Abstract
African and Caribbean Black women in Canada have new HIV infection rates 7 times higher than their white counterparts. This overrepresentation is situated in structural contexts of inequities that result in social, economic and health disparities among African and Caribbean Black populations. Economic insecurity is a distal driver of HIV vulnerability, reducing access to HIV testing, prevention and care. Less is known about how economic insecurity indicators, such as housing security, continue to influence the lives of women living with HIV following HIV-positive diagnoses. The aim of this study was to test a conceptual model of the pathways linking HIV-related stigma, racial discrimination, housing insecurity, and wellbeing (depression, social support, self-rated health). We implemented a cross-sectional survey with African and Caribbean Black women living with HIV in 5 Ontario cities, and included 157 participants with complete data in the analyses. We conducted structural equation modeling using maximum likelihood estimation to evaluate the hypothesized conceptual model. One-fifth (22.5%; n = 39) of participants reported housing insecurity. As hypothesized, racial discrimination had significant direct effects on: HIV-related stigma, depression and social support, and an indirect effect on self-rated health via HIV-related stigma. HIV-related stigma and housing insecurity had direct effects on depression and social support, and HIV-related stigma had a direct effect on self-rated health. The model fit the data well: χ2 (45, n = 154) = 54.28, p = 0.387; CFI = 0.997; TLI = 0.996; RMSEA = 0.016. Findings highlight the need to address housing insecurity and intersecting forms of stigma and discrimination among African and Caribbean Black women living with HIV. Understanding the complex relationships between housing insecurity, HIV-related stigma, racial discrimination, and wellbeing can inform multi-level interventions to reduce stigma and enhance health.
Introduction
African and Caribbean Black (ACB) women remain overrepresented in Canada’s HIV epidemic with new infection rates 7 times higher than their white counterparts. [1] This is similar to the experience of African American women in the United States, who have HIV infection rates close to 4 times that of white women. [2] Heightened HIV vulnerability among women and ethno-racial minorities, and people at the intersection of these identities, is situated in structural contexts of social, economic and political inequities. [3, 4] Structural factors such as economic insecurity have a complex and indirect association with HIV risk, operating distally to reduce access to HIV testing, prevention, and care. [3, 5–10]
Prior research indicates that ACB women experience higher rates of HIV-related stigma then non-racialized women. [11, 12] Marginalized women experience discrimination in the form of classism, racism and sexism, among others.[13–16] This marginalization may be exacerbated for ACB women living with HIV (WLHW). The convergence of gender and racial inequities produce unique and distinct experiences of HIV stigma among ACB women that reflect sexist and racist stereotypes. [11, 17, 18] Little is known about dimensions of economic insecurity, such as housing insecurity, and its interplay with stigma and health among ACB WLHW. This study aims to address this knowledge gap by modeling the relationships between housing insecurity, racial discrimination, HIV-related stigma, and wellbeing (depression, social support, self-rated health[SRH]) among ACB WLWH. We first review the effects of HIV-related stigma and racial discrimination on people living with HIV (PLHIV), and then explore housing insecurity and wellbeing among PLHIV. We theoretically situate this study in the fundamental causes of health; finally we report the study design and findings.
HIV Related Stigma, Racial Discrimination, and Wellbeing
Structural perspectives articulate that stigma processes occur across micro, meso and macro levels, and include labeling, loss of status, and discrimination in contexts of unequal power dynamics. [19, 20] Social environments with chronic and acute stressors—such as stigma and discrimination—enhance susceptibility to health problems. [21] There is a rich body of literature highlighting deleterious impacts of HIV-related stigma on mental and physical health, as well as social support, among PLHIV. [22–26] Processes by which HIV-related stigma can effect psychological and health outcomes are complex. For example, internalized stigma—acceptance of negative views about PLHIV—may be associated with shame, which in turn contributes to depression. [26, 27] Enacted stigma, negative treatment from others, and perceived stigma, awareness of negative social norms and attitudes towards PLHIV, contribute to psychological distress and reduced wellbeing. [26] The convergence of internalized, enacted and perceived stigma may reduce health care services utilization and medication adherence, in turn compromising physical wellbeing of PLHIV. [27]
The deleterious impacts of racial discrimination on health are well documented; systematic review findings highlight the impacts of racism on poorer mental health and reduced health behaviors. [28] Racial discrimination refers to inequitable and oppressive systems founded on ethno-racial differences, including beliefs, attitudes, exclusion, harassment, and institutional policies and practices. [29, 30] Few studies, however, have examined racial discrimination and wellbeing among PLHIV. [22] One study in the Canadian context examined gender and ethnicity differences in HIV-related stigma; the gender-ethnicity interaction term was significant and Black women reported among the highest HIV-related stigma scores. [11] Race is also a known determinant of housing insecurity. [31] The impacts of race on socioeconomic status are shaped by reduced access to education and employment opportunities, and, in a large part, residential segregation. In the US numerous studies have demonstrated that race and ethnicity powerfully impact the housing markets that individuals have access to. [31–33] This is largely attributed to discrimination and limited social capital of poor and minority individuals. [31, 32] Health is not simply connected to race indirectly through socioeconomic status, but racism and discrimination also have direct impacts on health status, for example, through neighbourhood segregation which leads to inequitable service provision. [31] In Canada, ethno-racial groups have been identified as high-risk for homelessness, although public discussions of homelessness are often silent on the issue of race and racism as determinants of homelessness. [34]
For ACB women, these factors are heightened if they are also immigrants. Canadian studies show that racialized immigrants are likely to face stigma and discrimination both on account of their race and on their immigration status.[35–38] Immigrants may be stigmatized through ‘othering’, a process that differentiates persons based on perceived differences [39] and contributes to marginalization and social exclusion [40]. Immigrants, in general, experience poorer wellbeing than the general population with elevated risk of depression, chronic pain, and other somatic complaints. [41, 42] Psychotic disorders may be elevated among immigrants post-migration. [43–45] In Canada exposure to racism and discrimination has been shown to have negative impacts on the mental health of immigrants and refugees. [46–48] Racism also presents as a barrier to accessing housing for immigrants. Teixeira (2006) found that recent Angolan and Mozambican immigrants in Toronto, Canada encountered barriers to securing affordable and adequate housing, including prejudice and discrimination based on their race and skin colour. [49] The experiences of immigrant PLHIV may be compounded by limited knowledge of local health systems, poverty, and immigration status. [50–52] A study from the United Kingdom found that stigma and discrimination because of their migrant status greatly impacted the ways in which migrants PLHIV accessed HIV-related care and support. [51] The experiences of immigrant ACB WLWH are understudied in the Canadian context.
Housing Insecurity and Wellbeing Among People With HIV
Across the globe complex causal pathways contribute to health inequities among people with lower socio-economic status (SES) in comparison with their higher SES counterparts. [53–56] In Canada individuals with lower SES are four times more likely to report fair or poor health than higher-income individuals. [57, 58] Longitudinal studies reveal that Canadians living in the poorest 20% of urban neighborhoods die earlier than other Canadians. [57, 58] In a US population-based study, socio-economic disparities accounted for a significant proportion of health disparities across multiple health outcomes including AIDS mortality. [59]
The link between housing insecurity and HIV is well documented, and complex. Homelessness and HIV interact in two distinct ways: homeless individuals are at a greater risk of HIV infection, women in particular, [60, 61] and homelessness can have negative impacts on the health of PLHIV. [62–64] To manage their chronic condition, PLHIV must follow drug regimens, secure ample nutrition and rest, and access frequent monitoring and social support by health professionals. [65] This is difficult to do in the face of housing insecurity. [66] Housing insecurity is particularly important to examine among PLHIV, as it is associated with faster progression from HIV to AIDS and AIDS mortality. [67] However, more research is needed in the Canadian context of health and social correlates of SES disparities among PLHIV.
