Abstract
Objective
To examine the dynamic relationship between treatment expectations and treatment outcome over the course of a clinical trial for winter seasonal affective disorder (SAD).
Method
Currently depressed adults with Major Depression, Recurrent with Seasonal Pattern (N = 177) were randomized to 6-weeks of group-delivered cognitive-behavioral therapy for SAD (CBT-SAD) or light therapy (LT). The majority was female (83.6%) and white (92.1%), with a mean age of 45.6 years. Treatment expectations for CBT-SAD and LT were assessed using a modification of the Treatment Expectancy and Credibility Survey (Borkovec & Nau, 1972). Depression severity was assessed using the Beck Depression Inventory-Second Edition (Beck, Steer, & Brown, 1996). All measures were administered at pre-treatment, mid-treatment, and post-treatment.
Results
As treatment progressed, expectations for the treatment received increased across time steeply in CBT-SAD patients and moderately in LT patients. Collapsing across time, patients with higher treatment expectations had lower depression severity than those with lower treatment expectations. In a cross-lagged panel path analysis, there was a significant effect of treatment expectations at mid-treatment on depression severity at post-treatment among CBT-SAD patients.
Conclusions
Treatment expectations changed across treatment, affected outcome, and should be assessed and monitored repeatedly throughout treatment. Findings suggest that treatment expectations at mid-treatment are a mechanism by which CBT-SAD reduces depression, which should be replicated in SAD samples and examined for generalizability to non-seasonal depression. These findings underscore the importance of further research examining treatment expectations in mediating CBT’s effects in depression and other types of psychopathology.
Public Health Significance
This study highlights the importance of monitoring treatment expectations repeatedly during treatment regardless of treatment type. Moreover, therapists administering cognitive-based therapy for depression should actively attend to the degree of patient “buy-in” early in treatment as it has clear indications for depression severity at treatment endpoint.
Keywords: Treatment expectations, seasonal affective disorder, cognitive-behavioral therapy, light therapy
Treatment expectations, regarded as one of several non-specific therapeutic factors, are the amount of improvement patients think will occur over the course of a given treatment (Ilardi & Craighead, 1994). In a cognitive framework, treatment expectations are framed as cognitions that are expected to influence a patient’s affective and behavioral responses to the treatment, potentially impacting measures of treatment efficacy. In a meta-analytic review (Constantino, Arnkoff, Glass, Ametrano, & Smith, 2011) including 8,016 patients across 46 studies, patients’ treatment expectancies had a small but statistically significant association with treatment outcome (r = .12, d = .24). This quantitative review indicates a need for further research regarding how, and to what extent, treatment expectancies play a role in treatment outcome.
In order to increase specificity for the construct of treatment expectations, Borkovec and Nau (1972) developed a five-item measure called the Credibility/Expectancy Questionnaire (CEQ). The sole item on the measure that directly assesses outcome expectancy (i.e., a 1–10 Likert rating of perceived confidence that the treatment will successfully eliminate the presenting problem) has been previously used in studies of treatment expectations as a measure of outcome expectancy (Price, Anderson, Henrich, & Rothbaum, 2008; Vogel, Hansen, Stiles, & Götestam, 2006). Other items on the scale assess related constructs (e.g., motivation to undergo a treatment, the perceived logicalness of the treatment’s rationale). The majority of research examining treatment expectations has used the Borkovec and Nau (1972) scale in its entirety or a later revision of it (Constantino et al., 2011).
One limitation of the existing treatment expectancy literature is that most studies relate this construct, as assessed at baseline, to outcomes at treatment endpoint. However, it is possible that this construct relates to outcome during the course of treatment, such as rate of improvement. For example, Price and Anderson (2012) examined treatment expectancy as a predictor of treatment response in a sample of individuals with social anxiety disorder, specifically, a fear of public speaking. Patients were randomized to exposure therapy delivered through one of two modalities: group-based exposure therapy or virtual reality. A multilevel modeling analysis revealed that treatment expectancy significantly impacted the rate of change in public speaking fears, such that higher levels of pre-treatment expectancy predicted faster rates of improvement on measures of public speaking fears across both treatment conditions. This study indicates that treatment expectancy may be a more complex predictor of change during the course of treatment than simple pre/post analyses of treatment outcome reveal.
Holt and Heimberg (1990) proposed that treatment expectancies are fluid over the course of treatment and should be treated as a dynamic variable that might change. Given that treatment expectancies have not been routinely measured repeatedly, the potentially dynamic relationship between treatment expectancy and outcome remains speculative. To our knowledge only one study has measured treatment expectations repeatedly during treatment (Newman & Fisher, 2010). Newman and Fisher (2010) examined treatment expectations of CBT for Generalized Anxiety Disorder (GAD) four times: after Sessions 4 (after establishing the treatment rationale), 5, 6, and 7 (mid-point in the 14-week treatment), a crucial time for making treatment gains (Tang & DeRubeis, 1999). The primary goal of Newman and Fisher (2010) was to examine if and how change in expectancy mediated treatment outcome. Using data from sessions 4–7 allowed Newman and Fisher to examine treatment expectations in such a way that expectancies were not likely to be confounded with baseline measurements or final outcome measurements. Newman and Fisher showed that expectations of CBT were dynamic, whereby the average expectancy score rose significantly between sessions 4 and 7. Moreover, the rate of change in expectancy between sessions 4–7 positively predicted the extent of change in GAD symptoms at post-treatment after accounting for prior and concurrent anxiety levels, thereby demonstrating that expectancy change preceded GAD symptom change in CBT. Newman and Fisher’s (2010) work is the first to measure and track the potentially dynamic nature of treatment expectations; however, they noted that future work should assess whether the changes in treatment expectations and their effects on outcome are unique to CBT.
The present study extended the work of Newman and Fisher (2010) by measuring changes in treatment expectations over the course of two distinct treatment modalities for seasonal affective disorder (SAD): light therapy (LT) or group cognitive-behavioral therapy tailored for SAD (CBT-SAD). We extended the current literature by repeatedly measuring outcome expectancies across an acute treatment (from baseline to mid-treatment to post-treatment), and as a predictor of outcome in a randomized clinical trial. Treatment outcome expectancies were assessed at baseline (prior to randomization and in-depth presentation of treatment rationales), at treatment mid-point (Week 3), and at treatment endpoint. The study design compared two distinct treatment modalities in terms of theoretical basis, purported target of treatment engagement, and the practical requirements of treatment delivery for the patient and provider. Whereas CBT-SAD is based on cognitive theory and targets modifying maladaptive behaviors and cognitions through a structured psychotherapy intervention (Rohan, 2008), LT is based on chronobiological theory and aims to correct misaligned circadian rhythms via timed bright artificial light to the retina (Wirz-Justice, Benedetti, & Terman, 2013). The parent randomized clinical trial found that CBT-SAD and LT were comparably effective in treating SAD symptoms following acute treatment, with very similar remission rates (47.6% CBT-SAD vs. 47.2% LT) and comparable pre- to post-treatment improvements in depression severity across a 6-week trial (Rohan, Mahon, et al., 2015). Recurrence rates were comparable between the treatments at the first winter follow-up (28.9% CBT-SAD vs. 24.9% LT), but differed at the second winter follow-up, with fewer recurrences in CBT-SAD than in LT (27.3% CBT-SAD vs. 45.6% LT; Rohan, Meyerhoff, et al., 2015).
