Abstract
Background: Previous studies have evaluated the associations between the cholesteryl ester transfer protein (CETP) TaqIB polymorphism (rs708272), the risk of developing composite ischemic cardiovascular disease (CVD) and the concentration of high-density lipoprotein cholesterol (HDL-C), but results remain controversial. The objective of this study was to investigate whether a relationship exists between these factors. Methods: We conducted a meta-analysis of available studies to clarify the associations of the CETP TaqIB polymorphism with HDL-C concentration and the composite ischemic CVD risk in both Asians and Caucasians. All statistical analyses were done with Stata 12.0. Results: Through utilization of the Cochrane Library, Embase, PubMed, Web of Science, Springer, China Science and Technology Journal Database, China National Knowledge Infrastructure, Google Scholar, and Baidu Library, a total of 45 studies from 44 papers with 20,866 cases and 21,298 controls were combined showing a significant association between the CETP TaqIB variant and composite ischemic CVD risk. Carriers of allele TaqIB-B1 were found to have a higher risk of composite ischemic CVD than non-carriers: OR = 1.15, 95% CI = 1.09–1.21, p < 0.001. Meanwhile, 28 studies with 23,959 subjects were included in the association between the CETP TaqIB polymorphism and the concentration of HDL-C. Results suggested that carriers of the B1B1 genotype had lower concentrations of HDL-C than those of the B2B2 genotype: SMD = 0.50, 95% CI = 0.36–0.65, p < 0.001. Conclusions: The synthesis of available evidence demonstrates that the CETP TaqIB polymorphism protects against composite ischemic CVD risk and is associated with a higher HDL-C concentration in both Asians and Caucasians.
Keywords: cholesteryl ester transfer protein, polymorphism, composite ischemic cardiovascular disease, HDL-C, meta-analysis
1. Introduction
Composite ischemic cardiovascular disease (CVD), including coronary artery disease (CAD), ischemic stroke (IS), and myocardial infarction (MI) has become a serious public health problem around the world because of their high morbidity and mortality [1,2]. However, their exact mechanisms are still unclear. For a long time, atherosclerosis (AS) has attracted attention because it is the pathological foundation of CAD, IS, and MI. Abnormal cholesterol metabolism was considered to be the main factor for atherosclerosis, and epidemiological evidence considered low concentrations of serum high-density lipoprotein cholesterol (HDL-C) to be an independent risk factor [3,4]. However, high-density lipoprotein (HDL) has now been shown to play a pivotal role in mediating the transfer of cholesterol from extra hepatic tissues to the liver and reducing the deposition of cholesterol on the artery wall [5].
Serum HDL-C concentrations are affected by many genetic and environmental factors. The cholesteryl ester transfer protein (CETP) gene located on chromosome 16q21, encodes the key plasma protein that mediates the transfer of esterified cholesterol from HDL to apolipoprotein B-containing particles in exchange for triglycerides [6,7]. Mutation of the gene may affect the transcription and expression of CETP, thereby affecting serum HDL-C concentrations [8]. The CETP TaqIB (rs708272) polymorphism is the most common polymorphism in intron 1 of the CETP gene and its mutation can affect the concentration as well as activity of plasma CETP, which affected the level of HDL-C [9]. Recently, though numerous studies have shown a relationship between the CETP TaqIB polymorphism in the synthesis of HDL-C and composite ischemic CVD risk, research has remained inconsistent, possibly due to the small sample sizes used in the individual studies.
In 2005, Boekholdt et al. performed a meta-analysis to evaluate the association the CETP TaqIB polymorphism in the synthesis of serum HDL-C and CAD risk, and demonstrated that the CETP TaqIB variant is associated with HDL-C level and CAD risk in Caucasians [10]. Li et al. also conducted a meta-analysis to evaluate the association of this variant with CAD in Chinese; however, no relationship between the CETP TaqIB polymorphism and CAD was observed [11]. Cao et al. and Wang et al. performed meta-analysis to evaluate the association the CETP TaqIB variant and MI. Their results showed that the CETP TaqIB-B2 allele protects against the development of MI [12,13]. No meta-analysis was found on the association between the CETP TaqIB polymorphism and IS. Considering the four meta-analyses above focused only on the association of the CETP TaqIB polymorphism with a single atherosclerotic disease and results were controversial in regards to ethnicity (Asians and Caucasians), we performed this meta-analysis to clarify the role of the CETP TaqIB polymorphism in the synthesis of HDL-C and the composite ischemic CVD risk.
2. Materials and Methods
2.1. Literature Search
The protocol was approved by the Institutional Ethics Review Board (IERB) of the First Affiliated Hospital of Shihezi University School of Medicine (IERB No. SHZ2010LL01). Using the standards of the Meta-analysis of Observational Studies in Epidemiology group (MOOSE) [14] and the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) [15], searches were performed using the following electronic databases: the Cochrane Library, Embase, PubMed, Web of Science, Springer, China Science and Technology Journal Database (CSTJ), China National Knowledge Infrastructure (CNKI), Google Scholar, and Baidu Library (the last search was conducted on 31 January 2016). Searches were performed using combinations of the following key words: (“cholesteryl ester transfer protein” OR “CETP”) and (“variation” OR “variant” OR “mutation” OR “polymorphism” OR “genotype”) and (“CAD” OR “coronary artery disease” OR “coronary heart disease” OR “CHD” OR “myocardial infarction” OR “MI” OR “ischemic cardiovascular disease” OR “IS”) and (“high-density lipoprotein cholesterol” OR “HDL-C” OR “blood lipid” OR “serum lipid”).
2.2. Eligibility Criteria
The eligibility criteria for the inclusion of articles in the present meta-analysis were the following: (1) The publication evaluated the associations of the CETP TaqIB polymorphism with AS or HDL-C level; (2) CAD and MI diagnosis required the result of coronary angiography, and the diagnosis of IS depended on the result of magnetic resonance imaging or computed tomography; (3) published in either Chinese or English; (4) for the composite ischemic CVD association, sufficient published data for calculating odds ratios (ORs) with their 95% confidence intervals (CIs); for HDL-C concentrations association, the population, the mean of HDL-C concentrations, and the standard deviations (SD) by genotype should be available.
2.3. Exclusion Criteria
The exclusion criteria were as follows: (1) Duplicate publications; (2) incomplete information; (3) insufficient or insignificant statistical data; (4) review articles.
2.4. Data Extraction
Two reviewers (Minghong Yao and Yusong Ding) independently screened full-length articles according to the pre-specified inclusion criteria. For the composite ischemic CVD association, the following information was extracted: name of the first author, year of publication, study population (country, ethnicity), source of controls, case/control sample size, minor allele frequency (MAF), genotype counts in the cases/controls, and evidence of Hardy-Weinberg equilibrium (HWE); for HDL-C concentrations association, name of the first author, year of publication, study population (country, ethnicity), population number, mean of HDL-C concentrations, and their SD by genotype. If key data were not presented in the relevant publications, we tried to obtain them directly from the authors of the relevant studies. When the two reviewers’ opinions differed, a third reviewer (ShuXia Guo) was asked to make final decisions regarding the results.
2.5. Quality Assessment for Individual Studies
The Newcastle-Ottawa Scale (NOS) was used to assessed the methodologic quality of the individual studies by two reviewers (Minghong Yao and Yizhong Yan) [16]. Each study was evaluated and scored based on three criteria: selection (4 stars), comparability (2 stars), and exposure (3 stars). The NOS point ranges between zero up to nine stars. Any disagreement was resolved by discussion with a third reviewer (Jiaming Liu).
2.6. Data Analysis
All statistics were analyzed in Stata 12.0 (StataCorp, College Station, TX, USA). All the tests were two-sided and a p-value of less than 0.05 was considered statistically significant. The HWE was assessed using the chi-square test. The strength of associations between the CETP TaqIB polymorphism and atherosclerosis were assessed by summary odds ratios (ORs) with 95% confidence intervals (CIs). Pooled ORs were performed for the allele contrasts as followed: (B1 allele vs. B2 allele), additive genetic model (B1B1 vs. B2B2), recessive genetic model (B1B1 vs. B1B2 + B2B2), and dominant genetic model (B1B1 + B1B2 vs. B2B2), respectively. A pooled standardized mean difference (SMDs) and its 95% CIs were used for the meta-analysis of HDL-C concentrations and the CETP TaqIB polymorphism. Heterogeneity across individual studies was calculated using the Cochran’s-Q statistic and the I2 statistic (p < 0.10 and I2 > 50% indicated evidence of heterogeneity) [17,18]. With no heterogeneity among studies, the ORs or SMDs estimate of each study was calculated by the fixed effect model (Mantel-Haenszel) [19]. Otherwise, the random effect model (DerSimonian and Laird) was used [20,21]. Subsequently, the Galbraith plot and meta-regression were performed to explore the sources of heterogeneity [22]. For the composite ischemic CVD association, subgroup analyses were performed based on ethnicity, atherosclerotic diseases, source of controls, and study type; for HDL-C association, subgroup analyses were performed based on ethnicity. Sensitivity analyses were performed based on HWE (studies without HWE were excluded) and sample size (n < 400 were excluded). Potential risk of publication bias was tested by funnel plot and Egger’s test.
