.001). However, there was no significant association between mother's BMI and household food security in the baseline and at the end of the study (P > 0.05).
Conclusions:
Findings show that the food supplementary program for children can also improve the household food security status. Further research is needed to assess other factors that affect the effectiveness of this kind of programs.
Keywords: Food security, food supplementary program, Iran, nutritional status
INTRODUCTION
Food insecurity at the household level is a public health, as well as a development problem, especially in low-income communities in both developed and developing countries.[1] A household is considered food insecure (FI) when there is limited or uncertain availability of nutritionally adequate and safe foods or limited or uncertain ability to acquire acceptable food in socially acceptable ways.[2] This situation is contributed to poor health and nutritional status of household members, including children.[3] Based on the UNICEF framework, household food insecurity is one of the underlying risk factors for child malnutrition.[4] Food aid programs in the form of in-kind food distribution, voucher, or cash transfer are considered as strategies to reduce poverty, increase household food consumption, and increase the use of preventive and curative health and nutrition services among low-income families.[5]
In Iran, about 20% of the population suffers from energy and protein insufficiency.[6] The Multidisciplinary Program for Improvement of Nutritional Status of Children in Iran (MuPINSC) was initiated nationwide aiming to improve the nutritional status of children under 5-year-old, especially those from socially or economically deprived families. It consists of two major sections: Collaborative and supportive. The “collaborative” section has an intersectoral approach and some parts of this section of the program are implementing, and this issue is not included in our discussion. The “supportive” section of the program however has a targeted approach. It provides monthly food supplements by in-kind food, vouchers, or electronic card (E-card) distribution for malnourished or growth mentally challenged children who live in low-income families. Families could buy approved food items by food vouchers or E-cards at authorized food stores. Households qualify for the program based on their economic status in addition to growth failure of the children. The monetary value of the food basket is approximately 16 US$ per child per month. Nearly, 74,000 children from low-income families were under the coverage of supportive section by late 2014. This study is a part of a comprehensive evaluation of MuPINSC which aimed to evaluate the effect of food distribution for the nourishment of malnourished or growth retarded children on households’ food security and maternal weight (data on the effect of the program on the children nutritional status will be presented elsewhere). It was hypothesized that distributing food rations for the nourishment of child could also affect the food security status of the family.
METHODS
This longitudinal study is a part of a comprehensive evaluation study on the national nutritional program and was conducted between June 2014 and March 2015 in two provinces of Iran; Semnan and Qazvin. The study sample included mothers of children aged 6–72 months who were under the coverage of supportive section of the MuPINSC. A sample size of 324 was estimated according to the minimum samples required for effectiveness evaluation of MuPINSC on child growth. This estimation was based on alpha set at 5%, power of 90%, and relative risk of 2.5 that with consideration to the attrition; the sample size was defined as 350 children and their mothers. Multistage random sampling procedure with proportional allocation was used for selecting the sample. Demographic and socioeconomic characteristics of households, including age, level of education, and occupation of mother and father (head of the household), as well as family size, expenditure and living condition, and some major assets, were assessed by a structured questionnaire through an interview with mothers. A household wealth index was used as a proxy indicator for socioeconomic status of households. Household's ownership of some selected assets, including television, refrigerator, freezer, oven, and automobile, and some facilities in the house such as electricity, kitchen, and tap water and family income were scored according to a previous study.[7] These scores were added up to make the total score. The total score was categorized into tertiles, with T1, T2, and T3 labeled as low, middle, and high wealth index, respectively.
Food security and anthropometric data were collected at the baseline (from June to September 2014) and 6 months thereafter (from November 2014 to March 2015). Between the two phase of data collection, families received a food basket for the nourishment of their child. Food security status of the household was assessed by locally adapted Household Food Insecurity Access Scale (HFIAS)[8] through a face-to-face interview with mothers. The scale is comprised 9 items with 4 frequency options that ask whether a specific condition associated with the experience of food insecurity ever occurred during the previous 30 days. Households were categorized as food secure (FS), mild FI, moderate FI, and severe FI according to their HFIAS. Change in food security status of each household at the end of the study was defined as “better” when the family's food security status had changed from each food insecurity category to the upper category or had become FS. It was defined as “worse” when the FS household had become FI or when different categories of food insecurity change to any lower level of food insecurity at the follow-up. Finally, it was defined as unchanged, when there was not any change in the household food security status after 6 months follow-up in comparison to the baseline.
