Abstract
Objectives
Many adolescents who die by suicide have never obtained mental health services. In response to this, the National Strategy for Suicide Prevention recommends screening for elevated suicide risk in emergency departments (EDs). This cross-sectional study was designed to examine 1) the concurrent validity and utility of an adolescent suicide risk screen for use in general medical EDs and 2) the prevalence of positive screens for adolescent males and females using two different sets of screening criteria.
Methods
Participants were 298 adolescents seeking pediatric or psychiatric emergency services (50% male; 83% white, 16% black or African American, 5.4% Hispanic). The inclusion criterion was age 13 to 17 years. Exclusion criteria were severe cognitive impairment, no parent or legal guardian present to provide consent, or abnormal vital signs. Parent or guardian consent and adolescent assent were obtained for 61% of consecutively eligible adolescents. Elevated risk was defined as 1) Suicidal Ideation Questionnaire-Junior [SIQ-JR] score of ≥31 or suicide attempt in the past 3 months or 2) alcohol abuse plus depression (Alcohol Use Disorders Identification Test-3 [AUDIT-3] score of ≥3, Reynolds Adolescent Depression Scale-2 [RADS-2] score of ≥76). The Beck Hopelessness Scale (BHS) and Problem Oriented Screening Instrument for Teenagers (POSIT) were used to ascertain concurrent validity.
Results
Sixteen percent (n = 48) of adolescents screened positive for elevated suicide risk. Within this group, 98% reported severe suicide ideation or a recent suicide attempt (46% attempt and ideation, 10% attempt only, 42% ideation only) and 27% reported alcohol abuse and depression. Nineteen percent of adolescents who screened positive presented for nonpsychiatric reasons. One-third of adolescents with positive screens were not receiving any mental health or substance use treatment. Demonstrating concurrent validity, the BHS scores of adolescents with positive screens and the POSIT scores of those with positive screens due to alcohol abuse and depression indicated substantial impairment. The addition of alcohol abuse with co-occurring depression as a positive screen criterion did not result in improved case identification. Among the subgroup screening positive due to depression plus alcohol abuse, all but one (>90%) also reported severe suicide ideation and/or a recent suicide attempt. This subgroup (approximately 17% of adolescents who screened positive) also reported significantly more impulsivity than other adolescents who screened positive.
Conclusions
The suicide risk screen showed evidence of concurrent validity. It also demonstrated utility in identifying 1) adolescents at elevated risk for suicide who presented to the ED with unrelated medical concerns and 2) a subgroup of adolescents who may be at highly elevated risk for suicide due to the combination of depression, alcohol abuse, suicidality, and impulsivity.
Keywords: adolescent, emergency department, suicide risk, public health, depression, screening
Tragically, suicide is the third leading cause of death among adolescents,1 and a history of suicide attempts is common among adolescents who die by suicide.2–4 The nationally representative Youth Risk Behavior Survey revealed that 8.4% of high school students in the United States attempted suicide in the past year, and a total of 16.9% seriously considered a suicide attempt.5
Primary risk factors for suicide attempts and suicide among adolescents include previous suicide ideation and behavior, depressive disorders, and alcohol use, in addition to other factors such as conduct disorder or aggressive behavior, a history of sexual abuse, and exposure to adverse life events.6–8 Further, the presence of depression with comorbid alcohol or substance abuse is predictive of more chronic depressive episodes,9,10 more severe alcohol-related problems,11 and escalated risk of suicidal behaviors12 and suicide.13
Unfortunately, the majority of adolescents who die by suicide have never received any type of psychiatric treatment or mental health service.2,4,14,15 “Psychological autopsy studies” involve examining available records and documents (health care, forensic, school, medical examiner, toxicology results, suicide notes) and conducting structured interviews with the families, friends, teachers, and health care professionals of the youths who died by suicide. In one such study of 53 completed suicides, Marttunen et al.4 reported that only 44% of the females and 34% of the males had ever had contact with the psychiatric care system. In a similar study, Shaffer et al.14 reported that only 24 of 120 youth had been evaluated or treated by a mental health professional during the 3 months prior to their suicide.14
The emergency department (ED) is ideally suited for the identification of adolescents who are at elevated risk for suicidal behavior and suicide. Approximately 30% of adolescents seek ED services each year.16 Moreover, many adolescents use the ED as their primary source of health care, and research indicates that the incidence of risk factors such as depression and alcohol abuse are higher in adolescents who use the ED in this manner.17 Finally, in a retrospective study, Gairin et al.18 reported that 39% of a consecutive sample of 219 suicide deaths (ages 16–93 years) had attended an ED in the year prior to their death.18 Taken together, these studies support the ED as a strong potential setting for adolescent suicide risk screening.
This study examined the concurrent validity and utility of an ED-based screening protocol for elevated risk of suicidal behavior and suicide among adolescents. Evidence-based psychosocial treatments for adolescent alcohol abuse19 and depression20–24 exist, and the newer antidepressants have demonstrated some benefit for adolescents.25 However, as noted above, many adolescents at elevated risk for suicide have never obtained any mental health services. The study aims to take a first step in addressing this problem by closely examining a screening protocol designed to identify adolescent males and females at elevated risk.
