Abstract
Objective
This study evaluated the efficacy of brief gambling treatments in patients attending substance abuse treatment clinics.
Methods
Substance abuse treatment patients with gambling problems (N = 217) were randomly assigned to: a 10–15 minute Brief Psychoeducation intervention about gambling; a 10–15 minute Brief Advice intervention addressing gambling norms, risk factors, and methods to prevent additional problems; or four 50-min sessions consisting of motivational enhancement therapy plus cognitive-behavioral therapy for reducing gambling (MET+CBT). Gambling and related problems were assessed at baseline and throughout 24 months.
Results
In the sample as a whole, days and dollars wagered as well as gambling problems decreased markedly from baseline through month 5; thereafter, reductions in dollars wagered and gambling problems continued to decrease modestly but significantly, while days gambled remained constant. Brief Advice significantly reduced days gambled between baseline and month 5 relative to Brief Psychoeducation. The MET+CBT condition engendered no benefit beyond Brief Advice in terms of days gambled, but it did lead to more precipitous reductions in dollars gambled and problems experienced in the initial five months, and it engendered greater clinically significant improvements in gambling in both the short and long term. MET+CBT also resulted in initial decreases in self-reported alcohol use and problems, but it did not differentially impact self-reported illicit drug use problems or submission of positive samples.
Conclusions
Gambling problems tend to dissipate over time regardless of the intervention applied, but offering MET+CBT was more efficacious in decreasing gambling than providing a brief single session intervention.
Keywords: gambling, treatment, brief interventions, cognitive behavioral treatment, motivational enhancement, substance abuse
Gambling disorder is now classified alongside substance use disorders in the fifth revision of the Diagnostic and Statistical Manual for Mental Disorders (DSM-5: American Psychiatric Association, 2013), a move that should raise awareness of the condition and increase access to treatment (Petry et al., 2013). In community samples, less than 1% of the population experiences significant gambling problems (Gerstein et al., 1999; Kessler et al., 2008; Petry, Stinson, & Grant, 2005; Welte, Barnes, Wieczorek, Tidwell, & Parker, 2001), but up to 20% of substance use disorder treatment patients suffer from gambling disorder or its subthreshold condition often referred to as problem gambling (Cowlishaw, Merkouris, Chapman, & Radermacher, 2014).
Despite the prevalence of problem gambling in substance use treatment patients, little is known about efficacious treatments in this population. In patients seeking treatment for gambling explicitly, cognitive-behavioral therapy (CBT) is efficacious at least over the short term (e.g., Carlbring & Smit, 2008; Carlbring, Jonsson, Josephson, & Forsberg, 2010; Dowling, Smith, & Thomas, 2007; Grant, Donahue, Odlaug, Kim, Miller, & Petry, 2009; Larimer et al., 2012; Oei, Raylu, & Casey, 2010; Petry et al., 2006). However, less than 10% of patients with gambling disorder access treatment for it (Cunningham, 2005; Slutske, 2006). Delivering gambling interventions in the context of substance abuse treatment may be an ideal avenue in which to address gambling in a group that experiences disproportionate rates of problems.
Among individuals who do initiate gambling treatment, less than half successfully complete it (Carlbring, Degerman, Jonsson, & Andersson, 2012; Carlbring & Smit, 2008; Carlbring et al., 2010; Larimer et al., 2012; Petry et al., 2006). Thus, patients may find brief interventions more acceptable. Brief interventions appear efficacious in reducing gambling problems and consist of phone calls in conjunction with CBT workbooks, minimal feedback or advice interventions, and motivational enhancement therapy (MET) alone or in combination with CBT (e.g., Cunningham, Hodgins, Toneatto, & Murphy, 2012; Hodgins, Currie, & el-Guebaly, 2001; Hodgins, Currie, Currie, & Fick, 2009; Larimer et al., 2012; Petry, Weinstock, Ledgerwood, & Morasco, 2008; Petry, Weinstock, Morasco, & Ledgerwood, 2009; Toneatto & Gunaratne, 2009). However, these studies all employed wait list or no treatment control conditions, which impact expectancy effects, and in the case of wait lists, also obviate the ability to assess long-term effects of interventions. Further, studies that included more than one intervention generally did not find differences between them, leaving questions as to whether any specific treatment is uniquely efficacious in reducing gambling.
This study builds upon prior reports by evaluating three interventions in patients with substance use and gambling problems. All interventions involved at least minimal therapist contact, thereby controlling for expectancy effects, and two interventions were of the same duration. One was a 10–15 min Psychoeducation intervention providing information about gambling and correlates of problem gambling. The second was a Brief Advice intervention, modelled after those efficacious in reducing heavy drinking (Bien, Miller, & Tonigan, 1993) and designed to enhance motivation to decrease gambling and provide information about methods to reduce it in a 10–15 min session. A MET+CBT condition contained some aspects similar to the Brief Advice condition, but it was more thorough in extent, content and duration, consisting of four 50-min sessions. The primary hypotheses were that Brief Advice would decrease gambling to a greater extent than Brief Psychoeducation, and that MET+CBT would yield greater benefits than Brief Advice. Both short and long-term effects were evaluated. The study also examined predictors of clinically significant changes in gambling, and it evaluated changes in substance use in response to the gambling interventions.
Method
Setting and participants
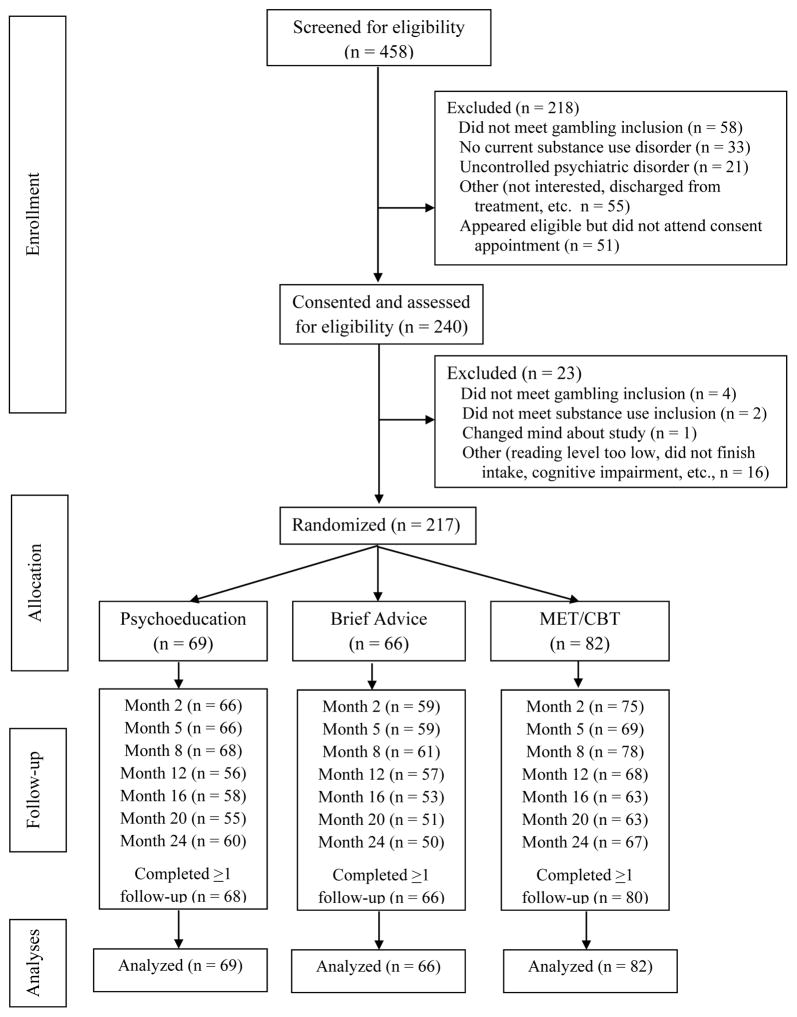
Participants were recruited at community-based outpatient methadone and psychosocial (non-opioid substitution clinics) substance abuse treatment clinics between 2008 and 2012. Research assistants (RAs) spent about one day/week at clinics recruiting study patients. Individuals who were 18 years or older, met Diagnostic and Statistical Manual for Mental Disorders-IV criteria for alcohol, cocaine, opioid or marijuana use disorders, gambled more than four days and $100 in the past 2 months and scored >3 on past 2 month South Oaks Gambling Screen (Leisure & Blume, 1987) were included. Exclusion criteria were suicidal intent or active psychosis, cognitive impairment or inability to read, and already receiving gambling treatment or desiring more intense treatment than provided in this study. Those who appeared to meet the inclusion, but not exclusion, criteria were invited to an in-person evaluation, at which informed consent, approved by the University’s Institutional Review Board, was obtained. Figure 1 shows flow of participants through the protocol; 217 participants were eligible and randomized to a treatment condition.
