Abstract
Cerebral palsy (CP) is one of the most frequent causes of child disability in developed countries. Children with CP need lifelong assistance and care. The current prevalence of CP in industrialized countries ranges from 1.5 to 2.5 per 1,000 live births, with one new case every 500 live births. Children with CP have an almost normal life expectancy and mortality is very low. Despite the low mortality rate, 5%–10% of them die during childhood, especially when the severe motor disability is comorbid with epilepsy and severe intellectual disability. Given this life expectancy, children with CP present with a lifelong disability of varying severity and complexity, which requires individualized pathways of care. There are no specific treatments that can remediate the brain damage responsible for the complex clinical–functional dysfunctions typical of CP. There are, however, a number of interventions (eg, neurorehabilitation, functional orthopedic surgery, medication, etc) aimed at limiting the damage secondary to the brain insult and improving these patients’ activity level and participation and, therefore, their quality of life. The extreme variability of clinical aspects and the complexity of affected functions determine a multifaceted skill development in children with CP. There is a need to provide them with long-term care, taking into account medical and social aspects as well as rehabilitation, education, and assistance. This long-term care must be suited according to children’s developmental stage and their physical, psychological, and social development within their life contexts. This impacts heavily on the national health systems which must set up a network of services for children with CP, and it also impacts heavily on the family as a whole, due to the resulting distress, adjustment efforts, and changes in quality of life. This contribution is a narrative review of the current literature on long-term care for children with CP, aiming at suggesting reflections to improve these children’s care.
Keywords: cerebral palsy, rehabilitation, long-term care, disability
Introduction
Cerebral palsy (CP) is one of the most frequent causes of child disability in developed countries. Children with CP need lifelong assistance and care. The current prevalence of CP in industrialized countries ranges from 1.5 to 2.5 per 1,000 live births, with one new case every 500 live births.1,2 Children with CP have an almost normal life expectancy and mortality is very low. Despite the low mortality rate, 5%–10% of them die during childhood, especially when the severe motor disability is comorbid with epilepsy and severe intellectual disability.3–5 Given this life expectancy, children with CP present with a lifelong disability of varying severity and complexity which requires individualized pathways of care. CP is an umbrella term for the following:
a group of disorders of the development of movement and posture, causing activity limitation, attributed to nonprogressive disturbances, occurred in the developing fetal/infant brain. The motor disorders are often accompanied by disturbances of sensation, perception, cognition, communication, behaviour, epilepsy, and musculoskeletal problems.6
This condition is due to alterations in the central nervous system due to pre-, peri-, and postnatal events before its development is complete.7–9 There are several classifications of CP based on factors such as type of tonus, distribution of impairments, and level of independence (Table 1).6,8,10,11 Today, the prevailing trend in clinical practice is to classify CP by functional independence in terms of gross motor function, fine motor function, communication ability, and eating and drinking ability. Four classifications reflect this trend. The Gross Motor Function Classification System-Expanded and Revised and the Manual Abilities Classification System were developed to characterize mobility and manual function in CP, respectively, based on the severity of motor functioning/performance impairments.12–14 More recently, two other classification systems were proposed: the Communication Function Classification System, which is used to characterize the daily communication abilities of children with CP, and the Eating and Drinking Ability Classification System, which provides a valid and reliable system for classifying the eating and drinking performance of people with CP.15–17 The Gross Motor Function Classification System-Expanded and Revised, the Manual Abilities Classification System, the Communication Function Classification System, and the Eating and Drinking Ability Classification System were designed to clearly delineate the functional profile of children with CP by focusing on activity and participation levels, as described in the World Health Organization’s International Classification of Functioning, Disability, and Health (ICF) and in the ICF Children and Youth Version (ICF-CY).18–21 These measures classify people with CP by functional independence on a five-level scale, ranging from level I =independence to level V =complete assistance (Table 2).
Table 1.
Classifications of CP based on type of tonus and distribution of impairments
| Type of tonus approach | Topographical approach | |
|---|---|---|
| Spastic | Monoplegia | Unilateral |
| Ataxic | Hemiplegia | Bilateral |
| Dyskinetic | Diplegia | |
| Dystonic | Triplegia | |
| Choreoathetotic | Quadriplegia | |
Abbreviation: CP, cerebral palsy.
Table 2.