Given that CBT-SAD and LT are theoretically distinct but comparably effective treatments, the design of the parent trial lent itself to exploring the potentially time-varying nature of treatment expectancies during treatment and how these expectancies may be related to outcome over time. The comparable efficacy of CBT-SAD and LT for SAD allows us to evaluate whether treatment expectations for theoretically distinct treatments show different patterns of change and whether treatment expectations affect outcome. To our knowledge, this is one of the first studies to repeatedly measure treatment expectancies across acute treatment, an approach that enables capturing the time-varying nature of treatment expectations.
The present study had three (3) aims. Aim 1 was to examine whether expectations for the treatment received changed over the course of treatment (pre-, mid-, and post-treatment). Aim 2 was to examine whether treatment expectations and treatment modality predicted depression severity over the course of treatment (pre-, mid-, and post-treatment). Aim 3 was to examine whether changes in depression severity were driven by changes in treatment expectations or whether changes in treatment expectations were driven by changes in depression severity over the course treatment (pre-, mid-, and post-treatment).
Method
Participants
Data for this project were collected as part of a randomized clinical trial testing the relative efficacy of LT and CBT-SAD for SAD (Rohan et al., 2013). Participants provided informed consent prior to enrolling in the study. The study was conducted at the University of Vermont and was approved by the institutional review board. Participants, aged 18 and older, were recruited for this study from Burlington, VT, and surrounding areas. Participants were included in the study if they: met DSM-IV-TR criteria for Major Depression, Recurrent, with Seasonal Pattern assessed using the Structured Clinical Interview for DSM-IV Axis I Disorders–Clinician Version (First, Spitzer, Gibbon, & Williams, 1995) and scored at least 20 (and at least 5 on the atypical scale) on the Structured Interview Guide for the Hamilton Rating Scale for Depression—Seasonal Affective Disorder Version (SIGH-SAD; Williams, Link, Rosenthal, Amira, & Terman, 1992). Screened individuals were excluded if they: were receiving or planning on receiving either LT or psychotherapy for depression during the winter of enrollment; had history of LT or CBT for SAD; had a comorbid Axis I disorder for which immediate treatment was indicated; or had serious suicidal ideation, hypothyroidism (assessed via thyroid panel at medical workup), or travel plans through March.
The sample was comprised of 177 community adults (88 randomized to CBT-SAD and 89 randomized to LT). The majority of participants were female (83.6%) and non-Hispanic white (92.1%). The mean age was 45.6 years. For the CONSORT flow diagram and detailed demographic information and baseline characteristics, see Rohan, Mahon, et al., 2015. Eligible participants were randomized to CBT-SAD or LT using random permuted blocks of four and six with conditions stratified based on sex, major comorbid Axis I diagnosis at baseline (present or absent), and current antidepressant medication (taking medication or not; Rohan et al., 2013).
Treatments
Six-week treatment with either CBT-SAD or LT began following randomization. CBT-SAD was conducted in a group therapy format following a manual (Rohan, 2008). The CBT-SAD protocol uses a group-format to enhance its cost-effectiveness and has demonstrated efficacy in prior trials (Rohan et al., 2007; Rohan, Roecklein, Lacy, & Vacek, 2009; Rohan, Mahon, et al., 2015; Rohan, Meyerhoff, et al., 2015). Groups were led by, either the P.I. or one of two Ph.D.-level community therapists unaffiliated with the Rohan lab. The CBT-SAD protocol was designed to be administered during the winter months, before spontaneous springtime remission of SAD symptoms occurs. As such, CBT-SAD includes 12 90-minute sessions at a frequency of two sessions per week over 6 weeks. This contrasts with traditional CBT for depression, which is delivered in twice-weekly 50-minute sessions over the first two weeks followed by weekly 50-minute sessions over the remaining 14 weeks for a total of 20 sessions in 16 weeks (Beck, Rush, Shaw, & Emery, 1979). CBT-SAD uses traditional CBT components such as behavioral activation, cognitive restructuring, and relapse-prevention planning within the context of coping with the winter season and reduced availability of natural light. Some cognitive restructuring focuses specifically on negative thoughts about the winter season, reduced light availability, and weather conditions. Behavioral activation surrounds identifying pleasant activities that can be done in the winter and increasing their frequency. The 6-week LT protocol used standard light therapy light boxes (SunRay by SunBox Company©, Gaithersburg, MD), which deliver 10,000-lux of cool-white fluorescent light filtered through an ultraviolet shield. Participants received a scripted demonstration of light box assembly, positioning, and rationale for LT as well as instructions for use and potential side effects. Participants were instructed to administer a 30-minute daily dose of light promptly upon waking in the morning in week 1. LT dosage adjustments were made weekly using the following treatment algorithm in order to maximize response, address inappropriate phase shifts, and minimize side effects. If participants did not have a reduction in SIGH-SAD scores of 30% or greater by the end of treatment week 1, and a reduction of 50% or greater by the end of week 2, and did not meet remission criteria by the end of week 3, daily dose was increased by 15 minutes each week with an upper limit of 2 hours of daily light therapy. In the event of significant side effects, treatment was titrated down incrementally with a minimum of 30 minutes per day. Severe side effects prompted single day hiatuses from LT, with a reduction of dose by 50% when treatment resumed. Insomnia also prompted titration of LT. An outside LT expert and chronobiological psychiatrist made all recommended adjustments.
