Abstract
Objectives
To review research and evidence-based resources on skin cancer prevention and early detection and their importance for oncology nurses.
Data Sources
Journal articles, federal reports, cancer surveillance data, behavioral surveillance data.
Conclusion
Most cases of skin cancer are preventable. Survivors of many types of cancer are at increased risk of skin cancers.
Implications for Nursing Practice
Oncology nurses can play an important role in protecting their patients from future skin cancer morbidity and mortality.
Keywords: skin cancer, melanoma, ultraviolet radiation, cancer survivors, skin cancer prevention, cancer prevention
Most skin cancers are preventable, but incidence rates continue to rise, leading the US Surgeon General to deem skin cancer “a major public health problem.”1 In the United States, nearly 5 million people are treated for skin cancer each year, at a cost of $8.1 billion.2 The three most common types of skin cancer, in order of incidence, are basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and melanoma. Cutaneous BCC alone is thought to be more common than any other cancer and can be disfiguring, but is generally treatable.3 Cutaneous SCC is less common than BCC but, in rare cases, can lead to death.4 Melanoma is less common than BCC and SCC, but is the skin cancer responsible for the most deaths, and is also the most common skin cancer for which incidence and mortality data are systematically tracked in the US.1 According to national cancer incidence data, invasive melanoma is among the 10 most common invasive cancers for both men and women in the US.5 In 2012, the most recent year for which national data are available, 67,753 people in the US were diagnosed with melanomas of the skin, and 9,251 people in the US died from the disease.5
Skin cancer incidence has been increasing. The number of persons treated for all skin cancers combined increased by 44% from the period 2002–2006 to 2007–2011.2 The incidence of melanoma has been increasing for several decades, with rates doubling between 1982 and 2011.6,7 Mortality rates have remained relatively stable, although rates have risen slowly among males.6
Overall, skin cancers are most common among sun-sensitive populations, especially non-Hispanic whites, who have approximately 25 times the incidence rate of melanoma compared with blacks and approximately six times the rate among Hispanics.1 Incidence rates are most common overall among males, although among those younger than age 50, rates are higher among females than males.1 Mortality rates are also higher among males and increase with age, similar to incidence rates. Although whites have the highest incidence and mortality rates, black and Hispanic populations are often diagnosed at later stages and have poorer survival outcomes.8
Skin cancer reporting poses challenges to our understanding of the disease. BCC and SCC are not captured in central cancer registries.9 Melanomas are required by law to be reported to central registries in all states. However, melanomas diagnosed at in situ or early invasive stages are often diagnosed and treated in outpatient settings and thus are prone to underreporting or delayed reporting.10
Risk Factors for Skin Cancer
Most skin cancers are caused by a combination of both non-modifiable (eg, genetic) and modifiable (eg, environmental) risk factors. The most common modifiable risk factor for skin cancer is exposure to ultraviolet radiation (UV). Table 1 provides estimates of relative risk for modifiable and non-modifiable skin cancer risk factors that have been reported in different epidemiologic studies.
TABLE 1.
Modifiable and Non-Modifiable Risk Factors and Estimated Relative Risk by Subtype of Skin Cancer
| Cutaneous Melanoma
|
Squamous Cell Carcinoma
|
Basal Cell Carcinoma
|
||||
|---|---|---|---|---|---|---|
| N | Excess Risk % (95% CI) | N | Excess Risk % (95% CI) | N | Excess Risk % (95% CI) | |
| Non-Modifiable Risk Factors | ||||||
| Skin that sunburns easily (vs. skin that never burns) | 23 | 109 (67, 158)a | 1 | 173 (47, 286)b | 11 | 103 (73, 138)c |
| Natural red hair (vs. dark) | 23 | 264 (156, 437)a | 1 | 116 (−9, 410)b | 13 | 102 (68, 144)c |
| Natural blond hair (vs. dark) | 28 | 96 (41, 174)a | 1 | 34 (−23, 132)b | 12 | 38 (12, 71)c |
| Multiple nevi (101–120 nevi vs. < 15 nevi) | 26 | 589 (363, 925)d | n.a. | n.a. | ||
| Dysplastic nevi (5 vs. 0 dysplastic nevi) | 13 | 536 (280, 933)d | n.a. | n.a. | ||
| Family history of melanoma | 14 | 74 (41, 114)a | 1 | 17 (−3, 41)e | 2 | 31 (25, 37)f |
| Modifiable Risk Factors | ||||||
| Intermittent sun exposure | 34 | 61 (31, 99)g | 2 | −30 – −10h | 8 | 20 – 350h |
| Occupational (ie, chronic) sun exposure | 41 | −5 (−13, 4)g | 18 | 77 (37, 130)i | 23 | 43 (23, 66)j |
| Sunburn in childhood | 27 | 91 (59, 130)k | 1 | 50 (0–130)l | 2 | −10 – 160l |
| Ever sunburned | 28 | 59 (37, 83)k | 1 | 20 (−20, 80)l | 2 | 70–260l |
| Ever indoor tanned | 27 | 20 (8, 34)m | 10 | 67 (29, 117)n | 10 | 29 (8, 53)h |
| Frequent indoor tanning | 15 | 42 (15, 74)m | 1 | 15 (1, 31)n | 4 | 50 (−19, 177)n |
| Indoor tanned before age 35 years | 13 | 59 (36, 85)m | n.a. | n.a. | ||
| Indoor tanned before age 25 years | 6 | 35 (−1, 84)o | 2 | 102 (−30, 486)n | 3 | 40 (29, 52)n |
Abbreviation: N, number of studies; CI, confidence interval; n.a., not available.
NOTES. When available, we used summary estimates. Otherwise, we provided ranges based on the available studies or individual estimates (when only one study is available). We did not differentiate between measures of relative risk (eg, odds ratio, rate ratio, risk ratio) for melanoma because this meets the rare disease assumption by which these measures can be interpreted to be the same. Measures of relative risk for basal cell carcinoma and squamous cell carcinoma are based on odds ratios. Data Sources for Table 1:
Source: Gandini S, Sera F, Cattaruzza MS, et al. Meta-analysis of risk factors for cutaneous melanoma: III. Family history, actinic damage and phenotypic factors. Eur J Cancer. 2005;41(14):2040–59. PMID: 16125929.
Source: Veierod MB, Couto E, Lund E, et al. Host characteristics, sun exposure, indoor tanning and risk of squamous cell carcinoma of the skin. Int J Cancer. 2013. PMID: 24408678.
Source: Khalesi M, Whiteman DC, Tran B, et al. A meta-analysis of pigmentary characteristics, sun sensitivity, freckling and melanocytic nevi and risk of basal cell carcinoma of the skin. Cancer Epidemiol. 2013;37(5):534–43. PMID: 23849507.
Source: Gandini S, Sera F, Cattaruzza MS, et al. Meta-analysis of risk factors for cutaneous melanoma: I. Common and atypical naevi. Eur J Cancer. 2005;41(1):28–44. PMID: 15617989.
Source: Wu S, Han J, Laden F, Qureshi AA. Long-term ultraviolet flux, other potential risk factors, and skin cancer risk: a cohort study. Cancer Epidemiol Biomarkers Prev. 2014;23(6):1080–1089.
Source: Wu S, Han J, Li WQ, Qureshi AA. Basal-cell carcinoma incidence and associated risk factors in US women and men. Am J Epidemiol 2013;178(6):890–897.
Source: Gandini S, Sera F, Cattaruzza MS, Pasquini P, Picconi O, Boyle P, Melchi CF. Meta-analysis of risk factors for cutaneous melanoma: II. Eur J Cancer 2005;41(1):45–60.
Source: Almahroos M, Kurban AK. Ultraviolet carcinogenesis in nonmelanoma skin cancer part II: review and update on epidemiologic correlations. Skinmed 2004;3(3):132–9.
Source: Schmitt J, Seidler A, Diepgen TL, Bauer A. Occupational ultraviolet light exposure increases the risk for the development of cutaneous squamous cell carcinoma: a systematic review and meta-analysis. Br J Dermatol 2011;164(2):291–307.
Source:Bauer A, Diepgen TL, Schmitt J. Is occupational solar ultraviolet irradiation a relevant risk factor for basal cell carcinoma? A systematic review and meta-analysis of the epidemiological literature. 2011;165(3):612–625.