Housing insecurity is associated with deleterious physical and mental health outcomes among PLHIV. [66] In a longitudinal US study of PLHIV with unstable housing, Riley et al. [68] found unmet subsistence needs were associated with poor mental and physical health outcomes among HIV-positive men, and negative impacts on mental and gynecological health among WLWH. [69] A 2004 Canadian study found HIV related illnesses to be a leading cause of death among homeless women aged 18–44. [70] A systematic review of the effects of housing status on health-related outcomes among PLHIV found a positive association between housing stability and improved health-related outcomes, including: medication adherence, health and social services utilization, and health status. [65] One study in this review examined mental health status, finding housing stability not to be significantly associated with mental health functioning. [71] Both the author of the study and authors of the review highlight the need for further research that includes psychological health-related outcomes. [65] Furthermore, only 1 of the 29 studies in this review included Canadian populations, underscoring the need for further research on housing insecurity among PLHIV in this context. Qualitative research reported that housing instability, homelessness and transience pose barriers to accessing health services and social support, in particular for ACB WLWH in Toronto, Canada. [72, 73] Another qualitative study highlighted that ACB WLWH experiencing housing insecurity face increased stressors, including barriers to supports. [74]
Social support and social networks often have positive influences on health, buffering the adverse physical and mental health effects of stressors. [75, 76] Persons with robust and high quality social networks have decreased mortality and morbidity. [77] Social support has also been shown have beneficial health effects for PHLIV, including increased quality of life, coping skills, and treatment success. [78] Poverty, however, is associated with reduced social support. Kawachi and Kennedy [79] reported that income inequality reduces the ability to achieve social cohesion. A recent U.S. study demonstrated that among the urban poor, poverty-specific stressors are associated with poor health, and social supports may not have as great a health impact as previously understood. [80] Associations between housing insecurity and social support among PLHIV are less understood. This is a salient area to examine as HIV-related stigma is widely associated with reduced social support among PLHIV. [22]
Housing insecurity has been linked with higher rates of HIV-related stigma. [22, 81] Precariously housed PLHIV may experience intersecting forms of stigmatization based on their HIV positive status and their housing status. Wolitski et al. [62] note that in the US homeless PLHIV may experience higher HIV-related stigma due to stereotypes that they are “responsible” for their HIV infection, as well as due to intersections with stigma already experienced based on race, ethnicity and housing status, among other factors.
Housing insecurity has also been linked with broad experiences of discrimination, not limited to HIV. Persons with lower SES may perceive themselves to experience higher rates of stigma and discrimination, particularly in Western contexts where values of meritocracy can place personal responsibility for poverty on individuals. [82–84] In a US study, poverty was correlated with allostatic load and perceived discrimination. [85] This study used a general, unspecified discrimination measure to assess inequitable treatment based on any aspect of one’s background or identity.
We did not find quantitative studies with PLHIV that examined associations between housing insecurity and forms of stigma beyond HIV-related stigma—such as racism. More research is needed to conceptualize the complex relationships between different forms of stigma and discrimination, housing insecurity, and wellbeing among ACB WLWH, particularly in the Canadian context.
Theoretical Approach
Our study was guided by fundamental cause theory. Link and Phelan [86] developed fundamental cause theory to conceptualize the linkages between distal factors, such as social contexts and SES, and persistent health disparities. Fundamental causes refer to factors associated with multiple health inequities across varied contexts and manifold risk factors. [86, 87] Another key aspect is that fundamental causes, such as SES, reduce access to resources—such as money, status, social support, housing—that could reduce vulnerability to disease as well as limit its consequences. [86, 87] Hatzenbuehler, Link and Phelan [88] also highlight the role of stigma as a fundamental cause, whereby multiple stigmatized identities (race, gender, sexuality, etc.) can lead to limited access to resources and increased vulnerability to poor health. The relationships between housing insecurity with health outcomes may be further complicated when multiple forms of discrimination are considered.
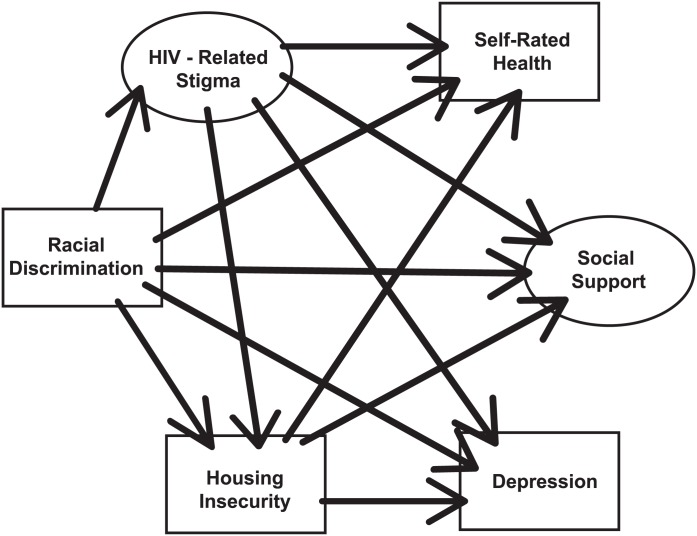
The purpose of this study was to extend prior research on stigma and health correlates of housing insecurity among WLWH by examining pathways between a) forms of social inequities (racial discrimination → HIV-related stigma; racial discrimination and HIV-related stigma → housing insecurity), and b) social inequities (HIV-related stigma, racial discrimination, housing insecurity) and indicators of wellbeing (depression, social support, self-rated health). We developed a conceptual model building on prior research, depicted in Fig 1. As illustrated in the model, we hypothesized that a) racial discrimination would increase HIV-related stigma; b) HIV-related stigma and racial discrimination would be associated with increased housing insecurity; c) racial discrimination, HIV-related stigma, and housing insecurity would contribute to reduced wellbeing, specifically higher depression, lower social support and lower self-rated health.
Fig 1. Tested conceptual model of the relationship between HIV-related stigma, racial discrimination, housing insecurity and wellbeing among African and Caribbean women living with HIV in Ontario.
Fig 1 depicts hypothesized relationships between variables analyzed in the model. Solid lines represent hypothesized direct effects. Ovals represent latent variables, and rectangles represent observed variables.
Methods
We implemented a cross-sectional survey in 5 Ontario cities to explore stigma, health and social support factors associated with food and housing insecurity among ACB WLWH. The survey completion time was approximately 90 minutes, and participants were provided referrals and resources for social and health services in their region upon completion. Participant inclusion criteria were being 18 years or older, self-identifying as a HIV-positive woman, English speaking, and identifying as being an African or Caribbean Black (ACB) woman. Respondents provided written informed consent prior to survey participation and received a small honorarium. Research Ethics Board approval was obtained from Women’s College Research Institute at Women’s College Hospital, University of Toronto.
We worked with nine peer research assistants (PRA) who were ACB WLWH, employed or volunteers with community organizations serving PLHIV in 3 Ontario cities. Following adaptations made from recommendations following a pilot test, the questionnaire was implemented by PRA between June 2010 and January 2011. Participants were recruited using purposive and convenience sampling from community-based ethno-racial and HIV organizations, community health centers, clinics and hospitals. We aimed to recruit 200 participants with an equal proportion of African and Caribbean ethnicity. There is no standardized sample size for SEM; [89] with 6 variables, including 2 latent variables with a combined 9 indicators, this sample size included at least 10 cases per variable.
Measures
We assessed socio-demographic variables including income, age, education and ethnicity. We assessed housing insecurity with a dichotomous measure (yes/no) of monthly ability to pay for rent/mortgage. We measured two types of stigma and discrimination: HIV-related and racial. We used the 10-item “Stigma Scale Revised” to measure multidimensional forms of HIV-related stigma, including personalized, disclosure concerns, negative self-image, and public attitudes. [90, 91] Cronbach’s αs were: personalized stigma subscale = 0.89, disclosure subscale = 0.76, negative self-image subscale = 0.87, public attitudes subscale = 0.76. We adapted the 8-item “Everyday Discrimination Scale” items from measuring general discrimination (‘In your day-to-day life how often have any of the following things happened to you?’) to assess racial discrimination (based on your race) (Cronbach’s α = 0.91). [92]
Social support was assessed using the 19-item MOS Social Support Survey that included emotional, informational, tangible, affectionate, and positive social interaction sub-scales. [93] Social support access was assessed on a 5-point scale. Cronbach’s αs were: emotional support subscale = 0.92, informational support subscale = 0.79, tangible support subscale = 0.86, affectionate support subscale = 0.61, positive social interaction subscale = 0.93. To assess depression we used the 7-item Beck Depression Inventory Fast-Screen (BDI-FS) to elicit a rapid assessment of affective and cognitive dimensions of depression (Cronbach’s α = 0.85). [94] We omitted the suicidality item due to lack of PRA training on mental health crises; prior studies found omission of this item did not alter scale reliability. [95] A single-item global self-rated health indicator recommended by the World Health Organization was used. [96]
Statistical Analyses
We conducted descriptive statistics to calculate means and standard deviations of continuous variables, and frequencies of categorical variables. Scale items were summed in order to calculate total scale scores, and sub-scale scores where applicable. Scale reliability was assessed using Cronbach’s alpha. Non-missing responses were included in data analyses. There were 173 participants who completed the survey; we included 157 participants with complete data in the analyses. There were no significant differences in socio-demographics or outcome variables between participants included and excluded in the analyses. We conducted independent sample t-tests for continuous variables, and chi-square analyses for categorical variables, to examine differences across key outcome variables between persons who were, and were not, experiencing housing insecurity. We also assessed differences between African and Caribbean participants using independent sample t-tests and chi-square analyses.