Treatment integrity was monitored by examining therapist behavior at each session using an adaptation of the National Institute of Mental Health’s Collaborative Study Psychotherapy Rating (reviewed in Rohan et al., 2013). 25% of CBT-SAD sessions (48 sessions) were randomly selected across CBT-SAD groups, therapists, and session numbers. These sessions were rated by two trained clinical graduate students, blind to condition and session (inter-rater reliability intraclass correlation coefficient = 0.76). Mann-Whitney tests revealed that CBT-SAD differed significantly from LT on all cognitive-behavioral and clinical management subscales aside from the relapse prevention subscale supporting that conclusion that CBT-SAD and LT consist of theoretically distinct treatments that were administered consistently across groups and time. Participants randomized to CBT-SAD attended most sessions (M=9.1, SD=3.5). Of those who withdrew, 7 participants attended 0 sessions and 6 attended between 2 and 7 sessions. Light therapy adherence was monitored using LT diaries (Rohan, Mahon, et al., 2015). For a more detailed account of the treatment protocols and acute outcomes, see previously published protocol and outcomes (Rohan et al., 2013; Rohan, Mahon, et al., 2015).
Measures
The following measures were administered at pre-, mid-, and post-treatment. The pretreatment assessment took place after fully meeting all inclusion criteria and prior to randomization. Brief treatment rationales were presented in the informed consent document and reviewed at the initial diagnostic interview. The mid-treatment assessment occurred after 3 weeks of treatment. Therefore, mid-treatment encompassed exposure to the fully articulated treatment rationale, presented in the first two sessions of CBT-SAD and in the LT instructional session immediately prior to initiating LT. The post-treatment assessment followed completion of the 6-week treatment phase.
Beck Depression Inventory-Second Edition (BDI-II)
The BDI-II (Beck et al., 1996) is a 21-item self-report measure of depressive symptom severity. The BDI-II has shown good test-retest reliability and convergent validity (Beck et al., 1996). Cronbach’s alpha for the BDI-II were high at each timepoint (0.89 at pre-treatment, 0.87 at mid-treatment, and 0.88 at post-treatment).
Credibility/Expectancy Questionnaire (CEQ)
The original version of the CEQ (Borkovec & Nau, 1972) is a 5-item self-report measure. Items are rated on a Likert scale ranging from 1 (low/poor expectation of treatment) to 10 (high/favorable expectation of treatment). Items are framed without reference to a specific time-point. To fit the current study, we administered an adapted form of the CEQ (Borkovec & Nau, 1972). Items were worded as follows: (1) “How logical does each treatment option seem to you?” (2) “How confident are you that each treatment would be successful in eliminating your SAD?” (3) “How confident would you be in recommending each treatment to a friend who has SAD?” (4) “How willing would you be to undergo each treatment?” (5) (“How successful do you feel each treatment would be in decreasing a different problem, for example, non-seasonal depression?” For each of the five original items, participants were asked to rate CBT-SAD and LT, separately, at pre-, mid-, and post-treatment. The scores for four of the five items were summed to create a composite expectation score. These composite scores constitute the treatment expectations scores used in the analyses. The fifth item was not included in the composite score because doing so might have artificially decreased expectations for LT, given that LT is not a well-established treatment for non-seasonal depression. Cronbach’s alphas were high at each timepoint (CEQ-CBT: 0.85 at pretreatment, 0.91 at mid-treatment=.91, and 0.93 at post-treatment; CEQ-LT: 0.73 at pre-treatment, 0.85 at mid-treatment, and 0.89 at post-treatment). To further characterize treatment expectations at baseline, participants were asked to rank order CBT-SAD and LT in order of how effective they thought the treatments would be and in order of preference along with the pre-treatment CEQ.
Data Analytic Plan
To address the question of whether expectations for the treatment received change over the course of treatment, we first examined the Ordinary Least Squares (OLS) residual values of the data following a linear regression in which the dependent variable was treatment-congruent expectation scores and the independent variable was time. The residual values were then plotted. This process enabled us to evaluate whether there was an observable time trend to the data, determining the type of mixed model that would be used in subsequent analyses. No clear time trend to the linear residual values was apparent, as a result analyses proceeded with a series of linear mixed models (LMM) with full maximum likelihood (ML) estimation. The use of LMM allows for the inclusion of individuals with only partial data in analyses. To determine the model that fit the data best with regard to covariance structure, mean structure, and random effects structure; we built models from a basic unconditional model structure that included linear change over time, a random effect of individual differences (intercept), and a random effect of linear change over time (slope). The best fitting model, determined using likelihood ratio test (LRT) comparisons, is shown below:
Note: Treatment Expectation = Raw, uncentered, treatment expectancy composite score for treatment received, TxGrp= treatment received.
To compare models, we used LRT for ML models with static random effects and for models that used restricted estimated maximum likelihood (REML), we used AIC weighted comparisons. All linear mixed models (LMM) were estimated using R version 3.1.1 packages that included lme4, nlme, and ggplot2. Marginal R2 (the proportion of variance explained by the fixed effects alone) and conditional R2 (the proportion of variance explained by the fixed and random effects) are global LMM effect sizes (Nakagawa & Schielzeth, 2013; Johnson, 2014) that were calculated using the sem.model.fit functions in the peicewiseSEM package (Lefcheck, 2015). The best fitting LMM model had a level 1 (within-subject) fixed effect of time (pre-treatment, mid-treatment, and post-treatment), a level 2 fixed effect of treatment group (CBT-SAD or LT), and an interaction of time and treatment group. Random effects included an intercept and slope. A heterogeneous autoregressive standard covariance structure fit the data best and was used in the final model for Aim 1.
To examine whether treatment expectations and treatment modality predicted depression severity over the course of the acute treatment phase, again, we examined OLS residuals values of the data following a linear regression. In this case, the dependent variable was BDI-II score and the independent variable was time. The residual values were plotted. There was no observable time trend to the linear residual values. Based on this result, we conducted a series of linear mixed models with full ML estimation examining depression severity (on the BDI-II and SIGH-SAD in separate models) as a single repeated measure variable. The best fitting model, determined using likelihood ration test (LRT) comparisons, is shown below:
Note: Depression = BDI-II score, TxGrp= treatment, Treatment Expectation = Grand-mean centered treatment expectancy composite score for treatment received.
Our final models included a level 1 fixed effect of time (pre-treatment, mid-treatment, and post-treatment), a level 2 fixed effect of treatment group (CBT-SAD or LT), a dynamic continuous covariate of grand-mean centered treatment expectation score, and a two-way interactions of time and treatment group. Random effects included an intercept and slope. For these data, a heterogeneous autoregressive covariance structure fit best and was used for final analyses.
To examine whether changes in depression severity were driven by treatment expectations or whether changes in treatment expectations were driven by depression severity changes over the course of the acute treatment phase, we employed cross-lagged panel structural equation modeling path analyses to identify the extent to which expectation scores at pre- or mid-treatment predict depression severity at mid- or post-treatment respectively. Additionally, we explored the reverse pattern, examining the extent to which depression severity at pre- or mid-treatment predicted expectation scores at mid- or post-treatment. All models were built and tested using IBM SPSS AMOS v. 22. All models used full maximum likelihood estimation. Final models were chosen based on evaluation of fit statistics (χ2: p > 0.05 excellent), Comparative Fit Index (CFI; > 0.90 acceptable, > 0.95 excellent), Root Mean Square Error of Approximation (RMSEA; < 0.08 acceptable, < 0.05 excellent).