Source: Dennis LK, Vanbeek MJ, Beane Freeman LE, Smith BJ, Dawson DV, Coughlin JA. Sunburns and risk of cutaneous melanoma, does age matter: a comprehensive meta-analysis. Ann Epidemiol 2008;18(8):614–27.
Source: IARC Monographs on the evaluation of carcinogenic risks to humans. Radiation. Volume 100D; 20012. http://monographs.iarc.fr/ENG/Monographs/vol100D/.
Source: Boniol M, Autier P, Boyle P, Gandini S. Cutaneous melanoma attributable to sunbed use: systematic review and meta-analysis. BMJ 2012;345.
Source: Wehner MR, Shive ML, Chren MM, Han J, Qureshi AA, Linos E. Indoor tanning and non-melanoma skin cancer: systematic review and meta-analysis. BMJ 2012;345:e5909.
Source: Colantonio S, Bracken MB, Beecker J. The association of indoor tanning and melanoma in adults: systematic review and meta-analysis. J Am Acad Dermatol 2014;70(5):847–57.
Genetic Risk Factors
Genetic factors strongly influence the risk of skin cancer. The following individual characteristics increase the risk of skin cancer: having a naturally fair skin tone, light colored eyes, blonde or red hair, dysplastic nevi or many common moles, and skin that burns, freckles, reddens, or becomes painful after too much time in the sun.11 Having a previous diagnosis or family history of skin cancer, especially melanoma, also increases risk.12,13 Less obvious genetic factors, such as gene variants or mutations, may also play a role in some melanomas among those without the traditional risk factors of fair skin and hair, and rarely, genetic syndromes such as Familial Atypical Mole Melanoma Syndrome and xeroderma pigmentosum are responsible for the development of melanoma.14–16
Melanocytes, cells found in the basal layer of skin that give skin and eyes their color, are genetically programmed to produce a specific amount of melanin. The amount of melanin or degree of pigmentation is inversely correlated with sun sensitivity and skin cancer risk.17 Melanin absorbs and scatters energy from UV light, protecting the epidermal cells from damage. The Fitzpatrick skin phototyping system provides a numerical classification based on the reaction of unexposed skin to UVA (tanning) and UVB (burning) radiation exposure. For example, Fitzpatrick Type I phototype is defined as very fair skin that burns easily and never tans; Type III is skin that burns and tans moderately; and Type VI skin never burns, tans profusely, and is naturally dark brown.18
In addition to skin tone, melanoma risk is associated with total nevi count. Melanomas often develop from nevi, and nevi indicate both genetic propensity to develop melanoma and UV exposure.19 Skin tone and nevi count are also somewhat associated; studies show that children with light skin, pales eyes, freckles, and a tendency to sunburn have a significantly higher nevi count.20 In addition, patterns of nevi differ by skin type, both by site on the body and by cell type.21
Melanoma incidence and mortality rates are highest among non-Hispanic whites because of their typically lighter skin tone. However, black and Hispanic patients tend to be diagnosed with melanoma at later stages and subsequently have poorer survival outcomes.8,22 Differences in prognosis and survival rates may also be related to socioeconomic factors, which may include insurance or transportation disparities that delay diagnosis and treatment.23–25 Acral lentiginous melanoma (ALM) is a rare subtype of melanoma that is not thought to be UV-related because of its occurrence on the palms of the hands and soles of the feet. Blacks and non-Hispanic whites have similar rates of ALM, with slightly higher rates among Hispanics and lower among Asian/Pacific Islanders.26 However, the lower proportion of UV-related cancers among black and Hispanics means that a greater proportion of melanomas diagnosed among these groups are ALM type, which has poor prognosis; greater proportions of ALM may contribute, in part, to higher mortality rates among these groups as well.26
Modifiable Risk Factors: UV Exposure
Although genetic factors have perhaps the greatest influence on skin cancer risk, nearly all skin cancers are also related, at least in part, to UV exposure. UV exposure stimulates melanocytes to produce melanin, which can appear as tanned skin, and indicates damage to the skin, skin cells, and DNA; more intense exposures can result in sunburn, indicating cell death.27
Types of UV radiation
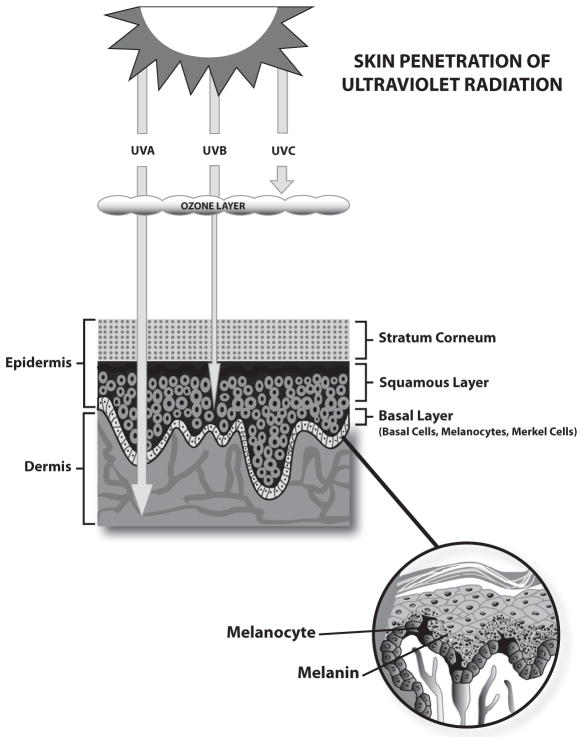
UV radiation is one part of the electromagnetic spectrum measuring in wavelength from 100 to 400 nanometers (nm). There are three subtypes of UV radiation: UVA, UVB, and UVC (Fig. 1). UVA rays have the longest wavelength, measuring from 315 to 400 nm. They are not absorbed by the ozone layer and penetrate deep into the skin, through the epidermal junction where the melanocytes reside in the basal layer, and are primarily responsible for premature skin aging. UVB rays are shorter, measuring from 280 to 315 nm. Both UVA and UVB exposure can result in a tanned appearance.28 UVB creates a tan by increasing melanin production that confers a minimal amount of photoprotection, equivalent to about an SPF of 3, and also indicates damage to the skin.29 UVA-induced tans are not thought to provide photoprotection.28,30 Most UVB radiation is absorbed by the ozone layer, but climate conditions can affect the amount.31 Overexposure to UVB radiation causes erythema, swelling, and pain, the characteristic signs of sunburn, which generally take several hours to develop.32 UVC rays are the shortest, measuring from 100 to 280 nm, and are absorbed by the ozone layer and the atmosphere.
FIGURE 1.
Types of ultraviolet (UV) radiation and skin penetration. (Figure courtesy of the Children’s Melanoma Prevention Foundation, with permission).
Patterns of UV Exposure
UV exposure patterns have been associated with the development of different types of skin cancer and different anatomical distribution patterns.17 Chronic cumulative exposure, including occupational outdoor exposure, has been associated more commonly with BCC and SCC skin cancer.33 The distribution of BCC by anatomic site varies by histologic type, with nodular BCC most commonly appearing on the head and superficial BCC most commonly occurring on the trunk.34 In contrast to SCC skin cancers, melanoma is generally associated with intermittent exposure and a history of sunburn.17,35,36 Similar to BCC, though, melanoma may develop through multiple pathways, with one study finding that women with more nevi on the arm were at increased risk for developing a melanoma on the trunk; those with lower nevi counts tended to develop melanoma on the head and neck.37 Although outdoor workers are traditionally thought to be at increased risk of BCC and SCC, but not for melanoma, a pooled analysis combining 15 studies showed that outdoor workers in UV-intense areas were at increased risk of melanoma.38
Variations in UV by Time and Place
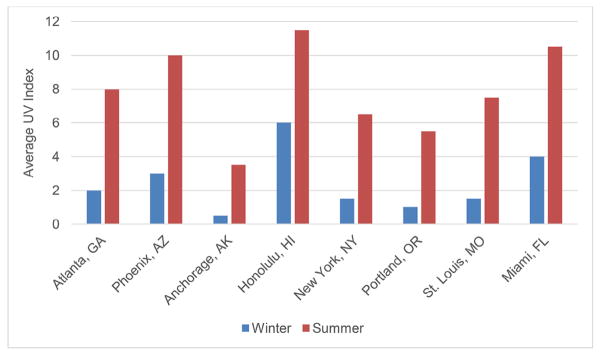
UV radiation varies dramatically both daily and seasonally, as well as by latitude and altitude. The US Environmental Protection Agency has developed the UV Index, a tool to help individuals avoid overexposure to the sun. The UV Index Web site (http://www.epa.gov/sunsafety/uv-index-1) and mobile app provide daily and hourly UV intensity forecasts that are measured on a scale from 1 (low risk of danger from the sun’s UV rays for the average person) to 11 + (extreme risk of harm from unprotected sun exposure). UV intensity peaks at midday and on the summer solstice. For a list of average winter versus summer UV Indices for selected American cities, see Figure 2. UV intensity cannot be felt and must be measured. Because temperature does not always correlate with UV intensity, it is important to check the UV Index and heed the corresponding precautions.