Structural equation modeling (SEM) using maximum likelihood estimation was conducted to evaluate the hypothesized conceptual model (Fig 1). SEM can include observed as well as latent variables; we developed 2 latent variables (HIV-related stigma that included personalized, disclosure concerns, negative self-image, and public attitudes sub-scales; social support that included emotional, informational, tangible, affectionate and positive social interaction subscales). The observed variables of depression and racial discrimination were continuous variables, and housing insecurity categorical. Model fit was determined using: chi-square; Root-Mean Square Error of Approximation (RMSEA), where a score less than 0.08 indicates an acceptable fit; Comparative Fit Index (CFI), where a score greater than 0.90 is an acceptable fit, and the Tucker-Lewis Index (TLI) with a desired value of >0.90.[97] Analyses were conducted using IBM SPSS 22 and IBM AMOS 23.
Results
We present descriptive statistics of participant characteristics in Table 1 by African and Caribbean ethnicity.
Table 1. Socio-demographic Characteristics of Survey Participants (n = 173) by Ethnicity in the African and Caribbean Black Women’s Stigma and Health Study: Ontario, Canada, 2010–2011.
| Individual Variables | Mean (SD)* | |||
|---|---|---|---|---|
| Overall sample mean score | African participants (n = 73)* | Caribbean participants (n = 72)* | p-value of differences | |
| Age (years) (n = 173) | 40.7 (8.8) | 40.2 (SD: 9.1) | 40.9 (SD: 8.7) | t = 0.52 (df: 142), p = 0.61 |
| Monthly income (US$) | 3917.8 (11589.3); median: 1400.00 (range 0–7916) | 3753.1 (SD: 12112.3) | 4175.7 (SD: 11885.3) | t = 0.20 (df: 124), p = 0.84 |
| n (%)* | n (%)* | |||
| African participants (n = 73) | Caribbean participants (n = 72) | p-value of differences | ||
| Highest level of education completed | χ2(3, N = 137) = 2.98, p = 0.70 | |||
| Less than high school | 16 (23%) | 20 (29%) | ||
| High school | 16 (23%) | 20 (29%) | ||
| College diploma | 23 (33%) | 18 (27%) | ||
| University degree | 14 (20%) | 10 (15%) | ||
| Location of residence | χ2 (5, N = 145) = 26.26, p<0.001 | |||
| Toronto | 22 (30%) | 50 (69%) | ||
| Ottawa | 17 (23%) | 8 (11%) | ||
| Windsor | 8 (11%) | 0 (0%) | ||
| Niagara Falls | 8 (11%) | 6 (8%) | ||
| Kitchener | 9 (12%) | 4 (6%) | ||
| Hamilton | 9 (12%) | 4 (6%) | ||
| Relationship status | χ2 (6, N = 142) = 4.12, p = 0.66 | |||
| Single | 27 (38%) | 33 (49%) | ||
| Married | 14 (20%) | 12 (18%) | ||
| Separated | 8 (11%) | 11 (16%) | ||
| In a relationship/dating | 11 (16%) | 5 (7%) | ||
| Widowed | 7 (10%) | 5 (7%) | ||
| Common law/living with partner | 2 (3%) | 1 (1%) | ||
| Divorced | 2 (3%) | 1 (1%) | ||
| Employment status | χ2 (4, N = 145) = 0.73, p = 0.95 | |||
| Part-time | 9 (12%) | 12 (17%) | ||
| Full-time | 14 (19%) | 11 (15%) | ||
| ODSP (disability) | 37 (51%) | 35 (49%) | ||
| Social assistance (welfare) | 9 (12%) | 10 (14%) | ||
| Canadian Pension Plan (retired) | 4 (6%) | 4 (6%) | ||
| Income insecurity+ | ||||
| Rent/mortgage in full every month on time | 14 (20%) | 19 (28%) | χ2 (1, N = 140) = 1.19, p = 0.28 | |
| Food each month | 29 (40%) | 36 (50%) | χ2 (1, N = 145) = 1.55, p = 0.21 | |
| Medication costs not covered by other sources | 21 (30%) | 22 (33%) | χ2 (1, N = 136) = 0.18, p = 0.67 | |
| Transportation costs every month | 32 (44%) | 31 (44%) | χ2 (1, N = 142) = 0.00, p = 0.99 | |
| Childcare costs | 34 (49%) | 24 (36%) | χ2 (1, N = 136) = 2.52, p = 0.11 | |
| Heating/cooling of your room/apartment/home | 47 (64%) | 46 (66%) | χ2 (1, N = 143) = 0.03, p = 0.87 | |
| Supplements, or other forms of healthcare | 47 (65%) | 49 (70%) | χ2 (1, N = 142) = 0.36, p = 0.55 | |
| Fun activities (i.e. movies, go out to dinner) | 54 (74%) | 46 (68%) | χ2 (1, N = 141) = 0.68, p = 0.41 | |
| Perceived poverty: “I think of myself as poor” | χ2(4, N = 141) = 8.23, p = 0.14 | |||
| Strongly disagree | 3 (4%) | 7 (10%) | ||
| Disagree | 3 (4%) | 9 (13%) | ||
| Neither agree nor disagree | 17 (23%) | 18 (27%) | ||
| Agree | 29 (40%) | 22 (32%) | ||
| Strongly agree | 21 (29%) | 12 (18%) |
+ Income insecurity assessed by participant reporting not enough income monthly to pay for each variable listed (i.e. rent, food).
*calculated from non-missing responses; participants were permitted to decline responding to items
In the overall sample, participants' (n = 173) mean age was 40.7 years (SD 8.8) and median monthly income was $1400.00 (range 0–7917). Out of 145 participants who reported their ethnicity, about half identified as African and half as Caribbean ethnicity; over two-thirds had completed high school or more; and two-thirds were receiving government assistance as their income, including disability, welfare or pension plans. Almost one-quarter of participants (n = 157) reported not having enough income to pay for rent/mortgage each month (22.5%; n = 39). There were no significant differences between African and Caribbean participants with the following variables: age, income, HIV-related stigma, social support, income security, including housing security, depression, or quality of life (not shown). African participants were more likely than Caribbean participants to live outside of Toronto, and to experience higher racial discrimination: t (138) = 3.14, p = 0.002, (CI: 1.48, 6.52) (not shown).
As presented in Table 2, participants reporting housing insecurity had significantly lower income and social support, and higher HIV-related stigma and depression scores, than participants with secure housing.
Table 2. Socio-demographic, Stigma, and Health Variables by Housing Insecurity Among Survey Participants in the African and Caribbean Black Women’s Stigma and Health Study: Ontario, Canada, 2011.
| Variable | Experiencing Housing Insecurity (n = 157) | ||||
|---|---|---|---|---|---|
| Yes (n = 39) | No (n = 118) | T-test/Chi-square test result | p value | ||
| Socio-demographics | |||||
| Age (mean) | 40.31 | 40.64 | t(155) = 0.205, (CI: -2.89, 3.55) | 0.84 | |
| Income (mean) | 1772.06 | 4729.84 | t(155) = -2.52, (CI: -637.52, -5278.03) | 0.01** | |
| Ethnicity | |||||
| African | 14 | 57 | χ2(1, N = 140) = 0.79 | 0.37 | |
| Caribbean | 19 | 50 | |||
| Education (n = 148) | |||||
| High school or less | 19 | 62 | χ2(1, N = 148) = 0.23 | 0.63 | |
| More than high school | 18 | 49 | |||
| Place of Residence | |||||
| Outside Toronto | 18 | 56 | χ2(1, N = 157) = 0.02 | 0.89 | |
| In Toronto | 21 | 62 | |||
| Stigma (mean) | |||||
| HIV-related stigma | 37.53 | 34.62 | t(155) = 2.02, (CI: 0.07, 5.75) | 0.04* | |
| Racial discrimination | 31.01 | 28.93 | t(155) = 1.41, (CI: -0.84, 5.00) | 0.16 | |
| Health Outcomes (mean) | |||||
| Depression | 6.46 | 4.82 | t(155) = 2.21, (CI: 0.17, 3.10) | 0.03* | |
| Social support | 50.92 | 59.60 | t(155) = -2.64, (CI: -15.19, -2.17) | 0.01** | |
| Self-rated health | 3.08 | 3.37 | t(155) = -1.49, (CI: -0.69, 0.09) | 0.14 | |
Total sample size = 173, but for these analyses, n = 157 for housing insecurity (unless otherwise specified for ethnicity and education) because of missing data on outcomes of interest; participants were permitted to decline responding to items.