A food checklist and a questionnaire were used to determine the percentage of consumption of different food items provided by the program by the target child or other family members.
Mother's weight and height were measured by a trained nutritionist at the baseline and at the end of the study. Body mass index (BMI) was calculated as weight (in kilogram) divided by height squared (in meter) and categorized into underweight (defined as BMI <18.5 kg/m2), normal weight (≥18.5 and <25 kg/m2), and overweight/obese (BMI ≥25 kg/m2).
Data were analyzed using the Stata (Version 11., Stata Corp, College Station, Texas) and SPSS software (Inc 2009, Version. 20.0. Armonk, NY: IBM Corp). All statistical tests were two-tailed, and statistical significance was accepted as P < 0.05. Chi-square and Kendall's tau-b analyses were used to explore the relations among food insecurity and households demographic characteristics and wealth index. Paired t-test conducted to evaluate the differences in maternal BMI and food security score at the baseline and at the end of the study. Ordinal logistic regressions were used to control for the effect of possible confounding factors.
RESULTS
The study sample included 359 mothers with the mean age of 32.3 ± 6.47 years, who had at least one child in the program. The sociodemographic characteristics of the studied households are presented in Table 1. More than half of the mothers were Fars (the major ethnicity in Iran), and about one-third were Azeri (Turkish speaking).
Table 1.
Sociodemographic characteristics of households (n=359)

Figure 1 presents the food security status of the household at the baseline and 6 months thereafter. Results showed that more than 80% of households at the baseline of the study suffered from moderate-to-severe food insecurity, while only 4.7% were FS. After 6 months, the proportion of FS families increased to 7.9%, and severe and mild food insecurity decreased from 43.5% and 13.1% to 38% and 11.6%, respectively. These changes were significant at the end of the study (P < 0.05) [Figure 1]. In more than half of the studies households, food security status did not change at the end of the study. Food security status of 19.3% and 28.2% of the studied household became worse and better, respectively, at the end of the study.
Figure 1.
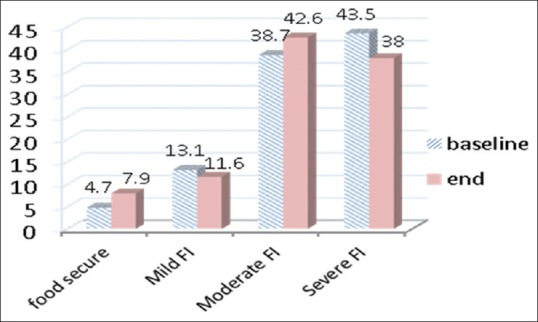
Food security status of the household at the baseline and 6 months thereafter. FI differences were significant at the end of the study: P < 0.05. FI: Food insecure
Table 2 presents household food security status stratified by characteristics of household at the end of the study. In the studied samples, more FI households were resident in urban areas, but the differences were not significant (P > 0.05). FI households had lower SES as measured by wealth index compared to FSs.
Table 2.