Missing Data
Missing data were minimal. 148 of 177 (83.6%) participants provided complete (all measures at all 3 time-points) BDI-II, and CEQ data (69/88 in the CBT-SAD treatment group and 79/89 in the LT group). See Table 1 for specific cell sizes. Missingness of depression and expectation scores did not appear to be related to the predicted value of those scores, thus data was assumed to be missing at random (MAR). In order to accommodate missing data, full maximum likelihood (ML) estimation was used for analyses. 14 individuals withdrew from treatment, 13 from CBT-SAD and 1 from LT. In accordance with the intent-to-treat principle, participants who withdrew from treatment were encouraged to provide data. Only 4 individuals (all in CBT-SAD) did not provide data at post treatment. Those who withdrew from treatment had lower pre-treatment expectation scores for their treatment (n=12, M=5.69, SD=2.34) than those who remained in treatment (n=162, M=7.31, SD=1.81).
Table 1.
Sample Means on Outcome Measures (N = 177)
| Measure | Pre-treatment (M, SD) | Mid-treatment (M, SD) | Post-treatment (M, SD) | |
|---|---|---|---|---|
| CBT-SAD | CEQ-CBT |
n=86 6.28 (1.88) |
n=76 8.14 (1.53) |
n=83 8.25 (2.05) |
| CEQ-LT |
n=86 7.99 (1.31) |
n=76 7.22 (1.77) |
n=83 6.88 (2.02) |
|
| BDI-II |
n=88 22.67 (9.33) |
n=77 13.43 (6.69) |
n=84 8.24 (6.68) |
|
| LT | CEQ-CBT |
n=88 6.42 (1.94) |
n=85 6.31 (2.32) |
n=88 6.38 (2.28) |
| CEQ-LT |
n=88 8.08 (1.42) |
n=85 8.42 (1.30) |
n=89 8.61 (1.33) |
|
| BDI-II |
n=87 23.44 (8.42) |
n=88 12.13 (7.25) |
n=79 7.14 (6.01) |
Note. CBT-SAD = cognitive-behavioral therapy for seasonal affective disorder, LT = light therapy, CEQ-CBT = expectancy score for cognitive-behavioral therapy, CEQ-LT = expectancy score for light therapy, BDI-II = Beck Depression Inventory Second Ed.
Results
Table 1 displays sample characteristics and descriptive information for the CEQ and BDI-II by treatment group. At baseline, the majority of participants ranked LT as first in efficacy (76% vs. 15.8% CBT-SAD first and 5.1% tied) and as first choice in preference (81.9% vs. 12.4% CBT-SAD first and 2.3% tied), indicating positive bias towards LT.
Aim 1: Do Treatment Expectations Change Over Time?
Treatment expectations, changed over time in both CBT-SAD and LT. We tested each of the random effects components of the model examining expectations for the treatment received. Each of the variance components for the model was necessary and significantly different from zero. There was significant variance in the intercepts (Var(b0i)=1.63) and slopes across participants (Var(b1i)= 0.37). Additionally, we found that the slopes and intercepts covaried (Cov(b0ib1i)= −0.21). The model (R2marginal= 0.1725; R2conditional=0.7365) revealed significant main effects of time, treatment group, as well as a significant interaction of time and treatment group (Table 2).
Table 2.
AIM 1LMM Model Coefficients
| Outcome: Treatment Expectation Scores (CEQ) | ||||
|---|---|---|---|---|
| b | S.E. | t-ratio | P | |
| Intercept | 6.60 | 0.18 | 36.13 | <0.001 |
| Time | 0.94 | 0.10 | 9.11 | <0.001 |
| Treatment Group | 1.51 | 0.26 | 5.86 | <0.001 |
| Time*Treatment Group | −0.68 | 0.14 | −4.67 | <0.001 |
b=unstandardized beta estimate, S.E.=Standard Error of b, t-ratio = parameter effect size, Time coded as: Pre-treatment=0, mid-treatment=1, post-treatment=2, Treatment group coded as: CBT-SAD=0, LT=1
This model suggests that treatment expectations became more favorable over time, but the magnitude of change differed depending on treatment received. Individuals in CBT-SAD generally reported a substantial increase in their expectations of CBT-SAD as treatment progressed over time (simple slope=1.01, p<.001). However, individuals randomized to LT had a more modest increase in their expectations of LT over time (simple slope=−0.27, p<.05; Figure 1).
Figure 1. Predicted treatment expectation scores over time.
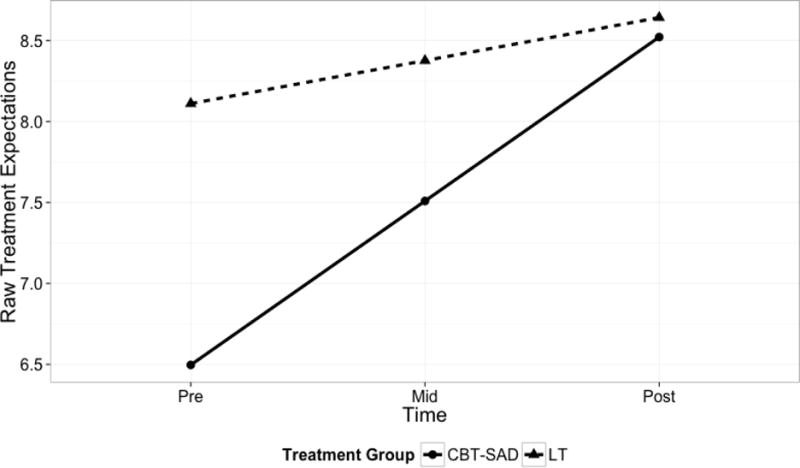
Note: Time coded as: Pre-treatment=0, mid-treatment=1, post-treatment=2, Treatment group coded as: CBT-SAD=0, LT=1
Aim 2: Do Treatment Expectations Predict Depression Outcome?