FIGURE 2.
Average seasonal UV index value for selected US cities. (Data source: US Environmental Protection Agency. 2004. A Guide to the UV Index. Available at http://www.epa.gov/sites/production/files/documents/uviguide.pdf).
Individuals living in locations closer to the equator or at higher altitudes have been considered to be at greatest risk for melanoma because of early studies linking latitude and altitude with the disease worldwide.39 However, differences in population demographics, sun protection behaviors, risk awareness, physician density, and melanoma case reporting also influence the observed association between area-level UV and melanoma incidence rates.39 One study found that melanoma risk did correlate with average annual UV exposure and residential history by county, although time spent outdoors was only associated with an increased risk of melanoma for those reporting this exposure at a young age.40 National cancer incidence data on melanoma has revealed a different risk pattern for American children. Wong et al41 found that children living in areas with low UV exposure had a significantly greater incidence of melanoma compared with children living in areas with high UV exposure. The reasons for this finding have not been clearly elucidated, but sunburn in children living in low UV exposure areas may be a sign of intense, intermittent exposure (for example, during vacations).
Occupational UV Exposure
Occupational exposure to UV can increase risk of skin cancer among outdoor workers. Studies clearly demonstrate that outdoor workers are at increased risk of BCC and SCC.17,42 Some studies have not found an increased risk of melanoma among outdoor workers, or have even found a lower risk than indoor workers.42–44 However, studies examining outdoor workers in UV-intense areas have shown that these workers do appear to be at increased risk of melanomas of the head and neck.38,45 Studies of melanoma and occupation are often limited by lack of information on other related factors, such as recreational exposure, protective gear used, and socioeconomic factors.
Risk of Skin Cancer among Cancer Survivors
Oncology patients and cancer survivors, whether skin cancers or other types of cancer, are at increased risk of a later diagnosis of BCC, SCC, or melanoma.46 Increased risk may be conferred by treatment (eg, radiation or BRAF inhibitors) or genetic factors such as BRCA mutations, which may increase risk of skin cancers.46–50 Additionally, immunosuppression related to the initial development of cancer or to treatment (such as an organ or stem cell transplant) can increase risk of a later skin cancer.51,52 Organ transplant recipients are at very high risk for developing UV-induced skin tumors, especially cutaneous SCCs.53,54 An increased risk of melanoma has been documented in patients with a history of prior skin cancer, Kaposi sarcoma, female breast cancer, ocular melanoma, prostate cancer, thyroid cancer, non-Hodgkin lymphoma, and chronic lymphocytic leukemia.46 Patients diagnosed with chronic lymphocytic leukemia and non-Hodgkin lymphoma are at increased risk for developing particularly aggressive skin cancers associated with poorer outcomes.55 Childhood cancer survivors are also more likely to be diagnosed with skin cancers in adulthood.56,57
The risk of developing a second melanoma within 1 year after an initial diagnosis of melanoma is about 2%, with about 1% of patients developing a second melanoma each year for 2 to 15 years.58 Melanoma survivors are at increased risk of developing a second primary cancer at another site, especially skin cancers, but also cancers of the bone, soft tissue, colon and rectum, female breast, kidney, prostate, thyroid, non-Hodgkin lymphoma, and chronic lymphocytic leukemia.59,60 In one study, melanoma patients receiving a BRAF inhibitor for metastatic disease (vemurafenib) had a 26% chance of developing a SCC within a median timeframe of approximately 8 weeks; most of the SCCs were keratoacanthomatype, which generally have a good prognosis.61
Patients with different types of skin cancer vary regarding their prognosis, consequences, and experiences.62 In addition, the diagnosis of skin cancer may put patients at greater risk for subsequent skin cancers and other malignancies. Patients with BCC or SCC may be at increased risk of a later diagnosis of female breast cancer, lung cancer, and melanoma.63 Prior diagnosis with a cutaneous SCC appeared to be associated with poorer survival for later cancers.64 Additionally, a history of BCC or SCC imparts a very high risk of subsequent skin cancers; the risk of developing a second BCC within 3 years was 44%, and SCC was 18%; both representing a 10-fold increase in incidence compared with the general population.65
Behavioral Surveillance Data on UV Exposure
Because of the long lag time from UV exposure to development of skin cancer, self-reported behaviors (eg, use of sun protection and indoor tanning) and sunburn are often used as more immediate measures by which the success of skin cancer prevention efforts can be evaluated. Although any amount of UV exposure can affect skin cancer risk, entirely avoiding UV from the sun is neither realistic nor advisable. Spending time outdoors can provide opportunities for increased physical activity and improved mental health.66,67 Sun protection can help reduce risks of overexposure to UV when spending time outdoors.
Sun Protection and Sunburn
Although the scientific evidence clearly links excessive UV exposure to an increased risk for skin cancer, people in the US continue to report low rates of using sun protection, and high rates of indoor tanning device use and sunburn. Federal surveys such as the Youth Risk Behavior Survey and the National Health Interview Survey (NHIS) have periodically included questions about use of sun protection and indoor tanning in the past year. Data on sunburn among adults are available from NHIS, and from special studies for children and adolescents.
Sunburn
Sunburn is often used as a proxy for skin cancer risk because it takes into account individual sun sensitivity as well as UV exposure. Data from the NHIS demonstrated that sunburn was common among adults, with about 38% of adults (37% of women and 39% of men) in 2010 reporting having experienced a sunburn in the past year. Sunburns were most common among non-Hispanic whites (47%) and adults under the age of 25 years (51%).68 Although federal surveys do not routinely ask children about sunburn, a longitudinal study from Massachusetts conducted in 2004 and 2007 found that more than 50% of children aged 10 to 14 surveyed reported having been sunburned during the summer.69
Sun Protection
The NHIS asked respondents about the following methods of sun protection when outdoors for more than an hour on a sunny day: sunscreen with a sun protection factor (SPF) of 15 or higher, wearing protective clothing (wide-brimmed hats, long sleeves, long pants, or other clothing that reaches the ankles), and staying in the shade. NHIS data from 2010 (the most recent year for which data are available) indicated suboptimal skin cancer risk-related behaviors among US adults. For example, approximately 21% of men and 41% of women reported usually or always protecting themselves from the sun by using sunscreen with SPF 15 or higher,68 and some of these individuals, particularly women, may have used sunscreen to protect their faces but not other exposed skin.70 Approximately 46% of men and 34% of women usually or always protected themselves by wearing protective clothing, and about 31% of men and 44% of women reported usually or always seeking shade to protect themselves from the sun.68 According to data from the 2013 Youth Risk Behavior Survey, only about 10% of US high school students used sunscreen with an SPF of 15 or higher always or most of the time when outside for more than 1 hour on a sunny day.71 There has also been a decrease in the prevalence of routine sunscreen use among high school students over time, dropping from 13.3% in 1999 to 10.1% in 2013.72
Indoor Tanning
Indoor tanning exposes users to intense UV to tan the skin for cosmetic purposes. Meta-analyses have shown that indoor tanning increases risk of BCC, SCC, and melanoma.73–75 The UV exposure from tanning devices is usually significantly more intense than the UV exposure one would receive when outdoors, especially the levels of UVA.76,77 For example, tanning devices have been found to expose users to an average of four to 13 times the amount of UVA present in noonday summer sun in Washington DC, with some devices exposing users to even higher amounts.78,79 The magnitude of the association between indoor tanning and melanoma varies from study to study, reflecting different populations and settings, although tanning more frequently and at younger ages is consistently associated with increased risk.1 A recent study conducted in Minnesota found that among women diagnosed with melanoma younger than age 30, 97% had participated in indoor tanning, reflecting a 6-fold increase in risk.80 Indoor tanning is most common among young non-Hispanic white females ages 16 to 25, with more than 30% of this demographic group reporting indoor tanning in the past year, often frequently.81 In 2013, 13% of high school students reported that they had used an indoor tanning device in the past year, and use was even more common among older, female (20%) and non-Hispanic white (18%) students.71 Highest use was observed among non-Hispanic white female students (31%) and 12th-grade female students (27%). Analyses of indoor tanning device use from 2009 to 2013 indicated significant decreases among females, non-Hispanic white females, and non-Hispanic black male students.82 Indoor tanning also remains common among certain adult groups. Although in 2013, only 4% of all US adults reported indoor tanning in the past year, indoor tanning was much more common among women under the age of 30 years (14%).83
Evidence-Based Strategies to Reduce Skin Cancer Risk
Many strategies have been proven effective in increasing use of sun protection and reducing sunburn and use of indoor tanning, thereby lowering the risk of skin cancer.