Functional classifications for cerebral palsy
| Level I | Level II | Level III | Level IV | Level V | |
|---|---|---|---|---|---|
| GMFCS | Can walk without limitations | Walk with limitations | Walk with assistive mobility device | Walking ability severely limited even with assistive devices. Use of power wheelchair | Transported by manual wheelchair |
| MACS | Handles objects easily and successfully | Handles most objects, but with somewhat reduced quality and/or speed of achievement | Handles objects with difficulty; needs help to prepare and/or modify activities | Handles a limited selection of easily managed objects in adapted situations | Does not handle objects and has severely limited ability to perform even simple actions |
| CFCS | Effective sender and receiver with unfamiliar and familiar partners | Effective but slower-paced sender and/or receiver with unfamiliar and familiar partners | Effective sender and receiver with familiar partners | Sometimes effective sender and receiver with familiar partners | Seldom effective sender and receiver even with familiar partners |
| EDACS | Eats and drinks safely and efficiently | Eats and drinks safely, but with some limitations to efficiency | Eats and drinks with some limitations to safety; there may be limitations to efficiency | Eats and drinks with significant limitations to safety | Unable to eat or drink safely – tube feeding may be considered to provide nutrition |
Note: Copyright ©2014. Elsevier Ltd. Adapted from Compagnone E, Maniglio J, Camposeo S, et al. Functional classifications for cerebral palsy: correlations between the gross motor function classification system (GMFCS), the manual ability classification system (MACS) and the communication function classification system (CFCS). Res Dev Disabil. 2014;35(11):2651–657.19
Abbreviations: CFCS, Communication Function Classification System; EDACS, Eating and Drinking Ability Classification System; GMFCS, Gross Motor Function Classification System-Expanded and Revised; MACS, Manual Abilities Classification System.
There are no specific treatments that can remediate the brain damage responsible for the complex clinical–functional dysfunctions typical of CP. There are, however, a number of interventions (eg, neurorehabilitation, functional orthopedic surgery, medication, aids and devices, etc) aimed at limiting the damage secondary to the brain insult and improving these patients’ activity level and participation and, therefore, their quality of life (Table 3).22,23 The extreme variability of clinical aspects and the complexity of affected functions determine a multifaceted skill development in children with CP. Thus, there is a need to provide them with long-term care, taking into account medical and social aspects as well as rehabilitation, education, and assistance. This long-term care must be suited according to children’s developmental stage and their physical, psychological, and social development within their life contexts.24 This impacts heavily on the national health systems which need to set up a network of services for children with CP, and it also impacts heavily on the family as a whole, due to the resulting distress, adjustment efforts, and changes in quality of life. This contribution is a review of the current literature on long-term care for children with CP, aiming at suggesting strategies to improve these children’s care.
Table 3.
Interventions for cerebral palsy
| Rehabilitative interventions | Bimanual therapy Constraint-induced movement therapy Goal-directed training Occupational therapy Home programs for improving motor activity performance and/or self-care Robotic rehabilitation (for arm and leg training) Virtual reality rehabilitation |
| Spasticity management | Baclofen (oral format or intrathecal baclofen) BoNT Diazepam Selective dorsal rhizotomy Orthopedic surgery Single-event multilevel surgery Hip surveillance for maintaining hip joint integrity Orthoses and casting |
| Other movement disorders management:dystonia | Anticholinergic medications (eg, trihexiphenidyl), tetrabenazine, benzodiazepines (eg, diazepam), and baclofen DBS |
| Cognitive behavior and social skills interventions | Behavior therapy and coaching; cognitive behavior therapy Communication training (alternative and augmentative communication) Parent training Counseling |
| Comorbidities interventions | Management of epilepsy (antiepileptic drugs, VNS) Nutritional management, reflux management, swallowing safety, and drooling (eg, dysphagia management, fundoplication, percutaneous endoscopic gastrostomy/jejunostomy) Pain management Bone health management (bisphosphonate medication, vitamin D) Management of bladder dysfunction (urinary retention and incontinence) and bowel dysfunction (constipation and soiling) Management of respiratory complications Management of visual and hearing impairment |
| Environmental interventions | Assistive technology and assistive devices (eg, wheelchairs, robotics, and communication devices), ECS, and HAS |
Abbreviations: BoNT, botulinum toxin; DBS, deep brain stimulation; ECS, environmental control systems; HAS, home automation systems; VNS, vagus nerve stimulation.