Higher treatment expectations predicted lower depression severity, and lower treatment expectations predicted relatively higher depression severity in both CBT-SAD and LT. Our analyses indicate that higher treatment expectations predict lower depression severity, and that lower treatment expectations predict relatively higher depression severity. Random effects components for the model examining depression severity were tested. Each component of variance was found to be necessary and differed significantly from zero. Random effects included variance in the intercepts (Var(b0i)=52.03) and slopes across participants (Var(b1i)=7.02). We also found that the slopes and intercepts covaried (Cov(b0ib1i)= −16.23.). The model (R2marginal=0.4379; R2conditional=0.7549) revealed significant main effects of time, grand-mean centered treatment expectations scores, and a marginally significant interaction of time and treatment group (Table 3). The main effect of time suggests that depression severity decreased over the course of treatment, regardless of treatment group. The main effect of grand-mean centered treatment expectations indicates that, collapsing across timepoints, participants with higher expectations of their treatment had better outcomes, despite no difference in overall outcomes between treatment groups (Figure 3). The interaction of time and treatment group was probed using a simple slope analysis which revealed that the interaction of time and treatment group significantly improved the overall fit of the linear mixed model, probably because BDI-II scores at each timepoint differed from the other two timepoints, as reported in the primary analysis (Rohan et al., 2015). However, a simple slopes analysis revealed that no significant differences in depression severity between CBT-SAD and LT at any of the three timepoints. This suggests that our results are in accord with the main effect of time reported in the acute efficacy results for the trial (Rohan et al., 2015), indicating that depression severity improved as treatment progressed and no interaction of treatment group and time.
Table 3.
AIM 2 LMM Model Coefficients
| Outcome: Depression Severity (BDI-II) | ||||
|---|---|---|---|---|
| b | S.E. | t-ratio | P | |
| Intercept | 20.67 | 0.96 | 21.53 | <0.001 |
| Time | −6.14 | 0.52 | −11.78 | <0.001 |
| Treatment Group | 1.82 | 1.33 | 1.37 | >0.05 |
| C.Treatment Expectations | −0.94 | .20 | −4.64 | <0.001 |
| Time*Treatment Group | −1.38 | 0.70 | −1.96 | >0.05 |
b=unstandardized beta estimate, S.E.=Standard Error of b, t-ratio = parameter effect size, C.Treatment Expectations=Grand-mean centered treatment expectation scores (CEQ), Time coded as: Pre-treatment=0, mid-treatment=1, post-treatment=2, Treatment group coded as: CBT-SAD=0, LT=1
Figure 3. Saturated Model Examining Relationships between Treatment Expectations and Depression Scores.
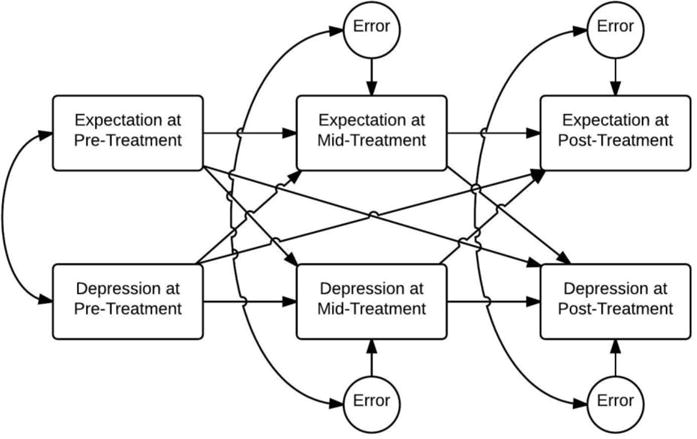
Note: Single-sided arrows= regression pathways. Double-sided arrows=Covariance pathways. Expectations=Treatment-congruent expectations, Depression = BDI-II score. Separate analyses completed for participants who received CBT-SAD or LT.
Aim 3: Are Treatment Expectations Mechanistic of Depression Change or is Depression Change Mechanistic of Treatment Expectancy Change?
Treatment expectations were a mechanism of change under certain circumstances, namely, in CBT-SAD (and not LT) and at mid-treatment, following several sessions of CBT-SAD. Preliminary analyses included an examination of the correlations between treatment expectations and depression severity at each time point (Table 4). Based on the presence of a significant correlation between treatment expectation score and depression severity, model comparisons were conducted with saturated models for each treatment group. The structure of the saturated model is displayed in Figure 3. Only models that had significant time-lagged correlations were explored.
Table 4.
Correlations between Treatment Expectation Scores and Depression Severity
| BDI-II | ||||
|---|---|---|---|---|
|
| ||||
| Treatment Group | Pre-Tx (n) | Mid-Tx (n) | Post-Tx (n) | |
| CBT-SAD (CEQ-CBT) | Mid-Tx (n) | 0.065 (76) | −0.092 (76) | −0.224 (75) |
| Post-Tx (n) | −0.103 (83) | −0.144 (76) | −0.326 (83) | |
|
| ||||
| LT (CEQ-LT) | Mid-Tx (n) | −0.128 (85) | −0.216 (85) | −0.048 (84) |
| Post-Tx (n) | −0.010 (89) | −0.178 (87) | −0.263 (88) | |
Note: All significant correlations are shown. Bolded correlations represent significant correlations (p<.05), Tx= Treatment.
Model pathways that were non-significant were pruned in order to yield the most parsimonious model with the best-fit statistics. The model examining the relationship between treatment expectations in CBT-SAD and depression severity yielded excellent fit statistics (Figure 4). In CBT-SAD, there was a small but significant effect of change in CBT-SAD expectations at mid-treatment on BDI-II scores at post-treatment (β=−.178, p<.05). There was significant correlation (r(86) = −.264) between the residual errors of treatment expectations and depression severity at mid-treatment, but not at post-treatment. This model suggests that pre-treatment expectation scores and depression severity are uncorrelated until mid-treatment, when they become related. The association between these two variables is then captured by a significant relationship of treatment expectations at mid-treatment driving changes in depression severity at post-treatment.
Figure 4. Final Model Examining Relationships between CBT-SAD Expectations and BDI-II.
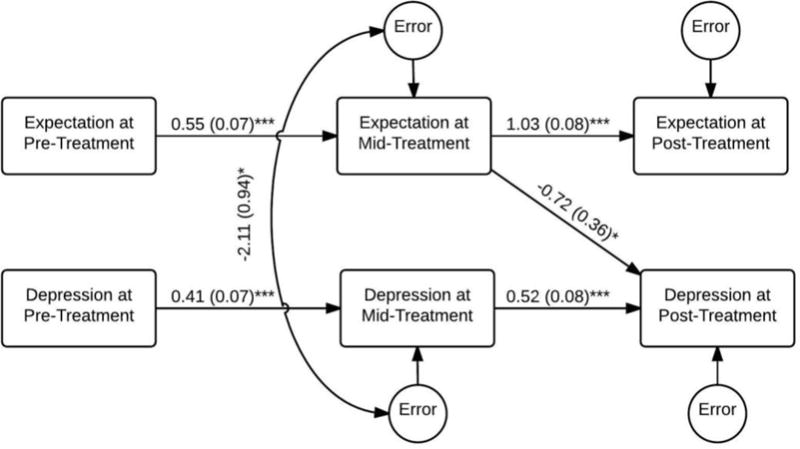
Note: ***=p<.0001, **=p<.01, *=p<0.05. Single-sided arrows=Unstandardized regression coefficients (SE). Double-sided arrows=Covariance coefficients (SE). The final model demonstrated excellent fit (χ2 (9, N = 88) = 7.277, p > 0.05, CFI = 1.00, RMSEA = 0.000, 90% CI 0.000, 0.103).