Household food security status according to socioeconomic characteristics and mothers’ weight status of the household (n=359)
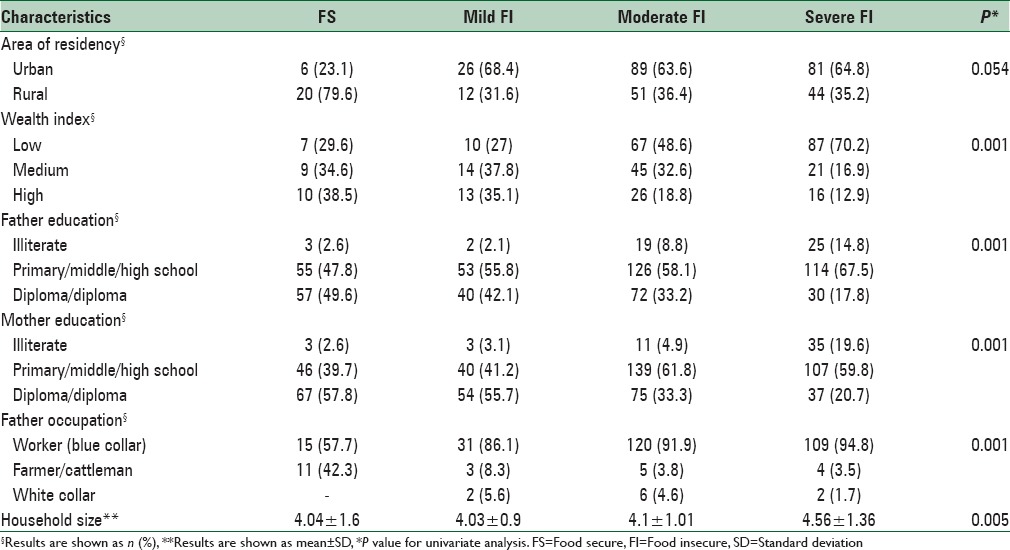
The education level of fathers and mothers in FI household was significantly lower than FSs. Moreover, household size was significantly smaller in FS households compared with FIs.
When the household and demographic characteristics were taken into account in the ordinal logistic regression analysis [Table 3], for each person increase in family size, the odds of having worse food insecurity, increased by 38% (odds ratio [OR] =1.38, 95% confidence interval [CI]: 1.1–1.73). The wealth index was inversely associated with food insecurity status. The likelihood of having worse food insecurity after 6 months in medium and high wealth index level was 65% and 87% lower than low wealth index, respectively (OR = 0.35, 95% CI: 0.2–0.61 and OR = 0.23, 95% CI: 0.12–0.43). In households where fathers were farmer/cattleman, the odds of worse food insecurity was 97–70% lower than those who were worker (OR = 0.09, 95% CI: 0.03–0.3) [Table 3].
Table 3.
Odds ratios (95% confidence interval) and P values of changing in the household food security status by socioeconomic characteristics using ordinal logistic regression modeling

In <5% of the studied children, (target) child was the only person who consumed supplementary foods; however, more than 95% of mothers reported intrahousehold food sharing practices and food items offered mostly consumed by all the members of the families. In almost half of the studied households, target child was the only person in the house consuming 75–100% of distributed milk and cake/biscuit and 20% butter, eggs, and canned Tuna. Honey, canned peas, sugar, and dates were not consumed by the child in nearly half of the cases. More than 50% of children consumed <50% of rice, vegetable oil, pasta, lentil, cheese, and soybean. Therefore, sharing was greatest for the latter group of food items and the lowest for milk and cake/biscuit.
Mean maternal BMI increased significantly after 6 months (P < 0.001). However, there was no significant association between mother's BMI and household food security in the baseline and at the end of the study (P > 0.05). The proportion of underweight mothers decreased from 6.3% to 3.8% and overweight/obesity increased from 54% to 62% after 6 months. The odds of mothers being overweight/obese increased by 80% in household with high wealth index (OR = 1.8, 95% CI: 1.04–3.34) [Table 4].
Table 4.
Odds ratios (95% confidence interval) and P values of changing in maternal body mass index categories by food security status at the end of the study, level of wealth index, and mothers’ educational level using ordinal logistic regression modeling

DISCUSSION
Based on the results, there was a high prevalence of different levels of food insecurity among the studied households under the coverage of the supportive section of MuPINSC at the beginning of the study. Considering the eligibility criteria of the program (having malnourished or growth retarded children who live in socioeconomically deprived family), this was well expected. After 6 months of food distribution among children, the frequency and the probability of severe food insecurity declined compared with the beginning of the study. It can be concluded that the supplementary food program may have had an effect on this trend. Considering the fact that the majority of the samples were low-income families who could not afford their essential foods, it may not be unusual that they share child's supplementary food between all the family members. Although nutrient intake of children was not measured, assessing the proportion of supplementary foods distributed and consumed by the target child showed that especially in the case of staple food items, i.e. rice, sugar, lentil, and oil, consumption by other family members was common. Food sharing is a common practice in low-income families.[9] This could dilute the effect of the program on the nutritional status of children in one hand (the results are not presented here), but at the same time could affect the food consumption of the other family member(s) and indirectly influence the household food security status or food access.