Methods
The review is based on a comprehensive literature review. We undertook a comprehensive literature search using the following online databases: PubMed, Medline, ProQuest, and Scopus. Our aim was to identify original research papers that explored rehabilitation in CP. Search terms used to identify literature included: rehabilitation, multidisciplinary, care, disability, “quality of life”, all in combination with “cerebral palsy”. We applied these search terms to title and abstracts in all databases. There was no date restriction for any of the searches, and studies using any methodological approach were considered. A selection process by relevance to each of the domains selected was conducted by the authors, aiming at a narrative review and not a systematic literature review. The final number of studies included in this narrative review is 48.
Multidisciplinary rehabilitation
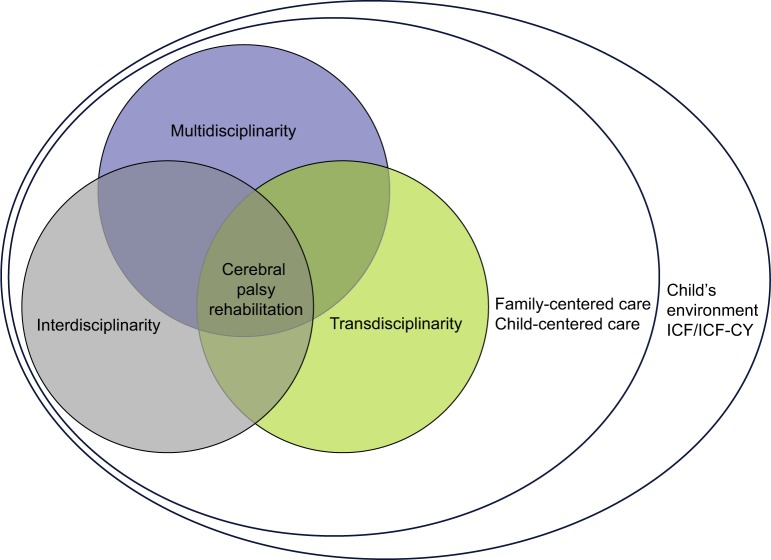
Multidisciplinary rehabilitation is now considered the key approach in rehabilitation and health care paradigms. Also, if this is generally true, it is of fundamental importance in the rehabilitation of CP. CP rehabilitation is a complex process aiming at ensuring children and their families the best possible quality of life. By acting both directly and indirectly, CP rehabilitation considers the individual under all physical, mental, emotional, communicative, and relational aspects (holistic feature) and involves their familial, social, and environmental context (ecological feature) too. Rehabilitation consists of a number of integrated interventions in the fields of remediation, education, and care.25 This holistic and ecological approach is supported by the World Health Organization’s ICF. The adult version of the ICF, published in 2001, and the child and adolescent version (ICF-CY), published in 2007, are biopsychosocial models which are increasingly being recognized as an efficacious tool to describe health and disability and a framework for planning and monitoring rehabilitation interventions over time.20,21 The ICF and the ICF-CY classify the outcome of a condition (disorder or illness) in terms of body functions/structures, activity level, and participation, underlying the need for a global pathway of care through the involvement of many stakeholders and moving from a multidisciplinary perspective only to an integrated multi-, inter-, and transdisciplinary perspective. The ICF is a sort of common language guiding this approach. Many published studies stress the importance of implementation of the ICF in the global management of pathways of care in CP.26,27 While multidisciplinarity in CP rehabilitation relies on practitioners’ knowledge from various disciplines (neurologist, physiatrist, ophthalmologist, pediatrician, psychologist, speech therapists, educator, etc), each operating within their own field of competence, interdisciplinarity integrates, subsumes, and harmonizes the connections between the different disciplines in a coordinated and consistent manner to support the development of a life project for children with CP.26 However, according to the biopsychosocial model underlying the ICF, the added value of this approach is transdisciplinarity, namely, a perspective integrating the natural, social, and health sciences in a humanities context, and in so doing, enabling each to transcend their traditional boundaries.28 But the actual value of transdisciplinarity is its going over and above multi- and interdisciplinary models, as it acts as a common thread for people from different disciplines who collaborate toward a common goal and, in order to achieve it, develop a common framework. Transdisciplinarity combines multi- and interdisciplinarity with a participative approach, is able to generate new knowledge, and sets a holistic approach to CP rehabilitation in which all stakeholders set aside their own specific perspectives to embrace a global one that is respectful of all individual instances and make a better contribution to optimal long-term care of children with CP (Figure 1).
Figure 1.
Multi-inter-transdisciplinary approach for cerebral palsy.
Abbreviations: ICF, International Classification of Functioning, Disability, and Health; ICF-CY, ICF Children and Youth Version.