The model examining the relationship between expectations of LT and depression severity in LT yielded good fit statistics (Figure 5), but no significant pathways between time-lagged treatment expectations and depression severity. However, there was significant correlation (r(87) = −.347) between the residual errors of treatment expectations and depression severity at post-treatment. This model suggests that LT expectations and depression severity are uncorrelated with one another at pre-treatment in LT and that this pattern continues until post-treatment when a significant covariance emerges, whereby higher treatment expectations are correlated with lower depression severity and lower treatment expectations are correlated with higher levels of depression severity. It is important to note that causation cannot be assumed in this case.
Figure 5. Final Model Examining Relationships between LT Expectations and BDI-II.
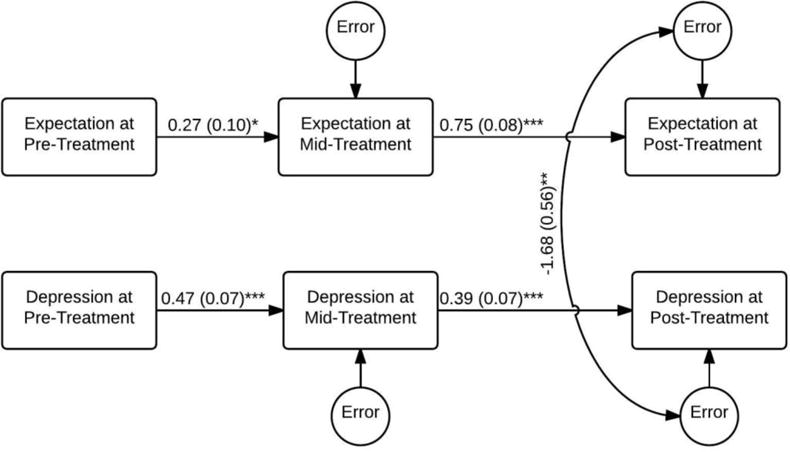
Note: ***=p<.0001, **=p<.01, *=p<0.05. Single-sided arrows=Unstandardized regression coefficients (SE). Double-sided arrows=Covariance coefficients (SE). The final model demonstrated good fit (χ2 (10, N = 89) = 10.371, p > 0.05, CFI = 0.997, RMSEA = 0.021, 90% CI 0.000, 0.119).
Discussion
In the context of a randomized clinical trial comparing CBT-SAD and LT for winter depression, the purpose of this study was to (1) examine whether expectations for the treatment received changed over the course of treatment, (2) examine whether treatment expectations and treatment modality predicted depression severity over the course of treatment, and (3) examine whether changes in depression severity were driven by changes in treatment expectations or whether changes in treatment expectations were driven by changes in depression severity over the course of treatment. In each case, the course of treatment refers to pre- to mid- to post-treatment over a 6-week trial.
Consistent with Newman and Fisher’s (2010) finding that expectations changed over the course of CBT for GAD, SAD participants’ expectations for the treatment received increased across acute treatment with either CBT-SAD or LT. Moreover, treatment expectations increased more rapidly in CBT-SAD than they did in LT. This study extends the existing literature by providing additional evidence that expectations are not static across treatment, but dynamic, supporting the need for monitoring treatment expectations beyond pre-treatment and instead measuring treatment expectations repeatedly across the course of treatment in a similar manner to that of Newman and Fisher (2010).
Additionally, our findings suggest that regardless of treatment condition, higher treatment expectancies corresponded to better outcome (less depression) across all three timepoints included: pre-, mid-, and post-treatment. CBT-SAD and LT did not differ on depression severity at week throughout acute treatment in the primary efficacy analyses (Rohan et al., 2015). Despite the strong treatment effect, treatment expectations explain some of the additional variance in depression severity. This highlights the importance of monitoring treatment expectations in different treatment modalities as expectations have broad implications for outcome.
In an exploration of treatment expectations as a predictor of depression severity within each treatment condition, we found that within the CBT-SAD treatment group, there was a significant effect of expectations of CBT-SAD at mid-treatment on depression severity at post-treatment. We found no such effect in LT, only a correlation between depression severity and expectations of LT at post-treatment. One possible explanation for this finding is that the treatment rationale for CBT-SAD is presented in the first two sessions and is therefore completed by mid-treatment leading to a measurable effect of increase in patient “buy-in” on subsequent depression only after mid-treatment. Thus, the time needed to completely establish a treatment rationale may be one reason a significant relationship exists only from mid-treatment expectations to post-treatment depression severity. This is, in part, the same logic underlying Newman and Fisher’s (2010) choice to focus on weeks 4–7 of treatment, a treatment window far enough removed from session 1 such that the treatment rationale was already established and baseline measurements would not dampen the predictive power of treatment expectations. The lack of a predictive relationship between time-lagged LT expectations and depression severity in LT may be due, in part, to the restricted range of the CEQ in patients receiving LT. LT expectations began relatively high and remained high through treatment without a great deal of variability (Table 1). More sensitive measurement instruments than the CEQ should be explored. The present study also extends the existing literature by highlighting the role of treatment expectations for CBT-SAD to drive therapeutic change. These findings should be replicated in SAD samples and examined for generalizability to non-seasonal depression as they underscore the importance of further research examining treatment expectations in mediating CBT’s effects in depression and other types of psychopathology.
Both physiological and cognitive vulnerabilities play important roles in the SAD onset and maintenance (Young, Reardon, & Azam, 2008). Thus, treatments targeting disorder-commensurate vulnerabilities may result in more positive expectations for that treatment leading to better treatment outcomes. Our data indicates that SAD patients overwhelmingly display a preference for LT at pre-treatment (76.3%) and that expectations for LT begin high and remain high if patients are receiving LT. Therefore, clinicians do not typically need to convince SAD patients of the treatment rationale for LT. However, this is not the case for patients receiving CBT-SAD. Overall, SAD patients tend to possess high perceived external locus of control and low levels of personal agency in controlling their symptoms (Murray, Hay, & Armstrong, 1995).