Figure 1.
Flow of participants through study protocol.
Assessments
Research assistants (RAs) administered assessments at baseline and 2, 5, 8, 12, 16, 20, and 24 months later. They conducted month 8 and 20 evaluations by phone, and others in person. Participants received $25 for phone and $50 for in-person interviews. Some post-baseline data were available on all but 3 (1.3%) participants (Fig 1). Staff conducting follow-ups differed from those randomizing participants when possible, but for 28 participants (8–10/group; 12.9% overall), the same RA who randomized the participant conducted all follow-ups and was not blinded to treatment. There were no differences in group, demographics or outcomes between these and other participants. Further, participants who completed versus did not complete follow-ups did not differ by any variable assessed.
Pathological gambling was determined at baseline using a module adapted from the Structured Clinical Interview for Diagnostic and Statistical Manual-IV (Grant, Steinberg, Kim, Rounsaville, & Potenza, 2004). The South Oaks Gambling Screen (SOGS; Lesieur & Blume, 1987) evaluated past 2-month gambling problems at baseline and through follow-up. The SOGS is a widely used problem gambling screening instrument and it correlates with DSM criteria and other measures of gambling severity (Hodgins, 2004; Stinchfield, 2002) and is a good indicator of severity of problems over time (Petry et al., 2006; Wulfert et al., 2005).
The Timeline Follow-back (TLFB; Sobell & Sobell, 1992) uses calendar prompts to elicit frequency and intensity of past behaviors. It has good test-retest reliability and validity for verifiable events (Sobell & Sobell, 1992), including gambling (Petry, 2003; Weinstock, Whelan, & Meyers, 2004). Days gambled and dollar amounts risked were recorded over the past 30 days.
Staff contacted collaterals, individuals whom participants identified as knowing about their gambling, for about half the participants. Collaterals who agreed to participate (N = 91; 28 from Brief Psychoeducation, 30 from Brief Advice, and 33 from MET+CBT conditions) were asked over the phone, “How often did (participant) gamble during the past two months on average?” Responses were coded on a 5-point scale: 0=“not at all;” 1=“once;” 2=“more than once but less than once a week;” 3=“more than once a week, but less than 4 times per week;” and 4=“four or more times per week.” A “don’t know” response was also possible, and these responses, which did not differ by group, were not included in analyses. Collaterals received a $5 gift card for each phone interview completed; 76.4% of collaterals completed at least one follow-up.
The Addiction Severity Index (ASI; McLellan, et al., 1988) evaluates problems in domains commonly affected by addictive disorders, including medical, employment, psychiatric, and alcohol and illicit drug use. Scores range from 0 to 1.0, with higher scores reflecting more severe problems. Psychometric properties of the ASI are established in substance abuse treatment patients (McLellan et al., 1988) and gamblers (Petry, 2003, 2007). Breath and urine samples were also collected at in-person study baseline and follow-up visits and tested for alcohol, stimulants, opioids, marijuana and benzodiazepines using testing kits from Instant Technologies Incorporated (Norfolk, VA).
Randomization
After the baseline evaluation, a computerized program (Stout, Wirtz, Carbonari, & Del Boca, 1994) randomized participants and balanced groups on diagnosis (>5 or <5 DSM-IV gambling criteria), clinic type (methadone or psychosocial), and study therapist. Participants were randomized according to a 3:3:4 ratio to treatments described below, planning for more participants in MET+CBT, as not all were expected to attend sessions beyond the first. The sample size to detect differences between two groups at power = 0.80 and alpha = .05 was estimated using effect sizes from Petry et al. (2008); in that study, the effect size for clinically significant changes of a brief intervention was phi = 0.37. Because this study employed an active control condition and longer follow-up, we projected phi = 0.30, which can be detected with ns > 60 per group.
Treatments
The study did not alter substance abuse treatment. All clinics provided standard outpatient substance abuse care, which was eclectic in nature, consisting of groups for case management, daily planning, cognitive-behavioral therapy, relapse prevention, 12-step interventions, focus groups on parenting, depression, etc. Methadone clinics also provided daily dosing and tested at least one urine sample per month, but outpatient clinics rarely screened for drug use; clinic samples were independent of study samples, and results not shared between teams. Patients could continue with substance use treatment even if they did not participate in gambling treatment, and vice versa. Research staff provided no information about study participants to the substance abuse treatment clinicians.
The first two gambling treatments outlined below were delivered in a one-time 10–15 min session by study therapists (see below); participants in these conditions did not meet again with a research therapist. The gambling treatment was delivered primarily at the substance abuse treatment clinics, but locations could be altered to accommodate patient preference.
Brief Psychoeducation
A research therapist provided and reviewed a one-page handout describing basic information about gambling, including types of gambling and relationships between gambling, drug use, moods, and legal problems. This 10–15 min session occurred right after the intake and did not provide suggestions about ways to reduce gambling. Topics were selected because they did not overlap with the Brief Advice yet controlled for contact and expectations between these conditions. After the Psychoeducation, therapists reminded participants about follow-ups and provided a toll-free number to call if they experienced increases in gambling.
Brief Advice
A research therapist provided a 10–15 min intervention after the evaluation. Using a one-page handout (Petry, 2005), the therapist described the participant’s gambling in relation to the general population, outlined risk factors for development of more severe problems, and discussed four steps to curtail their development. Steps included limiting gambling money (e.g., to <$10/week), reducing time and days gambling, not viewing gambling as a way to make money, and spending time on other activities. Therapists also informed participants about follow-up interviews and a toll-free number to call if they experienced increases in gambling problems.
MET+CBT
These participants met with a research therapist for a 50-minute MET session; they received personalized feedback, explored positive and negative consequences of gambling, and discussed how gambling fit within goals and values. They completed a change plan worksheet, and therapists encouraged them to return for three sessions of CBT in the next three weeks. Sessions focused on: determining internal and external triggers of gambling; discussing methods for coping with internal triggers such as lonely, depressed or anxious moods; and developing coping skills for external gambling triggers or cues. Petry (2005) contains handouts, which were modified to emphasize reductions in gambling, rather than abstinence, as the goal (Dowling, Smith & Thomas, 2009; Slutske, Piasecki, Blaszczynski, & Martin, 2010). Anecdotally, few had abstinence goals.
Therapists
Five BA to MA level research therapists delivered gambling therapy. They received didactic training and close supervision of at least one case per condition. Ongoing supervision consisted of regular review of therapy notes and audiotapes and case discussion. Using a modification of the Yale Adherence Competence Scale (Carroll et al., 2000), four MA to PhD level therapists rated 63 randomly selected tapes for Psychoeducation, Brief Advice, MET, and CBT items on 7-point likert scales (1=not at all/poor, 3=somewhat/adequate, 7=extensive/excellent). An example of a Psychoeducational item was, “To what extent did the therapist present the client with factual information about gambling, including types of gambling, frequently co-occurring problems, and legal problems?” A Brief Advice item was, “To what extent did the therapist provide concrete recommendations for reducing gambling?” An MET item was, “To what extent were the therapist’s questions open-ended and reflective?” A CBT item included, “To what extent did the therapist attempt to teach, model, or rehearse specific coping skills (problem solving, coping with craving, social skills)?” Inter-rater reliability, using the intraclass correlation coefficient, was 0.88.
In Brief Psychoeducation sessions, means (and standard deviations; SD) on Psychoeducation items were 5.7 (SD = 0.7) (reflecting “considerably/good”); average ratings on Brief Advice, MET and CBT items were 1.0 (SD = 0.1), 1.1 (SD = 0.1), and 1.0 (SD = 0.0), respectively. In contrast, Brief Advice sessions were rated 5.9 (SD = 0.6) on Brief Advice items and 1.0 (SD = 0.0), 1.0 (SD = 0.1), and 1.0 (SD = 0.0) on Psychoeducation, MET and CBT items. In MET sessions, MET items were rated 5.2 (SD = 0.7) versus 1.0 (SD = 0.0), 1.0 (SD = 0.2), and 1.1 (SD = 0.2) for Psychoeducation, Brief Advice, and CBT items, respectively. CBT sessions were rated as 4.6 (SD = 0.8) for CBT, 1.0 (SD = 0.0) for Psychoeducation, 1.0 (SD = 0.0) for Brief Advice, and 1.5 (SD = 0.6) for MET items. Thus, the therapies were distinguishable (ps <.001). Brief Psychoeducation sessions on average were 11 (SD = 2) min and did not differ from Brief Advice sessions at 12 (SD = 2) min, while MET and CBT sessions were significantly longer at 51 (SD = 8) min, p < .001.