The findings indicated father's occupation and mother's educational level as the predictors of household food insecurity. This was in concordance with the previous studies.[10,11]
Food supplementary programs are useful policies that are widely used in low- and middle-income or even high-income countries for the improvement of nutritional status of malnourished children living in low-income single parent families or ethnic minorities.[11,12] The findings of this study confirm that such programs could also affect the household food security.
Petralias et al. examined the effect of school feeding program on children residing in low-socioeconomic areas on household food security status in Greece. Their result also showed that after 8 months intervention household food insecurity was also declined. They showed that for each additional month of participation in the program, the odds of a reduction in food insecurity score increased by 6.3%.[10]
Food assistance is one approach that government may use to increase food security level of low-income families. This effect can be strengthened if proper strategies on family empowerment and income generating activities are also in place. To ensure sustainable effects on food security status of the households, food aid programs need to put more emphasis on household wealth, education, occupation, and income generating strategies along with health and nutrition interventions.[13]
The present study showed that maternal BMI increased significantly at the end of the study, and the number of overweight/obese women increased. However, there was not any association between maternal BMI as a nutritional status and household food insecurity at the beginning and end of the study. However, the mean value of mother's BMI in the FS households was higher than FIs at the end of the study. These results were in line with Budd et al. study among low-income adults in Baltimore City. They did not find any significant association between BMI and food security status and concluded food insecurity was not a predictor of obesity among the low-income families.[14] On the other hand, a study by Adams et al. on women in California showed that food insecurity with hunger was associated with increased risk of obesity in minorities and risk of obesity was higher in black FI women.[15] Similar results were reported by Shariff and Khor in Malaysia.[16] These results were not in line with our studied samples that food insecurity was not significantly associated with maternal BMI.
Saaka and Osman in a study on food insecurity and its consequences on the nutritional status of mothers/child in Ghana showed that women in the FI households had lower BMI than women who were FS. Based on their report, BMI was not associated with household food insecurity as measured by HFIAS.[17] In addition, wealth index was associated with greater odds of overweight/obesity.[17] This result was in line with the result of our study that mothers in high wealth index household had higher odds of overweight/obesity. These conditions are consistent with what is commonly seen in developing countries where the individuals of higher socioeconomic classes are more at the risk of overweight and obesity.[17] This result could explain in the way that wealthy households are more likely of purchasing high dense energy foods and less exercise. In the other hand, low-income families may have less access to such kind of foods and may do more physical activity through their work.
This study is the first comprehensive evaluation study of MuPINSC in Iran. It is primarily limited by the nonexperimental design which makes it difficult to attribute the results to the effects of MuPINSC. However, longitudinal studies may be less vulnerable to self-selection bias than the cross-sectional studies. Moreover, we were not able to measure the dietary intake of children and their mothers which limited our analysis of food security only to food access. However, assessment of the percentage of distributed foods consumed by the target child and the other family members helped to have some estimation of how the food baskets may have had affected household food consumption.
CONCLUSIONS
This study showed that distribution of supplementary food for low-income malnourished children may improve household food security but could not eliminate food insecurity completely along with its main purpose for the improvement of nutritional status of malnourished or growth retarded children. More researches are needed to identify other factors that affect the effectiveness of supplementary foods on household food security and nutritional status of low-income families.
Financial support and sponsorship
The author(s) disclosed receipt of the financial support by the UNICEF office in IRAN under the cooperative agreement with NNFTRI for the research and with support from community nutrition Department of MOHME and health deputies in medical universities of Qazvin and Semnan.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We would like to thank Dr. Zahra Abdollahi and Mrs. Mina Minaee in the community Department of MOHME for their great support facilitating and enabling data gathering. The authors are grateful to Maryam Aghaian for data entering. We also are thankful to Mostafa Hosseini, Ali Aziz-Khani, and Atiyeh Razzazi who coordinated the surveys in Semnan and Qazvin Provinces.