3. Results
3.1. Selection and Characteristics of Studies
The present study met the PRISMA statements (Checklist S1) and MOOSE guidelines (Table S1). The study selection process is detailed in Figure 1. Through a comprehensive retrieval and evaluation, 45 studies from 44 papers with 20,866 cases and 21,298 controls met the inclusion criteria to assess the association between the CETP TaqIB polymorphism and the composite ischemic CVD [23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65]. The selected study characteristics and data are listed in Table 1. Among these studies, 28 involved CAD [23,24,25,26,27,28,29,30,31,32,34,35,36,37,38,39,44,46,47,50,52,53,54,55,59,60,61,66], three involved IS [63,64,65], and 14 involved MI [33,40,41,42,43,45,48,49,51,56,57,58,62]. In addition, there were 26 studies on Caucasians [23,24,25,27,30,38,39,40,41,42,43,44,45,47,48,50,51,53,56,57,58,60,62,63,64] and 19 studies on Asians [26,28,29,31,32,33,34,35,36,37,46,49,52,54,55,59,61,65,66]. Controls of 23 studies were hospital-based [23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,57,58,59,61,63,64,65,66], while those of the other 22 studies were population-based [38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,60,62]. Seven studies did not follow the Hardy-Weinberg equilibrium [23,35,36,40,42,43,58]. In addition, NOS results showed that the average scores were 6.8.
Figure 1.
Flow diagram of the study selection process.
Table 1.
Characteristics of individual studies included in the meta-analysis of atherosclerosis and the CETP TaqIB polymorphism.
| First Author | Year | Country | Ethnicity | Disease | Source of Controls | Study Type | Size (Case/Control) | MAF | HWE | Genotypes Distribution (Case/Control) | Score | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B1B1 | B1B2 | B2B2 | |||||||||||
| Tenkanen et al. [51] | 1991 | Finland | Caucasian | MI | PB | CS | 72/115 | 0.44 | Yes | 19/33 | 40/65 | 13/17 | 8 |
| Fumeron et al. [41] | 1995 | France | Caucasian | MI | PB | CCS | 608/724 | 0.40 | Yes | 209/258 | 312/346 | 87/120 | 8 |
| Kuivenhoven et al. [44] | 1998 | The Netherlands | Caucasian | CAD | PB | CS | 380/427 | 0.41 | Yes | 129/152 | 183/214 | 68/61 | 7 |
| Wu et al. [33] | 2001 | China | Asian | MI | HB | CCS | 149/274 | 0.46 | Yes | 45/63 | 79/159 | 25/52 | 8 |
| Arca et al. [38] | 2001 | Italy | Caucasian | CAD | PB | CCS | 408/180 | 0.41 | Yes | 153/67 | 187/77 | 68/36 | 8 |
| Eiriksdottir et al. [40] | 2001 | Iceland | Caucasian | MI | PB | CS | 378/745 | 0.45 | No | 128/194 | 191/396 | 59/155 | 8 |
| Liu et al. [45] | 2002 | USA | Caucasian | MI | PB | CS | 384/384 | 0.43 | Yes | 125/122 | 196/193 | 63/69 | 8 |
| Freeman et al. [56] | 2003 | UK | Caucasian | MI | PB | CS | 499/1105 | 0.50 | Yes | 164/239 | 259/541 | 76/225 | 8 |
| Zhang et al. [35] | 2003 | China | Asian | CAD | HB | CCS | 234/164 | 0.41 | No | 76/49 | 126/95 | 32/20 | 6 |
| Qin et al. [29] | 2004 | China | Asian | CAD | HB | CCS | 249/167 | 0.41 | Yes | 81/49 | 131/97 | 37/21 | 6 |
| Wang et al. [32] | 2004 | China | Asian | CAD | HB | CCS | 128/247 | 0.42 | Yes | 50/72 | 66/123 | 12/52 | 6 |
| Yan et al. [34] | 2004 | China | Asian | CAD | HB | CCS | 106/64 | 0.41 | Yes | 41/19 | 46/34 | 19/11 | 6 |
| Zhao et al. [36] | 2004 | China | Asian | CAD | HB | CCS | 238/203 | 0.41 | No | 95/60 | 105/109 | 38/34 | 6 |
| Zheng et al. [37] | 2004 | China | Asian | CAD | HB | CCS | 203/100 | 0.39 | Yes | 66/33 | 114/55 | 23/12 | 6 |
| Bernard et al. [43] | 2004 | UK | Caucasian | MI | PB | CCS | 4442/3273 | 0.43 | No | 1477/1100 | 2175/1527 | 790/646 | 8 |
| Yilmaz et al. [42] | 2005 | Turkey | Caucasian | MI | PB | CCS | 173/111 | 0.42 | No | 66/39 | 72/46 | 35/26 | 6 |
| Fidani et al. [63] | 2005 | Greek | Caucasian | IS | HB | CCS | 96/100 | 0.41 | Yes | 35/34 | 47/45 | 14/21 | 6 |
| Whiting et al. [53] | 2005 | USA | Caucasian | CAD | PB | CS | 2392/827 | 0.42 | Yes | 792/279 | 1200/377 | 400/171 | 8 |
| Zhang et al. [54] | 2005 | China | Asian | CAD | PB | CCS | 88/94 | 0.41 | Yes | 31/32 | 40/50 | 17/12 | 6 |
| Dedoussis et al. [57] | 2007 | Greece | Caucasian | MI | HB | CCS | 237/237 | 0.41 | Yes | 83/78 | 121/120 | 33/39 | 7 |
| Morgan et al. [58] | 2007 | USA | Caucasian | MI | HB | CCS | 805/656 | 0.44 | No | 250/224 | 387/297 | 168/135 | 6 |
| Hsieh et al. [59] | 2007 | China | Asian | CAD | HB | CCS | 101/264 | 0.31 | Yes | 19/23 | 47/111 | 35/130 | 5 |
| Quarta et al. [64] | 2007 | Italy | Caucasian | IS | HB | CCS | 215/236 | 0.43 | Yes | 79/73 | 105/108 | 31/55 | 6 |
| Muendlein et al. [27] | 2008 | Austria | Caucasian | CAD | HB | CS | 332/225 | 0.40 | Yes | 125/71 | 162/116 | 45/38 | 8 |
| Rejeb et al. [30] | 2008 | Tunisian | Caucasian | CAD | HB | CS | 212/104 | 0.41 | Yes | 104/45 | 93/47 | 15/12 | 8 |
| Meiner et al. [48] | 2008 | USA | Caucasian | MI | PB | CCS | 550/620 | 0.45 | Yes | 173/166 | 282/320 | 95/134 | 6 |
| Wang et al. [52] | 2008 | China | Asian | CAD | PB | CCS | 317/298 | 0.41 | Yes | 117/99 | 148/146 | 52/53 | 6 |
| Jensen et al. [62] a | 2008 | USA | Caucasian | MI | PB | CS | 247/486 | 0.42 | Yes | 84/166 | 120/235 | 42/85 | 8 |
| Jensen et al. [62] b | 2008 | USA | Caucasian | MI | PB | CS | 259/513 | 0.41 | Yes | 89/180 | 126/244 | 44/89 | 8 |
| Padmaja et al. [28] | 2009 | Indian | Asian | CAD | HB | CCS | 504/338 | 0.45 | Yes | 163/86 | 264/161 | 77/91 | 6 |
| Poduri et al. [49] | 2009 | India | Asian | MI | PB | CCS | 265/150 | 0.41 | Yes | 117/3 | 107/82 | 41/35 | 6 |
| Tanrikulu-Kucuk et al. [23] | 2010 | Turkey | Caucasian | CAD | HB | CCS | 135/112 | 0.46 | No | 40/33 | 71/50 | 24/29 | 6 |
| Corella et al. [39] | 2010 | Spanish | Caucasian | CAD | PB | CS | 557/1180 | 0.47 | Yes | 224/482 | 247/537 | 86/161 | 8 |
| Bhanushali et al. [66] | 2010 | Indian | Asian | CAD | HB | CCS | 90/150 | 0.46 | Yes | 33/38 | 40/77 | 17/35 | 7 |
| Kolovou et al. [25] | 2011 | Greek | Caucasian | CAD | HB | CCS | 374/96 | 0.42 | Yes | 126/22 | 202/45 | 46/29 | 6 |
| Zhang et al. [55] | 2011 | China | Asian | CAD | PB | CCS | 334/301 | 0.34 | Yes | 172/136 | 106/120 | 56/45 | 8 |
| Jiang et al. [65] | 2012 | China | Asian | IS | HB | CCS | 220/220 | 0.29 | Yes | 130/103 | 72/86 | 18/31 | 6 |
| Tayebi et al. [61] | 2012 | Singapore | Asian | CAD | HB | CCS | 659/927 | 0.45 | Yes | 228/245 | 322/491 | 109/191 | 7 |
| Lu et al. [46] | 2013 | Singapore | Asian | CAD | PB | CCS | 659/927 | 0.45 | Yes | 228/245 | 322/491 | 109/191 | 8 |
| Mehlig et al. [47] | 2014 | Sweden | Caucasian | CAD | PB | CCS | 618/2921 | 0.43 | Yes | 209/938 | 313/1420 | 96/563 | 8 |
| El-Aziz et al. [50] | 2014 | Egypt | Caucasian | CAD | PB | CCS | 116/119 | 0.46 | Yes | 38/30 | 60/57 | 18/32 | 6 |
| Kaman et al. [24] | 2015 | Turkey | Caucasian | CAD | HB | CCS | 210/100 | 0.44 | Yes | 44/29 | 81/45 | 85/26 | 6 |
| Liu et al. [26] | 2015 | China | Asian | CAD | HB | CCS | 322/108 | 0.42 | Yes | 113/40 | 145/47 | 64/21 | 6 |
| Shi et al. [31] | 2015 | China | Asian | CAD | HB | CCS | 312/88 | 0.42 | Yes | 112/29 | 138/44 | 62/15 | 6 |
| Cyrus et al. [60] | 2016 | Saudi Arabia | Caucasian | CAD | PB | CCS | 990/618 | 0.41 | Yes | 376/183 | 454/321 | 160/114 | 6 |
a: Nurses’ Health Study, b: Health Professionals Follow-up Study, USA: The United States, UK: United Kingdom, CAD: coronary artery disease, MI: myocardial infraction, IS: ischemic stroke, HB: hospital-based, PB: population-based, MAF: minor allele frequencies, HWE: Hardy-Weinberg equilibrium, CS: cohort study, CCS: case control study.