The role of the family: family-centered care (FCC)
Many studies focus on the central role of the family in the long-term care of children with CP and consider the family part of a multi-inter-transdisciplinary approach. Today, FCC is considered the best approach in CP rehabilitation.29,30 Devised by the Association for the Care of Children’s Health,31 it focuses on the daily needs of children with CP, views parents as key resources for their children’s lives, supports the idea that families and practitioners should collaborate within a child’s rehabilitation program, that practitioners should support parents in coping with their responsibilities, and that effective interventions by services and facilities must be based on the values, preferences, priorities, and needs of families.32 According to the FCC approach, the primary aim of long-term care is improving the child and the family’s quality of life, increasing the parents’ satisfaction with, and their involvement in, the rehabilitation program, as they are the ones who know their child’s needs and abilities better. Improving long-term care by putting the family at the center of this approach means recognizing their central role in the child’s development and in the successful outcome of rehabilitation, as well as their knowledge of their child’s needs.33 This shows how the family fits into multi-inter-transdisciplinary care delivery and collaborates with other stakeholders in the health care decision making. This approach helps relieve the parents’ distress and improve their perception of the care their child is receiving. Clarifying and valuing their parental role improves compliance with the practitioners’ instructions.
The role of the child with CP: child-centered care
Besides the FCC, which, in the literature, is considered the best approach to the care of children with CP, the role of children with CP across developmental stages is relevant too. A child-centered approach enables us not to lose sight of the main recipient of care, namely, children with CP, and to widen the spatial and temporal frame of care delivery targeted to the real needs of these children.25 This way, children with CP and their families are recognized in their central role and families become involved in a rehabilitation program aimed at delivering the children the best possible opportunities in terms of health care, improving their activity level and participation, and improving their quality of life. The needs of children with CP are recognized and taken into account, as are their difficulties, achievements, and developmental stages, knowing that the objectives of care delivery can and must change according to age, life contexts, and environment.24 A child-centered approach sets personalized and individually targeted objectives.
The role of the environment
The environment plays a fundamental role in CP rehabilitation. Both the ICF and the ICF-CY stress the importance of its role for health.20,21 Every individual, given their health status, can live in an environment limiting or impacting their functional skills and social participation. The ICF correlates health status and environment and promotes a measurement system for health, skills, and difficulties, which allows for identification of obstacles to be removed or interventions to be implemented, so as to help individuals in their self-realization. In children with CP, development, functioning, activity level, and participation are all part of a dynamic process depending on a constant interaction with the family or other caregivers in the immediate social environment. For this reason, in order to understand their functioning, one must observe them within the family and in their own environment.26 By environment, we are not only referring to a physical, social, and psychological dimension, but to contexts where rehabilitation takes place across, updating the rehabilitation program according to the child’s achievements and using aids and devices according to their residual functions and their activity level and participation.
The role of aids and technologies
In recent years, there has been a change in CP rehabilitation due to the progressive integration of high-tech aids (robots, virtual reality, exoskeleton, telemedicine, e-health, etc) in rehabilitation practice and care delivery.22,34–37 Many studies have focused on the aids–therapist–patient relationship and relevant variables, each time stressing the role and the greater relevance of a variable as compared to others.38 However, they all support the view that the therapist–patient relationship is important, and aids are useful if used within this relationship. The term “relationship” refers to a connection between two individuals, “something” that ties them and by which they interact. Of course, any aids can support this interaction, but they can neither replace it nor induce any changes. The therapist–patient relationship defines the time and space of change; it is what supports change, and within it, any aids can be used by the therapist or the patient in order to achieve it. On the other hand, aids are defined as “any item, piece of equipment or system commonly used to increase, maintain or improve functional capabilities of people with disability”.39 Use of aids always raises a concern that the therapist–patient relationship may lose its relevance, with attention shifting to aids, their structure, usefulness, and technical perfection. Aids must then be looked at from within a three-way relationship formed by the patient with CP, the caregiver, and the family, who plays a central role in the child’s development and is crucial for a successful outcome. Shifting attention toward a concept of relationship understood as the context where a specific aid expresses its potential for change requires all stakeholders to demonstrate commitment and responsibility for one’s training, growth, and self-fulfillment – and also to give priority to individuals over aids.40
Conclusion
CP rehabilitation is a complex issue, owing to a number of factors. First of all, it is a complex issue as the umbrella term “cerebral palsy” subsumes a number of clinical pictures, because of the difficulties faced by people with CP in terms of facilitating function and inclusion, minimizing “activity limitation”, and enabling individual “participation”, and because complex is the subject of our action, that is, the child with its development dynamics, which becomes an adolescent and then adult, that grows and develops together with the disease. Ultimately, it is a complex issue because people with CP need long-term care owing to their varied needs. There are several axes that can help us draw some conclusions based on the published literature.