*p<0.05;
**p≤0.01
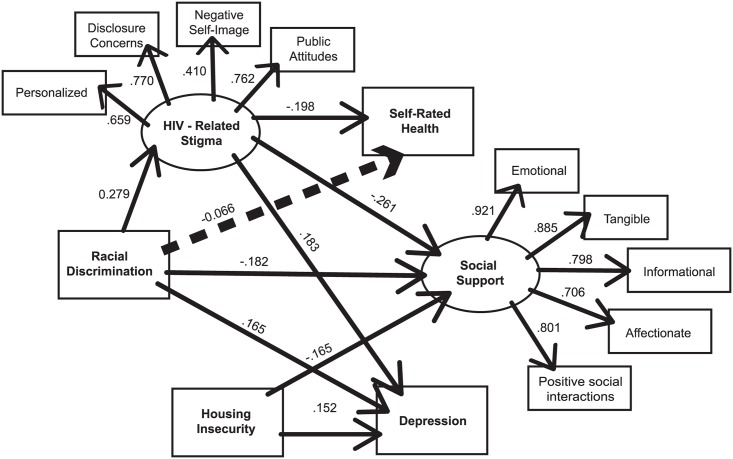
The goal of the study was to develop a useful conceptual model of the relationships between HIV-related stigma, racial discrimination, housing insecurity, and wellbeing (depression, social support, self-rated health). The final model fit the data very well: χ2 (45, n = 154) = 54.28, p = 0.387; CFI = 0.997; TLI = 0.996; RMSEA = 0.016. The significant paths are presented in Fig 2. Paths in the final model were significant except for direct paths between: HIV-related stigma → housing insecurity; racial discrimination → housing insecurity; racial discrimination → SRH, and housing insecurity → SRH. Standardized and unstandardized coefficients are presented in Table 3.
Fig 2. Final model of the relationship between HIV-related stigma, racial discrimination, housing insecurity and wellbeing among African and Caribbean women living with HIV in Ontario (n = 157).
Fig 2 depicts the relationships between the latent variables (depicted as ovals) and observed variables (depicted as rectangles). Solid lines represent statistically significant direct effects and dotted lines represent statistically significant indirect effects. The standardized path coefficients next to each arrow reflect the strength and direction of the effect between variables, and the coefficient is similar to standardized beta weights in regression modeling.
Table 3. Parameter Estimates for Final Path Model in African and Caribbean Black Women’s Stigma and Health Study: Ontario, Canada, 2011 (n = 157).
| Parameter | Coefficient (SE) | Critical Ratio | p | Standardized |
|---|---|---|---|---|
| Racial discrimination on | ||||
| HIV-related stigma | 0.082 (0.025) | 3.245 | 0.001 | 0.279 |
| Housing insecurity | 0.006 (0.005) | 1.299 | 0.194 | 0.103 |
| Depression | 0.081 (0.035) | 2.332 | 0.020 | 0.165 |
| Social support | -0.024 (0.010) | -2.473 | 0.013 | -0.182 |
| Self-rated health | -0.070 (0.042) | -1.654 | 0.098 | -0.132 |
| HIV-related stigma on | ||||
| Housing insecurity | 0.013 (0.018) | 0.708 | 0.479 | 0.063 |
| Depression | 0.309 (0.146) | 2.108 | 0.035 | 0.183 |
| Social support | -0.116 (0.038) | -3.076 | 0.002 | -0.261 |
| Self-rated health | -0.357 (0.167) | -2.142 | 0.032 | -0.198 |
| Housing insecurity on | ||||
| Depression | 1.275 (0.556) | 2.251 | 0.024 | 0.152 |
| Social support | -0.365 (0.155) | -2.353 | 0.019 | -0.165 |
| Self-rated health | 0.012 (0.691) | 0.018 | 0.986 | 0.001 |
| Latent variables: | ||||
| Social support | ||||
| Emotional support | 1.000 | 0.921 | ||
| Informational support | 0.906 (0.061) | 14.857 | <0.0001 | 0.885 |
| Tangible support | 0.869 (0.074) | 11.686 | <0.0001 | 0.798 |
| Affectionate support | 0.937 (0.084) | 11.096 | <0.0001 | 0.706 |
| Positive social interactions | 0.873 (0.064) | 13.629 | <0.0001 | 0.801 |
| HIV-related stigma | ||||
| Personalized stigma | 1.000 | 0.659 | ||
| Disclosure concerns | 0.685 (0.092) | 7.463 | <0.0001 | 0.770 |
| Negative self-image | 0.669 (0.146) | 4.592 | <0.0001 | 0.410 |
| Public attitudes | 0.671 (0.090) | 7.443 | <0.0001 | 0.762 |
SEM results are presented in Table 3. As hypothesized, racial discrimination had a significant direct effect on HIV-related stigma (standardized regression weight: 0.279, p = 0.005), depression (standardized regression weight: 0.164, p = 0.020) and social support (standardized regression weight: -0.182, p = 0.013). There was a significant indirect effect of racial discrimination on SRH via the mediator of HIV-related stigma (standardized regression weight = -0.066, p = 0.028).
HIV-related stigma had a significant direct effect on depression (standardized regression weight = 0.183, p = 0.035), social support (standardized regression weight = -0.261, p = 0.002), and SRH (standardized regression weight = -0.198, p = 0.032). Housing insecurity had significant direct effects on depression (standardized regression weight = 0.152, p = 0.024) and social support (standardized regression weight = -0.165, p = 0.019).
Discussion
Current available literature assessing the impacts of housing insecurity on PLHIV focuses on risk practices, [65, 98] drug use, [65, 99] adherence to ARVs, [99, 100] and access to health care. [101] To our knowledge, only two qualitative studies have explored housing insecurity and its connection with stigma, discrimination and health outcomes among WLWH in Canada. [72, 74] Our study builds on these, using SEM techniques, to further conceptualize the relationships between stigma, housing insecurity and wellbeing of WLWH.
We found housing insecurity had direct effects on both increased depression and reduced social support outcomes. This finding is consistent with prior research reporting correlations between economic insecurity, including housing insecurity, and deleterious health outcomes, [59, 68, 69, 102, 103] such as higher rates of depressive symptoms. [68, 69, 104]. Research also highlights that poor health outcomes such as depressive symptoms are particularly high among WLWH [15, 105–107] who experience economic insecurity. [108] This finding is also congruent with fundamental cause theory that posits SES as a distal cause of disease. [86] ACB WLWH who experienced more housing insecurity reported lower social support, corroborating prior research that posits economic insecurity is a barrier to realizing social cohesion. [79] Poverty may be associated with smaller social networks and connections, and reduced positive interpersonal relationships. [86, 109] Social isolation, rejection and devaluation are fundamental components of stigma associated with poverty, HIV and other marginalized identity characteristics. [110] This extends previous work on poverty and social support to highlight the relationship between a particular form of poverty (housing insecurity) and social support among an understudied group, ACB WLWH. We did not find significant differences in self-rated health between participants who experienced housing insecurity and those who did not; this is an area for future research.
Experiencing racial discrimination was associated with a greater likelihood of experiencing HIV-related stigma. This highlights intersectional stigma, [9] the intersection of social exclusion based on multiple marginalized identity categories such as race and HIV positive serostatus. [9] Since the beginning of the epidemic social constructions of HIV as a ‘Haitian’ or ‘African’ disease reproduced racist stereotypes of Black persons rooted in notions of danger and sexual deviance. [111–115] Stigma may be higher for WLWH who are racialized. [116] Racism is embedded in HIV-related stigma as experienced by Black PLHIV, [117] suggesting the need for complex and multi-level interventions to tackle intersectional stigma. [9]
As hypothesized, racial discrimination and HIV-related stigma were associated with depression and lower social support, and HIV-related stigma was directly correlated with lower-self rated health and mediated the relationship between racial discrimination and self-rated health. The mediation finding suggests that women who experienced higher racial discrimination also experienced higher HIV-related stigma, and this increased HIV-related stigma directly contributed to poorer self-rated health. This reflects literature conducted among general populations that demonstrates harmful impacts of racism on health and wellbeing, [28] among PLHIV that illuminates the negative psychosocial and physical health effects of HIV-related stigma, [22, 27] particularly among racialized women who are already marginalized (e.g. based on race, sex and class). [11, 12, 106, 107]
Prior research indicates that culturally-related factors, such as strong racial or ethnic identity, [118] may buffer the impacts of racial and ethnic discrimination. [119, 120] Other research, including the minority stress model [121, 122], postulates that factors such as social support may reduce the influence of daily stressors from discrimination on wellbeing. The role of strong racial/ethnic identity as a protective factor may be influenced by other factors such as HIV-related stigma, and little is known about the relationship between social support and racial/ethnic identity among WLWH. Exploring both social support and strong racial/ethnic identity as potential mediators of this relationship among ACB WLWH warrants further investigation.