Table 2 describes the characteristics of studies included in the association between the CETP TaqIB polymorphism and serum HDL-C concentrations. A total of 28 studies with 23,959 subjects were included in the analysis [8,33,35,36,40,44,45,50,53,59,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85]. Of these, there were 11 studies on Caucasians [8,40,44,45,50,53,67,69,71,81,83] and 17 studies on Asians [33,35,36,59,68,70,72,73,74,75,76,77,78,79,80,82,84,85]. Five studies did not follow the HWE [35,72,74,76,77]. Additionally, NOS results showed that the average scores were 6.4.
Table 2.
Characteristics of individual studies included in the meta-analysis of HDL-C level and the CETP TaqIB polymorphism.
| First Author | Year | Country | Ethnicity | MAF | HWE | B1B1 | B1B2 | B2B2 | Score | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | n | Mean | SD | n | Mean | SD | n | |||||||
| Kuivenhoven et al. [44] | 1998 | The Netherlands | Caucasian | 0.41 | Yes | 0.88 | 0.21 | 281 | 0.93 | 0.21 | 397 | 1.01 | 0.26 | 129 | 7 |
| Gudnason et al. [67] | 1999 | Mixed | Caucasian | 0.44 | Yes | 1.13 | 0.21 | 237 | 1.19 | 0.24 | 380 | 1.27 | 0.22 | 150 | 7 |
| Eiriksdottir et al. [40] | 2001 | Iceland | Caucasian | 0.45 | Yes | 1.09 | 0.31 | 328 | 1.12 | 0.29 | 596 | 1.25 | 0.40 | 210 | 8 |
| Goto et al. [68] | 2001 | Japan | Asian | 0.43 | Yes | 1.14 | 0.28 | 37 | 1.23 | 0.37 | 47 | 1.23 | 0.33 | 22 | 6 |
| Talmud et al. [8] | 2002 | UK | Caucasian | 0.45 | Yes | 0.79 | 0.25 | 500 | 0.84 | 0.25 | 896 | 0.90 | 0.27 | 317 | 6 |
| Liu et al. [45] | 2002 | USA | Caucasian | 0.43 | Yes | 1.17 | 0.28 | 247 | 1.24 | 0.34 | 389 | 1.30 | 0.34 | 132 | 8 |
| Goff et al. [69] | 2002 | UK and France | Caucasian | 0.47 | Yes | 1.33 | 0.40 | 410 | 1.29 | 0.60 | 889 | 1.26 | 0.45 | 504 | 7 |
| Zhang et al. [35] | 2003 | China | Asian | 0.41 | No | 1.26 | 0.22 | 125 | 1.30 | 0.25 | 221 | 1.42 | 0.22 | 52 | 6 |
| Katsunori et al. [70] | 2003 | Japan | Asian | 0.4 | Yes | 1.32 | 0.46 | 217 | 1.43 | 0.57 | 279 | 1.59 | 0.62 | 95 | 7 |
| Zhao et al. [36] | 2004 | China | Asian | 0.41 | Yes | 1.19 | 0.36 | 155 | 1.27 | 0.34 | 214 | 1.38 | 0.39 | 72 | 6 |
| Weitgasser et al. [71] | 2004 | Austrian | Caucasian | 0.41 | Yes | 1.49 | 0.39 | 358 | 1.55 | 0.41 | 475 | 1.67 | 0.41 | 184 | 7 |
| Jiang et al. [72] | 2005 | China | Asian | 0.37 | No | 1.16 | 0.27 | 49 | 1.20 | 0.33 | 38 | 1.34 | 0.29 | 21 | 6 |
| Whiting et al. [53] | 2005 | USA | Caucasian | 0.42 | Yes | 0.91 | 0.33 | 1071 | 0.95 | 0.34 | 1577 | 1.00 | 0.38 | 571 | 8 |
| Huang et al. [73] | 2006 | China | Asian | 0.40 | Yes | 1.08 | 0.29 | 121 | 1.13 | 0.29 | 163 | 1.27 | 0.48 | 56 | 6 |
| Zhang et al. [74] | 2007 | China | Asian | 0.40 | No | 1.26 | 0.31 | 24 | 1.34 | 0.35 | 20 | 1.42 | 0.43 | 13 | 6 |
| Cui et al. [75] | 2007 | China | Asian | 0.46 | Yes | 1.44 | 0.32 | 17 | 1.58 | 0.46 | 24 | 1.54 | 0.36 | 13 | 6 |
| Meena et al. [76] | 2007 | Indian | Asian | 0.21 | No | 1.20 | 0.20 | 15 | 1.10 | 0.10 | 36 | 1.10 | 0.20 | 106 | 6 |
| Hsieh et al. [59] | 2007 | China | Asian | 0.31 | Yes | 43.31 | 10.63 | 42 | 43.39 | 11.09 | 158 | 46.24 | 11.83 | 165 | 5 |
| Zhang et al. [77] | 2008 | China | Asian | 0.39 | No | 1.45 | 0.31 | 46 | 1.41 | 0.23 | 78 | 2.03 | 0.47 | 16 | 6 |
| Wang et al. [78] | 2008 | China | Asian | 0.44 | Yes | 1.31 | 0.38 | 66 | 1.39 | 0.38 | 98 | 1.61 | 0.44 | 41 | 6 |
| Qiu et al. [79] | 2009 | China | Asian | 0.41 | Yes | 1.18 | 0.36 | 38 | 1.25 | 0.33 | 32 | 1.28 | 0.42 | 21 | 6 |
| Tao et al. [80] | 2010 | China | Asian | 0.41 | Yes | 0.95 | 0.19 | 608 | 0.96 | 0.18 | 939 | 0.97 | 0.18 | 272 | 6 |
| Kappelle et al. [81] | 2013 | The Netherlands | Caucasian | 0.42 | Yes | 1.28 | 0.37 | 2301 | 1.35 | 0.40 | 3233 | 1.41 | 0.42 | 1246 | 6 |
| Li et al. [82] | 2014 | China | Asian | 0.33 | Yes | 0.99 | 0.23 | 82 | 1.10 | 0.32 | 73 | 1.10 | 0.27 | 21 | 6 |
| Galati et al. [83] | 2014 | Italia | Caucasian | 0.42 | Yes | 1.52 | 0.45 | 73 | 1.45 | 0.30 | 106 | 1.61 | 0.42 | 39 | 7 |
| El-Aziz et al. [50] | 2014 | Egypt | Caucasian | 0.49 | Yes | 0.81 | 0.11 | 68 | 1.14 | 0.21 | 117 | 1.53 | 0.19 | 62 | 6 |
| Zhai et al. [84] | 2015 | China | Asian | 0.48 | Yes | 0.96 | 0.28 | 12 | 1.10 | 0.25 | 34 | 1.12 | 0.31 | 14 | 6 |
| Jeenduang et al. [85] | 2015 | Thailand | Asian | 0.37 | Yes | 1.34 | 0.32 | 152 | 1.35 | 0.35 | 169 | 1.39 | 0.31 | 57 | 6 |
USA: The United States, UK: United Kingdom, HWE: Hardy-Weinberg equilibrium, SD: standard deviation, HDL-C: High density lipoprotein cholesterol, MAF: minor allele frequencies.
3.2. Association between the CETP TaqIB Polymorphism and the Composite Ischemic CVD Risk
The results of all 45 comparisons showed evidence of a significant association between the CETP TaqIB polymorphism and the composite ischemic CVD, suggesting that carriers of allele TaqIB-B1 have a higher risk of the composite ischemic CVD than non-carriers (OR = 1.15, 95% CI = 1.09–1.21) (Figure 2). The additive genetic model (B1B1 vs. B2B2: OR = 1.26, 95% CI = 1.19–1.34), dominant genetic model (B1B1 + B1B2 vs. B2B2: OR = 1.20, 95% CI = 1.14–1.27), and recessive genetic model (B1B1 vs. B1B2 + B2B2: OR = 1.13, 95% CI = 1.08–1.18) were also included in the analysis and results were similar with allele comparison (Figures S1–S3). Subgroup analyses by ethnicity showed significant associations in Asians consistent with that in Caucasians. In addition, significant associations were also found between this variant and susceptibility to the composite ischemic CVD in the population-based group, the hospital-based group, the CAD group, the MI group, the IS group, the case control study group, and the cohort study group, respectively. We also observed the association between CETP TaqIB-B2 polymorphism and the composite ischemic CVD risk where was stronger in the Asian than the Caucasians. The main results of the meta-analysis are shown in Table 3.