Previous projects have demonstrated the feasibility of adolescent depression screening26,27 and suicide risk screening for youths with psychiatric complaints28 in pediatric emergency settings. In addition, the key issues relevant to screening for suicide risk in pediatric emergency settings were recently reviewed.29 This study builds upon these contributions by screening adolescents who present with psychiatric and nonpsychiatric complaints and by taking into account the heterogeneity that characterizes suicidal adolescents. In this study, we examine two sets of screen criteria, defining a positive screen as either 1) severe suicide ideation or recent attempt or 2) co-occurring depression and alcohol abuse. To our knowledge, this is the first adolescent suicide risk screening study implemented in the ED with adolescents who present for nonpsychiatric complaints.
METHODS
Study Design and Population
This was a cross-sectional convenience sample of adolescents (ages 13–17 years). The study was approved by the institutional review board of the university. Written informed consent was obtained from the parent or guardian, and written informed assent was obtained from the adolescent. During the assent process, participants were informed that their parent/guardian and ED physician would be notified if they screened as “high risk” for suicide, as defined by the study risk management protocol. Screening was conducted by research staff members, with a bachelor's degree or higher, who were trained in the informed consent process, administration of self-report measures, and suicide-specific risk management protocol.
The study was conducted at the ED of a university teaching hospital. In 2007, the ED had over 75,000 visits. Consecutive adolescents seeking care were approached for study participation during late afternoon/evening shifts (three per week) between April 2007 and May 2008. Patients were included regardless of whether they were seeking nonpsychiatric or psychiatric care, both of which are offered in our ED. Exclusion criteria included 1) severe cognitive impairment, 2) no parent or legal guardian present, 3) abnormal vital signs, and 4) parent/guardian or adolescent do not speak English. Sixty-one percent of eligible adolescents participated.
Survey Content and Administration
Adolescents, without their parents present, completed the screen self-report measures in a written format, requiring 5 to 10 minutes. If the adolescent's medical condition prevented him or her from completing written forms, study measures were administered verbally. Demographic information was collected in an interview format with the parent or guardian.
Screen Survey
Depression
The 30-item self-report Reynolds Adolescent Depression Scale 2nd Edition (RADS-2) was used to screen for depression. Developed for community-based screening, it is brief and easy to read, has excellent psychometric properties, and has extensive grade- and sex-based norms.30 The validated clinical cutpoint of 76 was used.30
Suicide Ideation and Recent Suicide Attempt
The Suicidal Ideation Questionnaire-Junior (SIQ-JR) is a 15-item self-report scale assessing the frequency of a wide range of suicidal thoughts.31 It was developed for community-based screening, is relatively brief, and has grade- and sex-based norms. Total scores have excellent, well-documented psychometric properties.31,32 The SIQ-JR total scores of psychiatrically hospitalized adolescents have been found to be significant predictors of suicidal thoughts and attempts 6 months posthospitalization.33 In this study, a positive screen was defined as a score at or above the empirically established clinical cutpoint of 31.31 The occurrence of one or more suicide attempts during the previous 3 months was assessed with a dichotomous indicator, with further information requested for “yes” responses.
Alcohol Abuse
Alcohol consumption was assessed using the three-item Alcohol Use Disorders Identification Test (AUDIT-3).34 The AUDIT-3 has been validated for use with adolescents in the ED35 and, compared to other brief screening tools, has shown superior discrimination in identifying adolescents with alcohol use disorders. The three items of the AUDIT-3 assess frequency of alcohol consumption, typical quantity of alcohol use, and frequency of binge drinking (six or more drinks on one occasion). A cutpoint of 3 or greater was used in this study because it was determined to be optimal for identifying adolescents with alcohol use disorders.35
Positive Screen Criteria
A positive screen for elevated suicide risk was defined as a score at or above the clinical cutpoint of the SIQ-JR,31 a recent history of a suicide attempt, or a combination of scores at or above the cutpoint on both the RADS-230 and the AUDIT-3.35 The latter combination criteria were used, in addition to direct questioning about suicide ideation and behavior, because depression combined with alcohol use has been associated with increased risk of suicidal behaviors12 and suicide13 and because suicide ideation has not been strongly linked with suicide attempts in adolescent males.36 This is critical, as males are approximately four times more likely to die by suicide than females.1
Adolescents who screened positive for elevated suicide risk completed additional measures. If an adolescent was determined to be at “high risk” for suicide (acute risk requiring immediate attention, defined in study risk management protocol), the study screening staff notified ED personnel and the study project director. The risk determination was made by a licensed mental health professional.
Other Measures
Alcohol Abuse
For positively screened adolescents, the full 10 items of the AUDIT-1037 were used to assess alcohol abuse in detail. The AUDIT-10 was used to provide feedback to adolescents about problem areas related to drinking that were determined by a confirma-tory factor analysis.38
Alcohol Consequences
A 17-item scale from the Problem Oriented Screening Instrument for Teenagers (POSIT) was used to assess adolescent alcohol-related consequences.39,40 This scale was used to assess the concurrent validity of the three-item AUDIT alcohol screen.
Beck Hopelessness Scale
The Beck Hopelessness Scale (BHS) is a 20-item true–false self-report scale that assesses the extent of negative attitudes about the future.41,42 It is scored by summing the answers to each item (as 0 or 1), with a total score ranging between 0 and 20. Concurrent validity has been established in studies reporting significant correlations between BHS scores and measures of depression and suicide ideation in psychiatrically hospitalized adolescents.43 Studies have also reported that adolescents with a history of suicide attempts had significantly higher BHS scores than community samples and inpatients without a history of attempts.44
Services
The Services Assessment Record Review (SARR, available from first author CAK) was completed by interview with parents and is available for 41 of the 48 adolescents with positive screens. It assesses which types of services the adolescent has used in the past year (including health, mental health, substance use, and other services) as well as the frequency of use for those services. It also assesses history of psychiatric medications prescribed during the past year.