The Surgeon General’s Call to Action
In 2014, the Surgeon General released The Call to Action to Prevent Skin Cancer. This document described skin cancer as a major public health issue, and identified five strategic goals to reduce skin cancer in the US.1 The first goal aimed to increase opportunities for sun protection outdoors, for instance, by increasing the availability of shade in recreational, occupational, and educational settings. The second goal aimed to provide individuals with accurate information about UV exposure, through strategies such as developing targeted messages about UV and skin cancer prevention, and ensuring that effective sun safety education is available in schools and workplaces. One strategy related to this goal that is relevant for nurses and other health care providers is the use of recommended preventive services, particularly the US Preventive Services Task Force (USPSTF) recommendations.84 The third strategic goal of the Call to Action related to promoting policies that advance the national goal of preventing skin cancer; for instance, supporting inclusion of sun protection in school and workplace policies and education, strengthening policies enabling electronic reporting of reportable skin cancers, and supporting shade policies. The fourth strategic goal aimed to reduce harms from indoor tanning by communicating the harms of indoor tanning, ensuring that regulations and policies are enforced, and considering new ones. The fifth strategic goal aimed to strengthen research, surveillance, monitoring, and evaluation related to skin cancer prevention.
The Call to Action is a first step in promoting community awareness to prevent skin cancer. Using an existing health promotion model applied to melanoma prevention, some have suggested that patients need the knowledge, tools, and incentives to change behavior, and that community health awareness is also key.85 The Surgeon General’s goals to educate the community about UV exposure, the hazards of indoor tanning, and skin cancer prevention, as well as conducting research, are all well within the scope of practice for the oncology nurse.
One nursing organization has taken the lead on promoting the Call to Action. The Dermatology Nurses’ Association in their Position Statement recommends educating patients and the community about both primary and secondary prevention. In 2007, Dermatology Nurses’ Association endorsed the Children’s Melanoma Prevention Foundation’s “SunAWARE” acronym as their official prevention standard because it recommends avoiding unprotected exposure to UV radiation, never indoor tanning, proven sun protection practices, and routine skin self-examination.
The Community Guide
The Community Preventive Services Task Force (Task Force) is an independent, nonfederal, unpaid panel of public health and prevention experts that provides evidence-based findings and recommendations about community preventive services, programs, and policies to improve health.86 Its members represent a broad range of research, practice, and policy expertise in community preventive services, public health, health promotion, and disease prevention. Findings from the Task Force are published in “The Guide to Community Preventive Services” (The Community Guide).
Educational and Environmental/Policy Approaches
The Task Force recently conducted a review of the latest evidence regarding the effectiveness of interventions that combine educational and environmental/policy approaches to increase sun-safety behaviors.87 Educational interventions generally provide information about sun safety and the effects of UV radiation. Messages delivered in lectures or through small media can be reinforced by modeling or role playing (for children). Sun-protective environmental and policy changes include increasing the availability of sun-protective items (eg, sunscreen or protective clothing), adding sun-protective features to the physical environment (eg, shade structures), and implementing sun-protection policies (eg, clothing guidelines, restrictions on outdoor activities during peak sunlight hours).
The Task Force found sufficient evidence to recommend such intervention approaches in several community settings, specifically childcare centers, primary and middle schools, outdoor occupational settings, and outdoor recreational and tourism settings. At the time of the review, the Task Force found insufficient evidence to issue a recommendation regarding the effectiveness of such intervention strategies in high schools and colleges.
Community-Wide Interventions
The Task Force also conducted a review of the evidence regarding the effectiveness of community-wide interventions.88 Such interventions seek to increase sun-safety behaviors within a community by targeting a large part of the population in a defined area. The Task Force found sufficient evidence to recommend multi-component community-wide interventions to prevent skin cancer. Multi-component community-wide interventions use a combination of at least two or more strategies (ie, individual-directed strategies, mass media campaigns, and/or environmental/policy approaches) across at least two or more settings within a defined geographic area (eg, city, state province, country) in a coordinated effort to influence sun-safety behaviors. The Task Force also reviewed the scientific evidence regarding the effectiveness of mass media interventions for skin cancer prevention. Mass media interventions use communication channels such as print media (eg, newspapers, magazines), broadcast media (eg, radio, television), billboards, or the internet to disseminate information and/or behavioral guidance to wide audiences. The Task Force found insufficient evidence to determine the effectiveness of mass media interventions when implemented alone rather than in combination with other intervention strategies.
Provider-Focused Interventions
Since 2012, the USPSTF has recommended counseling children, adolescents, and young adults aged 10 to 24 years of age who have fair skin about minimizing their exposure to UV radiation to reduce the risk for skin cancer.84 The USPSTF found moderate-level evidence of a moderate net benefit of counseling among this population, with minimal harms. During the review, the USPSTF concluded that the current evidence regarding the benefits and harms of counseling adults older than age 24 years about minimizing exposure to UV is insufficient.84
In 2009 the USPSTF stated that the current evidence regarding skin cancer screening was insufficient to recommend screening for the general population. The USPSTF is currently (as of June 2016) re-reviewing the evidence regarding screening, and a draft recommendation released November 2015 stated that the latest evidence is still insufficient to recommend skin cancer screening for the average-risk population.89
Although screening is not recommended for the general population, many patients commonly seen by oncology nurses may be at increased risk of melanoma. Patients at high risk may include those having a previous history of cancer or other risk factors, such as having atypical nevi or many common nevi, having a family or personal history of skin cancer, occupational exposure, or intense exposure such as indoor tanning. Oncology nurses can play an important role in raising awareness of skin cancer among these patients. Some of these high-risk patients may benefit from screening, skin self-exam, or increased awareness about skin cancer prevention and risk. In some cases, oncology nurses can assist patients by teaching them how to perform a total skin self-exam.90 Some patients with a history of melanoma, atypical nevi, or large number of common acquired nevi may benefit from total body photography, in which patients are usually provided a copy of their photographs for use in home surveillance.91,92 Electronic apps that capture and record nevi for subsequent comparison are also available.93
There are many valuable online resources available for nurses to complement their patient and community education. For more information on relevant resources including the UV Index, mole mapping, indoor tanning, skin cancer carcinogenesis, skin cancer diagnosis, and skin cancer self-assessment, please refer to Table 2.
TABLE 2.