REFERENCES
- 1.Furness BW, Simon PA, Wold CM, Asarian-Anderson J. Prevalence and predictors of food insecurity among low-income households in Los Angeles County. Public Health Nutr. 2004;7:791–4. doi: 10.1079/phn2004608. [DOI] [PubMed] [Google Scholar]
- 2.Rome Declaration on World Food Security and World Food Summit Plan of Action. World Food Summit, 13-17 November, Rome. 1996 [Google Scholar]
- 3.Mohamadpour M, Sharif ZM, Keysami MA. Food insecurity, health and nutritional status among sample of palm-plantation households in Malaysia. J Health Popul Nutr. 2012;30:291–302. doi: 10.3329/jhpn.v30i3.12292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.UNICEF. Strategy for Improved Nutrition of Women and Children in Developing Countries. A UNICEF Policy Review. New York: UNICEF; 1990. [Google Scholar]
- 5.Ruel MT, Alderman H Maternal and Child Nutrition Study Group. Nutrition-sensitive interventions and programmes: How can they help to accelerate progress in improving maternal and child nutrition? Lancet. 2013;382:536–51. doi: 10.1016/S0140-6736(13)60843-0. [DOI] [PubMed] [Google Scholar]
- 6.Ghassemi H. Food and Nutrition Security in Iran: Studies of Planning and Implementation Models. Final Report of Research project. Tehran: National Nutrition and Food Thechnology Research Institute; 1998. [Google Scholar]
- 7.Eini-Zinab H. Evaluation of Multivariate Indices and the Total Fertility Rate in Iran. Tehran: Asia-Pacific Population Research Center; 2013. [Google Scholar]
- 8.Mohammadi F, Omidvar N, Houshiar-Rad A, Khoshfetrat MR, Abdollahi M, Mehrabi Y. Validity of an adapted Household Food Insecurity Access Scale in urban households in Iran. Public Health Nutr. 2012;15:149–57. doi: 10.1017/S1368980011001376. [DOI] [PubMed] [Google Scholar]
- 9.Beckett AG. Acceptability and use of ready-to-use supplementary food as targeted ration in hiv program in haiti. Yale Medicine Thesis Digital Library. 2014 [Google Scholar]
- 10.Petralias A, Papadimitriou E, Riza E, Karagas MR, Zagouras AB, Linos A DIATROFI Program Research Team. The impact of a school food aid program on household food insecurity. Eur J Public Health. 2016;26:290–6. doi: 10.1093/eurpub/ckv223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carter MA, Dubois L, Tremblay MS, Taljaard M. Local social environmental factors are associated with household food insecurity in a longitudinal study of children. BMC Public Health. 2012;12:1038. doi: 10.1186/1471-2458-12-1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bartfeld J, Dunifon R. State-level predictors of food insecurity among households with children. J Policy Anal Manage. 2006;25:921–42. [Google Scholar]
- 13.Sraboni E, Malapit HJ, Quisumbing AR, Ahmed AU. Women's empowerment in agriculture: What role for food security in Bangladesh? World Dev. 2014;61:11–52. [Google Scholar]
- 14.Budd N, Liu D, Cuccia A, Jock B, Jeffries J, Frick K, et al. Food insecurity is not associated with body mass index (BMI) among low-income African American (AA) adult residents in Baltimore City. The FASEB J. 2013;27(No 1 Supplement):1054. [Google Scholar]
- 15.Adams EJ, Grummer-Strawn L, Chavez G. Food insecurity is associated with increased risk of obesity in California women. J Nutr. 2003;133:1070–4. doi: 10.1093/jn/133.4.1070. [DOI] [PubMed] [Google Scholar]
- 16.Shariff ZM, Khor GL. Obesity and household food insecurity: Evidence from a sample of rural households in Malaysia. Eur J Clin Nutr. 2005;59:1049–58. doi: 10.1038/sj.ejcn.1602210. [DOI] [PubMed] [Google Scholar]
- 17.Saaka M, Osman SM. Does household food insecurity affect the nutritional status of preschool children aged 6–36 months? Int J Popul Res 2013. 2013 doi: 10.1155/2013/304169. [Google Scholar]