Impulsivity
The 30-item self-report Barratt Impulsivity Scale (BIS-11) has three factors that assess motor impulsiveness, nonplanning, and attentional impulsiveness.45 Each item is scored with a four-point Likert scale from 1 to 4, with total scores ranging between 30 and 120. The BIS-11 is correlated with other measures of impulsivity and aggression, appears to discriminate between more impulsive groups such as prison inmates and less impulsive groups such as college students, and has been associated with increased levels of substance use and suicidality.45
Medical Chart Abstraction
Chief complaints were extracted from medical charts and coded by trained research assistants, in keeping with the criteria described by Gilbert et al.46 All data were independently coded by two research staff. We used two primary and six secondary categories: nonpsychiatric complaint (medical, unintentional injury, intentional injury by other) and psychiatric complaint (psychiatric-nonsuicidal, suicide ideation, suicide attempt). The intercoder percentage agreement for the six secondary categories was 97.6%. Adolescents were determined to have nonsuicidal self-injuries if they inflicted self-harm without any evidence of even possible fleeting suicidal intent. This classification is in accordance with a widely accepted taxonomy of suicidal behavior set forth by O'Carroll et al.47 and Silverman et al. 48 Such injuries were classified into “nonpsychiatric complaint” if there were no psychiatric symptoms recorded, and into “psychiatric complaint” if they co-occurred with a psychiatric symptom (e.g., superficial cut, depressive symptoms).
Data Analyses
Data were analyzed in SPSS Version 15 (SPSS Inc., Chicago, IL). Descriptive statistics are reported. Chi-square tests were used for comparisons involving categorical variables and t-tests were used for group comparisons of continuous variables. Internal consistencies were calculated using the alpha coefficient.
RESULTS
A total of 491 adolescents meeting inclusion/exclusion criteria were approached and 298 consented (61% consent rate). There were 148 males and 150 females ranging in age from 13 years to 17 years (mean ± standard deviation [SD] = 15.02 ± 1.39 years). The consent rate was not significantly different for females compared to males (63.56% vs. 57.42%, χ2(1, N = 491) = 1.933; p = 0.16). Similarly, there were no age differences between those who did and did not consent (mean ± SD = 15.04 ± 1.37 vs. mean ± sd = 15.04 ± 1.38, t(489) = −0.037; p = 0.97). The racial/ethnic distribution for consented subjects was as follows: 83% (n = 247) white, 16% (n = 48) black or African American, 2.4% (n = 7) American Indian or Alaskan Native, and 3.0% (n = 9) Asian (participants could select more than one race; see Table 1). Of the sample, 5.4% (n = 16) were Hispanic. Due to institutional review board regulations that limited the data available to us prior to study consent, we were unable to obtain racial/ethnic information for subjects who refused participation.
Table 1.
Comparisons of Adolescents with Negative and Positive Screens
| Clinical/Demographic Variable | Negative Screens (n = 247) | Positive Screens (n = 48) |
|---|---|---|
| SIQ-JR | 5.96 ± 6.34 | 52.48 ± 20.88 |
| RADS-2 | 53.95 ± 13.92 | 85.40 ± 12.55 |
| AUDIT-3 (for alcohol use) | 0.53 ± 1.33 | 2.11 ± 2.61 |
| Age, yr | 15.00 ± 1.37 | 15.10 ± 1.33 |
| Male | 131 (53.0) | 16 (33.3)* |
| Female | 116 (47.0) | 32 (66.7)* |
| Hispanic | 4 (5.7) | 2 (4.2) |
| Race† | ||
| White | 207 (83.8) | 40 (83.3) |
| Black or African American | 39 (15.8) | 6 (12.5) |
| Asian | 8 (3.2) | 1 (2.1) |
| American Indian or Alaskan Native | 4 (1.6) | 3 (6.3) |
| Other race | 7 (2.8) | 2 (4.2) |
Data are reported as mean ± SD or number (%).
AUDIT-3 = Alcohol Use Disorders Identification Test; RADS-2 = Reynolds Adolescent Depression Scale-2; SIQ-JR = Suicidal Ideation Questionnaire-Junior.
The greater proportion of females screening positive was significant (p < 0.01).
Participants could respond “Yes” to multiple categories.
Positive Versus Negative Screens for Elevated Suicide Risk
Among consenting adolescents, 295 adolescents (99.0%) completed the suicide risk screen and 48 adolescents (16%) screened positive for elevated suicide risk. Sex was the only demographic variable differentiating positive and negative screens. Females screened positive for elevated suicide risk significantly more than males (n = 32 or 21.3% of females vs. n = 16 or 10.8% of males, χ2(1, N = 295) = 6.24; p < 0.01). Table 1 presents demographic characteristics and screening results for the positively screened adolescents in comparison to the total sample. (Note: Three adolescents did not complete enough of the screening measures for the screens to be considered valid.)