Contrary to our hypotheses, we did not find that racial discrimination or HIV-related stigma were significantly associated with housing insecurity. Rather, results suggest that ACB WLWH who were housing secure and housing insecure experienced similar levels of racial discrimination and HIV-related stigma. We employed measures of individual-level racial discrimination and HIV-related stigma, or of stigma and discrimination perceived by participants from other individuals. Future work may aim to include measures of structural racism and HIV-related stigma (e.g., federal policy, bank lending practices, real estate industry discrimination) to determine whether structural-level discrimination is associated with housing insecurity within this population. [31–33] Future research could also involve longitudinal analyses to better understand trajectories of housing insecurity and how these may be associated with changing levels of HIV-related stigma and/or racial discrimination following HIV diagnoses.
Limitations
Our study design has limitations. First, our small non-probability sample limits generalizability of findings to other ACB WLWH. The purposive sampling design resulted in participants who had access to HIV services and organizational support, so we could have oversampled WLWH who were experiencing challenges with poverty and stigma. To produce generalizable findings with ACB WLWH, researchers should utilize random sampling to engage a representative sample of participants. Second, the cross-sectional nature of the study precludes assessment of causation, limiting our understandings of the exact nature of the relationship between economic insecurity, stigma and health. Causal pathways could be better clarified with a longitudinal study design. Third, we did not measure stigma associated with poverty, which could reproduce social exclusion. [110] Fourth, the racial discrimination scale focused on enacted stigma and did not assess the multi-dimensional aspects of stigma included in the HIV-related stigma scale. Conceptually stigma includes discriminatory processes but extends beyond this to integrate stereotypes and negative attitudes towards one’s groups. [123] Fifth, we aimed to recruit 200 participants but were not able to reach this target; this could be indicative of HIV-related stigma as a barrier to HIV research participation among ACB WLWH. If persons who experienced high levels of HIV-related stigma did not participate in this study, the study results may in fact underestimate the harmful effects of stigma on wellbeing among ACB WLWH. Finally, we aggregated data for African and Caribbean WLWH due to the small sample sizes in this study. African participants reported higher racial discrimination than Caribbean participants, and future research could further explore this phenomenon and its impact on health and wellbeing among WLWH.
Conclusions
Our study has several strengths despite these limitations. To our knowledge this is the first study to examine associations between housing insecurity, racial discrimination, HIV-related stigma, and several indicators of wellbeing (social support, depression, self-rated health) among WLWH. Findings support the salience of housing insecurity as a fundamental cause of health, and highlight the utility of applying intersectionality theory [9] to better understand the unique experiences of HIV-related stigma, racial discrimination, and wellbeing among precariously housed ACB WLWH. The confluence of poverty, HIV-related stigma and racial discrimination appears to result in multiple pathways that contribute to poor wellbeing.
We highlight alarming rates of housing insecurity among ACB WLWH. This points to the urgent need for poverty reduction strategies and for understanding the root causes of economic insecurity. Approximately two-thirds of participants received government assistance, raising questions about social policies that may perpetuate institutionalized economic exclusion of PLHIV. Further attention to social policies and assessment of their impact on PLHIV’s wellbeing is warranted. [124]
In addition to addressing housing insecurity, preventive interventions could focus on reducing stigma and building social support. A recent systematic review on stigma reducing interventions for African and Black women highlighted limited interventions developed to reduce stigma among ACB WLWH, and none that addressed poverty, gender or racial discrimination. [23] While there were promising studies from the U.S. that demonstrated the potential to help ACB WLHW cope with stigma and promote self-care, the focus was on the individual. [23] Future interventions could address multiple forms of stigma—and how they are intertwined with poverty—at community and structural levels. Another recent systematic review reported that support group participation was correlated with reduced mortality and morbidity, improved retention in care, and higher QOL among PLHIV. [78] Future interventions could tailor social support groups for ACB WLHW, with a focus on reducing stigma, poverty and depression.
To conclude, our results underscore the salience of fundamental cause theory to explore experiences of housing insecurity among ACB WLWH. The significant pathway between racial discrimination and HIV-related stigma supports the examination of marginalization associated with multiple identities. Understanding the complex interactions between structural issues such as housing insecurity, community level stigma and social exclusion, and wellbeing among ACB WLWH can inform multi-level interventions to alleviate poverty, reduce stigma, and build social support networks.
Acknowledgments
We would like to acknowledge of all of the women who participated and shared their time, knowledge, and experiences as peer research assistants and in-depth interview participants. We are grateful to the executive director, staff, and research coordinators at Women’s Health in Women’s Hands Community Health Centre; the frontline AIDS Service Organizations in Toronto, Ottawa, Hamilton, London and Windsor; Black Coalition for AIDS Prevention (BlackCAP). We also thank Megan Rio, the graphic designer who created the figures.
Data Availability
Due to the small sample size and confidentiality concerns, the research team members only have access to the dataset. The authors can be contacted to provide the dataset for researchers; this will necessitate applying for and receiving an amended research ethics approval for non-research team members to access the data. Please contact Women’s College Hospital Research Ethics Board, Toronto, ON, Canada. Contact information: Melissa Sidhu, REB Coordinator; WCH Research Ethics Board; 76 Grenville Street, Room 6341; Toronto ON M5S 1B2; phone: 416-351-3732 x 2723; email: melissa.sidhu@wchospital.ca.
Funding Statement
This work was funded by Canadian Institutes of Health Research, grant# ZNF-107573. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.PHAC. HIV and AIDS in Canada Surveillance Reort to December 31, 2008. Ottawa: Public Health Agency of Canada, 2009. [Google Scholar]
- 2.Centre for Disease Control. HIV Among African Americans Online2014 [cited 2016 June 9]. Available: http://www.cdc.gov/hiv/group/racialethnic/africanamericans/index.html.
- 3.Gupta GR, Parkhurst JO, Ogden JA, Aggleton P, Mahal A. Structural approaches to HIV prevention. Lancet. 2008;372(9640):764–75. 10.1016/S0140-6736(08)60887-9 . [DOI] [PubMed] [Google Scholar]
- 4.Auerbach JD, Parkhurst JO, Caceres CF. Addressing social drivers of HIV/AIDS for the long-term response: conceptual and methodological considerations. Global public health. 2011;6 Suppl 3:S293–309. 10.1080/17441692.2011.594451 . [DOI] [PubMed] [Google Scholar]
- 5.Baral S, Logie C, Grosso A, Wirtz AL, Beyrer C. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health. 2011;13:482 10.1186/1471-2458-13-482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buot ML, Docena JP, Ratemo BK, Bittner MJ, Burlew JT, Nuritdinov AR, et al. Beyond race and place: distal sociological determinants of HIV disparities. PloS one. 2014;9(4):e91711 10.1371/journal.pone.0091711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sherr L, Clucas C, Harding R, Sibley E, Catalan J. HIV and depression—a systematic review of interventions. Psychology, health & medicine. 2011;16(5):493–527. 10.1080/13548506.2011.579990 . [DOI] [PubMed] [Google Scholar]
- 8.Newman PA, Williams CC, Massaquoi N, Brown M, Logie C. HIV prevention for Black women: structural barriers and opportunities. Journal of health care for the poor and underserved. 2008;19(3):829–41. 10.1353/hpu.0.0043 . [DOI] [PubMed] [Google Scholar]