Figure 2.
Meta-analysis of atherosclerosis and the CETP TaqIB polymorphism (B1 vs. B2).
Table 3.
Metal-analysis of CETP TaqIB polymorphism and risk of atherosclerosis in each subgroup.
| Position | Size (Case/Control) | Allele Model | Additive Model | Recessive Model | Dominant Model | ||||
|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | ||
| Overall analysis | 20,866/21,298 | 1.15 (1.09–1.21) | p < 0.001 | 1.26 (1.19–1.34) | p < 0.001 | 1.13 (1.08–1.18) | p < 0.001 | 1.20 (1.14–1.27) | p < 0.001 |
| Subgroup analysis based on ethnicity | |||||||||
| Asian | 5178/5084 | 1.24 (1.15–1.35) | p < 0.001 | 1.52 (1.35–1.72) | p < 0.001 | 1.41 (1.29–1.53) | p < 0.001 | 1.28 (1.15–1.42) | p < 0.001 |
| Caucasian | 15,688/16,214 | 1.09 (1.04–1.16) | 0.001 | 1.19 (1.11–1.27) | p < 0.001 | 1.05 (1.00–1.11) | 0.041 | 1.18 (1.11–1.25) | p < 0.001 |
| Subgroup analysis based on type of diseases | |||||||||
| MI | 9067/9393 | 1.10 (1.03–1.19) | 0.009 | 1.18 (1.08–1.29) | p < 0.001 | 1.05 (0.99–1.12) | 0.104 | 1.17 (1.08–1.26) | p < 0.001 |
| IS | 531/556 | 1.39 (1.17–1.66) | p < 0.001 | 1.92 (1.33–2.77) | 0.001 | 1.40 (1.09–1.79) | p < 0.001 | 1.76 (1.25–2.47) | 0.001 |
| CAD | 11,268/11,349 | 1.15 (1.08–1.24) | p < 0.001 | 1.31 (1.21–1.43) | p < 0.001 | 1.19 (1.12–1.27) | p < 0.001 | 1.21 (1.13–1.31) | p < 0.001 |
| Subgroup analysis based on source of controls | |||||||||
| PB | 14,735/11,618 | 1.11 (1.05–1.17) | p < 0.001 | 1.21 (1.13–1.29) | p < 0.001 | 1.09 (1.04–1.15) | 0.001 | 1.17 (1.10–1.25) | p < 0.001 |
| HB | 6131/5180 | 1.20 (1.10–1.31) | p < 0.001 | 1.42 (1.26–1.59) | p < 0.001 | 1.24 (1.14–1.35) | p < 0.001 | 1.28 (1.16–1.42) | p < 0.001 |
| Subgroup analysis based on study type | |||||||||
| CCS | 15,155/15,187 | 1.14 (1.10–1.18) | p < 0.001 | 1.30 (1.21–1.39) | p < 0.001 | 1.16 (1.11–1.22) | p < 0.001 | 1.22 (1.15–1.30) | p < 0.001 |
| CS | 5711/6111 | 1.07 (1.01–1.13) | 0.023 | 1.16 (1.03–1.30) | 0.012 | 1.05 (0.97–1.14) | 0.277 | 1.15 (1.04–1.28) | 0.007 |
| Sensitivity analysis | |||||||||
| BHWE | 14,461/16,034 | 1.16 (1.09–1.23) | p < 0.001 | 1.33 (1.23–1.42) | p < 0.001 | 1.18 (1.12–1.24) | p < 0.001 | 1.24 (1.16–1.32) | p < 0.001 |
| BS | 18,902/19,454 | 1.12 (1.08–1.15) | p < 0.001 | 1.25 (1.18–1.33) | p < 0.001 | 1.13 (1.08–1.18) | p < 0.001 | 1.20 (1.14–1.27) | p < 0.001 |
CAD: coronary artery disease, MI: myocardial infraction, IS: ischemic stroke, HB: hospital-based, PB: population-based, HWE: Hardy-Weinberg equilibrium, CS: cohort study, CCS: case control study, BHWE: based on Hardy-Weinberg equilibrium (Studies without Hardy-Weinberg equilibrium were excluded), BS: based on sample size (Studies with sample size < 400 were excluded).
3.3. Association between the CETP TaqIB Polymorphism and HDL-C Concentrations
Figure 3 describes the results of the meta-analysis of the CETP TaqIB polymorphism and HDL-C concentrations. Our analysis strongly suggested that carriers of the B1B1 genotype had lower concentrations of HDL-C than those of the B2B2 genotype (B1B1 vs. B2B2: SMD = 0.50, 95% CI = 0.36–0.65). We also compared carriers of the B1B1 genotype with those of the B1B2 genotype (Figure S4: B1B1 vs. B1B2: SMD = 0.18, 95% CI = 0.10–0.26) and B1B2 genotype with those of B2B2 genotype (Figure S5: B1B2 vs. B2B2: SMD = 0.32, 95% CI = 0.21–0.42). Subgroup analyses by ethnicity confirmed that the relationship between the CETP TaqIB-B2 polymorphism and the HDL-C concentration in Asians was less consistent than that in Caucasians (Figure 2, Figures S4 and S5).
Figure 3.
Association between the CETP TaqIB polymorphism and HDL-C level (B1B1 vs. B2B2).
3.4. Sensitivity Analysis
Sensitivity analysis was performed to determine the robustness of the study results. The included studies were limited to those conforming to HWE and sample size. We performed sensitivity analysis by removing studies without HWE and an n < 400. Overall, the corresponding pooled ORs and SMD were not materially altered for either analysis. Results of the sensitivity analysis suggested that the overall results were relatively robust and credible. The main results of the sensitivity analyses are shown in Table 3 and Figures S6–S11.
3.5. Heterogeneity Analysis
For the relationship between the CETP TaqIB polymorphism and the composite ischemic CVD, significant heterogeneity among the available studies were observed in the overall comparisons for the allelic model: PQ < 0.001, I2 = 57.8%; additive model: PQ < 0.001, I2 = 55.8%; recessive model: PQ < 0.001, I2 = 52.0%; and dominant model: PQ = 0.001, I2 = 41.7%. To clarify the sources of heterogeneity, we conducted a meta-regression analysis. The results showed that heterogeneity can be explained by the source of controls for the allelic model: p = 0.046, additive model: p = 0.025, and dominant model: p = 0.039, and ethnicity for the additive model: p = 0.048.
For the relationship between the CETP TaqIB polymorphism and HDL-C concentrations, significant heterogeneity among the available studies was also observed in the overall comparisons for B1B1 vs. B2B2: PQ < 0.001, I2 = 90.8%; B1B1 vs. B1B2: PQ < 0.001, I2 = 79.9%; and B1B2 vs. B2B2: PQ < 0.001, I2 = 85.1%. Four studies were identified as the main contributors of heterogeneity in the Asian studies [74,76,77,80] and four studies were identified as the main contributors of heterogeneity in the Caucasian studies [44,50,67,69] using the Galbraith plot (Figures S12 and S13). Figures S14–S16 show the association between the CETP TaqIB polymorphism and HDL-C concentrations after exclusion of these outlier studies. However, the significant association between the CETP polymorphism and HDL-C concentrations was unchanged both in the Asian subgroup (B1B1 vs. B2B2: SMD = 0.47, 95% CI = 0.36–0.57; B1B1 vs. B1B2: SMD = 0.19, 95% CI = 0.11–0.26; B1B2 vs. B2B2: SMD = 0.28, 95% CI = 0.18–0.37) and Caucasian subgroup (B1B1 vs. B2B2: SMD = 0.35, 95% CI = 0.30–0.40; B1B1 vs. B1B2: SMD = 0.16, 95% CI = 0.12–0.19; B1B2 vs. B2B2: SMD = 0.19, 95% CI = 0.15–0.20).
3.6. Publication Bias
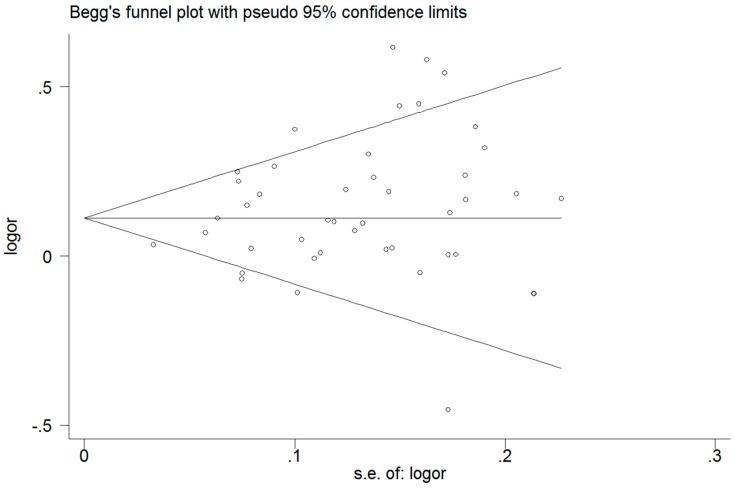
Funnel plots and Egger’s test were performed to access the publication bias of literature. For the CETP polymorphism and the composite ischemic CVD risk analysis (B1 vs. B2), the shape of the funnel plot (Figure 4) did not reveal obvious asymmetry, which means no publication bias. This was confirmed by Egger’s test (p = 0.074). For the CETP polymorphism and HDL-C analysis (B1B1 vs. B2B2), neither the shape of the funnel plot (Figure 5) nor Egger’s test (p = 0.058) revealed any obvious asymmetry.