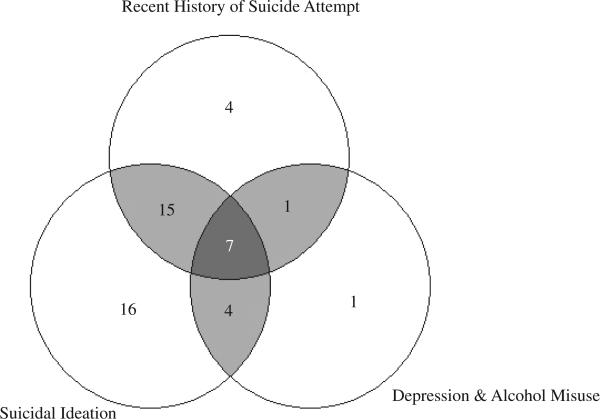
Figure 1 presents detailed findings on reasons that adolescents screened positive for elevated suicide risk. Of the 48 adolescents who screened positive, 98% (n = 47) screened positive due to a recent suicide attempt and/or suicide ideation as measured on the SIQ-JR. Forty-six percent (n = 22) of the adolescents reported a recent attempt paired with suicide ideation, 10% (n = 5) reported only a recent attempt, and 42% (n = 20) reported only suicide ideation. Largely overlapping with this, 27% (n = 13) screened positive due to the combination of alcohol abuse and depression. In comparing the two sets of screen criteria, only one additional suicide risk case was identified by the alcohol abuse plus depression screen criterion. The screen measures each exhibited high internal consistency in this sample (RADS-2, α = 0.95; SIQ-JR, α = 0.97; AUDIT-3, α = 0.89).
Figure 1.
Reasons for positive suicide risk screens; n = 48.
Positive screen adolescents who presented for psychiatric versus nonpsychiatric chief complaints did not differ in terms of demographic characteristics (age, sex, and race/ethnicity) or scores on depression, suicide ideation, or alcohol/substance use scales (RADS-2, SIQ-JR, Suicide Attempt Question; AUDIT-10, POSIT, BHS).
Screening Validity
Adolescents who screened positive for depression and alcohol abuse, with or without suicide ideation or recent suicide attempt, reported significantly more negative consequences from alcohol use on the POSIT than those not screening positive for depression and alcohol abuse (mean ± SD = 6.8 ± 5.6 vs. mean ± SD = 1.1 ± 2.6, t(12.86) = 3.44; p < 0.01). Similarly, these adolescents reported significantly more impulsivity on the BIS-11 than those who reported significant suicide ideation or a recent suicide attempt but not depression and alcohol abuse (mean ± SD = 83.8 ± 8.2 vs. mean ± SD = 76.0 ± 12.1, t(42) = 2.04; p < 0.05). Adolescents who screened positive for elevated suicide risk had results on the BHS (mean ± SD = 11.7 ± 5.3) comparable to or higher than those previously reported for psychiatrically hospitalized adolescents (mean ± SD = 6.9 ± 4.9).49 This supports the screen's concurrent validity, as BHS scores have shown predictive validity for suicide attempts in adolescents43 and for eventual suicide in adults.42 Validation measures demonstrated high internal consistency in this sample (AUDIT-10, α = 0.92; POSIT, α = 0.94; BHS, α = 0.88; BIS, α = 0.82).
Within the total sample of screened adolescents, mean scores on all screen measures were significantly higher for adolescents with a psychiatric chief complaint compared to those with a nonpsychiatric chief complaint. SIQ-JR mean (±SD) scores were higher: 40.82 (±27.01) versus 6.26 (±7.87), t(63.78) = 9.96, p < 0.01. RADS-2 mean (±SD) scores were higher: 81.73 (±13.64) versus 53.04 (±13.63), t(293) = 14.72, p < 0.01. Similarly, AUDIT-3 mean (±SD) scores were higher 1.55 (±2.41) versus 0.58 (±1.40), t(70.79) = 3.02, p < 0.01.
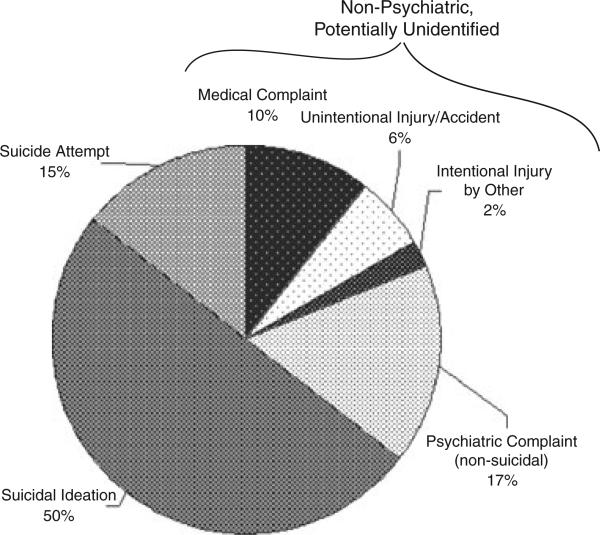
Screening Utility
Among adolescents who screened positive for elevated suicide risk, 19% (n = 9) presented for nonpsychiatric reasons and 35.4% (n = 17) presented for complaints other than suicide ideation and behavior, including psychiatric and nonpsychiatric complaints. Figure 2 displays the chief complaints for all adolescents with positive suicide risk screens.
Figure 2.