- 9.Logie CH, James L, Tharao W, Loutfy MR. HIV, gender, race, sexual orientation, and sex work: a qualitative study of intersectional stigma experienced by HIV-positive women in Ontario, Canada. PLoS Med. 2011;8(11):e1001124 10.1371/journal.pmed.1001124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mahajan AP, Sayles JN, Patel VA, Remien RH, Sawires SR, Ortiz DJ, et al. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. Aids. 2008;22 Suppl 2:S67–79. Epub 2008/07/25. 10.1097/01.aids.0000327438.13291.62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loutfy MR, Logie CH, Zhang Y, Blitz SL, Margolese SL, Tharao WE, et al. Gender and ethnicity differences in HIV-related stigma experienced by people living with HIV in Ontario, Canada. PloS one. 2012;7(12):e48168 10.1371/journal.pone.0048168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Emlet CA. Experiences of stigma in older adults living with HIV/AIDS: a mixed-methods analysis. AIDS patient care and STDs. 2007;21(10):740–52. 10.1089/apc.2007.0010 . [DOI] [PubMed] [Google Scholar]
- 13.Herek GM, Mitnick L, Burris S, Chesney M, Devine P, Fullilove MT, et al. Workshop report: AIDS and stigma—A conceptual framework and research agenda. AIDS and Public Policy Journal. 1998;13:36–47. [PubMed] [Google Scholar]
- 14.Mcnair LD, Prather CM. African American women and AIDS: Factors influencing risk and reaction to HIV disease. Journal of Black Psychology. 2004;30:106–23. [Google Scholar]
- 15.Sandelowski M, Lambe C, Barroso J. Stigma in HIV-positive women. J Nurs Scholarsh. 2004;36(2):122–8. . [DOI] [PubMed] [Google Scholar]
- 16.Sandelowski M, Barroso J, Voils CI. Gender, race/ethnicity, and social class in research reports on stigma in HIV-positive women. Health Care Women Int. 2009;30(4):273–88. 10.1080/07399330802694880 . [DOI] [PubMed] [Google Scholar]
- 17.Collins PH. Black Feminist Thought: Knowledge, Consciousness, and the Politics of Empowerment: Psychology Press; 2000. [Google Scholar]
- 18.Purdie-Vaughns V, Eibach RP. Intersectional Invisibility: the Distinctive Advantages and Disadvantages of Multiple Subordinate-Group Identities. Sex Roles. 2008;59:377–91. [Google Scholar]
- 19.Link BG, Phelan JC. Conceptualizing Stigma. Annu Rev Socio. 2001;27:363–85. [Google Scholar]
- 20.Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. American journal of public health. 2013;103(5):813–21. 10.2105/AJPH.2012.301069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krieger N. Theories for social epidemiology in the 21st century: an ecosocial perspective. International journal of epidemiology. 2001;30(4):668–77. . [DOI] [PubMed] [Google Scholar]
- 22.Logie C, Gadalla TM. Meta-analysis of health and demographic correlates of stigma towards people living with HIV. AIDS care. 2009;21(6):742–53. 10.1080/09540120802511877 . [DOI] [PubMed] [Google Scholar]
- 23.Loutfy M, Tharao W, Logie C, Aden MA, Chambers LA, Wu W, et al. Systematic review of stigma reducing interventions for African/Black diasporic women. Journal of the International AIDS Society. 2015;18:19835 10.7448/IAS.18.1.19835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? Journal of the International AIDS Society. 2013;16(3 Suppl 2):18734 10.7448/IAS.16.3.18734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mak WW, Poon CY, Pun LY, Cheung SF. Meta-analysis of stigma and mental health. Social science & medicine. 2007;65(2):245–61. 10.1016/j.socscimed.2007.03.015 . [DOI] [PubMed] [Google Scholar]
- 26.Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS and behavior. 2009;13(6):1160–77. 10.1007/s10461-009-9593-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS and behavior. 2013;17(5):1785–95. 10.1007/s10461-013-0437-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Paradies Y. A systematic review of empirical research on self-reported racism and health. International journal of epidemiology. 2006;35(4):888–901. 10.1093/ije/dyl056 . [DOI] [PubMed] [Google Scholar]
- 29.Jones CP. Levels of racism: a theoretic framework and a gardener's tale. American journal of public health. 2000;90(8):1212–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shorter-Gooden K. Multiple resistance strategies: How African American women cope with racism and sexism. Journal of Black Psychology. 2004;30(19). [Google Scholar]
- 31.Williams DR. Race, socioeconomic status, and health. The added effects of racism and discrimination. Annals of the New York Academy of Sciences. 1999;896:173–88. . [DOI] [PubMed] [Google Scholar]
- 32.Saegert SC, Evan GW. Poverty, housing niches, and health in the United States. Journal of Social Issues. 2003;59(3):569–89. [Google Scholar]
- 33.Massey DE, Denton NA. American apartheid: Segregation and the making of the underclass. Cambridge, MA: Harvard University Press; 1993. [Google Scholar]
- 34.Lenon S. Living on the edge: women, poverty and homelessness in Canada. Canadian Woman Studies. 2000;20(3). [Google Scholar]
- 35.Badets J, Howatson-Lwo L. Recent immigrants in the workforce. Canadian Social Trends. 2000;3:15–21. [Google Scholar]
- 36.Kunz JL, M A, S S. Unequal Access: A Canadian Profile of Racial Differences in Education, Employment and Income. Toronto: Canadian Race Relations Foundation, 2002. [Google Scholar]
- 37.Li P. Earning disparities between immigrants and native-born Canadians. Canadian Review of Social Anthropology. 2000;37(3):289–311. [Google Scholar]
- 38.Simich L, Beiser M, Stewart M, Mwakarimba E. Providing social support for immigrants and refugees in Canada: Challenges and Directions. Journal of Immigrant Health. 2005;7(4):259–68. [DOI] [PubMed] [Google Scholar]
- 39.Weis L. Identity formation and the proces of 'othering': unraveling sexual threads. Educational Foundation. 1995;17–33. [Google Scholar]
- 40.Grove NJ, Zwi AB. Our health and theirs: Forced migration, othering, and public health Social Science and Medicine. 2006;62:1931–42. [DOI] [PubMed] [Google Scholar]
- 41.Kirmayer LJ, Narasiah L, Munoz M, Rashid M, Ryder AG, Guzder J, et al. Common mental health problems in immigrants and refugees: general approach in primary care. CMAJ: Canadian Medical Association journal = journal de l'Association medicale canadienne. 2011;183(12):E959–67. 10.1503/cmaj.090292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lindert J, Ehrenstein OS, Priebe S, Mielck A, Brahler E. Depression and anxiety in labor migrants and refugees—a systematic review and meta-analysis. Social science & medicine. 2009;69(2):246–57. 10.1016/j.socscimed.2009.04.032 . [DOI] [PubMed] [Google Scholar]
- 43.Cantor-Graae E. Ethnic minority groups, particularly African–Caribbean and Black African groups, are at increased risk of psychosis in the UK. Evidence Based Mental Health. 2007;10:95 [DOI] [PubMed] [Google Scholar]
- 44.Coid JW, Kirkbride JB, Barker D, Cowden F, Stamps R, Yang M, et al. Raised incidence rates of all psychoses among migrant groups: findings from the East London first episode psychosis study. Arch Gen Psychiatry. 2008;65(11):1250–8. 10.1001/archpsyc.65.11.1250 . [DOI] [PubMed] [Google Scholar]
- 45.Jarvis GE. The social causes of psychosis in North American psychiatry: a review of a disappearing literature. Canadian journal of psychiatry Revue canadienne de psychiatrie. 2007;52(5):287–94. . [DOI] [PubMed] [Google Scholar]
- 46.Noh S, Kaspar V, Wickrama KA. Overt and subtle racial discrimination and mental health: preliminary findings for Korean immigrants. American journal of public health. 2007;97(7):1269–74. 10.2105/AJPH.2005.085316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Noh S, Kaspar V. Perceived discrimination and depression: moderating effects of coping, acculturation, and ethnic support. American journal of public health. 2003;93(2):232–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Noh S, Beiser M, Kaspar V, Hou F, Rummens J. Perceived racial discrimination, depression, and coping: a study of Southeast Asian refugees in Canada. Journal of health and social behavior. 1999;40(3):193–207. . [PubMed] [Google Scholar]
- 49.Teixeira C. Housing experiences of Black Africans in Toronto's Rental Market: A Case Study of Angolan and Mozambican Immigrants. Canadian Ethnic Studies. 2006;38(3):58. [Google Scholar]
- 50.Allan CL, Clarke J. Are HIV/AIDS services in Leeds, UK, able to meet the needs of asylum seekers? Public Health. 2005;119(4):305–11. [DOI] [PubMed] [Google Scholar]
- 51.Chinouya M, Hildreth A, Goodall D, Aspinall P, Hudson A. Migrants and HIV stigma: findings from the Stigma Index Study (UK). Health and Social Care. 2014. 10.1111/hsc.12179 [DOI] [PubMed] [Google Scholar]
- 52.Prost A, Elford J, Imrie J, Petticrew M, Hart GJ. Social, behavioural, and intervention research among people of Sub-Saharan African origin living with HIV in the UK and Europe: literature review and recommendations for intervention. AIDS and behavior. 2008;12(2):170–94. 10.1007/s10461-007-9237-4 . [DOI] [PubMed] [Google Scholar]