As a treatment that targets a cognitive vulnerability and invokes a sense of personal agency, CBT-SAD results in a better outcome at post-treatment for those who can be convinced that CBT-SAD is a viable SAD treatment by mid-treatment. This is especially important given the overwhelming preference for LT in our sample at baseline. Clinicians treating SAD patients with CBT-SAD should actively attend to the degree of patient “buy-in” throughout treatment, however, this may be especially important early in treatment. Clinicians delivering CBT-SAD may wish to assess the degree to which patients attribute a role for cognitions and behavior in maintaining their SAD symptoms and feel a sense of personal agency to change them after the treatment rationale is articulated. At that point, if a patient maintains low expectations for CBT-SAD despite the clinician’s best attempt to sell the CBT-SAD rationale, the patient may be a candidate for an alternate treatment such as LT.
This study has a number of important limitations. First, these results are secondary analyses from a larger parent randomized clinical trial of CBT-SAD and LT for winter SAD, the original sample size was chosen in order to test the primary hypothesis that CBT-SAD would be superior to LT in depression recurrences following treatment of the index episode (Rohan, Mahon, et al., 2015; Rohan, Meyerhoff, et al., 2015). This study focuses on a secondary analysis of treatment expectations data that is exploratory in nature and, therefore, may be underpowered. Second, it is unknown whether these results generalize to non-seasonal depression. CBT for non-seasonal depression includes a longer treatment interval (20 sessions over 16 weeks) compared to CBT-SAD (12 90-minute twice weekly sessions), which is designed to be administered during the winter months, before spontaneous springtime remission occurs. Our results may also be restricted to SAD; specifically, to comparisons of CBT-SAD and LT. CBT-SAD and LT are theoretically distinct treatment modalities. CBT-SAD involves significant human contact (12 90-minute group sessions twice weekly), whereas LT involves less direct human interaction (LT is self-administered in 30 minute daily doses upon waking with adjustments as needed). Another primary limitation of the current study includes a lack of diversity in participant demographics. Future studies may also wish to include more sensitive measures of treatment expectations. We used the original version of the CEQ, but there are several updates and recent developments in the field with respect to measuring treatment expectations (Devilly & Borkovec, 2000; Eddington, Dozois, & Backs-Dermott, 2013). An additional limitation of the current study is that our first assessment of expectations occurred at at pre-treatment, before randomization. At that point, subjects had a brief exposure to the two treatment rationales in the consent form, which was reviewed by the staff member who obtained consent. After randomization, LT subjects attended an instructional session where they received a scripted treatment rationale and learned how to assemble and use a light box. The first two sessions of CBT-SAD present the treatment rationale. Subsequently, mid-treatment might capture an increase in expectations for either CBT-SAD or LT after hearing the full treatment rationale. Finally, there are other factors that may account for the relationship between treatment expectations and depression outcome such as treatment participation and compliance. Future research should focus on examining the relationship between treatment adherence (i.e., homework compliance and session attendance in CBT-SAD; LT daily prescription adherence in LT) and treatment expectations in predicting treatment outcomes. Future work should also examine treatment expectations as they relate to more distal outcomes such as recurrence and symptom severity at long-term follow-up visits. The parent trial found that CBT-SAD was associated with fewer depression recurrences and less severe symptoms than LT over the next two winters (Rohan, Meyerhoff, et al., 2015). It is possible that CBT-SAD participants become more favorably disposed towards CBT-SAD in future winters given these long-term benefits and that LT participants become less favorably disposed towards LT given the potential burden of a daily treatment each fall/winter season indefinitely.
Figure 2. Effect of high and low treatment expectations on depression by treatment group.
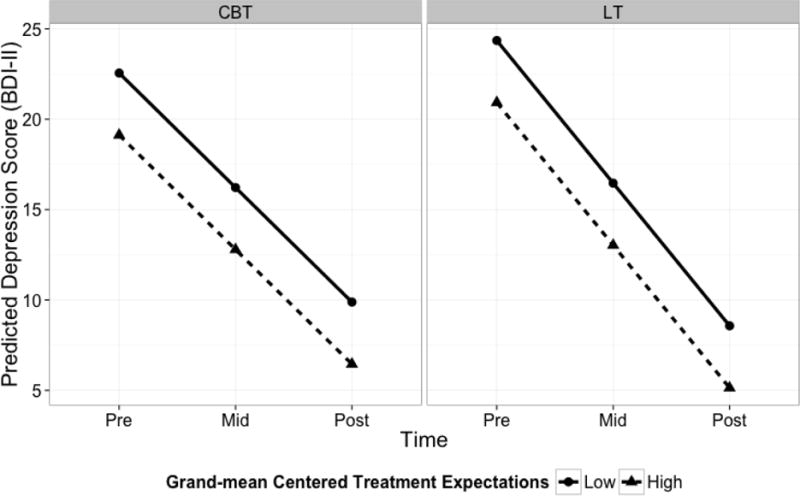
Note: Grand-mean centered treatment expectation = treatment congruent composite CEQ score (SD = 1.78). High and low CEQ scores were tested at +/−1 SD above and below the mean.
Acknowledgments
This work was supported by grant R01MH078982 from the National Institute of Mental Health to Kelly J. Rohan. The authors would like to thank Matthew Price and Rex Forehand for their comments on an earlier version of this manuscript.
Footnotes
Kelly Rohan receives royalties from Oxford University Press for SAD treatment manual.
References
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression Cognitive Therapy of Depression 1979 [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II Psychological Corporation. San Antonio, TX: Psychological Corporation; 1996. pp. 1–82. [Google Scholar]
- Borkovec T, Nau S. Credibility of analogue therapy rationales. Journal of Behavior Therapy and Experimental Psychiatry 1972 [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd. Hillsdale, N.J: L. Erlbaum Associates; 1988. [Google Scholar]
- Constantino MJ, Arnkoff DB, Glass CR, Ametrano RM, Smith JZ. Expectations. Journal of Clinical Psychology. 2011;67:184–192. doi: 10.1002/jclp.20754. http://doi.org/10.1002/jclp.20754. [DOI] [PubMed] [Google Scholar]
- Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. Journal of Behavior Therapy and Experimental Psychiatry. 2000;31(2):73–86. doi: 10.1016/s0005-7916(00)00012-4. [DOI] [PubMed] [Google Scholar]
- Eddington KM, Dozois DJA, Backs-Dermott BJ. Evaluation of the Internal Consistency, Factor Structure, and Validity of the Depression Change Expectancy Scale. Assessment. 2013 doi: 10.1177/1073191113517929. 1073191113517929. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders (Clinician Version) for DSMIV. New York: New York, New York State Psychiatric Institute Biometrics Department; 1995. [Google Scholar]
- Holt CS, Heimberg RG. The Reaction to Treatment Questionnaire: Measuring treatment credibility and outcome expectancies. Behavior Therapist. 1990;13:213–214. [Google Scholar]
- Ilardi SS, Craighead Edward W. The role of nonspecific factors in cognitive-behavior therapy for depression. Clinical Psychology: Science and Practice. 1994;1:138–155. http://doi.org/10.1111/j.1468-2850.1994.tb00016.x. [Google Scholar]
- Johnson PCD. Extension of Nakagawa & Schielzeth’s R2GLMM to random slopes models. Methods in Ecology and Evolution. 2014;5(9):944–946. doi: 10.1111/2041-210X.12225. http://doi.org/10.1111/2041-210X.12225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lefcheck JS. piecewiseSEM: Piecewise structural equation modeling in R for ecology, evolution, and systematics. Methods in Ecology and Evolution. 2015:n/a–n/a. http://doi.org/10.1111/2041-210X.12512.