Figure 4.
Funnel plot for allele comparison of atherosclerosis and the CETP TaqIB polymorphism. Each small circle represents a separate study for the indicated association.
Figure 5.
Funnel plot of CETP TaqIB polymorphism and HDL-C level (B1B1 vs. B2B2). Each small circle represents a separate study for the indicated association.
4. Discussion
In the present meta-analysis, a total of 45 studies from 44 papers with 20,866 cases and 21,298 controls, we found that the TaqIB-B2 allele was significantly associated with reduction of composite ischemic CVD both in Caucasians and Asians. Additionally, 28 studies with 23,959 subjects were included in the analysis on the association between the CETP TaqIB polymorphism and HDL-C concentrations. According to the results, the TaqIB-B2 allele was significantly associated with a higher level of HDL-C both in Caucasians and Asians. Therefore, it is reasonable to assume that the CETP TaqIB polymorphism is influencing HDL-C metabolism to protect against the development of AS. This result suggests that we can use CETP inhibitors to prevent and treat dyslipidemia and the composite ischemic CVD. In 2014, Keene et al. performed a meta-analysis to investigate association between the CETP inhibitors and cardiovascular outcomes [86]. The results show that CETP inhibitors neither increase the serum HDL-C concentration nor reduce the mortality rate of the composite ischemic CVD. It is probably because the trial design or the use of a drug with serious off-target adverse effects. On the other hand, it is well known that the serum HDL-C concentrations affected by multiple environmental and genetic factors. Therefore, the use of CETP inhibitor alone may not be able to reduce the risk of having a clinical atherosclerotic cardiovascular event.
To create a more comprehensive analysis of the association between the CETP TaqIB polymorphism and composite ischemic CVD, we performed subgroup analyses based on ethnicity, source of controls, atherosclerotic disease, and study type in the allelic model, additive model, recessive model, and dominant model. Significant associations were found between this variant and susceptibility to composite ischemic CVD in the Caucasian group, Asian group, population-based group, hospital-based group, IS group, CAD group, MI group (except for the recessive model), case control study group, and the subgroup of the cohort study group (except for the recessive model), respectively. For the association between the CETP TaqIB polymorphism and HDL-C, we also performed subgroup analysis based on ethnicity in the B1B1 vs. B2B2 model, B1B2 vs. B2B2 model, and B1B1 vs. B1B2 model. Significant associations were found between this variant and serum HDL-C concentrations in both the Caucasian and Asian group. These results further strengthen the conclusion that the CETP TaqIB-B2 allele protects against atherosclerosis by influencing HDL-C metabolism both in Asians and Caucasians. We also found that the association between CETP TaqIB-B2 polymorphism and composite ischemic CVD risk was stronger in Asians than Caucasians, but the relationship between the CETP TaqIB-B2 polymorphism and the HDL-C concentration in Asians was less consistent than that in Caucasians, which can be attributed to different environmental factors, lifestyle, etc.
Considering the influence of small-study effects on the overall results, we performed sensitivity analyses by excluding studies with low sample size or without the HWE. However, the corresponding pooled ORs and SMDs were unchanged in all comparisons, indicating statistically robust results.
Meanwhile, the existence of heterogeneity among the available studies, either for the CETP TaqIB polymorphism and composite ischemic CVD or for the CETP TaqIB polymorphism and HDL-C may affect the reliability of the results to a large extent. For the relationship between CETP TaqIB polymorphism and composite ischemic CVD, the heterogeneity can be explained by the source of controls (hospital controls and population controls) and ethnicity (Asians and Caucasians); for the relationship between CETP TaqIB polymorphism and serum HDL-C concentrations, the Galbraith plot was used to detect the source of heterogeneity for Asians and Caucasians. We identified four studies were as the main contributors of heterogeneity for Asians [74,76,77,80] and four for Caucasians [44,50,67,69]. The heterogeneity among Asians and Caucasians was effectively removed after excluding these outliers; however, the significant association between the CETP TaqIB polymorphism and serum HDL-C concentrations was unchanged. According to these outlier studies, the heterogeneity may be explained by the HWE, sample size, and disease.
There are several potential limitations in our present meta-analysis that should be acknowledged. First, there was significant heterogeneity in our study. Although we used appropriate meta-analytic techniques, we could not completely exclude the influence of the heterogeneity. Second, we may have missed eligible articles reported in other languages because our study only focused on articles published in English and Chinese. Third, the sample sizes of some studies were rather small. In summary, it is well-known that the composite ischemic CVD is affected by multiple environmental and genetic factors. Here, we discussed a single gene polymorphism and its impact on disease; however, several factors remain to be elucidated.
5. Conclusions
The present meta-analysis shows that the CETP TaqIB-B2 allele is associated with a higher serum HDL-C concentration and plays a protective role in composite ischemic CVD risk both in Asians and in Caucasians. Further investigations with the consideration of genetic and environmental interactions are needed.
Acknowledgments
This work was supported by grants from the National Science and Technology Support Projects for the “Eleventh Five-Years Plan” of China (No. 2009BAI82B04) and National Natural Science Foundation of China (No. 81560551).
Supplementary Materials
The following are available online at www.mdpi.com/1660-4601/13/9/882/s1, Figure S1: Meta-analysis of the composite ischemic CVD and the CETP TaqIB polymorphism (additive genetic model: B1B1 vs. B2B2). Figure S2: Meta-analysis of the composite ischemic CVD and the CETP TaqIB polymorphism (dominate genetic model: B1B1+B1B2 vs. B2B2). Figure S3: Meta-analysis of the composite ischemic CVD and the CETP TaqIB polymorphism (recessive genetic model: B1B1 vs. B1B2 + B2B2). Figure S4: Association between the CETP TaqIB polymorphism and HDL-C concentrations (B1B1 vs. B1B2). Figure S5: Association between the CETP TaqIB polymorphism and HDL-C concentrations (B1B2 vs. B1B2). Figure S6: Sensitivity analysis based on sample size for the associations between the CETP TaqIB polymorphism and HDL-C concentrations (B1B1 vs. B2B2). Figure S7: Sensitivity analysis based on Hardy–Weinberg equilibrium for the associations between the CETP TaqIB polymorphism and HDL-C concentrations (B1B1 vs. B2B2). Figure S8: Sensitivity analysis based on sample size for the associations between the CETP TaqIB polymorphism and HDL-C concentrations (B1B2 vs. B2B2). Figure S9: Sensitivity analysis based on Hardy–Weinberg equilibrium for the associations between the CETP TaqIB polymorphism and HDL-C concentrations (B1B2 vs. B2B2). Figure S10: Sensitivity analysis based on sample size for the associations between the CETP TaqIB polymorphism and HDL-C concentrations (B1B1 vs. B1B2). Figure S11: Sensitivity analysis based on Hardy–Weinberg equilibrium for the associations between the CETP TaqIB polymorphism and HDL-C concentrations (B1B1 vs. B1B2). Figure S12: Analysis of heterogeneity for Asian studies by Galbraith plot (B1B1 vs. B2B2). Figure S13: Analysis of heterogeneity for Caucasian studies by Galbraith plot (B1B1 vs. B2B2). Figure S14: Association between the CETP TaqIB polymorphism and HDL-C concentrations after exclusion of these outlier studies (B1B1 vs. B2B2). Figure S15: Association between the CETP TaqIB polymorphism and HDL-C concentrations after exclusion of these outlier studies (B1B1 vs. B1B2). Figure S16: Association between the CETP TaqIB polymorphism and HDL-C concentrations after exclusion of these outlier studies (B1B2 vs. B2B2). Checklist S1: PRISMA 2009 checklist. Table S1: MOOSE checklist.