- 53.Mackenbach JP, Stirbu I, Roskam AJ, Schaap MM, Menvielle G, Leinsalu M, et al. Socioeconomic inequalities in health in 22 European countries. The New England journal of medicine. 2008;358(23):2468–81. 10.1056/NEJMsa0707519 . [DOI] [PubMed] [Google Scholar]
- 54.Bambra C, Netuveli G, Eikemo TA. Welfare state regime life courses: the development of western European welfare state regimes and age-related patterns of educational inequalities in self-reported health. International journal of health services: planning, administration, evaluation. 2010;40(3):399–420. . [DOI] [PubMed] [Google Scholar]
- 55.Aldabe B, Anderson R, Lyly-Yrianainen M, Parent-Thirion A, Vermeylen G, Kelleher CC, et al. Contribution of material, occupational, and psychosocial factors in the explanation of social inequalities in health in 28 countries in Europe. Journal of Epidemiology and Community Health. 2011;65(12):1123–31. 10.1136/jech.2009.102517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Auger N, Alix C. Income, Income Distribution and Health in Canada In: Raphael D, editor. Social Determinants of Health: Canadian Perspectives. 2 ed Toronto, Canada: Canadian Scholar's Press; 2009. p. 61–74. [Google Scholar]
- 57.James PD, Wilkins R, Detsky AS, Tugwell P, Manuel DG. Avoidable mortality by neighbourhood income in Canada: 25 years after the establishment of universal health insurance. J Epidemiol Community Health. 2007;61(4):287–96. 10.1136/jech.2006.047092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wilkins R, Tjepkema M, Mustard C, Choiniere R. The Canadian census mortality follow-up study, 1991 through 2001. Canada: 2008. [PubMed] [Google Scholar]
- 59.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Painting a truer picture of US socioeconomic and racial/ethnic health inequalities: the Public Health Disparities Geocoding Project. American journal of public health. 2005;95(2):312–23. 10.2105/AJPH.2003.032482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Weinreb L, Goldberg R, Lessard D, Perloff J, Bassuk E. HIV-risk practices among homeless and low-income housed mothers. J Fam Pract. 1999;48(11):859–67. . [PubMed] [Google Scholar]
- 61.Culhane DP, Gollub E, Kuhn R, Shpaner M. The co-occurrence of AIDS and homelessness: results from the integration of administrative databases for AIDS surveillance and public shelter utilisation in Philadelphia. J Epidemiol Community Health. 2001;55(7):515–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wolitski RJ, Pals SL, Kidder DP, Courtenay-Quirk C, Holtgrave DR. The effects of HIV stigma on health, disclosure of HIV status, and risk behavior of homeless and unstably housed persons living with HIV. AIDS and behavior. 2009;13(6):1222–32. 10.1007/s10461-008-9455-4 . [DOI] [PubMed] [Google Scholar]
- 63.Herek GM, Capitanio JP. Public reactions to AIDS in the United States: a second decade of stigma. American journal of public health. 1993;83(4):574–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Herek GM, Capitanio JP, Widaman KF. HIV-related stigma and knowledge in the United States: prevalence and trends, 1991–1999. American journal of public health. 2002;92(3):371–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Leaver CA, Bargh G, Dunn JR, Hwang SW. The effects of housing status on health-related outcomes in people living with HIV: a systematic review of the literature. AIDS and behavior. 2007;11(6 Suppl):85–100. 10.1007/s10461-007-9246-3 . [DOI] [PubMed] [Google Scholar]
- 66.Anderson WJ, Weatherburn P. The needs of people with HIV in the UK: findings from a national survey. Int J STD AIDS. 2004;15(12):793–6. . [DOI] [PubMed] [Google Scholar]
- 67.Raphael D. Poverty in Canada: Implications for health and quality of life. 2 ed Toronto, Canada: Canadian Scholar's Press Inc.; 2011. [Google Scholar]
- 68.Riley ED, Neilands TB, Moore K, Cohen J, Bangsberg DR, Havlir D. Social, structural and behavioral determinants of overall health status in a cohort of homeless and unstably housed HIV-infected men. PloS one. 2012;7(4):e35207 10.1371/journal.pone.0035207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Riley ED, Moore K, Sorensen JL, Tulsky JP, Bangsberg DR, Neilands TB. Basic subsistence needs and overall health among human immunodeficiency virus-infected homeless and unstably housed women. American journal of epidemiology. 2011;174(5):515–22. 10.1093/aje/kwr209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cheung AM, Hwang SW. Risk of death among homeless women: a cohort study and review of the literature. CMAJ: Canadian Medical Association journal = journal de l'Association medicale canadienne. 2004;170(8):1243–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Stewart KE, Cianfrini LR, Walker JF. Stress, social support and housing are related to health status among HIV-positive persons in the deep south of the United States. AIDS care. 2005;17(3):350–8. 10.1080/09540120412331299780 . [DOI] [PubMed] [Google Scholar]
- 72.Greene S, Chambers L, Masinde K, O'Brien-Teengs D. A house is not a home: The housing experiences of African and Caribbean mothers living with HIV. Housing Studies. 2013;28(1):116–34. [Google Scholar]
- 73.Ndlovu U, Ion A, Carvalhal A. "My children and my home": the most recent and challenging stressors of HIV-positive women. Archives of women's mental health. 2010;13(3):215–22. 10.1007/s00737-010-0148-4 . [DOI] [PubMed] [Google Scholar]
- 74.Greene S, Tucker R, Rourke SB, Monette L, Koornstra J, Sobota M, et al. "Under My Umbrella": the housing experiences of HIV positive parents who live with and care for their children in Ontario. Archives of women's mental health. 2010;13(3):223–32. 10.1007/s00737-009-0090-5 . [DOI] [PubMed] [Google Scholar]
- 75.Reblin M, Uchino BN. Social and emotional support and its implication for health. Current opinion in psychiatry. 2008;21(2):201–5. 10.1097/YCO.0b013e3282f3ad89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241(4865):540–5. . [DOI] [PubMed] [Google Scholar]
- 77.Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Social science & medicine. 2000;51(6):843–57. . [DOI] [PubMed] [Google Scholar]
- 78.Bateganya MH, Amanyeiwe U, Roxo U, Dong M. Impact of support groups for people living with HIV on clinical outcomes: a systematic review of the literature. Journal of acquired immune deficiency syndromes. 2015;68 Suppl 3:S368–74. 10.1097/QAI.0000000000000519 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kawachi I, Kennedy BP. Socioeconomic determinants of health: Health and social cohesion: why care about income inequality? British Medical Journal. 1997;(314):1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Moskowitz D, Vittinghoff E, Schmidt L. Reconsidering the effects of poverty and social support on health: a 5-year longitudinal test of the stress-buffering hypothesis. Journal of urban health: bulletin of the New York Academy of Medicine. 2013;90(1):175–84. 10.1007/s11524-012-9757-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Tsai AC, Bangsberg DR, Weiser SD. Harnessing poverty alleviation to reduce the stigma of HIV in Sub-Saharan Africa. PLoS Med. 2013;10(11):e1001557 10.1371/journal.pmed.1001557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.McCoy SK, Major B. Priming meritocracy and the psychological justification of inequality. Journal of Exp Soc Psychol. 2007;43(3):341–51. [Google Scholar]
- 83.Kwate NO, Meyer IH. The myth of meritocracy and African American health. American journal of public health. 2010;100(10):1831–4. 10.2105/AJPH.2009.186445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Simons AM, Groffen DA, Bosma H. Income-related health inequalities: does perceived discrimination matter? International journal of public health. 2013;58(4):513–20. 10.1007/s00038-012-0429-y . [DOI] [PubMed] [Google Scholar]
- 85.Fuller-Rowell TE, Evans GW, Ong AD. Poverty and health: The mediating role of perceived discrimination. Association for Psychological Science. 2012;23(7):734–9. [DOI] [PubMed] [Google Scholar]
- 86.Link BG, Phelan J. Social conditions as fundamental causes of disease. Journal of health and social behavior. 1995;Spec No:80–94. . [PubMed] [Google Scholar]
- 87.Phelan J, Link BG, Tehranifar P. Social conditions as a fundamental cause of health inequalities: Theory, evidence and policy implications. Journal of health and social behavior. 2010;51(S):S28–S40. 10.1177/0022146510383498 [DOI] [PubMed] [Google Scholar]