Chief complaints for adolescents with positive suicide risk screens; n = 48.
There were no significant differences in the proportion of positively screened adolescents who were obtaining mental health services based on whether they presented with a nonpsychiatric or psychiatric chief complaint. Sixty-seven percent of positively screened adolescents presenting with a psychiatric complaint were receiving mental health services, compared to 50% of positively screened adolescents presenting with a nonpsychiatric complaint (n = 41, degrees of freedom = 1, p = 0.434). Among all adolescents who screened positive (with services data), 23 (56.1%) were currently obtaining mental health treatment, two (4.9%) were obtaining substance abuse treatment and mental health treatment, and one (2.4%) was obtaining substance abuse treatment only. Fifteen positively screened adolescents (36.6%) were not receiving any mental health or substance use treatment.
DISCUSSION
This study demonstrated the concurrent validity and potential utility of a brief suicide risk screening protocol for adolescents seeking emergency services that addresses multiple suicide risk factors in boys and girls. Sixteen percent of consented adolescents screened positive for elevated suicide risk, which was defined as significant current suicidal thinking, a recent suicide attempt, or a combination of alcohol abuse and depression. The broad screening criteria were used due to the multiple and overlapping risk factors for suicidal behavior and suicide among adolescents,50 and the previous finding that self-reported suicide ideation is not a predictor of suicide attempts among male adolescents.36
Nearly twice as many females as males screened positive for elevated suicide risk. This was the only demographic variable that differentiated positive and negative screens. This is consistent with the higher prevalence rates of suicide ideation and suicide attempts in adolescent females versus males,5 which are primary suicide risk screen criteria. However, this finding, and the national prevalence rates for nonlethal suicidality, also reflect the difficulty in identifying high-suicide-risk males for whom the rate of death by suicide is four to five times higher that of females.1 Research consistently indicates that males are less likely to engage in professional help seeking than females.51 The ED may be one place where these high-risk adolescent males can be successfully identified, and one-third of adolescents who screened positive in this study were male. This risk identification may be the first step in meeting the challenge of reducing the toll of suicide among adolescent males.
A surprising finding in this study was that, after taking into account adolescents’ suicidal thoughts and behaviors as positive screen criteria, the combination of alcohol abuse and depression identified only one additional positive screen. Ninety-eight percent of positive screens were associated with a recent suicide attempt and/or current significant suicidal thoughts, defined as a score above the clinical cutpoint on the standardized SIQ-JR.31 Consistent with previous studies indicating a strong link between alcohol abuse, depression, and suicidality,9,10,12,13 almost all of the 27% who screened positive for alcohol abuse and depression also screened positive for suicide attempt and/or current suicidal thoughts. This suggests that one could shorten the 5- to 10-minute screen protocol to an even briefer screen of 2–5 minutes by screening only for severe suicide ideation or a recent suicide attempt. These time estimates are based on published scale administration times.30,31,37
The data also suggest, however, that the combination of screening tools used in the present study may be important in identifying adolescents at an even more highly elevated level of suicide risk. If resources are limited, this could be particularly important for maximally facilitating the next steps: treatment linkage and engagement. As noted above, adolescents who screened positive for alcohol abuse and depression generally reported some type of suicidality. Further, 17% of adolescents who screened positive reported a recent suicide attempt, alcohol abuse, and depression. Because those who screened positive for alcohol abuse and depression in our study reported significantly higher levels of impulsivity than other adolescents who screened positive, and because a recent suicide attempt is a risk factor for another suicide attempt and suicide,52 this subgroup may be at a highly elevated level of risk. Longitudinal outcome research is needed to determine the relative predictive validity of the briefer and more comprehensive screen criteria.
Protocols have been developed to screen adolescent ED patients for depression.26,27 Moreover, Horowitz et al.28 developed a four-item screen to identify suicide risk in child and adolescent ED patients using the SIQ to establish the criterion. However, the study by Horowitz only involved screening children and adolescents who presented with psychiatric chief complaints (as determined by a triage nurse). Our study's screening protocol builds upon these previous efforts by screening for suicide risk in adolescents who present with nonpsychiatric and psychiatric chief complaints and by examining the potential utility of screening for a broader range of suicide risk factors. The screen protocol we used showed evidence of strong concurrent validity. Those who screened positive had BHS scores in the clinical range, and previous research indicates that BHS scores predict suicide attempts and eventual suicide.42,43 Those who screened positive for alcohol and depression reported significant alcohol-related functional impairment and less treatment received for injuries. Given that depression may characterize only approximately 50% of male suicides,53 depression screening alone is insufficient to detect elevated suicide risk. Furthermore, among males, suicide attempts in young adulthood have not been associated with higher rates of reported suicide ideation during adolescence.36 Public health concerns may be better served through broader suicide screening measures, and this protocol offers a short, efficient means of screening for suicide risk in adolescent ED patients.
LIMITATIONS
The present study was conducted at one university hospital and the sample was predominantly white, which may limit the generalizability of findings. As a university ED with specialized psychiatric emergency services available, it is possible that psychiatric complaints were somewhat overrepresented in this sample. Further, because the study consent rate was 61% of consecutive patients meeting eligibility criteria, it is possible that some characteristic of adolescents or parents who refused consent may have been meaningful to screening for elevated suicide risk. However, this consent rate is similar to that obtained for other ED-based suicide screening protocols.26,27 Another possible limitation includes sole reliance on a self-report screening strategy. However, such a strategy has maximum feasibility in the ED setting and showed evidence of concurrent validity. Additionally, baseline assessments of functioning were not obtained for negatively screened adolescents, which somewhat limited the scope of data concerning the screening survey's concurrent validity.