Author Contributions
Conceived and designed the experiments: Shuxia Guo and Minghong Yao. Performed the experiments: Yu-song Ding, Jing-yu Zhang, Yi-zhong Yan, and Jia-ming Liu. Analyzed the data: Mei Zhang, Dong-sheng Rui, and Qiang Niu. Contributed reagents/materials/analysis tools: Jia He and Heng Guo. Wrote the paper: Shuxia Guo, Minghong Yao, and Ru-lin Ma.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Yusuf S., Hawken S., Ôunpuu S., Dans T., Avezum A., Lanas F., McQueen M., Budaj A., Pais P., Varigos J., et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 2.Costopoulos C., Niespialowska-Steuden M., Kukreja N., Gorog D.A. Novel oral anticoagulants in acute coronary syndrome. Int. J. Cardiol. 2013;167:2449–2455. doi: 10.1016/j.ijcard.2012.08.014. [DOI] [PubMed] [Google Scholar]
- 3.Goldbourt U., Yaari S., Medalie J.H. Isolated low HDL cholesterol as a risk factor for coronary heart disease mortality. A 21-year follow-up of 8000 men. Arterioscler. Thromb. Vasc. Biol. 1997;17:107–113. doi: 10.1161/01.ATV.17.1.107. [DOI] [PubMed] [Google Scholar]
- 4.Gotto A.M., Brinton E.A. Assessing low levels of high-density lipoprotein cholesterol as a risk factor in coronary heart disease: A working group report and update. J. Am. Coll. Cardiol. 2004;43:717–724. doi: 10.1016/j.jacc.2003.08.061. [DOI] [PubMed] [Google Scholar]
- 5.Shah P.K., Kaul S., Nilsson J., Cercek B. Exploiting the vascular protective effects of high-density lipoprotein and its apolipoproteins: An idea whose time for testing is coming, part I. Circulation. 2001;104:2376–2383. doi: 10.1161/hc4401.098467. [DOI] [PubMed] [Google Scholar]
- 6.Foitzik S., Kureck I.M., Rüger M.H., Metzler D. The role of plasma lipid transfer proteins in lipoprotein metabolism and atherogenesis. J. Lipid Res. 2009;50:S201–S206. doi: 10.1194/jlr.R800061-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tall A.R. Functions of cholesterol ester transfer protein and relationship to coronary artery disease risk. J. Clin. Lipid. 2010;4:389–393. doi: 10.1016/j.jacl.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Talmud P.J., Hawe E., Robertson K., Miller G.J., Miller N.E., Humphries S.E. Genetic and environmental determinants of plasma high density lipoprotein cholesterol and apolipoprotein AI concentrations in healthy middle-aged men. Ann. Hum. Genet. 2002;66:111–124. doi: 10.1046/j.1469-1809.2002.00105.x. [DOI] [PubMed] [Google Scholar]
- 9.Ordovas J.M. Genetic polymorphisms and activity of cholesterol ester transfer protein (CETP): Should we be measuring them? Clin. Chem. Lab. Med. 2000;38:945–949. doi: 10.1515/CCLM.2000.139. [DOI] [PubMed] [Google Scholar]
- 10.Boekholdt S.M., Sacks F.M., Jukema J.W., Shepherd J., Freeman D.J., Mcmahon A.D., Cambien F., Nicaud V., De Grooth G.J., Talmud P.J. Cholesteryl ester transfer protein TaqIB variant, high-density lipoprotein cholesterol levels, cardiovascular risk, and efficacy of pravastatin treatment: Individual patient meta-analysis of 13,677 subjects. Circulation. 2005;111:278–287. doi: 10.1161/01.CIR.0000153341.46271.40. [DOI] [PubMed] [Google Scholar]
- 11.Li Y.Y., Wu X.Y., Xu J., Qian Y., Zhou C.W., Wang B. Apo A5 −1131T/C, FgB −455G/A, −148C/T, and CETP TaqIB gene polymorphisms and coronary artery disease in the Chinese population: A meta-analysis of 15,055 subjects. Mol. Biol. Rep. 2013;40:1997–2014. doi: 10.1007/s11033-012-2257-9. [DOI] [PubMed] [Google Scholar]
- 12.Wang Q., Zhou S.B., Wang L.J., Lei M.M., Wang Y., Miao C., Jin Y.Z. Seven functional polymorphisms in the CETP gene and myocardial infarction risk: A meta-analysis and meta-regression. PLoS ONE. 2014;9:882. doi: 10.1371/journal.pone.0088118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cao M., Zhou Z.W., Fang B.J., Zhao C.G., Zhou D. Meta-analysis of cholesteryl ester transfer protein TaqIB polymorphism and risk of myocardial infarction. Medicine. 2014;93:e160. doi: 10.1097/MD.0000000000000160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stroup D.F., Berlin J.A., Morton S.C., Olkin I., Williamson G.D., Rennie D., Moher D., Becker B.J., Sipe T.A., Thacker S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis of Observational Studies in Epidemiology (MOOSE) group. J. Am. Med. Assoc. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 15.Moher D., Liberati A., Tetzlaff J., Altman D.G., Group P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Int. Med. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 16.Wells G.A., O’Connell D., Peterson J., Welch V., Shea B., Losos M., Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta- analyses. [(accessed on 20 Ocotber 2011)]. Available online: www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- 17.Higgins J.P.T., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. Br. Med. J. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berkey C.S., Hoaglin D.C., Mosteller F., Colditz G.A. A random-effects regression model for meta-analysis. Stat. Med. 1995;14:395–411. doi: 10.1002/sim.4780140406. [DOI] [PubMed] [Google Scholar]
- 19.Mantel N., Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J. Natl. Cancer Inst. 1959;22:639–640. [PubMed] [Google Scholar]
- 20.Dersimonian R., Kacker R. Random-effects model for meta-analysis of clinical trials: An update. Contem. Clin. Trials. 2007;28:105–114. doi: 10.1016/j.cct.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 21.Dersimonian R., Laird N. Meta-analysis in clinical trials. Controll. Clin. Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 22.Galbraith R.F. Graphical display of estimates having differing standard errors. Technometrics. 1988;30:271–281. doi: 10.1080/00401706.1988.10488400. [DOI] [Google Scholar]
- 23.Tanrikulu-Kucuk S., Ademoglu E., Gurdol F., Bilge A., Mutlu-Turkoglu U., Nisanci Y. Cholesteryl ester transfer protein Taq1B polymorphism in an angiographically assessed Turkish population: No effects on coronary artery disease risk. Genet. Test. Mol. Biol. 2010;14:637–642. doi: 10.1089/gtmb.2010.0069. [DOI] [PubMed] [Google Scholar]
- 24.Kaman D., N İ., N İ., Akbulut M. TaqIB and severity of coronary artery disease in the Turkish population: A pilot study. Bosn. J. Basic Med. Sci. 2015;15:5344–5346. doi: 10.17305/bjbms.2015.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kolovou G., Vasiliadis I., Kolovou V., Karakosta A., Mavrogeni S., Papadopoulou E., Papamentzelopoulos S., Giannakopoulou V., Marvaki A., Degiannis D. The role of common variants of the cholesteryl ester transfer protein gene in left main coronary artery disease. Lipid. Health Dis. 2011;10:1264–1271. doi: 10.1186/1476-511X-10-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu R., Liu Y.J., He L. Studies on the correlation between CETP TaqIB gene polymorphism and blood lipid and coronary heart disease. J. Tianjin Med. Univ. 2015;2:117–120. [Google Scholar]
- 27.Muendlein A., Saely C.H., Marte T., Schmid F., Koch L., Rein P., Langer P., Aczel S., Drexel H. Synergistic effects of the apolipoprotein E ɛ3/ɛ2/ɛ4, the cholesteryl ester transfer protein TaqIB, and the apolipoprotein C3 −482 C > T polymorphisms on their association with coronary artery disease. Atherosclerosis. 2008;199:179–186. doi: 10.1016/j.atherosclerosis.2007.10.030. [DOI] [PubMed] [Google Scholar]
- 28.Padmaja N., Kumar R.M., Balachander J., Adithan C. Cholesteryl ester transfer protein TaqIB, -629C>A and I405V polymorphisms and risk of coronary heart disease in an Indian population. Clin. Chim. Acta Int. J. Clin. Chem. 2009;402:139–145. doi: 10.1016/j.cca.2008.12.041. [DOI] [PubMed] [Google Scholar]
- 29.Qin Q., Zhao B.R., Geng J., Li Y.L., Cui R.Z. The association of the Hpoprotein Hpase $447X and cholesteryl ester transfer protein TaqlB polymorphism with coronary heart disease. Chin. J. Cardiol. 2004;32:522–525. [Google Scholar]
- 30.Rejeb J., Omezzine A., Rebhi L., Naffeti I., Kchok K., Belkahla R., Hadjmbarek I.B., Rejeb N.B., Nabli N., Boujelbene A. Association of the cholesteryl ester transfer protein Taq1 B2B2 genotype with higher high-density lipoprotein cholesterol concentrations and lower risk of coronary artery disease in a Tunisian population. Arch. Cardiovsc. Dis. 2008;101:629–636. doi: 10.1016/j.acvd.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 31.Shi C.X., Bian C.H., Liu R., Liu Y.J., Zhao Y.Q. The correlation study between CETP-TaqIB gene polymorphism and coronary heart disease. Chin. J. Care. Med. 2015;35:337–341. [Google Scholar]