- 88.Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. American journal of public health. 2013;103(5):813–21. 10.2105/AJPH.2012.301069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wolf EJ, Harrington KM, Clark SL, Miller MW. Sample Size Requirements for Structural Equation Models: An Evaluation of Power, Bias, and Solution Propriety. Educ Psychol Meas. 2013;76(6):913–34. 10.1177/0013164413495237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wright K, Naar-King S, Lam P, Templin T, Frey M. Stigma scale revised: reliability and validity of a brief measure of stigma for HIV+ youth. The Journal of adolescent health: official publication of the Society for Adolescent Medicine. 2007;40(1):96–8. 10.1016/j.jadohealth.2006.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Research in nursing & health. 2001;24(6):518–29. . [DOI] [PubMed] [Google Scholar]
- 92.Clark R, Coleman AP, Novak JD. Brief report: Initial psychometric properties of the everyday discrimination scale in black adolescents. Journal of adolescence. 2004;27(3):363–8. 10.1016/j.adolescence.2003.09.004 . [DOI] [PubMed] [Google Scholar]
- 93.Sherbourne CD, Stewart AL. The MOS social support survey. Social science & medicine. 1991;32(6):705–14. . [DOI] [PubMed] [Google Scholar]
- 94.Beck AT, Guth D, Steer RA, Ball R. Screening for major depression disorders in medical inpatients with the Beck Depression Inventory for Primary Care. Behaviour research and therapy. 1997;35(8):785–91. . [DOI] [PubMed] [Google Scholar]
- 95.Golden J, Conroy RM, O'Dwyer AM. Reliability and validity of the Hospital Anxiety and Depression Scale and the Beck Depression Inventory (Full and FastScreen scales) in detecting depression in persons with hepatitis C. Journal of affective disorders. 2007;100(1–3):265–9. 10.1016/j.jad.2006.10.020 . [DOI] [PubMed] [Google Scholar]
- 96.World Health Organization. Health interview surveys: towards international harmonization. de Bruin A, Picavet HSV, Nossikov N, editors. Copenhagen: World Health Organization; 1996. [PubMed] [Google Scholar]
- 97.Mueller R, Hancock G. Best practices in structural equation modelling In: Osborne J, editor. Best practices in qualtitative methods. Thousand Oaks, CA: Sage; 2008. [Google Scholar]
- 98.Aidala A, Cross JE, Stall R, Harre D, Sumartojo E. Housing status and HIV risk behaviors: implications for prevention and policy. AIDS and behavior. 2005;9(3):251–65. 10.1007/s10461-005-9000-7 . [DOI] [PubMed] [Google Scholar]
- 99.Palepu A, Milloy MJ, Kerr T, Zhang R, Wood E. Homelessness and adherence to antiretroviral therapy among a cohort of HIV-infected injection drug users. Journal of urban health: bulletin of the New York Academy of Medicine. 2011;88(3):545–55. 10.1007/s11524-011-9562-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Uthman OA, Magidson JF, Safren SA, Nachega JB. Depression and adherence to antiretroviral therapy in low-, middle- and high-income countries: a systematic review and meta-analysis. Curr HIV/AIDS Rep. 2014;11(3):291–307. 10.1007/s11904-014-0220-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Aidala AA, Lee G, Abramson DM, Messeri P, Siegler A. Housing need, housing assistance, and connection to HIV medical care. AIDS and behavior. 2007;11(6 Suppl):101–15. 10.1007/s10461-007-9276-x . [DOI] [PubMed] [Google Scholar]
- 102.An Q, Prejean J, McDavid Harrison K, Fnag X. Association between community socioeconomic position and HIV diagnosis among adults and adolescents in the United States, 2005 to 2009. American journal of public health. 2013;103:120–6. 10.2105/AJPH.2012.300853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Denning PH, DiNenno EA, Wiegand RE. Characteristics associated with HIV infection among heterosexuals in urban aeras with high AIDS prevalence—24 cities, United States, 2006–2007. Morbidity and Mortality Weekly Report 60 2011:1045–9. [PubMed] [Google Scholar]
- 104.Schulz AJ, Gravlee CC, Williams DR, Israel BA, Mentz G, Rowe Z. Discrimination, symptoms of depression, and self-rated health among african american women in detroit: results from a longitudinal analysis. American journal of public health. 2006;96(7):1265–70. 10.2105/AJPH.2005.064543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Vyavaharkar M, Moneyham L, Corwin S, Saunders R, Annang L, Tavakoli A. Relationships between stigma, social support, and depression in HIV-infected African American women living in the rural Southeastern United States. The Journal of the Association of Nurses in AIDS Care: JANAC. 2010;21(2):144–52. 10.1016/j.jana.2009.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Morrison MF, Petitto JM, Ten Have T, Gettes DR, Chiappini MS, Weber AL, et al. Depressive and anxiety disorders in women with HIV infection. Am J Psychiatry. 2002;159(5):789–96. 10.1176/appi.ajp.159.5.789 . [DOI] [PubMed] [Google Scholar]
- 107.Moneyham L, Sowell R, Seals B, Demi A. Depressive symptoms among African American women with HIV disease. Sch Inq Nurs Pract. 2000;14(1):9–39; discussion 41–6. . [PubMed] [Google Scholar]
- 108.Riley ED, Gandhi M, Hare C, Cohen J, Hwang S. Poverty, unstable housing, and HIV infection among women living in the United States. Curr HIV/AIDS Rep. 2007;4(4):181–6. . [DOI] [PubMed] [Google Scholar]
- 109.Anand P, Lea S. The psychology and behavioural economics of poverty. Journal of Economic Psychology. 2011;32:284–93. [Google Scholar]
- 110.Phelan JC, Lucas JW, Ridgeway CL, Taylor CJ. Stigma, status, and population health. Social science & medicine. 2014;103:15–23. 10.1016/j.socscimed.2013.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Herek GM. Thinking about AIDS and stigma: a psychologist's perspective. The Journal of law, medicine & ethics: a journal of the American Society of Law, Medicine & Ethics. 2002;30(4):594–607. . [DOI] [PubMed] [Google Scholar]
- 112.Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Social science & medicine. 2003;57(1):13–24. Epub 2003/05/20. . [DOI] [PubMed] [Google Scholar]
- 113.Gilman S. Disease and representation: Images of illness from maddness to AIDS. Ithaca, NY: Cornell University Press; 1988. [Google Scholar]
- 114.Patton C. Globalizing AIDS. Minneapolis: University of Minneapolis Press; 2002. [Google Scholar]
- 115.Farmer P. AIDS and accusation: Haiti, Haitians, and the geography of blame. Culture and AIDS. 1990:67–91. [Google Scholar]
- 116.Santana MA, Dancy BL. The stigma of being named "AIDS carriers" on Haitian-American women. Health Care Women Int. 2000;21(3):161–71. 10.1080/073993300245230 . [DOI] [PubMed] [Google Scholar]
- 117.Lekas HM, Siegel K, Schrimshaw EW. Continuities and discontinuities in the experiences of felt and enacted stigma among women with HIV/AIDS. Qualitative health research. 2006;16(9):1165–90. 10.1177/1049732306292284 . [DOI] [PubMed] [Google Scholar]
- 118.Sellers RM, Shelton JN. The role of racial identity in perceived racial discrimination. J Pers Soc Psychol. 2003;84(5):1079–92. . [DOI] [PubMed] [Google Scholar]
- 119.Lopez SJ, Prosser EC, Edwards LM, Magyar-Moe JL, Neufeld JE, Rasmussen HN. Putting positive psychology in a multicultural context In: Snyder CR, Lopez SJ, editors. Handbook of Positive Psychology. New York: Oxford University Press; 2002. p. 700–14. [Google Scholar]
- 120.Sue DW, Constantine MG. optimal human functioning in people of color in the United States In: Walsh WB, editor. Counseling psychology and optimal health. Mahwah, NJ: Lawrence Erlbaum; 2003. p. 151–69. [Google Scholar]
- 121.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychological bulletin. 2003;129(5):674–97. Epub 2003/09/06. 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Meyer IH. Prejudice and discrimination as social stressors In: Meyer IH, Northridge ME, editors. The Health of Sexual Minorities. USA: Springer US; 2007. p. 242–67. [Google Scholar]
- 123.Phelan JC, Link BG, Dovidio JF. Stigma and prejudice: one animal or two? Social science & medicine. 2008;67(3):358–67. 10.1016/j.socscimed.2008.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Rueda S, Chambers L, Wilson M, Mustard C, Rourke SB, Bayoumi A, et al. Association of reutrning to work with better health in working-aged adults: A systematic review. American journal of public health. 2012;102(3):541–56. 10.2105/AJPH.2011.300401 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to the small sample size and confidentiality concerns, the research team members only have access to the dataset. The authors can be contacted to provide the dataset for researchers; this will necessitate applying for and receiving an amended research ethics approval for non-research team members to access the data. Please contact Women’s College Hospital Research Ethics Board, Toronto, ON, Canada. Contact information: Melissa Sidhu, REB Coordinator; WCH Research Ethics Board; 76 Grenville Street, Room 6341; Toronto ON M5S 1B2; phone: 416-351-3732 x 2723; email: melissa.sidhu@wchospital.ca.