Data analysis
Analysis of variance and Chi-square tests examined baseline differences across groups. Non-normally distributed data were transformed, including log transformations for dollars wagered and square root transformations for SOGS scores.
Intent-to-treat analyses were conducted using hierarchical linear models (HLM; Hedeker, 1993). In these analyses, intercepts were allowed to vary randomly. Slopes were constrained to improve convergence and the reliability of estimates. Primary outcomes were defined a priori as days and dollars gambled, as well as past 2-month SOGS scores, reflecting severity of gambling-related problems. Two contrasts were evaluated. The “Brief Type” contrast assessed whether Brief Advice resulted in less gambling than Brief Psychoeducation; reference codes of +1 were assigned to Brief Advice and 0 to Brief Psychoeducation. The second assessed “Extent” of treatment, with reference codes of +1 assigned to the MET+CBT condition and 0 to Brief Advice. Note this contrast is more conservative than one comparing both brief interventions to the more extended one because Brief Advice was expected to yield benefits beyond Brief Psychoeducation (Petry et al., 2008, 2009). Contrast by time analyses evaluated if groups differed over time. Analyses were conducted from baseline to month 5 to assess initial treatment effects (with baseline day reference coded 0), and from months 5 to 24 to assess enduring effects (with month 5 day reference coded 0 and subsequent follow-up days coded relative to that). This approach was chosen because it is consistent with the specific a priori hypotheses of this study and provided a good fit for the data. It allows for separate estimation of rate of change across time periods, best reflecting the data obtained in that reductions in gambling were far more pronounced in early versus later time periods.
Participants were also classified into one of three categories based on clinically significant changes (Jacobson & Truax, 1991) at earlier (through month 5) and longer-term follow-ups. Categories were defined by SOGS scores and dollars wagered: “Recovered” (SOGS = 0 and dollars wagered in past month < $100), “Significantly improved” (SOGS < 3 or dollars wagered in past month < $100), or “Unchanged” (SOGS > 3 and dollars wagered in past month > $100). No participants were considered Deteriorated (e.g., dollars wagered or SOGS score increased by >1 SD from baseline). These definitions were selected because they included both subjective indices of problems (SOGS scores, 0=no problems and <3=non-problem) and amounts wagered, such that denial of problems alone would not constitute full recovery if amounts exceeded study inclusion criteria values. To ensure stability, categorizations were based on two consecutive assessments meeting criteria (e.g., months 2 and 5 for post-treatment, and months 20 and 24 for long-term). To include the most participants, data from the most proximal assessments were considered for those who missed an assessment (e.g., months 16 and 24 if month 20 was missed). Mann Whitney U tests evaluated group differences comparing the two Brief interventions and Brief Advice vs MET+CBT.
Logistic regressions evaluated baseline variables associated with substantial reductions or recovery from gambling problems at the 5-month evaluation. Gender, methadone maintenance status, past year DSM-IV pathological gambling status, and ASI medical, employment, psychiatric, alcohol and drug scores were entered in the first step. The first three were dichotomous variables, and the others were continuous. In Step 2, the categorical indicator for treatment group was entered. These variables were selected for inclusion in the model because they were theoretically related to outcomes or significantly correlated with them. Other potential variables (e.g., age, recruitment site, race/ethnicity, substance use diagnosis other than opioid dependence, which was highly correlated with methadone treatment status) were not associated with outcomes. A similar analysis was conducted at the most distal evaluations, predicting long-term recovery from problem gambling status. For primary moderator analyses, only participants who completed follow-ups were included; parallel analyses were conducted coding non-completers as unchanged in terms of gambling.
HLM analyses, assessing both the Brief Type and Extent contrasts, were also conducted on ASI-alcohol and drug scores over time; transformations attempted to correct for violations of normality assumptions were not successful and scores were therefore dichotomized (0 = no use or problems versus >0 = any use or problems) and nonlinear models specified. Similar HLM analyses evaluated changes in submission of substance positive samples over time.
Results
Sample description and treatment participation
Table 1 shows baseline variables for participants assigned to the three treatment conditions. There were no differences across groups on any baseline measure, including baseline indices of gambling (Table 2, left column), which likewise did not differ across groups, all ps > .17.
Table 1.
Demographic and baseline characteristics.
| Demographics | Brief Psychoeducation | Brief Advice | MET + CBT | F or χ2 | df | p |
|---|---|---|---|---|---|---|
| N | 69 | 66 | 82 | |||
| Clinic, No. (%) | 8.20 | 10 | .61 | |||
| Clinic A | 18 (26.1) | 19 (28.8) | 21 (25.6) | |||
| Clinic B | 12 (17.4) | 16 (24.2) | 18 (22.0) | |||
| Clinic C | 14 (20.3) | 11 (16.7) | 12 (14.6) | |||
| Clinic D | 13 (18.8) | 10 (15.2) | 12 (14.6) | |||
| Clinic E | 5 (7.2) | 8 (12.2) | 7 (8.5) | |||
| Miscellaneous clinics | 7 (10.1) | 2 (3.0) | 12 (14.6) | |||
| Age, mean (SD), y | 40.9 (10.5) | 42.1 (10.3) | 42.7 (11.3) | 0.54 | 2,214 | 0.58 |
| Female, No. (%) | 21 (30.4) | 26 (39.4) | 21 (25.6) | 3.27 | 2 | 0.20 |
| Race/ethnicity, No. (%) | 4.45 | 6 | 0.62 | |||
| African American | 37 (53.6) | 35 (53.0) | 38 (46.3) | |||
| White, non-Hispanic | 18 (26.1) | 20 (30.3) | 25 (30.5) | |||
| Hispanic | 12 (17.4) | 10 (15.2) | 19 (23.2) | |||
| Other | 2 (2.8) | 1 (1.6) | 0 (0.0) | |||
| Marital status, No. (%) | 3.49 | 4 | 0.48 | |||
| Never married | 43 (62.3) | 37 (56.1) | 40 (48.8) | |||
| Divorced or widowed | 16 (23.2) | 20 (30.3) | 30 (36.6) | |||
| Married or living with partner | 10 (14.5) | 9 (13.6) | 12 (14.6) | |||
| Education, mean (SD), years | 11.9 (1.8) | 11.5 (2.0) | 11.8 (1.8) | 0.87 | 2,214 | 0.42 |
| Employment status, No. (%) | 0.61 | 4 | 0.96 | |||
| Full- or part-time | 11 (15.9) | 10 (15.2) | 12 (14.6) | |||
| Unemployed | 44 (63.8) | 41 (62.1) | 49 (59.8) | |||
| Other, not in work force | 14 (20.3) | 15 (22.7) | 21 (25.6) | |||
| Annual income, mean (SD), $ | 10,974 (14,888) | 16,828 (26,604) | 12,404 (10,493) | 2.13 | 2,214 | 0.13 |
| Addiction Severity Index scores | ||||||
| Medical, mean (SD) | 0.31 (0.40) | 0.31 (0.39) | 0.23 (0.34) | 1.07 | 2,214 | 0.34 |
| Employment, mean (SD) | 0.83 (0.24) | 0.74 (0.28) | 0.77 (0.26) | 2.12 | 2,213 | 0.12 |
| Legal, mean (SD) | 0.14 (0.18) | 0.13 (0.21) | 0.10 (0.17) | 1.04 | 2,214 | 0.36 |
| Family/social, mean (SD) | 0.11 (0.16) | 0.13 (0.18) | 0.15 (0.18) | 1.25 | 2,212 | 0.29 |
| Psychiatric, mean (SD) | 0.21 (0.22) | 0.19 (0.20) | 0.17 (0.20) | 0.65 | 2,213 | 0.52 |
| Alcohol, mean (SD) | 0.11 (0.18) | 0.11 (0.20) | 0.09 (0.16) | 0.35 | 2,213 | 0.70 |
| Drug, mean (SD) | 0.07 (0.09) | 0.04 (0.07) | 0.04 (0.07) | 2.41 | 2,214 | 0.09 |
| Past year substance dependence | ||||||
| Alcohol, No. (%) | 35 (50.7) | 36 (54.5) | 44 (53.7) | 0.22 | 2 | 0.90 |
| Cocaine, No. (%) | 44 (63.8) | 46 (69.7) | 47 (57.3) | 2.42 | 2 | 0.30 |
| Opioids, No. (%) | 32 (46.4) | 27 (40.9) | 32 (39.0) | 0.87 | 2 | 0.65 |
| Marijuana, No. (%) | 19 (27.5) | 11 (16.7) | 16 (19.5) | 2.61 | 2 | 0.27 |
| Receiving methadone, No. (%) | 33 (47.8) | 34 (51.5) | 41 (50.0) | 0.19 | 2 | 0.91 |
| Methadone dose, mean (SD), mm | 77.9 (34.7) | 76.6 (29.1) | 75.1 (37.7) | 0.06 | 2,94 | 0.95 |
| Age first gambled, mean (SD), y | 15.7 (5.4) | 15.9 (6.4) | 16.7 (6.8) | 0.59 | 2,214 | 0.55 |
| Prior gambling treatment, No. (%) | 5 (7.2) | 3 (4.5) | 6 (7.3) | 0.47 | 2 | 0.79 |
| Pathological gambling, No. (%) | 58 (84.1) | 57 (86.4) | 72 (87.8) | 0.44 | 2 | 0.80 |
| Preferred gambling, No. (%) | 8.74 | 12 | 0.73 | |||
| Scratch/instant tickets | 25 (36.2) | 25 (37.9) | 29 (35.4) | |||
| Card games | 20 (29.0) | 19 (28.8) | 15 (18.3) | |||
| Lottery tickets | 12 (17.4) | 16 (24.2) | 19 (23.2) | |||
| Sports | 3 (4.3) | 1 (1.5) | 6 (7.3) | |||
| Slot machines | 3 (4.3) | 2 (3.0) | 5 (6.1) | |||
| Craps or dice games | 4 (5.8) | 1 (1.5) | 5 (6.1) | |||
| Other | 2 (2.9) | 2 (3.0) | 3 (3.7) | |||
Table 2.