A “temporal axis” is defined as the time of care. Multidisciplinarity becomes integrated with interdisciplinarity and transdisciplinarity because rehabilitation lasts a lifetime. As CP is a lifelong condition, habilitation/rehabilitation must start as early as possible and be delivered continuously – at least in the child’s first years of life – and intensively – according to individual needs – and be aimed at promoting skills that will support social participation and integration in adult life.24 Some published studies41–44 have pointed out how the term “infantile”, which is often associated to CP, had an impact on habilitation/rehabilitation plans in the past. Outcome studies confirm the influence that several variables have on social participation, such as severity of motor deficits, and presence of epilepsy or mental retardation. According to the literature, groups of young adults and adults with CP have reduced independence and social life.45,46 This means that, when devising therapeutic plans, a long-term perspective must be taken, so as to help these children lead a social life in the future that is as rewarding as possible given their capacities.
A “spatial axis” is defined as environments and contexts. All the environments and contexts where the patient with CP lives (ecological perspective) must be taken into account. Family, school, social gathering places, and the individual space must all be considered in the habilitation and rehabilitation plan. The individual–environment relationship can have positive outcomes (integration and participation) as well as negative ones (withdrawal, disability, difficulties), confirming the operational definition of “disability” that can be found in the ICF-CY and ICF: “Disability is characterized as the outcome or result of a complex relationship between an individual’s health condition and personal factors, and of the external factors that represent the circumstances in which the individual lives”.20,21
An “individual axis” is defined as the person’s functioning in his globality, focusing on the individual as a whole. In the literature, motor aspects are attributed more importance than other factors such as motivation, emotions, and decision making. However, all these factors are essential for subjective and relational well-being. Since the beginning, rehabilitation must look at the individual as an active player, and not as a passive recipient of care.
A “relational axis” is defined as the quality of interpersonal relationships. In this axis, the focus is on people who, in different roles, take care of the patient with CP. A consistent focus on the patient with CP is instrumental to a multi-inter-transdisciplinary intervention. A consistent focus implies that different people in different roles share the same “existential theory” on the patient with CP: “When we provide care, rehabilitation and assistance, we do this based on a conceptual model of man, although we are not aware of this most of the time”.47 Being aware that the patient with CP is the leading player in the relationship ensures long-term care plans with clear objectives and strategies.
The few studies on CP outcomes are not reassuring as they report a higher rate of psychopathological problems, pain, motor disability, and distress felt by patient and family with a lower quality of life than in other conditions.46,48 This raises questions on the effectiveness of habilitation and rehabilitation plans for CP.
Figure 2 provides guidance for planning interventions centered on the subjective and relational well-being of patients with CP. A consistent focus moves away from the concept that CP is a clinical condition mainly resulting in a motor limitation. A consistent focus shares the view that CP is a lifelong condition, impacting all dimensions, individual variables, and people to the relationship. A consistent focus promotes forward-looking habilitation and rehabilitation plans, interventions in all life contexts (from school in childhood to the workplace in adult life), an approach involving all aspects of individual life, including motivation and emotions, and a constant exchange with all the people to the relationship. A consistent focus can help shape habilitation and rehabilitation in order to promote the patient’s adjustment, participation, and subjective and relational well-being.
Figure 2.