Selected Internet Resources for Skin Cancer Prevention
| Resources | URL |
|---|---|
| General information | |
| SunWise (National Environmental Education Foundation [NEEF]) | https://www.neefusa.org/sunwise |
| Surgeon General’s Call to Action to Prevent Skin Cancer (Office of the Surgeon General) | http://www.surgeongeneral.gov/library/calls/prevent-skin-cancer/index.html |
| Information on Melanoma (National Cancer Institute [NCI]) | http://www.cancer.gov/types/skin |
| Skin cancer (CDC) | http://www.cdc.gov/cancer/skin/ |
| Skin cancer prevention fact sheets (CDC) | http://www.cdc.gov/cancer/skin/basic_info/fact_sheets.htm |
| What You Need to Know About Skin Cancer (NCI) For Patients | http://www.cancer.gov/publications/patient-education/wyntk-skin-cancer/ |
| Global Solar UV Index (EPA and the National Weather Service) | http://www.epa.gov/sunsafety |
| Skin Cancer (National Institutes of Health [NIH]) For Seniors | http://nihseniorhealth.gov/skincancer/skincancerdefined/01.html |
| Skin Care and Aging (NIH) | https://www.nia.nih.gov/health/publication/skin-care-and-aging |
| Sunscreen (US Food and Drug Administration [FDA]) | http://www.fda.gov/Drugs/ResourcesForYou/Consumers/BuyingUsingMedicineSafely/UnderstandingOver-the-CounterMedicines/ucm239463.htm |
| Indoor tanning (FDA) | http://www.fda.gov/ForConsumers/ConsumerUpdates/ucm186687.htm |
| Ultraviolet radiation (World Health Organization) | http://www.who.int/uv/en/ |
| SunSmart Resources (Cancer Council Victoria) | http://www.sunsmart.com.au/ |
| Recommendations | |
| Skin Cancer Screening Recommendations (US Preventive Services Task Force [USPSTF]) | http://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/skin-cancer-screening |
| Counseling to Prevent Skin Cancer: Recommendations and Rationale (USPSTF) | http://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/skin-cancer-counseling |
| Guide to Community Preventive Services | http://www.thecommunityguide.org/cancer/index.html |
| Preventing Skin Cancer: Findings of the Task Force on Community Preventive Services on Reducing Exposure to Ultraviolet Light | http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5215a1.htm |
| Partners | |
| American Academy of Dermatology | https://www.aad.org/ |
| American Academy of Family Physicians | http://www.aafp.org/home.html |
| American Academy of Pediatrics | https://www.aap.org/ |
| American Cancer Society | http://www.cancer.org/ |
| American Public Health Association | http://www.apha.org/ |
| American School Health Association | http://www.ashaweb.org/ |
| Children’s Melanoma Prevention Foundation | http://www.melanomaprevention.org/ |
| Melanoma Research Foundation | http://www.melanoma.org/ |
| National Association of School Nurses | http://www.nasn.org/ |
| National Cancer Institute | http://www.cancer.gov/ |
| National Council on Skin Cancer Prevention | http://www.skincancerprevention.org/ |
| National Institute of Environmental Health Sciences | http://www.niehs.nih.gov/ |
| Skin Cancer Foundation | http://www.skincancer.org/ |
| Society of Health and Physical Educators (SHAPE America) | http://www.shapeamerica.org/ |
| Sun Safety Alliance | http://www.sunsafetyalliance.org/ |
| SunSafe Project, Norris Cotton Cancer Center, Dartmouth Medical School | http://www.cancer.dartmouth.edu/pf/sunsafe_programs.html |
| US Environmental Protection Agency | http://www.epa.gov/ |
Importance of Prevention for Cancer Survivors and Their Families
Despite being at increased risk of future skin cancers, research shows that survivors of childhood cancers, as well as adults previously diagnosed with BCC, SCC, or melanoma, often do not adequately protect their skin from UV exposure.94–96 Similarly, children of melanoma survivors do not appear to have different sun protection practices than those at average risk.97
For those at increased risk of skin cancer related to a previous cancer diagnosis or because of family history, sun protection is especially important. Several interventions have shown promise in reducing future risks of skin cancer among survivors. For example, an intervention study demonstrated that increased use of sun protection may reduce risks of skin cancer among organ transplant recipients.98 A Web-based intervention aimed at melanoma survivors demonstrated improved sun protection behaviors.99 An intervention to increase sun protection targeted specifically to children of melanoma survivors was shown to increase participants’ use of hats and reapplication of sunscreen, although a reduction in sunburns was not observed.100
While more research is needed to determine effective interventions to prevent future skin cancers among cancer survivors, oncology nurses can be important sources of information to educate their patients about the importance of sun protection during and after treatment. Currently, the core curriculum for oncology nurse training includes information on how to counsel patients to reduce their risk of skin cancer in the following ways: minimizing midday sun exposure, avoiding sunburn, avoiding the use of indoor tanning devices, using sun protection including sun protective clothing, regular use of sunscreen with SPF of 15 or higher, wearing eye protection, and avoiding sun exposure for infants <6 months of age.101 These recommendations are consistent with the Centers for Disease Control and Prevention’s recommendations to reduce risk of skin cancers, available at: http://www.cdc.gov/cancer/skin/.
Role of Oncology Nurses
Oncology nurses play an important role in educating patients and their communities about skin cancer prevention. Nurses can work as advocates for their patients and communities, and can be involved in research regarding skin cancer prevention. Many oncology nurses orchestrate skin cancer screening events throughout the US in May for Skin Cancer Awareness Month. Others educate school children and promote the incorporation of shade in their communities. Nurses, working together with physicians, patients, and their communities, can play an important role in achieving the goals outlined in the Call to Action and preventing future cases of skin cancer.102
Acknowledgments
The authors would like to thank Laurie Sigmund, Illustrator with Sugar Shack Design, for assistance with graphics. They would also like to acknowledge the work of Dr. Boris Lushniak and Dr. Howard Koh, without whom this work would not have been possible.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Contributor Information
Meg Watson, Epidemiologist, Division of Cancer Prevention and Control, Centers for Disease Control and Prevention, Atlanta, GA.
Dawn M. Holman, Behavioral Scientist, Division of Cancer Prevention and Control, Centers for Disease Control and Prevention, Atlanta, GA.
Maryellen Maguire-Eisen, Executive Director, Children’s Melanoma Prevention Foundation, Norwell, MA.
References
- 1.US Department of Health and Human Services. The Surgeon General’s call to action to prevent skin cancer. Washington, DC: US Department of Health and Human Services, Office of the Surgeon General; 2014. [Google Scholar]
- 2.Guy GP, Machlin S, Ekwueme DU, Yabroff KR. Prevalence and costs of skin cancer treatment in the US, 2002–2006 and 2007–2011. Am J Prev Med. 2015;48:183–187. doi: 10.1016/j.amepre.2014.08.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lomas A, Leonardi-Bee J, Bath-Hextall F. A systematic review of worldwide incidence of nonmelanoma skin cancer. Br J Dermatol. 2012;166:1069–1080. doi: 10.1111/j.1365-2133.2012.10830.x. [DOI] [PubMed] [Google Scholar]
- 4.Karia PS, Han J, Schmults CD. Cutaneous squamous cell carcinoma: estimated incidence of disease, nodal metastasis, and deaths from disease in the United States, 2012. J Am Acad Dermatol. 2013;68:957–966. doi: 10.1016/j.jaad.2012.11.037. [DOI] [PubMed] [Google Scholar]
- 5.US Cancer Statistics Working Group. [Accessed July 4, 2016];United States cancer statistics: 1999–2012 incidence and mortality Web-based report. 2015 Available at: http://www.cdc.gov/uscs.
- 6.Kohler BA, Sherman RL, Howlader N, et al. Annual report to the nation on the status of cancer, 1975–2011, featuring incidence of breast cancer subtypes by race/ethnicity, poverty, and state. J Natl Cancer Inst. 2015;107:djv048. doi: 10.1093/jnci/djv048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guy GP, Jr, Thomas CC, Thompson T, Watson M, Massetti GM, Richardson LC. Vital signs: melanoma incidence and mortality trends and projections – United States, 1982–2030. MMWR Morb Mortal Wkly Rep. 2015;64:591–596. [PMC free article] [PubMed] [Google Scholar]
- 8.Pollack LA, Li J, Berkowitz Z, et al. Melanoma survival in the United States, 1992 to 2005. J Am Acad Dermatol. 2011;65(Suppl 1):S78.e01–S78.e10. doi: 10.1016/j.jaad.2011.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.United States Cancer Statistics (USCS) [Accessed January 20, 2015];Technical notes: incidence data sources. Available at: http://www.cdc.gov/cancer/npcr/uscs/technical_notes/data_sources/incidence.htm.