Baseline gambling measures and outcomes from random regression model analyses (N = 217).
| Variable | Baseline | Month 2 | Month 5 | Month 8 | Month 12 | Month 16 | Month 20 | Month 24 |
|---|---|---|---|---|---|---|---|---|
| Days gambled | ||||||||
| Psychoeducation | 16.8 (5.2) | 14.0 (5.2) | 9.7 (5.3) | 9.5 (7.4) | 8.9 (7.4) | 8.3 (7.3) | 7.7 (7.3) | 7.1 (6.7) |
| Brief advice | 19.4 (5.3) | 15.2 (5.9) | 8.5 (5.9) | 9.4 (6.6) | 9.1 (6.7) | 8.9 (6.6) | 8.7 (6.7) | 8.5 (6.7) |
| MET + CBT | 18.0 (4.5) | 13.5 (5.3) | 6.4 (5.1) | 7.2 (7.5) | 7.0 (7.7) | 6.9 (7.8) | 6.7 (8.0) | 6.6 (8.8) |
| Dollars gambled* | ||||||||
| Psychoeducation | 275 (380) | 96 (141) | 16 (26) | 15 (130) | 6 (20) | 4 (46) | 4 (29) | 3 (19) |
| Brief advice | 301 (421) | 98 (152) | 21 (27) | 11 (86) | 8 (62.7) | 5 (44) | 3 (30) | 2 (23) |
| MET + CBT | 240 (498) | 35 (98) | 3 (7) | 2 (39) | 1 (24) | 1 (22) | 1 (36) | 1 (16) |
| SOGS score | ||||||||
| Psychoeducation | 7.7 (2.6) | 5.7 (2.3) | 3.1 (1.7) | 2.7 (3.0) | 2.1 (2.5) | 1.7 (2.1) | 1.3 (1.9) | 1.0 (1.8) |
| Brief advice | 7.8 (2.8) | 5.6 (2.6) | 3.0 (1.9) | 2.6 (3.1) | 2.1 (2.9) | 1.6 (2.7) | 1.2 (2.6) | 1.0 (2.6) |
| MET + CBT | 7.9 (3.9) | 5.0 (3.6) | 1.9 (3.6) | 1.9 (2.7) | 1.5 (2.5) | 1.2 (2.2) | 1.0 (2.0) | 1.0 (1.8) |
| Variable | Baseline through month 5 analyses, β, p value, Effect sizeΨ | Month 5 through month 24 analyses, β, p value, Effect sizeΨ | |||||
|---|---|---|---|---|---|---|---|
| Contrast | Time effect | Contrast effect | Time × contrast | Contrast | Time effect Contrast effect | Time × contrast | |
| Days gambled | |||||||
| Brief type | −0.05,<.001 (−9 days) | 2.65, 0.09 | −0.02, <.05 (−3.8 days) | Brief type | −0.005, <.05 (−1.3 days) | −0.35, 0.84 | 0.003, 0.41 |
| Extent | −0.07,<.001 (−11.3 days) | −1.48, 0.32 | −0.04, 0.69 | Extent | −0.002, 0.54 | −2.27, 0.16 | 0.001, 0.84 |
| Dollars gambleda | |||||||
| Brief type | −0.008,<.001 (−$269.50) | −0.01, 0.95 | −0.0001, 0.93 | Brief type | −0.002,<.001 (−$16.00) | −0.01, 0.96 | −0.0001, 0.92 |
| Extent | −0.008,<.001 (−$258.50) | −0.07, 0.66 | −0.004, <.04 (−$43.00) | Extent | −0.002,<.001 (−$10.50) | −0.71, <0.05 (−$6.83) | 0.001, 0.09 |
| SOGS scoreb | |||||||
| Brief type | −0.01,<.001 (−4.7) | 0.02, 0.88 | −0.0003, 0.77 | Brief type | −0.001,<.001 (−2.1) | −0.04, 0.82 | 0.00005, 0.89 |
| Extent | −0.01,<.001 (−5.4) | 0.01, 0.94 | −0.002, <.05 (−1.2) | Extent | −0.001,<.001 (−1.5) | −0.17, 0.29 | −0.0003, 0.92 |
Values represent means and standard deviations derived from hierarchical linear modlels (back transformed for dollars gambled and SOGS scores) unless otherwise noted.
Values are raw medians (interquartile ranges).
Log-transformed values were analyzed.
Square-root transformed values were analyzed.
MET=Motivational Enhancement Therapy; CBT=Cognitive Behavioral Therapy; SOGS= South Oaks Gambling Screen Brief type contrast: Compares the Brief Psychoeducation (0) to the Brief Advice group (+1).
Extent contrast: Compares the Brief Advice (0) to the Motivational Enhancement + Cognitive Behavioral Therapy group (+1); although the term Extent is used to depict this contrast, content of the interventions differed in addition to the Extent. Bolded values are statistically significant, p < .05. ΨEffect sizes are presented for significant effects.
All participants assigned to brief interventions completed the session. Of 82 participants assigned to MET+CBT, 49 (59.8%) came to one or more of the CBT sessions scheduled a week after the initial MET session, with 23 (28.0%) completing all three CBT sessions. Gambling treatment attendance was not related to clinic type (methadone vs psychosocial); methadone patients attended 2.2 (SD = 1.5) sessions and non-methadone patients 2.0 (SD = 1.4), t(80) = 0.74, p = .50. Of patients recruited from methadone clinics, 74.3% remained in methadone treatment at Month 5, and 63.1% at Month 24. Of patients recruited from psychosocial clinics, 33.7% received some outpatient substance abuse treatment in the past month at Month 5 and 12.5% at Month 24. Only 3 participants (1.4%) reported receiving gambling treatment beyond that provided in the study in Months 8–24; none reported additional gambling treatment from baseline to Month 5.