- Murray GW, Hay DA, Armstrong SM. Personality factors in seasonal affective disorder: is seasonality an aspect of neuroticism? Personality and Individual Differences. 1995;19(5):613–617. [Google Scholar]
- Nakagawa S, Schielzeth H. A general and simple method for obtaining R2 from generalized linear mixed-effects models. Methods in Ecology and Evolution. 2013;4(2):133–142. http://doi.org/10.1111/j.2041-210x.2012.00261.x. [Google Scholar]
- Newman MG, Fisher AJ. Expectancy/credibility change as a mediator of cognitive behavioral therapy for generalized anxiety disorder: Mechanism of action or proxy for symptom change? International Journal of Cognitive Therapy. 2010;3:245. doi: 10.1521/ijct.2010.3.3.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price M, Anderson P, Henrich CC, Rothbaum BO. Greater expectations: Using hierarchical linear modeling to examine expectancy for treatment outcome as a predictor of treatment response. Behavior Therapy. 2008;39(4):398–405. doi: 10.1016/j.beth.2007.12.002. http://doi.org/10.1016/j.beth.2007.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price M, Anderson PL. Outcome expectancy as a predictor of treatment response in cognitive behavioral therapy for public speaking fears within social anxiety disorder. Psychotherapy (Chicago, Ill.) 2012;49:173–9. doi: 10.1037/a0024734. http://doi.org/10.1037/a0024734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohan KJ. Coping with the seasons: A cognitive-behavioral approach to seasonal affective disorder: Therapist guide Coping with the seasons: A cognitive-behavioral approach to seasonal affective disorder: Therapist guide. New York, NY: Oxford University Press; 2008. [Google Scholar]
- Rohan KJ, Evans M, Mahon JN, Sitnikov L, Ho SY, Nillni YI, Vacek PM. Cognitive-behavioral therapy vs. light therapy for preventing winter depression recurrence: Study protocol for a randomized controlled trial. Trials. 2013;14:82. doi: 10.1186/1745-6215-14-82. http://doi.org/10.1186/1745-6215-14-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohan KJ, Mahon JN, Evans M, Ho SY, Meyerhoff J, Postolache TT, Vacek PM. Randomized Trial of Cognitive-Behavioral Therapy Versus Light Therapy for Seasonal Affective Disorder: Acute Outcomes. American Journal of Psychiatry. 2015 doi: 10.1176/appi.ajp.2015.14101293. appi.ajp.2015.14101293. http://doi.org/10.1176/appi.ajp.2015.14101293. [DOI] [PMC free article] [PubMed]
- Rohan KJ, Meyerhoff J, Ho SY, Evans M, Postolache TT, Vacek PM. Outcomes One and Two Winters Following Cognitive-Behavioral Therapy or Light Therapy for Seasonal Affective Disorder. American Journal of Psychiatry. 2015 doi: 10.1176/appi.ajp.2015.15060773. appi.ajp.2015.1. http://doi.org/10.1176/appi.ajp.2015.15060773. [DOI] [PMC free article] [PubMed]
- Rohan KJ, Roecklein KA, Tierney Lindsey K, Johnson LG, Lippy RD, Lacy TJ, Barton FB. A randomized controlled trial of cognitive-behavioral therapy, light therapy, and their combination for seasonal affective disorder. Journal of Consulting and Clinical Psychology. 2007;75(3):489–500. doi: 10.1037/0022-006X.75.3.489. http://doi.org/10.1037/0022-006X.75.3.489. [DOI] [PubMed] [Google Scholar]
- Rohan K, Roecklein K, Lacy T, Vacek P. Winter depression recurrence one year after cognitive-behavioral therapy, light therapy, or combination treatment. Winter Depression Recurrence One Year after Cognitive-Behavioral Therapy, Light Therapy, or Combination Treatment. 2009;40 doi: 10.1016/j.beth.2008.06.004. http://doi.org/10.1016/j.beth.2008.06.004. [DOI] [PubMed] [Google Scholar]
- Tang TZ, DeRubeis RJ. Sudden gains and critical sessions in cognitive-behavioral therapy for depression. Journal of Consulting and Clinical Psychology. 1999;67:894–904. doi: 10.1037//0022-006x.67.6.894. http://doi.org/10.1037/0022-006X.67.6.894. [DOI] [PubMed] [Google Scholar]
- Vogel P, Hansen B, Stiles TC, Götestam KG. Treatment motivation, treatment expectancy, and helping alliance as predictors of outcome in cognitive behavioral treatment of OCD. Journal of Behavior Therapy and Experimental Psychiatry. 2006;37(3):247–55. doi: 10.1016/j.jbtep.2005.12.001. http://doi.org/10.1016/j.jbtep.2005.12.001. [DOI] [PubMed] [Google Scholar]
- Williams JB, Link MJ, Rosenthal NE, Amira L, Terman M. Structured Interview Guide for the Hamilton Depression Rating Scale—Seasonal Affective Disorder Version (SIGH-SAD) New York: New York State Psychiatric Institute; 1992. [Google Scholar]
- Wirz-Justice A, Benedetti F, Terman M. Chronotherapeutics for affective disorders: A clinician’s manual for light and wake therapy. 2nd. Basel, Switzerland: S. Karger AG; 2013. [DOI] [PubMed] [Google Scholar]
- Young M, Reardon A, Azam O. Rumination and vegetative symptoms: A test of the dual vulnerability model of seasonal depression. Rumination and Vegetative Symptoms: A Test of the Dual Vulnerability Model of Seasonal Depression. 2008;32 http://doi.org/10.1007/s10608-008-9184-z. [Google Scholar]