- 10.Cockburn M, Swetter SM, Peng D, Keegan THM, Deapen D, Clarke CA. Melanoma underreporting: why does it happen, how big is the problem, and how do we fix it? J Am Acad Dermatol. 2008;59:1081–1085. doi: 10.1016/j.jaad.2008.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gandini S, Sera F, Cattaruzza MS, et al. Meta-analysis of risk factors for cutaneous melanoma: III. family history, actinic damage and phenotypic factors. Eur J Cancer. 2005;41:2040–2059. doi: 10.1016/j.ejca.2005.03.034. [DOI] [PubMed] [Google Scholar]
- 12.Chen T, Fallah M, Kharazmi E, Ji J, Sundquist K, Hemminki K. Effect of a detailed family history of melanoma on risk for other tumors: a cohort study based on the nationwide Swedish family-cancer database. J Invest Dermatol. 2014;134:930–936. doi: 10.1038/jid.2013.460. [DOI] [PubMed] [Google Scholar]
- 13.Karagas MR, Stukel TA, Greenberg ER, Baron JA, Mott LA, Stern RS. Risk of subsequent basal cell carcinoma and squamous cell carcinoma of the skin among patients with prior skin cancer. Skin Cancer Prevention Study Group. JAMA. 1992;267:3305–3310. [PubMed] [Google Scholar]
- 14.Pasquali E, Garcia-Borron JC, Fargnoli MC, et al. MC1R variants increased the risk of sporadic cutaneous melanoma in darker-pigmented Caucasians: a pooled-analysis from the M-SKIP project. Int J Cancer. 2015;136:618–631. doi: 10.1002/ijc.29018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eckerle Mize D, Bishop M, Resse E, Sluzevich J. Familial atypical multiple mole melanoma syndrome. In: Riegert-Johnson DL, Boardman LA, Hefferon T, Roberts M, editors. Cancer syndromes. Bethesda, MD: 2009. [PubMed] [Google Scholar]
- 16.Gruber SB, Armstrong BK. Cutaneous and ocular melanoma. In: Schottenfeld D, Fraumeni JF, editors. Cancer epidemiology and prevention. New York, NY: Oxford University Press; 2006. pp. 1196–1229. [Google Scholar]
- 17.Karagas MR, Weinstock MA, Nelson HH. Keratinocyte carcinomas (basal and squamous cell carcinomas of the skin) In: Schottenfeld D, Fraumeni JF, editors. Cancer epidemiology and prevention. 3. New York, NY: Oxford University Press; 2006. pp. 1230–1250. [Google Scholar]
- 18.Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol. 1988;124:869–871. doi: 10.1001/archderm.124.6.869. [DOI] [PubMed] [Google Scholar]
- 19.Haenssle HA, Mograby N, Ngassa A, et al. Association of patient risk factors and frequency of nevus-associated cutaneous melanomas. JAMA Dermatol. 2016;152:291–298. doi: 10.1001/jamadermatol.2015.3775. [DOI] [PubMed] [Google Scholar]
- 20.Wiecker TS, Luther H, Buettner P, Bauer J, Garbe C. Moderate sun exposure and nevus counts in parents are associated with development of melanocytic nevi in childhood: a risk factor study in 1,812 kindergarten children. Cancer. 2003;97:628–638. doi: 10.1002/cncr.11114. [DOI] [PubMed] [Google Scholar]
- 21.Tuma B, Yamada S, Atallah AN, Araujo FM, Hirata SH. Dermoscopy of black skin: a cross-sectional study of clinical and dermoscopic features of melanocytic lesions in individuals with type V/VI skin compared to those with type I/II skin. J Am Acad Dermatol. 2015;73:114–119. doi: 10.1016/j.jaad.2015.03.043. [DOI] [PubMed] [Google Scholar]
- 22.Clairwood M, Ricketts J, Grant-Kels J, Gonsalves L. Melanoma in skin of color in Connecticut: an analysis of melanoma incidence and stage at diagnosis in non-Hispanic blacks, non-Hispanic whites, and Hispanics. Int J Dermatol. 2014;53:425–433. doi: 10.1111/j.1365-4632.2012.05713.x. [DOI] [PubMed] [Google Scholar]
- 23.Harvey VM, Patel H, Sandhu S, Wallington SF, Hinds G. Social determinants of racial and ethnic disparities in cutaneous melanoma outcomes. Cancer Control. 2014;21:343–349. doi: 10.1177/107327481402100411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jiang AJ, Rambhatla PV, Eide MJ. Socioeconomic and lifestyle factors and melanoma: a systematic review. Br J Dermatol. 2015;172:885–915. doi: 10.1111/bjd.13500. [DOI] [PubMed] [Google Scholar]
- 25.Bradford PT. Skin cancer in skin of color. Dermatol Nurs. 2009;21:170–177. 206. quiz 178. [PMC free article] [PubMed] [Google Scholar]
- 26.Bradford PT, Goldstein AM, McMaster ML, Tucker MA. Acral lentiginous melanoma: incidence and survival patterns in the United States, 1986–2005. Arch Dermatol. 2009;145:427–434. doi: 10.1001/archdermatol.2008.609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gilchrest B, Eller M, Geller AC, Yaar M. The pathogenesis of melanoma induced by ultraviolet radiation. N Engl J Med. 1999;340:1341–1348. doi: 10.1056/NEJM199904293401707. [DOI] [PubMed] [Google Scholar]
- 28.Miyamura Y, Coelho SG, Schlenz K, et al. The deceptive nature of UVA tanning versus the modest protective effects of UVB tanning on human skin. Pigment Cell Melanoma Res. 2011;24:136–147. doi: 10.1111/j.1755-148X.2010.00764.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sheehan JM, Potten CS, Young AR. Tanning in human skin types II and III offers modest photoprotection against erythema. Photochem Photobiol. 1998;68:588–592. [PubMed] [Google Scholar]
- 30.Coelho SG, Yin L, Smuda C, Mahns A, Kolbe L, Hearing VJ. Photobiological implications of melanin photoprotection after UVB-induced tanning of human skin but not UVA-induced tanning. Pigment Cell Melanoma Res. 2015;28:210–216. doi: 10.1111/pcmr.12331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bais AF, McKenzie RL, Bernhard G, et al. Ozone depletion and climate change: impacts on UV radiation. Photochem Photobiol Sci. 2015;14:19–52. doi: 10.1039/c4pp90032d. [DOI] [PubMed] [Google Scholar]
- 32. [Accessed January 20, 2016];Sunburn: MedlinePlus Encyclopedia. 2016 Available at: https://www.nlm.nih.gov/medlineplus/ency/article/003227.htm.