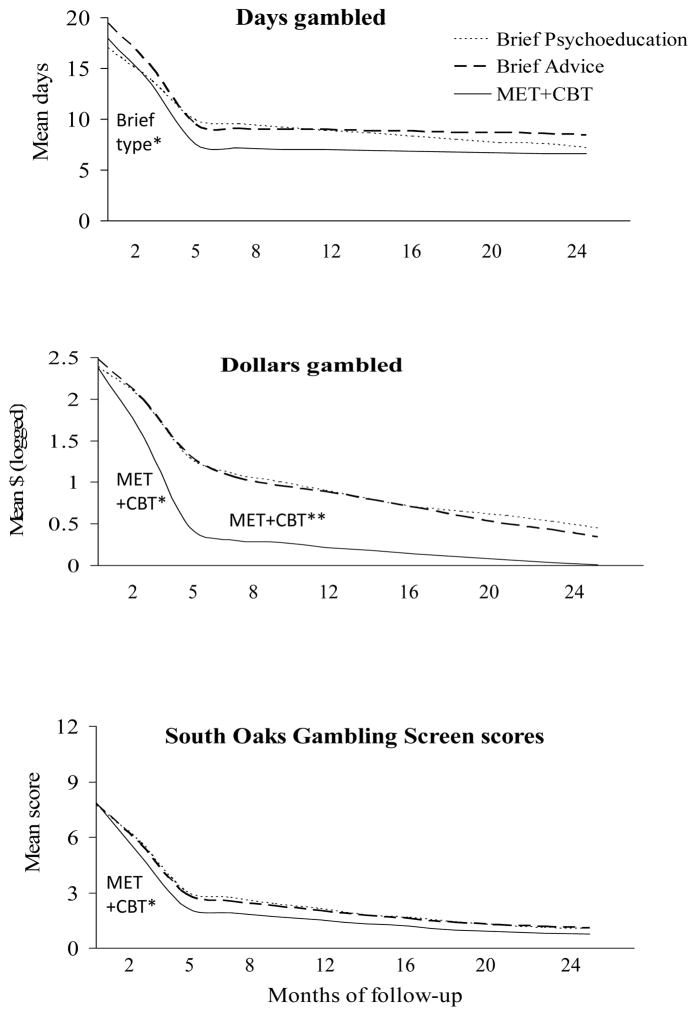
Short term effects of interventions on gambling
Table 2 (left side: baseline to Month 5) and Figure 2 (baseline to Month 5) show primary outcome measures and results from HLM analyses derived from all participants through the first five months after randomization. Time effects, indicating a substantial reduction in gambling over time, were significant for all three indices. The Brief Type by time contrast was significant for days gambled, with those assigned to Brief Advice showing more precipitous declines in days gambled from baseline through month 5 than those assigned to Brief Psychoeducation. The two brief interventions did not differ in dollars gambled or SOGS scores between baseline and month 5.
Figure 2.
Gambling variables by days since randomization to a treatment condition. Values represent past-month measures and are estimates from random effects regression analyses (square root South Oaks Gambling Scores were analyzed and back transformed for the figure). MET+CBT=Motivational enhancement therapy + cognitive behavioral therapy. Brief type* represents a significant (p < .05) contrast by time effect between the two briefest interventions from baseline throughout month 5. MET+CBT* denotes a significant (p < .05) contrast by time effect between the MET+CBT and Brief Advice interventions from baseline throughout month 5; MET+CBT** denotes a significant (p < .05) contrast effect between the MET+CBT and Brief Advice interventions from months 5 through month 24.
The Treatment Extent by time contrast was significant for dollars wagered and SOGS scores, with more pronounced decreases in amounts wagered and problems experienced in participants assigned to the 4-session intervention than the Brief Advice condition between baseline and month 5 (Table 2 and Figure 2). Days gambled did not differ over time between these groups.
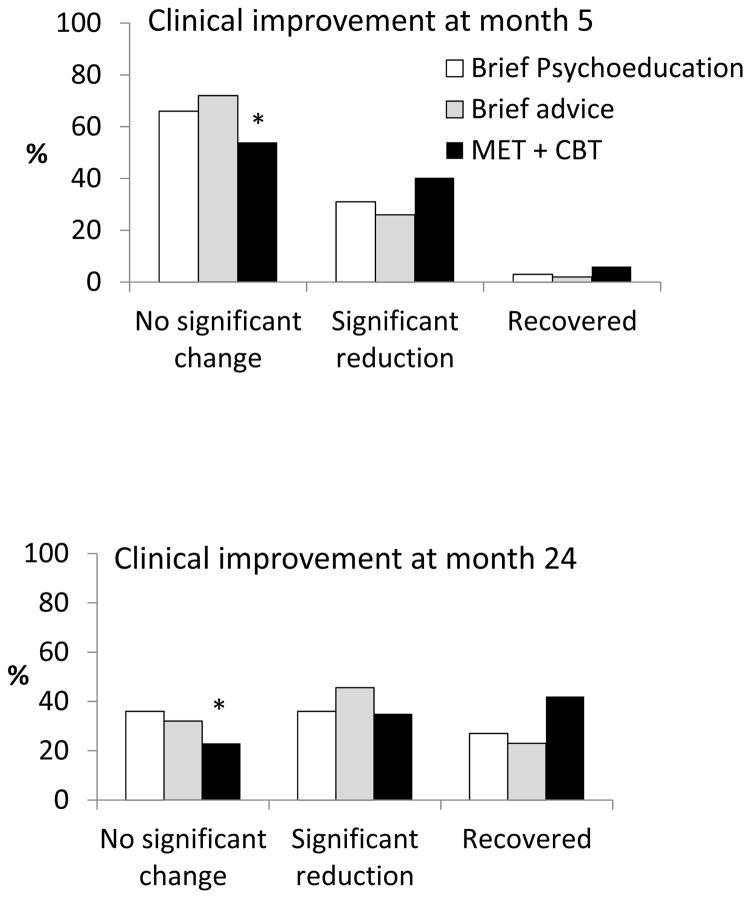
Categorizations of clinically significant improvements at month 5 differed between groups. Figure 3 (top panel) illustrates proportions classified as recovered, with significant reductions in gambling, or with no substantial changes in gambling between baseline and month 5. There were no differences between the two brief interventions, U = 1822, p = .48, but those assigned to MET+CBT evidenced greater improvements than those receiving Brief Advice, U = 1672, p < .05.
Figure 3.
(Top panel). Proportion of participants demonstrating clinically significant reductions in gambling or were recovered from problem gambling between baseline and the month 5 evaluation. Clinically significant reductions were classified by South Oaks Gambling Screen scores < 3 or dollars wagered per month <$100, and recovery as South Oaks Gambling Screen scores = 0 and dollars wagered per month <$100. MET+CBT=Motivational enhancement therapy + cognitive behavioral therapy. The * indicates significant differences in proportions classified in treatment conditions. See text for further details.
(Bottom panel). Proportion of participants demonstrating clinically significant reductions in gambling at the most distal follow-up evaluations.
Long-term effects of the interventions on gambling
Table 2 (right) depicts gambling variables through 24 months, and Figure 2 shows these variables throughout the study period. Time effects remained significant for dollars wagered and SOGS scores, representing continued declines in both these variables from months 5 to 24 in the sample as a whole. In contrast, days gambled remained constant after month 5. No group by time effects were significant between months 5 and 24, indicating no differential changes by group over time after the initial decreases baseline and month 5. However, the Extent contrast was significant for dollars wagered, indicating participants assigned to MET+CBT consistently reduced amounts wagered relative to those assigned to Brief Advice throughout the longer term follow-up period.
At the most distal follow-ups, proportions classified as recovered, substantially reduced, or not changed based on SOGS scores and dollars wagered differ by treatment (Figure 3 bottom). The two briefest interventions did not differ, U = 2065.5, p = .24, while MET+CBT yielded more clinically significant reductions in gambling than Brief Advice, U = 2257.5, p < .05.
Concordance with collateral reports
Spearman correlations between participant self reports (measured in days gambled, 0–30) and collaterals (measured by a 0–5 ordinal scale) were significant. The overall r was 0.29, p < .001, and similar across treatment groups (range: 0.24 to 0.36).
Variables associated with significant changes
At month 5, Step 1 including baseline variables was associated with substantial reductions in or recovery from gambling problems, χ2 (d.f. = 8, N = 194) = 22.32, p < .01. Inclusion of Step 2 (treatment condition) was also significant, χ2 (d.f. = 2, N = 194) = 7.79, p < .05, and improved the model, χ2 (d.f. = 10, N = 194) = 30.11, p < .001. Table 3 (middle columns) shows the final model. Females were approximately twice as likely as males to achieve substantial reductions or recovery from gambling problems by month 5. Patients receiving methadone were about 65% less likely to reduce gambling substantially relative to their counterparts in entirely psychosocial treatment. Patients with greater employment problems on the ASI were more likely to evidence clinically significant reductions in gambling in the short term than those with fewer employment problems. After controlling for baseline variables, those assigned to the MET+CBT condition were three times more likely to substantially decrease gambling in the five months after the intervention than those receiving the Brief Advice condition, who did not differ from those receiving Psychoeducation.
Table 3.