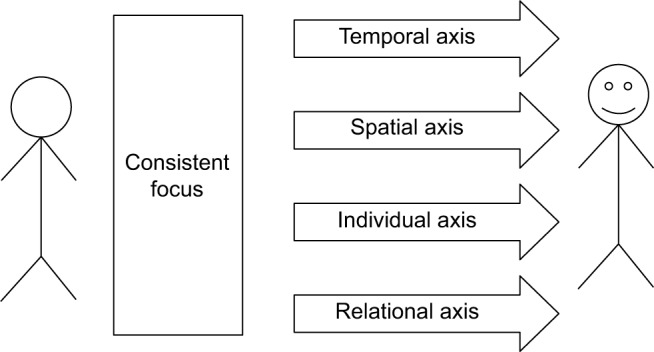
Guidance for planning interventions.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Oskoui M, Coutinho F, Dykeman J, Jette N, Pringsheim T. An update on the prevalence of cerebral palsy: a systematic review and meta-analysis. Dev Med Child Neurol. 2013;55(6):509–519. doi: 10.1111/dmcn.12080. [DOI] [PubMed] [Google Scholar]
- 2.Surman G, Hemming K, Platt MJ, Parkes J, Green A, Hutton J, Kurinczuk JJ. Children with cerebral palsy: severity and trends over time. Paediatr Perinat Epidemiol. 2009;23(6):513–521. doi: 10.1111/j.1365-3016.2009.01060.x. [DOI] [PubMed] [Google Scholar]
- 3.Novak I. Evidence-based diagnosis, health care, and rehabilitation for children with cerebral palsy. J Child Neurol. 2014;29(8):1141–1156. doi: 10.1177/0883073814535503. [DOI] [PubMed] [Google Scholar]
- 4.Strauss D, Shavelle R, Reynolds R, Rosenbloom L, Day S. Survival in cerebral palsy in the last 20 years: signs of improvement? Dev Med Child Neurol. 2007;49(2):86–92. doi: 10.1111/j.1469-8749.2007.00086.x. [DOI] [PubMed] [Google Scholar]
- 5.Westbom L, Bergstrand L, Wagner P, Nordmark E. Survival at 19 years of age in a total population of children and young people with cerebral palsy. Dev Med Child Neurol. 2011;53(9):808–814. doi: 10.1111/j.1469-8749.2011.04027.x. [DOI] [PubMed] [Google Scholar]
- 6.Rosenbaum P, Paneth N, Leviton A, et al. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl. 2007;109:8–14. [PubMed] [Google Scholar]
- 7.Bax M, Goldstein M, Rosenbaum P, et al. Proposed definition and classification of cerebral palsy, April 2005. Dev Med Child Neurol. 2005;47(8):571–576. doi: 10.1017/s001216220500112x. [DOI] [PubMed] [Google Scholar]
- 8.Bax MC. Terminology and classification of cerebral palsy. Dev Med Child Neurol. 1964;6:295–297. doi: 10.1111/j.1469-8749.1964.tb10791.x. [DOI] [PubMed] [Google Scholar]
- 9.Mutch L, Alberman E, Hagberg B, Kodama K, Perat MV. Cerebral palsy epidemiology: where are we now and where are we going? Dev Med Child Neurol. 1992;34(6):547–551. doi: 10.1111/j.1469-8749.1992.tb11479.x. [DOI] [PubMed] [Google Scholar]
- 10.Hagberg B, Hagberg G, Olow I. The changing panorama of cerebral palsy in Sweden 1954–1970. I. Analysis of the general changes. Acta Paediatr Scand. 1975;64(2):187–192. doi: 10.1111/j.1651-2227.1975.tb03820.x. [DOI] [PubMed] [Google Scholar]
- 11.Hagberg G, Hagberg G, Olow I. The changing panorama of cerebral palsy in Sweden 1954–1970. II. Analysis of the various syndromes. Acta Paediatr Scand. 1975;64(2):193–200. doi: 10.1111/j.1651-2227.1975.tb03821.x. [DOI] [PubMed] [Google Scholar]
- 12.Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39(4):214–223. doi: 10.1111/j.1469-8749.1997.tb07414.x. [DOI] [PubMed] [Google Scholar]
- 13.Palisano RJ, Rosenbaum P, Bartlett D, Livingston MH. Content validity of the expanded and revised gross motor function classification system. Dev Med Child Neurol. 2008;50(10):744–750. doi: 10.1111/j.1469-8749.2008.03089.x. [DOI] [PubMed] [Google Scholar]
- 14.Eliasson AC, Krumlinde-Sundholm L, Rosblad B, Beckung E, Arner M, Ohrvall AM, Rosenbaum P. The manual ability classification system (MACS) for children with cerebral palsy: scale development and evidence of validity and reliability. Dev Med Child Neurol. 2006;48(7):549–554. doi: 10.1017/S0012162206001162. [DOI] [PubMed] [Google Scholar]
- 15.Hidecker MJ, Paneth N, Rosenbaum PL, et al. Developing and validating the communication function classification system for individuals with cerebral palsy. Dev Med Child Neurol. 2011;53(8):704–710. doi: 10.1111/j.1469-8749.2011.03996.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Himmelmann K, Lindh K, Hidecker MJ. Communication ability in cerebral palsy: a study from the CP register of western Sweden. Eur J Paediatr Neurol. 2013;17(6):568–574. doi: 10.1016/j.ejpn.2013.04.005. [DOI] [PubMed] [Google Scholar]