- 33.Milon A, Bulliard JL, Vuilleumier L, Danuser B, Vernez D. Estimating the contribution of occupational solar ultraviolet exposure to skin cancer. Br J Dermatol. 2014;170:157–164. doi: 10.1111/bjd.12604. [DOI] [PubMed] [Google Scholar]
- 34.Scrivener Y, Grosshans E, Cribier B. Variations of basal cell carcinomas according to gender, age, location and histopathological subtype. Br J Dermatol. 2002;147:41–47. doi: 10.1046/j.1365-2133.2002.04804.x. [DOI] [PubMed] [Google Scholar]
- 35.Dennis LK, Vanbeek MJ, Beane Freeman LE, Smith BJ, Dawson DV, Coughlin JA. Sunburns and risk of cutaneous melanoma: does age matter? A comprehensive meta-analysis. Ann Epidemiol. 2008;18:614–627. doi: 10.1016/j.annepidem.2008.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gordon D, Gillgren P, Eloranta S, et al. Time trends in incidence of cutaneous melanoma by detailed anatomical location and patterns of ultraviolet radiation exposure: a retrospective population-based study. Melanoma Res. 2015;25:348–356. doi: 10.1097/CMR.0000000000000170. [DOI] [PubMed] [Google Scholar]
- 37.Olsen CM, Zens MS, Stukel TA, et al. Nevus density and melanoma risk in women: a pooled analysis to test the divergent pathway hypothesis. Int J Cancer. 2009;124:937–944. doi: 10.1002/ijc.24011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chang YM, Barrett JH, Bishop DT, et al. Sun exposure and melanoma risk at different latitudes: a pooled analysis of 5,700 cases and 7,216 controls. Int J Epidemiol. 2009;38:814–830. doi: 10.1093/ije/dyp166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Richards TB, Johnson CJ, Tatalovich Z, et al. Association between cutaneous melanoma incidence rates among white U.S. residents and county-level estimates of solar ultraviolet exposure. J Am Acad Dermatol. 2011;65(Suppl 1):S50.e1–S50.e9. doi: 10.1016/j.jaad.2011.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tatalovich Z, Wilson JP, Mack T, Yan Y, Cockburn M. The objective assessment of lifetime cumulative ultraviolet exposure for determining melanoma risk. J Photochem Photobiol B. 2006;85:198–204. doi: 10.1016/j.jphotobiol.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 41.Wong JR, Harris JK, Rodriguez-Galindo C, Johnson KJ. Incidence of childhood and adolescent melanoma in the United States: 1973–2009. Pediatrics. 2013;131:846–854. doi: 10.1542/peds.2012-2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gallagher RP, Elwood JM, Yang CP. Is chronic sunlight exposure important in accounting for increases in melanoma incidence? Int J Cancer. 1989;44:813–815. doi: 10.1002/ijc.2910440511. [DOI] [PubMed] [Google Scholar]
- 43.Garland FC, White MR, Garland CF, Shaw E, Gorham ED. Occupational sunlight exposure and melanoma in the U.S. Navy Arch Environ Health. 1990;45:261–267. doi: 10.1080/00039896.1990.10118743. [DOI] [PubMed] [Google Scholar]
- 44.Pukkala E, Martinsen JI, Lynge E, et al. Occupation and cancer – follow-up of 15 million people in five Nordic countries. Acta Oncol. 2009;48:646–790. doi: 10.1080/02841860902913546. [DOI] [PubMed] [Google Scholar]
- 45.Whiteman DC, Stickley M, Watt P, Hughes MC, Davis MB, Green AC. Anatomic site, sun exposure, and risk of cutaneous melanoma. J Clin Oncol. 2006;24:3172–3177. doi: 10.1200/JCO.2006.06.1325. [DOI] [PubMed] [Google Scholar]
- 46.Yang GB, Barnholtz-Sloan JS, Chen Y, Bordeaux JS. Risk and survival of cutaneous melanoma diagnosed subsequent to a previous cancer. Arch Dermatol. 2011;147:1395–1402. doi: 10.1001/archdermatol.2011.1133. [DOI] [PubMed] [Google Scholar]
- 47.Goggins W, Gao W, Tsao H. Association between female breast cancer and cutaneous melanoma. Int J Cancer. 2004;111:792–794. doi: 10.1002/ijc.20322. [DOI] [PubMed] [Google Scholar]
- 48.Goldstein AM, Fraser MC, Struewing JP, et al. Increased risk of pancreatic cancer in melanoma-prone kindreds with p16INK4 mutations. N Engl J Med. 1995;333:970–974. doi: 10.1056/NEJM199510123331504. [DOI] [PubMed] [Google Scholar]
- 49.Ginsburg OM, Kim-Sing C, Foulkes WD, et al. BRCA1 and BRCA2 families and the risk of skin cancer. Fam Cancer. 2010;9:489–493. doi: 10.1007/s10689-010-9377-y. [DOI] [PubMed] [Google Scholar]
- 50.Mersch J, Jackson MA, Park M, et al. Cancers associated with BRCA1 and BRCA2 mutations other than breast and ovarian. Cancer. 2015;121:269–275. doi: 10.1002/cncr.29041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Omland SH, Gniadecki R, Haedersdal M, Helweg-Larsen J, Omland LH. Skin cancer risk in hematopoietic stem-cell transplant recipients compared with background population and renal transplant recipients: a population-based cohort study. JAMA Dermatol. 2016;152:177–183. doi: 10.1001/jamadermatol.2015.3902. [DOI] [PubMed] [Google Scholar]
- 52.Wang D, DuBois RN. Immunosuppression associated with chronic inflammation in the tumor microenvironment. Carcinogenesis. 2015;36:1085–1093. doi: 10.1093/carcin/bgv123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ulrich C, Arnold R, Frei U, Hetzer R, Neuhaus P, Stockfleth E. Skin changes following organ transplantation: an interdisciplinary challenge. Dtsch Arztebl Int. 2014;111:188–194. doi: 10.3238/arztebl.2014.0188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wheless L, Jacks S, Mooneyham Potter KA, Leach BC, Cook J. Skin cancer in organ transplant recipients: more than the immune system. J Am Acad Dermatol. 2014;71:359–365. doi: 10.1016/j.jaad.2014.02.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Onajin O, Brewer JD. Skin cancer in patients with chronic lymphocytic leukemia and non-Hodgkin lymphoma. Clin Adv Hematol Oncol. 2012;10:571–576. [PubMed] [Google Scholar]
- 56.Pappo AS, Armstrong GT, Liu W, et al. Melanoma as a subsequent neoplasm in adult survivors of childhood cancer: a report from the childhood cancer survivor study. Pediatr Blood Cancer. 2013;60:461–466. doi: 10.1002/pbc.24266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Braam KI, Overbeek A, Kaspers GJ, et al. Malignant melanoma as second malignant neoplasm in long-term childhood cancer survivors: a systematic review. Pediatr Blood Cancer. 2012;58:665–674. doi: 10.1002/pbc.24023. [DOI] [PubMed] [Google Scholar]
- 58.Moore MM, Geller AC, Warton EM, Schwalbe J, Asgari MM. Multiple primary melanomas among 16,570 patients with melanoma diagnosed at Kaiser Permanente Northern California, 1996 to 2011. J Am Acad Dermatol. 2015;73:630–636. doi: 10.1016/j.jaad.2015.06.059. [DOI] [PubMed] [Google Scholar]
- 59.Caini S, Boniol M, Botteri E, et al. The risk of developing a second primary cancer in melanoma patients: a comprehensive review of the literature and meta-analysis. J Dermatol Sci. 2014;75:3–9. doi: 10.1016/j.jdermsci.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 60.Balamurugan A, Rees JR, Kosary C, Rim SH, Li J, Stewart SL. Subsequent primary cancers among men and women with in situ and invasive melanoma of the skin. J Am Acad Dermatol. 2011;65(Suppl 1):S69–S77. doi: 10.1016/j.jaad.2011.04.033. [DOI] [PubMed] [Google Scholar]
- 61.Sosman JA, Kim KB, Schuchter L, et al. Survival in BRAF V600-mutant advanced melanoma treated with vemurafenib. N Engl J Med. 2012;366:707–714. doi: 10.1056/NEJMoa1112302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Winterbottom A, Harcourt D. Patients’ experience of the diagnosis and treatment of skin cancer. J Adv Nurs. 2004;48:226–233. doi: 10.1111/j.1365-2648.2004.03191.x. [DOI] [PubMed] [Google Scholar]
- 63.Song F, Qureshi AA, Giovannucci EL, et al. Risk of a second primary cancer after non-melanoma skin cancer in white men and women: a prospective cohort study. PLoS Med. 2013;10:e1001433. doi: 10.1371/journal.pmed.1001433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Johannesdottir SA, Lash TL, Jensen AO, Farkas DK, Olesen AB. Mortality in cancer patients with a history of cutaneous squamous cell carcinoma–a nationwide population-based cohort study. BMC Cancer. 2012;12:126. doi: 10.1186/1471-2407-12-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Marcil I, Stern RS. Risk of developing a subsequent nonmelanoma skin cancer in patients with a history of nonmelanoma skin cancer: a critical review of the literature and meta-analysis. Arch Dermatol. 2000;136:1524–1530. doi: 10.1001/archderm.136.12.1524. [DOI] [PubMed] [Google Scholar]
- 66.Grinde B, Patil GG. Biophilia: does visual contact with nature impact on health and well-being? Int J Environ Res Public Health. 2009;6:2332–2343. doi: 10.3390/ijerph6092332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Thompson Coon J, Boddy K, Stein K, Whear R, Barton J, Depledge MH. Does participating in physical activity in outdoor natural environments have a greater effect on physical and mental wellbeing than physical activity indoors? A systematic review. Environ Sci Technol. 2011;45:1761–1772. doi: 10.1021/es102947t. [DOI] [PubMed] [Google Scholar]
- 68.National Cancer Institute. Cancer trends progress report. Prevention. UV exposure and sun protective practices. Available at: http://progressreport.cancer.gov/prevention/sun_protection.