Results from logistic regressions predicting significant reduction or recovery from gambling problems.
| Month 5 evaluation (N = 194) | Month 24 evaluation (N = 193) | |||||
|---|---|---|---|---|---|---|
| Beta (SE) | Wald, p | Odds ratio(95%CI) | Beta (SE) | Wald, p | Odds ratio (95%CI) | |
| Female gender | 0.78 (0.37) | 4.56, <.05 | 2.19 (1.07–4.48) | 0.53 (0.35) | 2.32, .13 | |
| Receiving methadone | −1.06 (0.34) | 9.72, <.01 | 0.35 (0.18–0.68) | −0.43 (0.33) | 1.65, .20 | |
| Past year pathological gambler | 0.42 (0.49) | 0.74, .39 | 0.23 (0.49) | 0.22, .64 | ||
| ASI-Medical score | 0.90 (0.46) | 3.81, .05 | 0.42 (0.45) | 0.88, .35 | ||
| ASI-Employment score | 1.53 (0.68) | 5.03, <.05 | 4.63 (1.21–17.69) | 0.59 (0.66) | 0.79, .38 | |
| ASI-Psychiatric score | −1.54 (0.86) | 3.20, .07 | −0.23 (0.84) | 0.08, .78 | ||
| ASI-Alcohol score | −0.35 (1.03) | 0.12, .73 | −1.09 (1.07) | 1.04, .31 | ||
| ASI-Drug score | 0.39 (2.27) | 0.03, .86 | −0.13 (2.27) | 0.00, .95 | ||
| Treatment | ||||||
| Brief Advice vs Psychoeducation | 0.35 (0.43) | 0.66, .42 | 0.30 (0.45) | 0.46, .50 | ||
| Brief Advice vs MET + CBT | 1.11 (0.43) | 6.69, <.01 | 3.02 (1.31–6.99) | 1.02 (0.42) | 5.92, <.02 | 2.78 (1.22–6.33) |
Notes: ASI=Addiction Severity Index; MET=Motivational Enhancement Therapy; CBT=Cognitive Behavioral Therapy.
Reference categories are male for gender, not receiving methadone maintenance, and not past year pathological gambling at baseline.
Bolded values are statistically significant, p < .05.
Results were similar when participants who did not complete short-term follow-ups were included as unchanged in terms of gambling. All variables significant in the primary analyses (Table 3) remained significant in the supplemental analyses including non-completers (data not shown; available from authors). The MET+CBT condition had an odds ratio (OR) and 95% confidence interval (CI) of 2.66 (1.20 to 5.89) in predicting substantial reductions in gambling.
In evaluating longer-term effects, Step 1, consisting of baseline variables, was not significant in predicting recovery from gambling problems, χ2 (d.f. = 8, N = 193) = 6.38, p = .61. Inclusion of Step 2 (treatment condition), however, was significant, χ2 (d.f. = 2, N = 193) = 7.12, p < .03, and relative to those assigned to Brief Advice, those assigned to the MET+CBT condition had over a two-fold increased likelihood of improving outcomes at the most distant follow-ups. No other variables were associated with clinically significant changes, and results were nearly identical when participants who did not complete the latter follow-up evaluations were included in analyses as unchanged with respect to gambling (data not shown; available from authors), with only the MET+CBT condition significant, OR (95% CI) = 2.83 (1.27 to 6.33).
Substance use
From baseline through month 5, the likelihood of scoring above 0 on the ASI-alcohol scale decreased in the sample overall, slope coefficient = −0.003 (SE = 0.001), T-ratio (df = 389) = −2.62, p = .01, OR (95% CI) = 0.997 (0.994, 0.999). These reduction were more precipitous in MET+CBT compared to Brief Advice, interaction term coefficient = −0.004 (SE = 0.002), T-ratio (d.f. = 389) = −2.07, p < .05, OR (95% CI) = 0.996, (0.993, 1.000). Over the same period, the likelihood of alcohol problems did not differ by Brief Type (p = .80). From months 5 to 24, the likelihood of reporting any alcohol use or problems did not change over time (p = .37), by Brief Type over time (p = .51), or by Treatment Extent (p = .19). Likelihood of scoring > 0 on the ASI-alcohol scale at baseline, month 5, and month 24, respectively, were 0.35, 0.24, and 0.19 for Brief Psychoeducation, 0.35, 0.34, and 0.16 for Brief Advice, and 0.34, 0.16, and 0.23 for MET+CBT.
On the ASI-drug scale, the likelihood of scoring above 0 decreased over time, with slope coefficient = −0.005 (SE = 0.001), T-ratio (d.f. = 389) = −4.30, p < .001, OR (95% CI) = 0.995 (0.992, 0.997) for baseline through month 5, and slope coefficient = −0.003 (SE = 0.000), T-ratio (d.f. = 857) = −9.125, p < .01, OR (95% CI) = 0.997 (0.997, 0.998) from months 5 to 24. This variable, however, did not vary significantly over time by treatment condition in the short or long term (ps ≥ .09). At baseline, month 5, and month 24, the predicted probabilities of scoring > 0 on the ASI-drug scale were 0.56, 0.50, and 0.32 for Brief Psychoeducation, 0.72, 0.58, and 0.34 for Brief Advice, and 0.39, 0.44, and 0.31 for MET+CBT.
From baseline to month 5, the proportions of participants testing positive for alcohol or an illicit drug increased in the sample overall, slope coefficient = 0.005 (SE = 0.001), T-ratio (d.f. = 346) = 3.60, p = < .001, OR (95% CI) = 1.005 (1.002, 1.008). The odds of testing positive did not change between months 5 and 24, and interactions by time and treatment conditions were non-significant (ps > .53). At baseline, month 5, and month 24, the predicted probabilities of testing positive were 0.30, 0.53, and 0.45 for Brief Psychoeducation, 0.33, 0.63, and 0.57 for Brief Advice, and 0.27, 0.43, and 0.33 for MET+CBT. No study related adverse events occurred.
Discussion
Gambling decreased over time among the majority of participants in this study. The most precipitous reductions occurred in the first 5 months, and thereafter amounts wagered and problems continued to decline modestly, although still significantly, through the 24-month period. Days wagered decreased substantially in the first 5 months and then remained steady. About one-third of participants significantly decreased or ceased gambling by month 5, and two-thirds recovered or significantly decreased gambling by month 24. These data are consistent with epidemiological studies finding that 50% or more of persons identified with gambling disorder over their lifetimes do not meet past-year criteria (e.g., Hodgins, Wynne, & Makarchuk, 1999; Kessler et al., 2008; Petry et al., 2005). Longitudinal studies likewise reveal decreases in gambling over time in young adults (Slutske, Jackson, & Sher, 2003). Other treatment studies also report declines in gambling in about two-thirds of participants (Carlbring & Smit, 2008; Hodgins, Currie, el-Guebaly, & Peden, 2004; Hodgins, Currie, el-Guebaly, & Diskin, 2007; Hodgins et al., 2009). Volunteering for a study, or monitoring alone, may relate to decreases in gambling. Gambling problems may resurface years later, but these data indicate they subside in many substance abusing problem gamblers over a 2-year period. These sharp decreases in gambling also warn against drawing conclusions about effectiveness of interventions in uncontrolled studies or those applying wait-list controls.
Although gambling decreased in the sample as a whole, reductions occurred more quickly depending on the intervention. Specifically, Brief Advice engendered more rapid declines in gambling frequencies than Brief Psychoeducation. No other changes in gambling were noted between the two minimal intervention groups in the short or longer term. Thus, although this directive Brief Advice may be efficacious in reducing gambling frequency, the content of brief interventions appears inconsequential in reducing gambling along other dimensions.
Compared to Brief Advice, MET+CBT significantly reduced amounts wagered and SOGS scores. These decreases occurred primarily in the first five months. Although MET+CBT resulted in lower amounts wagered than Brief Advice throughout month 24, amounts wagered were low overall by the end of the study period (median <$10 per month). Assignment to MET+CBT was the only significant predictor of long term recovery from problem gambling, measured out to 24 months. These results suggest that MET+CBT may be efficacious in reducing gambling, but it is unclear whether this intervention, or any intervention that controls for therapist contact time, would engender similar effects because this study had no control for therapist time for this intervention. Benefits of MET+CBT emerged even though only a little more than half the participants attended two or more of the four sessions. Consistent with studies of those who seek out treatment for gambling (Carlbring & Smit, 2008; Carlbring et al., 2012; Petry et al., 2006), few of these gamblers became actively engaged in treatment, suggesting that expectations for lengthy interventions are unacceptable to most individuals, many of whom benefited from much less intensive treatments. Nevertheless, availability of MET+CBT did yield some long-term benefits. Perhaps only patients who felt they needed more gambling treatment attended, and those who successfully reduced gambling after only one or two sessions maintained those benefits without further treatment. These results suggest a stepped care approach to gambling intervention may be warranted. Allowing patients to choose their desired level of intervention may results in similar benefits with lower burden to clinics, therapists, and the patients themselves.