- 32.Wang W., Zhou X., Liu F., Hu H.N., Han D.F. Association of the TaqIB polymorphism and D442G mutation of cholesteryl ester transfer protein gene with coronary heart disease. Chin. J. Cardiol. 2004;32:981–985. [Google Scholar]
- 33.Wu J.H., Lee Y.T., Hsu H.C., Hsieh L.L. Influence of CETP gene variation on plasma lipid levels and coronary heart disease: A survey in Taiwan. Atherosclerosis. 2001;159:451–458. doi: 10.1016/S0021-9150(01)00524-X. [DOI] [PubMed] [Google Scholar]
- 34.Yan S.K., Zhu Y.L., Cheng S., Song Y.H., Yan X.W. Relationship between coronary heart disease and TaqIB & MspI polymorphisms of cholesteryl ester transfer protein gene in Han nationality. Chin. J. Lab. Med. 2004;27:671–675. [Google Scholar]
- 35.Zhang Y.J., Geng J., Qin Q., Mao Y.M., Cui R.Z. The effects of TaqIB polymorphism of cholesteryl ester transfer proteinon coronary heart disease. Tianjin Med. J. 2003;31:758–760. [Google Scholar]
- 36.Zhao S.P., Li H., Xiao Z.J., Nie S. The effect of TaqIB polymorphism of cholesteryl ester transfer protein gene on the lipoprotein level. Chin. J. Cardiol. 2004;32:816–818. [Google Scholar]
- 37.Zheng K.Q., Zhang S.Z., He Y., Zhang L., Zhang K.L. Association between cholesteryl ester transfer protein gene polymorphisms and variations in lipid levels in patients with coronary heart disease. Chin. Med. J. 2004;117:1288–1292. [PubMed] [Google Scholar]
- 38.Arca M., Montali A., Ombres D., Battiloro E., Campagna F., Ricci G., Verna R. Lack of association of the common TaqIB polymorphism in the cholesteryl ester transfer protein gene with angiographically assessed coronary atherosclerosis. Clin. Genet. 2001;60:374–380. doi: 10.1034/j.1399-0004.2001.600510.x. [DOI] [PubMed] [Google Scholar]
- 39.Corella D., Carrasco P., Amiano P., Arriola L., Chirlaque M.D., Huerta J.M., Martínez C., Martinez-Camblor P., Molina E., Navarro C. Common cholesteryl ester transfer protein gene variation related to high-density lipoprotein cholesterol is not associated with decreased coronary heart disease risk after a 10-year follow-up in a Mediterranean cohort: Modulation by alcohol consumption. Atherosclerosis. 2010;211:531–538. doi: 10.1016/j.atherosclerosis.2010.03.026. [DOI] [PubMed] [Google Scholar]
- 40.Eiriksdottir G., Bolla M.K., Thorsson B., Sigurdsson G., Humphries S.E., Gudnason V. The −629C>A polymorphism in the CETP gene does not explain the association of TaqIB polymorphism with risk and age of myocardial infarction in Icelandic men. Atherosclerosis. 2001;159:187–192. doi: 10.1016/S0021-9150(01)00489-0. [DOI] [PubMed] [Google Scholar]
- 41.Fumeron F., Betoulle D., Luc G., Behague I., Ricard S., Poirier O., Jemaa R., Evans A., Arveiler D., Marques-Vidal P. Alcohol intake modulates the effect of a polymorphism of the cholesteryl ester transfer protein gene on plasma high density lipoprotein and the risk of myocardial infarction. J. Clin. Investig. 1995;96:1664–1671. doi: 10.1172/JCI118207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yilmaz H., İsbir T., Agachan B., Karaali Z.E. Effects of cholesterol ester transfer protein Taq1B gene polymorphism on serum lipoprotein levels in Turkish coronary artery disease patients. Cell Biochem. Funct. 2005;23:23–28. doi: 10.1002/cbf.1124. [DOI] [PubMed] [Google Scholar]
- 43.Bernard K., Alison P., Sarah P., Sarah C., Linda Y., John D., Colin M.K., Marc D., Mark L., Richard P. Lipid-related genes and myocardial infarction in 4685 cases and 3460 controls: Discrepancies between genotype, blood lipid concentrations, and coronary disease risk. Int. J. Epidemiol. 2004;33:1002–1013. doi: 10.1093/ije/dyh275. [DOI] [PubMed] [Google Scholar]
- 44.Kuivenhoven J.A., Jukema J.W., Zwinderman A.H., Knijff P.D., McPherson R., Bruschke A.V.G., Lie K.I., Kastelein J.J.P. The role of a common variant of the cholesteryl ester transfer protein gene in the progression of coronary atherosclerosis. N. Engl. J. Med. 1998;338:86–93. doi: 10.1056/NEJM199801083380203. [DOI] [PubMed] [Google Scholar]
- 45.Liu S., Schmitz C., Stampfer M.J., Sacks F., Hennekens C.H., Lindpaintner K., Ridker P.M. A prospective study of TaqIB polymorphism in the gene coding for cholesteryl ester transfer protein and risk of myocardial infarction in middle-aged men. Atherosclerosis. 2002;161:469–474. doi: 10.1016/S0021-9150(01)00673-6. [DOI] [PubMed] [Google Scholar]
- 46.Lu Y., Tayebi N., Li H., Saha N., Yang H., Heng C.K. Association of CETP Taq1B and -629C > A polymorphisms with coronary artery disease and lipid levels in the multi-ethnic Singaporean population. Lipid. Health Dis. 2013;12:1–13. doi: 10.1186/1476-511X-12-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mehlig K., Strandhagen E., Svensson P.A., Rosengren A., Torén K., Thelle D.S., Lissner L. CETP TaqIB genotype modifies the association between alcohol and coronary heart disease: The INTERGENE case-control study. Alcohol. 2014;48:695–700. doi: 10.1016/j.alcohol.2014.08.011. [DOI] [PubMed] [Google Scholar]
- 48.Meiner V., Friedlander Y., Milo H., Sharon N., Ben-Avi L., Shpitzen S., Leitersdorf E., Siscovick D.S., Schwartz S.M. Cholesteryl ester transfer protein (CETP) genetic variation and early onset of non-fatal myocardial infarction. Ann. Hum. Genet. 2008;72:732–741. doi: 10.1111/j.1469-1809.2008.00464.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Poduri A., Khullar M., Bahl A., Sharma Y.P., Talwar K.K.A. Combination of proatherogenic single-nucleotide polymorphisms is associated with increased risk of coronary artery disease and myocardial infarction in Asian Indians. DNA Cell Biol. 2009;28:451–460. doi: 10.1089/dna.2009.0887. [DOI] [PubMed] [Google Scholar]
- 50.El-Aziz T.A.A., Mohamed R.H., Hagrass H.A. Increased risk of premature coronary artery disease in Egyptians with ABCA1 (R219K), CETP (TaqIB), and LCAT (4886C/T) genes polymorphism. J. Clin. Lipid. 2014;8:381–389. doi: 10.1016/j.jacl.2014.06.001. [DOI] [PubMed] [Google Scholar]
- 51.Tenkanen H., Koskinen P., Kontula K., Aalto-Setälä K., Mänttäri M., Manninen V., Runeberg S.L., Taskinen M.R., Ehnholm C. Polymorphisms of the gene encoding cholesterol ester transfer protein and serum lipoprotein levels in subjects with and without coronary heart disease. Hum. Genet. 1991;87:574–578. doi: 10.1007/BF00209015. [DOI] [PubMed] [Google Scholar]
- 52.Wang S.H., Cui H.B., Wang D.Q., Chen X.M., Zhang H.K., Cui C.C., Chen X.Y., Liu X.H., Zhang Z., Bai F., et al. Geographical characteristics of single nucleotide polymorphism of candidate genes associated with coronary artery disease in Chinese Hart population. China J. Cardiol. 2008;36:24–29. [PubMed] [Google Scholar]
- 53.Whiting B.M., Anderson J.L., Muhlestein J.B., Horne B.D., Bair T.L., Pearson R.R., Carlquist J.F. Candidate gene susceptibility variants predict intermediate end points but not angiographic coronary artery disease. Am. Heart J. 2005;150:243–250. doi: 10.1016/j.ahj.2004.08.034. [DOI] [PubMed] [Google Scholar]
- 54.Zhang G.B., Jiang Z.W., Sun B.G., Lu Y.S., Wen Q.Z., Zhuang W.Y., Wang F. Relationship of Taq IB polymorphism in the cholesteryl ester transfer protein gene to coronary artery disease. Chin. J. Arterioscler. 2005;13:88–90. [Google Scholar]
- 55.Zhang Y., Xi J.L., Yun M.L., Zhang Y.X., Zhou D.F. Study on the relationship between CETP polymorphism and plasma lipid in patient with CHD of Han ethnic in Hannan. Mod. Prev. Med. 2011;38:691–693. [Google Scholar]
- 56.Freeman D.J., Samani N.J., Wilson V., McMahon A.D., Braund P.S., Cheng S., Caslake M.J., Packard C.J., Gaffney D. A polymorphism of the cholesteryl ester transfer protein gene predicts cardiovascular events in non-smokers in the west of scotland coronary prevention study. Eur. Heart J. 2003;24:1833–1842. doi: 10.1016/j.ehj.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 57.Dedoussis G.V., Panagiotakos D.B., Louizou E., Mantoglou I., Chrysohoou C., Lamnisou K., Pitsavos C., Stefanadis C. Cholesteryl ester-transfer protein (CETP) polymorphism and the association of acute coronary syndromes by obesity status in Greek subjects: The CARDIO2000-GENE study. Hum. Hered. 2007;63:155–161. doi: 10.1159/000099827. [DOI] [PubMed] [Google Scholar]
- 58.Morgan T.M., Krumholz H.M., Lifton R.P., Spertus J.A. Nonvalidation of reported genetic risk factors for acute coronary syndrome in a large-scale replication study. J. Am. Med. Assoc. 2007;297:1551–1561. doi: 10.1001/jama.297.14.1551. [DOI] [PubMed] [Google Scholar]