CONCLUSIONS
The suicide risk screen protocol demonstrated strong concurrent validity and utility in identifying adolescents with elevated suicide risk who may not otherwise have been identified. Sixteen percent of study-eligible adolescents who were seeking ED services and assented to study participation (with parent or guardian consent) screened positive for elevated suicide risk; one-third of these adolescents were not receiving any mental health or substance use treatment. Among those who screened positive, a significant minority (19%) presented for nonpsychiatric reasons and perhaps would not have been otherwise identified. This subgroup included at-risk males who, as a group, are at particularly high risk for suicide. Finally, the screen criterion of severe suicide ideation or recent suicide attempt performed as well in case identification as the more comprehensive screen criteria that also included depression and alcohol abuse.
Acknowledgments
We thank Chris Merchant, Nicole Klaus, and SunShine Mills for their assistance as evaluators; Melissa Webster and Anne Kramer for their help with project management; Ryan Hill for his help in data management and analysis; and all participating families.
Funding for this project was provided by the State of Michigan Department of Community Health and a National Institute of Mental Health K24 Award, “Health Behavior Interventions for Suicidal Adolescents,” to CAK (K24 MH077705).
Footnotes
Presented at the annual conference of the American Association of Suicidology, Boston, MA, April 2008; and the Society for Academic Emergency Medicine annual meeting, New Orleans, LA, May 2009.
References
- 1.Centers for Disease Control and Prevention [Jun 2, 2009];Web-based Injury Statistics Query and Reporting System (WISQARS) Available at: http://www.cdc.gov/injury/wisqars/index.html.
- 2.Brent DA, Perper JA, Goldstein CE, et al. Risk factors for adolescent suicide. A comparison of adolescent suicide victims with suicidal inpatients. Arch Gen Psychiatry. 1988;45:581–8. doi: 10.1001/archpsyc.1988.01800300079011. [DOI] [PubMed] [Google Scholar]
- 3.Borowsky IW, Ireland M, Resnick MD. Adolescent suicide attempts: risks and protectors. Pediatrics. 2001;107:485–93. doi: 10.1542/peds.107.3.485. [DOI] [PubMed] [Google Scholar]
- 4.Marttunen MJ, Aro HM, Lonnqvist JK. Adolescent suicide: endpoint of long-term difficulties. J Am Acad Child Adolesc Psychiatry. 1992;31:649–54. doi: 10.1097/00004583-199207000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance–United States, 2005. MMWR Surveill Summ. 2006;55(SS-5):1–112. [PubMed] [Google Scholar]
- 6.Fergusson DM, Woodward LJ, Horwood LJ. Risk factors and life processes associated with the onset of suicidal behaviour during adolescence and early adulthood. Psychol Med. 2000;30:23–39. doi: 10.1017/s003329179900135x. [DOI] [PubMed] [Google Scholar]
- 7.Shaffer D, Craft L. Methods of adolescent suicide prevention. J Clin Psychiatry. 1999;60:70–4. [PubMed] [Google Scholar]
- 8.Shields LB, Hunsaker DM, Hunsaker JC. Adolescent and young adult suicide: a 10-year retrospective review of Kentucky medical examiner cases. J Forensic Sci. 2006;51:874–9. doi: 10.1111/j.1556-4029.2006.00164.x. [DOI] [PubMed] [Google Scholar]
- 9.King CA, Ghaziuddin N, McGovern L, Brand E, Hill E, Naylor M. Predictors of comorbid alcohol and substance abuse in depressed adolescents. J Am Acad Child Adolesc Psychiatry. 1996;35:743–51. doi: 10.1097/00004583-199606000-00014. [DOI] [PubMed] [Google Scholar]
- 10.King CA, Naylor MW, Hill EM, Shain BN, Greden JF. Dysthymia characteristic of heavy alcohol use in depressed adolescents. Biol Psychiatry. 1993;33:210–2. doi: 10.1016/0006-3223(93)90142-z. [DOI] [PubMed] [Google Scholar]
- 11.Rohde P, Lewinsohn PM, Seeley JR. Psychiatric comorbidity with problematic alcohol use in high school students. J Am Acad Child Adolesc Psychiatry. 1996;35:101–9. doi: 10.1097/00004583-199601000-00018. [DOI] [PubMed] [Google Scholar]
- 12.Wagner BM, Cole RE, Schwartzman P. Comorbidity of symptoms among junior and senior high school suicide attempters. Suicide Life Threat Behav. 1996;26:300–7. [PubMed] [Google Scholar]
- 13.Bukstein OG, Brent DA, Perper JA, et al. Risk factors for completed suicide among adolescents with a lifetime history of substance abuse: a case-control study. Acta Psychiatr Scand. 1993;88:403–8. doi: 10.1111/j.1600-0447.1993.tb03481.x. [DOI] [PubMed] [Google Scholar]