Some baseline variables were related to short-term reductions in gambling, but none predicted long term outcomes. The only predictor of long-term recovery from gambling problems was assignment to MET+CBT. These data suggest that MET+CBT appears widely applicable to substance abusing problem gamblers, regardless of demographic or substance use characteristics.
Addressing gambling did not have pronounced effects on substance use, although MET+CBT did result in a lower likelihood of any alcohol use or problems between baseline and month 5 relative to Brief Advice. Although likelihood of self-reported problems on the ASI declined in the sample as a whole over time, submission of positive samples increased over time. These data may reflect discrepancies between subjective and objective indices, or patients may have resumed drug use which they did not consider problematic. A difficulty in interpreting these results is that patients could begin this gambling intervention study at any point during a substance abuse treatment episode. Consistent with treatment recommendations, most methadone patients had long treatment histories while patients in the psychosocial outpatient clinics generally were newly enrolled. Unfortunately, we did not collect detailed information on durations of time in substance abuse treatment, but clinic and methadone status were equally represented across conditions. The greater likelihood of submitting drug positive samples over time may reflect patients dropping out of psychosocial treatment. The range of substance use disorders and varying times in treatment allow for generalization of these findings but also increased heterogeneity of outcomes, making between group differences in drug use outcomes more difficult to detect. Nevertheless, relative to Brief Advice, MET+CBT had spillover effects in reducing alcohol use and problems. Decreases in drinking with gambling treatment occur in other samples as well (Rash, Weinstock, & Petry, 2011).
A limitation of the study design is that therapist attention and expectancy effects were not controlled in the longer duration intervention relative to the briefer ones. Future studies need to evaluate the efficacy of MET+CBT relative to other types of therapy that equate for common therapeutic processes and durations. Additionally, this study found somewhat differing results depending on the gambling outcome measure; these differences reflect debates in the field regarding methods of assessing gambling behaviors and problems (Walker et al., 2006). They also suggest that multiple indices may be necessary to capture changes in gambling over time. One can gamble frequently (e.g., purchase one lottery or scratch ticket every day) and not experience problems. Wagering large amounts often relates to problems, although perceptions of large amounts can relate to personal factors such as income. Further, problems experienced from gambling are broader than purely financial ones. More research is needed to identify the most sensitive and specific indices of gambling difficulties. Completing assessments or entering a gambling intervention study may have increased awareness of gambling and instigated changes. However, assessment effects were consistent across conditions in this study, and two of the interventions yielded more pronounced reductions in some gambling outcomes, despite any general assessment effects. As noted earlier, research assistants who conducted follow-up evaluations were sometimes aware of treatment assignments, and ideally blinded interviewers would conduct all assessments.
Another limitation is that diagnoses of other psychiatric disorders were not conducted to minimize assessment burden. Comorbidity with psychiatric conditions beyond substance use disorders was likely high (Kessler et al., 2008; Petry et al., 2005) and may influence outcomes (Hodgins & el Guebaly, 2010; Hodgins, Peden, & Cassidy, 2005). Nevertheless, baseline levels of psychiatric distress were not related to clinically significant changes in gambling in this sample. In addition, DSM-IV pathological gambling was used for a gambling diagnosis. Although the DSM-5 system does not appear to alter diagnosis substantially (Petry, Blanco, Jin, & Grant, 2014; Petry, Blanco, Stinchfield, & Volberg, 2013), results may differ slightly with the new classification.
Finally, these results can only be generalized to problem gamblers who present for substance use treatment. The demographics and gambling histories of these patients were similar to those of problem gamblers identified in other substance abuse treatment settings in the US (Ledgerwood & Downey, 2002), but they differ markedly in preferred form of gambling and other characteristics from treatment-seeking gamblers (e.g., Hodgins et al., 2009; Petry et al., 2006). Problem gamblers who are not receiving substance use treatment may respond differently, and they may not demonstrate such pronounced reductions. Additional studies should evaluate interventions in other populations, such as medical clinics that serve large proportions of individuals with gambling problems (Morasco, vom Eigen, & Petry, 2006; Sullivan, McCormick, Lamont, & Penfold, 2007).
Despite limitations, this study included a sizeable sample, and it is the largest study of treatments in substance abusing problem gamblers. It applied few exclusion criteria and was conducted in multiple community substance abuse treatment clinics, enhancing generalization. The study achieved reasonable follow-up rates and employed intent-to-treat analyses, including all randomized participants and as much follow-up data as possible. Multiple therapists provided each of the three interventions, reducing the impact of any particular therapist on outcomes. Collaterals corroborated participant reports, and the two were significantly concordant.
Results from this study indicate that problem gambling dissipates over time in the majority of substance abusing problem gamblers receiving gambling interventions, but provision of MET+CBT can lead to quicker and more pronounced reductions in gambling in both the short and longer term. Nevertheless, these data also suggest that relatively few persons seeking substance abuse treatment who also have gambling problems will participate in a 4-session intervention for gambling, and the statistically significant improvements associated with this intervention are somewhat modest in nature. Practical implications are that at least a brief intervention should be provided to all substance abuse treatment patients identified with gambling problems, and a more extended version (e.g., MET+CBT) should be recommended and offered, recognizing that few will complete it. Even if patients elect not to take full advantage of the four session gambling intervention, it yielded some benefits beyond the precipitous reductions in gambling associated with the briefest interventions.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems: A review. Addiction. 1993;88:315–336. doi: 10.1111/j.1360-0443.1993.tb00820.x. [DOI] [PubMed] [Google Scholar]
- Carlbring P, Degerman N, Jonsson J, Andersson G. Internet-based treatment of pathological gambling with a 3-year follow-up. Cognitive Behaviour Therapy. 2012;41:321–334. doi: 10.1080/16506073.2012.689323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlbring P, Jonsson J, Josephson H, Forsberg L. Motivational interviewing versus cognitive behavioral group therapy in the treatment of problem and pathological gambling: A randomized controlled trial. Cognitive Behaviour Therapy. 2010;39:92–103. doi: 10.1080/16506070903190245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlbring P, Smit F. Randomized trial of internet-delivered self-help with telephone support for pathological gamblers. Journal of Consulting & Clinical Psychology. 2008;76:1090–1094. doi: 10.1037/a0013603. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Nich C, Sifry RL, Nuro KF, Frankforter TL, Ball SA, … Rounsaville BJ. A general system for evaluating therapist adherence and competence in psychotherapy research in the addictions. Drug and Alcohol Dependence. 2000;57:225–238. doi: 10.1016/s0376-8716(99)00049-6. [DOI] [PubMed] [Google Scholar]
- Cowlishaw S, Merkouris S, Chapman A, Radermacher H. Pathological and problem gambling in substance use treatment: A systematic review and meta-analysis. Journal of Substance Abuse Treatment. 2014;46:98–105. doi: 10.1016/j.jsat.2013.08.019. [DOI] [PubMed] [Google Scholar]
- Cunningham JA. Little use of treatment among problem gamblers. Psychiatric Services. 2005;56:1024–1025. doi: 10.1176/appi.ps.56.8.1024-a. [DOI] [PubMed] [Google Scholar]