- 59.Hsieh M.C., Tien K.J., Chang S.J., Lo C.S., Hsin S.C., Hsiao J.Y., Hsu S.C., Liang H.T., Chen H.C., Shin S.J. Cholesteryl ester transfer protein B1B1 genotype as a predictor of coronary artery disease in Taiwanese with type 2 diabetes mellitus. Metab. Clin. Exp. 2007;56:745–750. doi: 10.1016/j.metabol.2006.12.023. [DOI] [PubMed] [Google Scholar]
- 60.Cyrus C., Vatte C., Al-Nafie A., Chathoth S., Al-Ali R., Al-Shehri A., Akhtar M.S., Almansori M., Al-Muhanna F., Keating B. The impact of common polymorphisms inCETPandABCA1genes with the risk of coronary artery disease in Saudi Arabians. Hum. Genom. 2016;10 doi: 10.1186/s40246-016-0065-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tayebi N. Master’s Thesis. National University of Singapore; Singapore: 2012. Association of CETP and ADTRP Genes with Coronary Artery Disease in Multi-Ethnic Singaporean Population. [Google Scholar]
- 62.Jensen M.K., Mukamal K.J., Kim O., Rimm E.B. Alcohol consumption, TaqIB polymorphism of cholesteryl ester transfer protein, high-density lipoprotein cholesterol, and risk of coronary heart disease in men and women. Eur. Heart J. 2008;29:104–112. doi: 10.1093/eurheartj/ehm517. [DOI] [PubMed] [Google Scholar]
- 63.Fidani L., Hatzitolios A.I., Goulas A., Savopoulos C., Basayannis C., Kotsis A. Cholesteryl ester transfer protein TaqIB and lipoprotein lipase Ser447Ter gene polymorphisms are not associated with ischaemic stroke in Greek patients. Neurosci. Lett. 2005;384:102–105. doi: 10.1016/j.neulet.2005.04.061. [DOI] [PubMed] [Google Scholar]
- 64.Quarta G., Stanzione R., Evangelista A., Zanda B., Sciarretta S., Angelantonio E.D., Marchitti S., Murro D.D., Volpe M., Rubattu S. A protective role of a cholesteryl ester transfer protein gene variant towards ischaemic stroke in Sardinians. J. Int. Med. 2007;262:555–561. doi: 10.1111/j.1365-2796.2007.01845.x. [DOI] [PubMed] [Google Scholar]
- 65.Jiang Y.Q., Wang F., Zhou L.F., Chen C.G., Qi J.Y. Relationship of cholesteryl ester transfer protein TAQIB polymorphisms with cerebral infraction. J. Med. Res. 2012;41:89–92. [Google Scholar]
- 66.Bhanushali A.A., Das B.R. Genetic variants at the APOE, lipoprotein lipase (LpL), cholesteryl ester transfer protein (CETP), and endothelial nitric oxide (eNOS) genes and coronary artery disease (CAD): CETP Taq1 B2B2 associates with lower risk of CAD in Asian Indians. J.Commun. Genet. 2010;1:55–62. doi: 10.1007/s12687-010-0005-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gudnason V., Kakko S., Nicaud V., Savolainen M., Kesäniemi Y., Tahvanainen E., Humphries S. Cholesteryl ester transfer protein gene effect on CETP activity and plasma high-density lipoprotein in European populations. Eur. J. Clin. Investig. 1999;29:116–128. doi: 10.1046/j.1365-2362.1999.00412.x. [DOI] [PubMed] [Google Scholar]
- 68.Goto A., Sasai K., Suzuki S., Fukutomi T., Ito S., Matsushita T., Okamoto M., Suzuki T., Itoh M., Okumura-Noji K. Cholesteryl ester transfer protein and atherosclerosis in Japanese subjects: A study based on coronary angiography. Atherosclerosis. 2001;159:153–163. doi: 10.1016/S0021-9150(01)00476-2. [DOI] [PubMed] [Google Scholar]
- 69.Goff W.L., Guerin M., Nicaud V., Dachet C., Luc G., Arveiler D., Ruidavets J.B., Evans A., Kee F., Morrison C. A novel cholesteryl ester transfer protein promoter polymorphism (−971G/A) associated with plasma high-density lipoprotein cholesterol levels. Atherosclerosis. 2002;161:269–279. doi: 10.1016/S0021-9150(01)00641-4. [DOI] [PubMed] [Google Scholar]
- 70.Katsunori I., Hiroshi M., Tamio T., Nobuhiro Y., Shinichi O., Jun S., Kouki T., Yasushi S. Association of cholesteryl ester transfer protein activity and TaqIB polymorphism with lipoprotein variations in Japanese subjects. Metab. Clin. Exp. 2003;52:1564–1570. doi: 10.1016/j.metabol.2003.07.011. [DOI] [PubMed] [Google Scholar]
- 71.Weitgasser R., Galvan G., Malaimare L., Derflinger I., Hedegger M., Lang J., Iglseder B., Ladurner G., Paulweber B. Cholesteryl ester transfer protein TaqIB polymorphism and its relation to parameters of the insulin resistance syndrome in an Austrian cohort. Biomed. Pharmacother. 2004;58:619–627. doi: 10.1016/j.biopha.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 72.Jiang T., Song X.X., Zhang M., Qi W.H., Zhang X.W. Association between insulin resistance and cholesteryl ester transfer protein gene polymorphism in type 2 diabetesmellitus. Chin. J. Med. Genet. 2005;22:298–301. [PubMed] [Google Scholar]
- 73.Huang Z.Y., Guo H.W., Xu Z.H., Xue K., Zhou X. Association of gene polymorphism at cholesterol ester transfer protein locus with obesity and response to dietary intervention in obesity. J. Hyg. Res. 2006;35:447–450. [PubMed] [Google Scholar]
- 74.Zhang Q., Deng B., Li P.L., Yan Y., Wang X.Y. Perioperative insulin resistance and TaqIB polymorphisms of cholesteryle ester transfer protein(CETP) in patients with essential hypertension. J. Clin. Anesthesiol. 2007;23:973–976. [Google Scholar]
- 75.Cui Y.L., Zhao X.L., Wu F., Guo S.J., Li J.J. Relationship between TaqIB genetic polymorphism at cholesterol ester transfer protein locus and the efficacy ofpolicosanol. Chin. J. New Drugs. 2007;16:240–243. [Google Scholar]
- 76.Meena K., Misra A., Pandey R.M., Luthra K. CETP TaqIB polymorphisms and CETP activity in normolipidemic healthy northern Indians. Diabet. Metab. Syndr. Clin. Res. Rev. 2007;1:239–244. doi: 10.1016/j.dsx.2007.09.010. [DOI] [Google Scholar]
- 77.Zhang P.H., Li G.M., Wang Y., Zheng K.Q. TaqIB polymorphism in CETP gene in 140 hyperlipemia patients and lipid regulating effects of statins. J. Guangdong Med. Coll. 2008;26:492–495. [Google Scholar]
- 78.Wang Y.Z., Yan S.K., Song Y.H. Relationship of cholesterol ester transfer protein TaqIB gene polymorphism with type2 diabetes mellitus in Chinese Han nationality patients. Chin. J. Clin. Lab. Sci. 2008;4:297–300. [Google Scholar]
- 79.Qiu H., Zhang Q., Deng B., Jiang B.H., Jin H.G. The association study of cerebrocardiac vascular diseasew ith TaqIB gene polymorphisms of cholesteryle ester transfer protein in the patients with prmiary hypertension. Chin. J. Clin. Med. 2009;16:341–343. [Google Scholar]
- 80.Tao X.M., Li G.J., Hou S.Q., Xiao Z.S., Tong W.J., Liu Y.Y., Gang W.U., Zhang Y.H., Qiu C.C. Association of cholesteryl ester transfer protein gene TaqIB polymorphism with essential hypertension in Chinese mongolian population. Basic Clin. Med. 2010;30:677–682. [Google Scholar]
- 81.Kappelle P.J.W.H., Gansevoort R.T., Hillege H.J., Wolffenbuttel B.H.R., Dullaart R.P.F. Common variation in Cholesteryl Ester Transfer Protein : Relationship of first major adverse cardiovascular events with the apolipoprotein B/apolipoprotein A-I ratio and the total cholesterol/high-density lipoprotein cholesterol ratio. J. Clin. Lipid. 2013;7:56–64. doi: 10.1016/j.jacl.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 82.Li J., Zhang L., Xie N.Z., Deng B., Lv L.X., Zheng L.Q. Relationship between the cholesterol ester transfer protein TaqIB polymorphism and the lipid-lowering effect of atorvastatin in patients with coronary atherosclerotic heart disease. Genet. Mol. Res. 2014;13:2140–2148. doi: 10.4238/2014.March.24.21. [DOI] [PubMed] [Google Scholar]
- 83.Galati F., Colonna P., Galati A., Ciardiello C., Bozzetti M.P., Massari S. CETP TaqIB polymorphism, serum lipid levels and risk of atrial fibrillation: A case-control study. J. Atr. Fibrillation. 2014;6:24–29. doi: 10.4022/jafib.964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhai X.H., Hu Y., Xu C.Y., Li Y.C., Zhang Z.Y. Correlation research and molecular regulation mechanism of cholesteryl ester transfer protein gene rs708272 polymorphism with exercise induced serum lipid changes in obese adolescent. J. Wuhan Inst. Phys. Educ. 2015;49:84–89. [Google Scholar]
- 85.Jeenduang N., Porntadavity S., Nuinoon M., Horpet D., Thepkwan N., Thaworn P., Theanmontri S. Studies of the CETP TaqIB and ApoE polymorphisms in Southern Thai subjects with the metabolic syndrome. Biochem. Genet. 2015;53:1–16. doi: 10.1007/s10528-015-9680-2. [DOI] [PubMed] [Google Scholar]
- 86.Keene D., Price C., Shunshin M.J., Francis D.P. Effect on cardiovascular risk of high density lipoprotein targeted drug treatments niacin, fibrates, and CETP inhibitors: Meta-analysis of randomised controlled trials including 117,411 patients. Br. Med. J. 2014;349:g4379. doi: 10.1136/bmj.g4379. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.