- 69.Dusza SW, Halpern AC, Satagopan JM, et al. Prospective study of sunburn and sun behavior patterns during adolescence. Pediatrics. 2012;129:309–317. doi: 10.1542/peds.2011-0104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Holman DM, Berkowitz Z, Guy GP, Jr, Hawkins NA, Saraiya M, Watson M. Patterns of sunscreen use on the face and other exposed skin among US adults. J Am Acad Dermatol. 2015;73:83–92. e1. doi: 10.1016/j.jaad.2015.02.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kann L, Kinchen S, Shanklin SL, et al. and the Centers for Disease Control and Prevention. Youth risk behavior surveillance – United States, 2013. MMWR Suppl. 2014;63:1–168. [PubMed] [Google Scholar]
- 72.Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance – United States, 2011. MMWR Surveill Summ. 2012;61:1–162. [PubMed] [Google Scholar]
- 73.El Ghissassi F, Baan R, Straif K, et al. A review of human carcinogens – part D: radiation. Lancet Oncol. 2009;10:751–752. doi: 10.1016/s1470-2045(09)70213-x. [DOI] [PubMed] [Google Scholar]
- 74.Wehner MR, Shive ML, Chren MM, Han J, Qureshi AA, Linos E. Indoor tanning and non-melanoma skin cancer: systematic review and meta-analysis. BMJ. 2012;345:e5909. doi: 10.1136/bmj.e5909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Colantonio S, Bracken MB, Beecker J. The association of indoor tanning and melanoma in adults: systematic review and meta-analysis. J Am Acad Dermatol. 2014;70:847–857. e018. doi: 10.1016/j.jaad.2013.11.050. [DOI] [PubMed] [Google Scholar]
- 76.Gerber B, Mathys P, Moser M, Bressoud D, Braun-Fahrlander C. Ultraviolet emission spectra of sunbeds. Photochem Photobiol. 2002;76:664–668. doi: 10.1562/0031-8655(2002)076<0664:uesos>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 77.Tierney P, Ferguson J, Ibbotson S, Dawe R, Eadie E, Moseley H. Nine out of 10 sunbeds in England emit ultraviolet radiation levels that exceed current safety limits. Br J Dermatol. 2013;168:602–608. doi: 10.1111/bjd.12181. [DOI] [PubMed] [Google Scholar]
- 78.Hornung RL, Magee KH, Lee WJ, Hansen LA, Hsieh YC. Tanning facility use: are we exceeding Food and Drug Administration limits? J Am Acad Dermatol. 2003;49:655–661. doi: 10.1067/s0190-9622(03)01586-x. [DOI] [PubMed] [Google Scholar]
- 79.Miller SA, Hamilton SL, Wester UG, Cyr WH. An analysis of UVA emissions from sunlamps and the potential importance for melanoma. Photochem Photobiol. 1998;68:63–70. [PubMed] [Google Scholar]
- 80.Lazovich D, Isaksson Vogel R, Weinstock MA, Nelson HH, Ahmed RL, Berwick M. Association between indoor tanning and melanoma in younger men and women. JAMA Dermatol. 2016;152:268–275. doi: 10.1001/jamadermatol.2015.2938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Guy GP, Berkowitz Z, Watson M, Holman DM, Richardson LC. Indoor Tanning among young non-Hispanic white females. JAMA Intern Med. 2013;173:1920–1922. doi: 10.1001/jamainternmed.2013.10013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Guy GP, Berkowitz Z, Everett Jones S, Holman DM, Garnett E, Watson M. Trends in indoor tanning among US high school students, 2009–2013. JAMA Dermatol. 2015;151:448–450. doi: 10.1001/jamadermatol.2014.4677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Guy GP, Berkowitz Z, Holman DM, Hartman AM. Recent changes in the prevalence of and factors associated with frequency of indoor tanning among US adults. JAMA Dermatol. 2015;151:1256–1259. doi: 10.1001/jamadermatol.2015.1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.U.S. Preventive Services Task Force. [Accessed May 16, 2013];Behavioral counseling to prevent skin cancer: US Preventive Services Task Force recommendation statement. Available at: http://www.uspreventiveservicestaskforce.org/uspstf11/skincancouns/skincancounsrs.htm.
- 85.Torrens R, Swan BA. Promoting prevention and early recognition of malignant melanoma. Dermatol Nurs. 2009;21:115–122. quiz 123. [PubMed] [Google Scholar]
- 86.Community Preventive Services Task Force. The community guide: what works to promote health. [Accessed July 4, 2016];The guide to community preventive services. Available at: http://www.thecommunityguide.org/index.html.
- 87.Community Preventive Services Task Force. [Accessed July 4, 2016];Preventing skin cancer: education and policy approaches. Available at: http://www.thecommunityguide.org/cancer/skin/education-policy/index.html.
- 88.Community Preventive Services Task Force. Preventing skin cancer: community-wide interventions. Available at: http://www.thecommunityguide.org/cancer/skin/community-wide/index.html.
- 89.U.S. Preventive Services Task Force. Draft recommendation statement. [Accessed January 11, 2016];Skin cancer: screening. Available at: http://www.uspreventiveservicestaskforce.org/Page/Document/draft-recommendation-statement168/skin-cancer-screening2.
- 90.Maguire-Eisen M. Risk assessment and early detection of skin cancers. Semin Oncol Nurs. 2003;19:43–51. doi: 10.1053/sonu.2003.50003. [DOI] [PubMed] [Google Scholar]
- 91.Moloney FJ, Guitera P, Coates E, et al. Detection of primary melanoma in individuals at extreme high risk: a prospective 5-year follow-up study. JAMA Dermatol. 2014;150:819–827. doi: 10.1001/jamadermatol.2014.514. [DOI] [PubMed] [Google Scholar]
- 92.Dengel LT, Petroni GR, Judge J, et al. Total body photography for skin cancer screening. Int J Dermatol. 2015;54:1250–1254. doi: 10.1111/ijd.12593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Oregon Health & Science University. [Accessed January 20, 2016];Mole mapper. Available at: https://www.ohsu.edu/xd/health/services/dermatology/war-on-melanoma/mole-mapper.cfm.
- 94.Levy-Shraga Y, Cohen R, Ben Ami M, Yeshayahu Y, Temam V, Modan-Moses D. Sun Exposure and protection habits in pediatric patients with a history of malignancy. PLoS ONE. 2015;10:e0137453. doi: 10.1371/journal.pone.0137453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Nahar VK, Allison Ford M, Brodell RT, et al. Skin cancer prevention practices among malignant melanoma survivors: a systematic review. J Cancer Res Clin Oncol. 2016;142:1273–1283. doi: 10.1007/s00432-015-2086-z. [DOI] [PubMed] [Google Scholar]
- 96.Nahar VK, Ford MA, Jacks SK, et al. Sun-related behaviors among individuals previously diagnosed with non-melanoma skin cancer. Indian J Dermatol Venereol Leprol. 2015;81:568–575. doi: 10.4103/0378-6323.168337. [DOI] [PubMed] [Google Scholar]
- 97.Glenn BA, Lin T, Chang LC, et al. Sun protection practices and sun exposure among children with a parental history of melanoma. Cancer Epidemiol Biomarkers Prev. 2015;24:169–177. doi: 10.1158/1055-9965.EPI-14-0650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ulrich C, Jurgensen JS, Degen A, et al. Prevention of non-melanoma skin cancer in organ transplant patients by regular use of a sunscreen: a 24 months, prospective, case-control study. Br J Dermatol. 2009;161(Suppl 3):78–84. doi: 10.1111/j.1365-2133.2009.09453.x. [DOI] [PubMed] [Google Scholar]
- 99.Bowen DJ, Burke W, Hay JL, Meischke H, Harris JN. Effects of web-based intervention on risk reduction behaviors in melanoma survivors. J Cancer Surviv. 2015;9:279–286. doi: 10.1007/s11764-014-0412-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Gritz ER, Tripp MK, Peterson SK, et al. Randomized controlled trial of a sun protection intervention for children of melanoma survivors. Cancer Epidemiol Biomarkers Prev. 2013;22:1813–1824. doi: 10.1158/1055-9965.EPI-13-0249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Itano JK, Brant J, Conde F, Saria M. Oncology Nursing Society. Core curriculum for oncology nursing. 5. Philadelphia, PA: Saunders; 2016. [Google Scholar]
- 102.Maguire-Eisen M. Skin cancer: a growing health problem for children. Semin Oncol Nurs. 2013;29:206–213. doi: 10.1016/j.soncn.2013.06.006. [DOI] [PubMed] [Google Scholar]