- 17.Sellers D, Mandy A, Pennington L, Hankins M, Morris C. Development and reliability of a system to classify the eating and drinking ability of people with cerebral palsy. Dev Med Child Neurol. 2014;56(3):245–251. doi: 10.1111/dmcn.12352. [DOI] [PubMed] [Google Scholar]
- 18.Hidecker MJ, Ho NT, Dodge N, et al. Inter-relationships of functional status in cerebral palsy: analyzing gross motor function, manual ability, and communication function classification systems in children. Dev Med Child Neurol. 2012;54(8):737–742. doi: 10.1111/j.1469-8749.2012.04312.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Compagnone E, Maniglio J, Camposeo S, et al. Functional classifications for cerebral palsy: correlations between the gross motor function classification system (GMFCS), the manual ability classification system (MACS) and the communication function classification system (CFCS) Res Dev Disabil. 2014;35(11):2651–2657. doi: 10.1016/j.ridd.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization . International Classification of Functioning, Disability and Health: ICF. Geneva: World Health Organization; 2001. [Google Scholar]
- 21.World Health Organization . International Classification of Functioning, Disability, and Health: Children & Youth Version: ICF-CY. Geneva: World Health Organization; 2007. [Google Scholar]
- 22.Novak I, McIntyre S, Morgan C, et al. A systematic review of interventions for children with cerebral palsy: state of the evidence. Dev Med Child Neurol. 2013;55(10):885–910. doi: 10.1111/dmcn.12246. [DOI] [PubMed] [Google Scholar]
- 23.Saleh MN, Korner-Bitensky N, Snider L, Malouin F, Mazer B, Kennedy E, Roy MA. Actual vs. best practices for young children with cerebral palsy: a survey of paediatric occupational therapists and physical therapists in Quebec, Canada. Dev Neurorehabil. 2008;11(1):60–80. doi: 10.1080/17518420701544230. [DOI] [PubMed] [Google Scholar]
- 24.Fazzi E, Castelli E. Presentation of recommendations for the rehabilitation of children with cerebral palsy. Eur J Phys Rehabil Med. 2015 Dec 1; Epub. [PubMed] [Google Scholar]
- 25.Gruppo Italiano per la Paralisi Cerebrale Infantile Manifesto per la riabilitazione del bambino. MR Giornale Italiano di Medicina Riabilitativa. 2000;14(4):14–15. Italian. [Google Scholar]
- 26.Trabacca A, Russo L, Losito L, et al. The ICF-CY perspective on the neurorehabilitation of cerebral palsy: a single case study. J Child Neurol. 2012;27(2):183–190. doi: 10.1177/0883073811415852. [DOI] [PubMed] [Google Scholar]
- 27.Trabacca A, Moro G, Gennaro L, Russo L. When one plus one equals three: the ICF perspective of health and disability in the third millennium. Eur J Phys Rehabil Med. 2012;48(4):709–710. [PubMed] [Google Scholar]
- 28.Choi BC, Pak AW. Multidisciplinarity, interdisciplinarity and transdisciplinarity in health research, services, education and policy: 1. definitions, objectives, and evidence of effectiveness. Clin Invest Med. 2006;29(6):351–364. [PubMed] [Google Scholar]
- 29.Law M, Hanna S, King G, Hurley P, King S, Kertoy M, Rosenbaum P. Factors affecting family-centred service delivery for children with disabilities. Child Care Health Dev. 2003;29(5):357–366. doi: 10.1046/j.1365-2214.2003.00351.x. [DOI] [PubMed] [Google Scholar]
- 30.Dirks T, Hadders-Algra M. The role of the family in intervention of infants at high risk of cerebral palsy: a systematic analysis. Dev Med Child Neurol. 2011;53(Suppl 4):62–67. doi: 10.1111/j.1469-8749.2011.04067.x. [DOI] [PubMed] [Google Scholar]
- 31.Shelton T, Jeppson E, Johnson B. Family-Centered Care for Children with Special Health Care Needs. 2nd ed. Washington, DC: Association for the Care of Children’s Health; 1987. [Google Scholar]