- 14.Shaffer D, Gould MS, Fisher P, Trautman P. Psychiatric diagnosis in child and adolescent suicide. Arch Gen Psychiatry. 1996;53:339–48. doi: 10.1001/archpsyc.1996.01830040075012. [DOI] [PubMed] [Google Scholar]
- 15.Tanney BL. Psychiatric diagnosis and suicidal acts. In: Maris RW, Berman AL, Silverman MM, editors. Comprehensive Textbook of Suicidology. Guilford Press; New York, NY: 2000. pp. 311–41. [Google Scholar]
- 16.Britto MT, Klostermann BK, Bonny AE, Altum SA, Hornung RW. Impact of a school-based intervention on access to healthcare for underserved youth. J Adolesc Health. 2001;29:116–24. doi: 10.1016/s1054-139x(01)00196-3. [DOI] [PubMed] [Google Scholar]
- 17.Wilson KM, Klein JD. Adolescents who use the emergency department as their usual source of care. Arch Pediatr Adolesc Med. 2000;154:361–5. doi: 10.1001/archpedi.154.4.361. [DOI] [PubMed] [Google Scholar]
- 18.Gairin I, House A, Owens D. Attendance at the accident and emergency department in the year before suicide: retrospective study. Br J Psychiatry. 2003;183:28–33. doi: 10.1192/bjp.183.1.28. [DOI] [PubMed] [Google Scholar]
- 19.American Academy of Child and Adolescent Psychiatry Practice parameter for the assessment and treatment of children and adolescents with substance use disorders. J Am Acad Child Adolesc Psychiatry. 2005;44:609–21. doi: 10.1097/01.chi.0000159135.33706.37. [DOI] [PubMed] [Google Scholar]
- 20.Compton SN, March JS, Brent DA, Albano AM, Weersing VR, Curry J. Cognitive-behavioral psychotherapy for anxiety and depressive disorders in children and adolescents: an evidence-based medicine review. J Am Acad Child Adolesc Psychiatry. 2004;43:930–59. doi: 10.1097/01.chi.0000127589.57468.bf. [DOI] [PubMed] [Google Scholar]
- 21.Lewinsohn PM, Clarke GN, Hops H, Andrews JA. Cognitive-behavioral treatment for depressed adolescents. Behav Ther. 1990;21:385–401. [Google Scholar]
- 22.Mufson LH, Dorta KP, Wickramaratne P, Nomura Y, Olfson M, Myrna MW. A randomized effectiveness trial of interpersonal psychotherapy for depressed adolescents. Arch Gen Psychiatry. 2004;61:577–84. doi: 10.1001/archpsyc.61.6.577. [DOI] [PubMed] [Google Scholar]
- 23.Rohde P, Clarke GN, Mace DE, Jorgensen JS, Seeley JR. An efficacy/effectiveness study of cognitive-behavioral treatment for adolescents with comorbid major depression and conduct disorder. J Am Acad Child Adolesc Psychiatry. 2004;43:660–8. doi: 10.1097/01.chi.0000121067.29744.41. [DOI] [PubMed] [Google Scholar]
- 24.Rossello J, Bernal G. The efficacy of cognitive-behavioral and interpersonal treatments for depression in Puerto Rican adolescents. J Consult Clin Psychol. 1999;67:734–45. doi: 10.1037//0022-006x.67.5.734. [DOI] [PubMed] [Google Scholar]
- 25.Treatment for Adolescent Study Team Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: treatment for adolescents with depression study (TADS) randomized controlled trial. JAMA. 2004;292:807–20. doi: 10.1001/jama.292.7.807. [DOI] [PubMed] [Google Scholar]
- 26.Rutman MS, Shenassa E, Becker B. Brief screening for adolescent depressive symptoms in the emergency department. Acad Emerg Med. 2008;15:17–22. doi: 10.1111/j.1553-2712.2007.00002.x. [DOI] [PubMed] [Google Scholar]
- 27.Scott EG, Luxmore B, Alexander H, Fenn RL, Christopher NC. Screening for adolescent depression in a pediatric emergency department. Acad Emerg Med. 2006;13:537–42. doi: 10.1197/j.aem.2005.11.085. [DOI] [PubMed] [Google Scholar]
- 28.Horowitz LM, Wang PS, Koocher GP, et al. Detecting suicide risk in a pediatric emergency department: development of a brief screening tool. Pediatrics. 2001;107:1133–7. doi: 10.1542/peds.107.5.1133. [DOI] [PubMed] [Google Scholar]
- 29.Wintersteen M, Diamond G, Fein J. Screening for suicide risk in the pediatric emergency and acute care setting. Curr Opin Pediatr. 2007;19:398–404. doi: 10.1097/MOP.0b013e328220e997. [DOI] [PubMed] [Google Scholar]
- 30.Reynolds WM. RADS-2, Reynolds Adolescent Depression Scale, 2nd ed., Professional Manual. Psychological Assessment Resource Inc.; Lutz, FL: 2002. [Google Scholar]
- 31.Reynolds WM. Suicidal Ideation Questionnaire: Professional Manual. Psychological Assessment Resources; Odessa, FL: 1988. [Google Scholar]
- 32.Reynolds WM. Ann Meet Am Assoc Suicidology. Chicago, IL: 1992. Measurement of suicidal ideation in adolescents. [Google Scholar]
- 33.King CA, Hovey JD, Brand E, Wilson R. Suicidal adolescents after hospitalization: parent and family impacts on treatment follow-through. J Am Acad Child Adolesc Psychiatry. 1997;36:85–93. doi: 10.1097/00004583-199701000-00021. [DOI] [PubMed] [Google Scholar]