- 32.King S, Teplicky R, King G, Rosenbaum P. Family-centered service for children with cerebral palsy and their families: a review of the literature. Semin Pediatr Neurol. 2004;11(1):78–86. doi: 10.1016/j.spen.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 33.Guyard A, Fauconnier J, Mermet MA, Cans C. Impact on parents of cerebral palsy in children: a literature review. Arch Pediatr. 2011;18(2):204–214. doi: 10.1016/j.arcped.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 34.Meyer-Heim A, van Hedel HJ. Robot-assisted and computer-enhanced therapies for children with cerebral palsy: current state and clinical implementation. Semin Pediatr Neurol. 2013;20(2):139–145. doi: 10.1016/j.spen.2013.06.006. [DOI] [PubMed] [Google Scholar]
- 35.Fasoli SE, Ladenheim B, Mast J, Krebs HI. New horizons for robot-assisted therapy in pediatrics. Am J Phys Med Rehabil. 2012;91(11 Suppl 3):S280–S289. doi: 10.1097/PHM.0b013e31826bcff4. [DOI] [PubMed] [Google Scholar]
- 36.Meyer-Heim A, van Hedel HJ. Robot-assisted and computer-based neurorehabilitation for children: the story behind. Praxis (Bern 1994) 2014;103(15):883–892. doi: 10.1024/1661-8157/a001725. [DOI] [PubMed] [Google Scholar]
- 37.James S, Ziviani J, King G, Boyd RN. Understanding engagement in home-based interactive computer play: perspectives of children with unilateral cerebral palsy and their caregivers. Phys Occup Ther Pediatr. 2015;25:1–15. doi: 10.3109/01942638.2015.1076560. [DOI] [PubMed] [Google Scholar]
- 38.Ferrari A. Proposte riabilitative nelle paralisi cerebrali infantili. Pisa: Edizioni Del Cerro; 1997. Italian. [Google Scholar]
- 39.Assistive Technology Act Putting technology into the hands of individuals with disabilities [updated 2004] [Accessed June 30, 2016]. Available from: http://archives.republicans.edlabor.house.gov/archive/issues/108th/education/at/billsummary.htm.
- 40.Trabacca A, Russo L. Pediatric rehabilitation: a changing panorama in the high-tech era? Eur J Phys Rehabil Med. 2016 May 10; Epub. [PubMed] [Google Scholar]
- 41.Carbonell PG. Compartmental pressure after percutaneous tenotomy of the Achilles tendon in children with infantile cerebral palsy. Childs Nerv Syst. 2015;31(2):297–300. doi: 10.1007/s00381-014-2574-5. [DOI] [PubMed] [Google Scholar]
- 42.Kozeis N, Panos GD, Zafeiriou DI, de Gottrau P, Gatzioufas Z. Comparative study of refractive errors, strabismus, microsaccades, and visual perception between preterm and full-term children with infantile cerebral palsy. J Child Neurol. 2015;30(8):972–975. doi: 10.1177/0883073814549248. [DOI] [PubMed] [Google Scholar]
- 43.Fernandez-Alcantara M, Garcia-Caro MP, Laynez-Rubio C, et al. Feelings of loss in parents of children with infantile cerebral palsy. Disabil Health J. 2015;8(1):93–101. doi: 10.1016/j.dhjo.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 44.Otapowicz D, Sobaniec W, Okurowska-Zawada B, et al. Dysphagia in children with infantile cerebral palsy. Adv Med Sci. 2010;55(2):222–227. doi: 10.2478/v10039-010-0034-3. [DOI] [PubMed] [Google Scholar]
- 45.Jiang B, Walstab J, Reid SM, Davis E, Reddihough D. Quality of life in young adults with cerebral palsy. Disabil Health J. 2016 May 3; doi: 10.1016/j.dhjo.2016.04.006. Epub. [DOI] [PubMed] [Google Scholar]
- 46.Colver A. Outcomes for people with cerebral palsy: life expectancy and quality of life. Paediatr Child Health. 2012;22(9):384–387. [Google Scholar]
- 47.Cannao M, Moretti A, editors. Riabilitazione e integrazione del disabile Dai principi ai metodi. Roma: Armando; 2006. [Google Scholar]
- 48.Roebroeck ME, Jahnsen R, Carona C, Kent RM, Chamberlain MA. Adult outcomes and lifespan issues for people with childhood-onset physical disability. Dev Med Child Neurol. 2009;51(8):670–678. doi: 10.1111/j.1469-8749.2009.03322.x. [DOI] [PubMed] [Google Scholar]