- 34.Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption–II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 35.Chung T, Colby SM, Barnett NP, Monti PM. Alcohol use disorders identification test: factor structure in an adolescent emergency department sample. Alcohol Clin Exp Res. 2002;26:223–31. [PubMed] [Google Scholar]
- 36.Lewinsohn PM, Rohde P, Seeley JR, Baldwin CL. Gender differences in suicide attempts from adolescence to young adulthood. J Am Acad Child Adolesc Psychiatry. 2001;40:427–34. doi: 10.1097/00004583-200104000-00011. [DOI] [PubMed] [Google Scholar]
- 37.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care. World Health Organization; Geneva, Switzerland: 2001. [Google Scholar]
- 38.Kelly TM, Donovan JE. Confirmatory factor analyses of the alcohol use disorders identification test (AUDIT) among adolescents treated in emergency departments. J Stud Alcohol. 2001;62:838–42. doi: 10.15288/jsa.2001.62.838. [DOI] [PubMed] [Google Scholar]
- 39.Rahdert ER. The Adolescent Assessment/Referral System Manual. U.S. Department of Health and Human Services, Alcohol, Drug Abuse, and Mental Health Administration; Rockville, MD: 1991. [Google Scholar]
- 40.Knight JR, Sherritt L, Harris SK, Gates EC, Chang G. Validity of brief alcohol screening tests among adolescents: a comparison of the AUDIT, POSIT, CAGE, and CRAFFT. Alcohol Clin Exp Res. 2003;27:67–73. doi: 10.1097/01.ALC.0000046598.59317.3A. [DOI] [PubMed] [Google Scholar]
- 41.Beck AT, Brown GK, Berchick RJ, Stewart BL, Steer RA. Relationship between hopelessness and ultimate suicide: a replication with psychiatric outpatients. Am J Psychiatry. 1990;147:190–5. doi: 10.1176/ajp.147.2.190. [DOI] [PubMed] [Google Scholar]
- 42.Beck AT, Steer RA, Kovacs M, Garrison B. Hopelessness and eventual suicide: a 10-year prospective study of patients hospitalized with suicidal ideation. Am J Psychiatry. 1985;142:559–63. doi: 10.1176/ajp.142.5.559. [DOI] [PubMed] [Google Scholar]
- 43.Huth-Bocks AC, Kerr DCR, Ivey AZ, Kramer AC, King CA. Assessment of psychiatrically hospitalized suicidal adolescents: self-report instruments as predictors of suicidal thoughts and behavior. J Am Acad Child Adolesc Psychiatry. 2007;46:387–95. doi: 10.1097/chi.0b013e31802b9535. [DOI] [PubMed] [Google Scholar]
- 44.Goldston DB. Measuring suicidal behavior and risk in children and adolescents. American Psychological Association; Washington, DC: 2003. [Google Scholar]
- 45.Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt Impulsiveness Scale. J Clin Psychol. 1995;51:768–74. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 46.Gilbert EH, Lowenstein SR, Koziol-McLain J, Barta DC, Steiner J. Chart reviews in emergency medicine research: where are the methods? Ann Emerg Med. 1996;27:305–8. doi: 10.1016/s0196-0644(96)70264-0. [DOI] [PubMed] [Google Scholar]
- 47.O'Carroll PW, Berman A, Maris RW, Moscicki EK. Beyond the tower of Babel: a nomenclature for suicidology. Suicide Life Threat Behav. 1996;26:237–52. [PubMed] [Google Scholar]
- 48.Silverman MM, O'Carroll PW, Joiner TE, Berman AL, Sanddal ND. Rebuilding the tower of Babel: a revised nomenclature for the study of suicide and suicidal behaviors. Part 2: suicide-related ideations, communications, and behaviors. Suicide Life Threat Behav. 2007;37:264–77. doi: 10.1521/suli.2007.37.3.264. [DOI] [PubMed] [Google Scholar]
- 49.Steer RA, Kumar G, Beck AT. Self-reported suicidal ideation in adolescent psychiatric inpatients. J Consult Clin Psychol. 1993;61:1096–9. doi: 10.1037//0022-006x.61.6.1096. [DOI] [PubMed] [Google Scholar]
- 50.Lewinsohn PM, Rohde P, Seeley JR. Adolescent suicidal ideation and attempts: prevalence, risk factors, and clinical implications. Clin Psychol Sci Pract. 1996;3:25–46. [Google Scholar]
- 51.Marcell AV, Klein JD, Fischer I, Allan MJ, Kokotailo PK. Male adolescent use of health care services: where are the boys? J Adolesc Health. 2002;30:35–43. doi: 10.1016/s1054-139x(01)00319-6. [DOI] [PubMed] [Google Scholar]
- 52.Goldston DB, Daniel SS, Reboussin DM, Reboussin BA, Frazier PH, Kelley AE. Suicide attempts among formerly hospitalized adolescents: a prospective naturalistic study of risk during the first 5 years after discharge. J Am Acad Child Adolesc Psychiatry. 1999;38:660–71. doi: 10.1097/00004583-199906000-00012. [DOI] [PubMed] [Google Scholar]
- 53.Shaffer D. The epidemiology of teen suicide: an examination of risk factors. J Clin Psychiatry. 1988;49:36–41. [PubMed] [Google Scholar]