- Cunningham JA, Hodgins DC, Toneatto T, Murphy M. A randomized controlled trial of a personalized feedback intervention for problem gamblers. PloS One. 2012;7:e31586. doi: 10.1371/journal.pone.0031586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowling N, Smith D, Thomas T. A comparison of individual and group cognitive-behavioural treatment for female pathological gambling. Behaviour Research and Therapy. 2007;45:2192–2202. doi: 10.1016/j.brat.2006.11.003. [DOI] [PubMed] [Google Scholar]
- Dowling N, Smith D, Thomas T. A preliminary investigation of abstinence and controlled gambling as self-selected goals of treatment for female pathological gambling. Journal of Gambling Studies. 2009;25(2):201–214. doi: 10.1007/s10899-009-9116-1. [DOI] [PubMed] [Google Scholar]
- Gerstein D, Murphy S, Toce M, Hoffmann J, Palmer A, Johnson R, … Engleman L. Gambling Impact and Behavior Study: A Report to the National Gambling Impact Study Commission. Chicago, IL: National Opinion Research Center; 1999. [Google Scholar]
- Grant JE, Donahue CB, Odlaug BL, Kim SW, Miller MJ, Petry NM. Imaginal desensitisation plus motivational interviewing for pathological gambling: Randomised controlled trial. The British Journal of Psychiatry. 2009;195:266–267. doi: 10.1192/bjp.bp.108.062414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant JE, Steinberg MA, Kim SW, Rounsaville BJ, Potenza MN. Preliminary validity and reliability testing of a structured clinical interview for pathological gambling. Psychiatry Research. 2004;128:79–88. doi: 10.1016/j.psychres.2004.05.006. [DOI] [PubMed] [Google Scholar]
- Hedeker DH. MIXREG: A Fortran program for mixed-effects linear regression models. (Computer program) Rockville, MD: NIMH Division of Services Research; 1993. [Google Scholar]
- Hodgins DC. Using NORC DSM screen for gambling problems as an outcome measure for pathological gambling: Psychometric evaluation. Addictive Behaviors. 2004;29:1685–1690. doi: 10.1016/j.addbeh.2004.03.017. [DOI] [PubMed] [Google Scholar]
- Hodgins DC, Currie SR, Currie G, Fick GH. Randomized trial of brief motivational treatments for pathological gamblers: More is not necessarily better. Journal of Consulting and Clinical Psychology. 2009;77:950–960. doi: 10.1037/a0016318. [DOI] [PubMed] [Google Scholar]
- Hodgins DC, Currie SR, el-Guebaly N. Motivational enhancement and self-help treatments for problem gambling. Journal of Consulting and Clinical Psychology. 2001;69:50–57. doi: 10.1037//0022-006x.69.1.50. [DOI] [PubMed] [Google Scholar]
- Hodgins DC, Currie SR, el-Guebaly N, Diskin KM. Does providing extended relapse prevention bibliotherapy to problem gamblers improve outcome? Journal of Gambling Studies. 2007;23:41–54. doi: 10.1007/s10899-006-9045-1. [DOI] [PubMed] [Google Scholar]
- Hodgins DC, Currie S, el-Guebaly N, Peden N. Brief motivational treatment for problem gambling: A 24-month follow-up. Psychology of Addictive Behaviors. 2004;18:293–296. doi: 10.1037/0893-164X.18.3.293. [DOI] [PubMed] [Google Scholar]
- Hodgins DC, el-Guebaly N. The influence of substance dependence and mood disorders on outcome from pathological gambling: Five-year follow-up. Journal of Gambling Studies. 2010;26:117–127. doi: 10.1007/s10899-009-9137-9. [DOI] [PubMed] [Google Scholar]
- Hodgins DC, Peden N, Cassidy E. The association between comorbidity and outcome in pathological gambling: A prospective follow-up of recent quitters. Journal of Gambling Studies. 2005;21:255–271. doi: 10.1007/s10899-005-3099-3. [DOI] [PubMed] [Google Scholar]
- Hodgins DC, Wynne H, Makarchuk K. Pathways to recovery from gambling problems: Follow-up from a general population survey. Journal of Gambling Studies. 1999;15:93–104. [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Hwang I, LaBrie R, Petukhova M, Sampson NA, Winters KC, Shaffer HJ. DSM-IV pathological gambling in the national comorbidity survey replication. Psychological Medicine. 2008;38:1351–1360. doi: 10.1017/S0033291708002900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larimer ME, Neighbors C, Lostutter TW, Whiteside U, Cronce JM, Kaysen D, Walker DD. Brief motivational feedback and cognitive behavioral interventions for prevention of disordered gambling: A randomized clinical trial. Addiction. 2012;107:1148–1158. doi: 10.1111/j.1360-0443.2011.03776.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ledgerwood DM, Downey KK. Relationship between problem gambling and substance use in a methadone maintenance population. Addictive Behaviors. 2002;27(4):483–491. doi: 10.1016/s0306-4603(01)00187-3. [DOI] [PubMed] [Google Scholar]
- Lesieur HR, Blume SB. The South Oaks Gambling Screen: A new instrument for the identification of pathological gamblers. American Journal of Psychiatry. 1987;144:1184–1188. doi: 10.1176/ajp.144.9.1184. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Cacciola J, Griffith J, McGahan P, O'Brien CP. U.S. DHHS Publication No. (ADM) 1988. Guide to the Addiction Severity Index: Background, administration, and field testing results; pp. 88–1419. [Google Scholar]
- Morasco B, vom Eigen K, Petry NM. Severity of gambling is associated with physical and emotional health in urban primary care patients. General Hospital Psychiatry. 2006;28:94–100. doi: 10.1016/j.genhosppsych.2005.09.004. [DOI] [PubMed] [Google Scholar]
- Oei TP, Raylu N, Casey LM. Effectiveness of group and individual formats of a combined motivational interviewing and cognitive behavioral treatment program for problem gambling: A randomized controlled trial. Behavioral & Cognitive Psychotherapy. 2010;38:233–238. doi: 10.1017/S1352465809990701. [DOI] [PubMed] [Google Scholar]
- Petry NM. Validity of the Addiction Severity Index in assessing gambling problems. Journal of Nervous and Mental Disease. 2003;191:399–407. doi: 10.1097/01.NMD.0000071589.20829.DB. [DOI] [PubMed] [Google Scholar]
- Petry NM. Pathological gambling: Etiology, comorbidity, and treatment. American Psychological Association; 2005. [Google Scholar]
- Petry NM. Concurrent and predictive validity of the addiction severity index in pathological gamblers. The American Journal on Addictions. 2007;16:272–282. doi: 10.1080/10550490701389849. [DOI] [PubMed] [Google Scholar]
- Petry NM, Ammerman Y, Bohl J, Doersch A, Gay H, Kadden R, … Steinberg K. Cognitive-behavioral therapy for pathological gamblers. Journal of Consulting and Clinical Psychology. 2006;74:555–567. doi: 10.1037/0022-006X.74.3.555. [DOI] [PubMed] [Google Scholar]
- Petry NM, Blanco C, Auriacombe M, Borges G, Bucholz K, Crowley TJ, … O'Brien C. An overview of and rationale for changes proposed for pathological gambling in DSM-5. Journal of Gambling Studies. 2013;30:493–502. doi: 10.1007/s10899-013-9370-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Blanco C, Jin C, Grant BF. Concordance between gambling disorder diagnoses in the DSM-IV and DSM-5: Results from the national epidemiological survey of alcohol and related disorders. Psychology of Addictive Behaviors. 2014;28(2):586–591. doi: 10.1037/a0034661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Blanco C, Stinchfield R, Volberg R. An empirical evaluation of proposed changes for gambling diagnosis in the DSM-5. Addiction. 2013;108(3):575–581. doi: 10.1111/j.1360-0443.2012.04087.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Stinson FS, Grant BF. Comorbidity of DSM-IV pathological gambling and other psychiatric disorders: Results from the national epidemiologic survey on alcohol and related conditions. The Journal of Clinical Psychiatry. 2005;66:564–574. doi: 10.4088/jcp.v66n0504. [DOI] [PubMed] [Google Scholar]
- Petry NM, Weinstock J, Ledgerwood DM, Morasco B. A randomized trial of brief interventions for problem and pathological gamblers. Journal of Consulting and Clinical Psychology. 2008;76:318–328. doi: 10.1037/0022-006X.76.2.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Weinstock J, Morasco BJ, Ledgerwood DM. Brief motivational interventions for college student problem gamblers. Addiction. 2009;104:1569–1578. doi: 10.1111/j.1360-0443.2009.02652.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rash CJ, Weinstock J, Petry NM. Drinking patterns of pathological gamblers before, during, and after gambling treatment. Psychology of Addictive Behavior. 2011;25:664–74. doi: 10.1037/a0025565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slutske WS. Natural recovery and treatment-seeking in pathological gambling: Results of two U.S. national surveys. The American Journal of Psychiatry. 2006;163:297–302. doi: 10.1176/appi.ajp.163.2.297. [DOI] [PubMed] [Google Scholar]
- Slutske WS, Jackson KM, Sher KJ. The natural history of problem gambling from age 18 to 29. Journal of Abnormal Psychology. 2003;112:263–274. doi: 10.1037/0021-843x.112.2.263. [DOI] [PubMed] [Google Scholar]
- Slutske WS, Piasecki TM, Blaszczynski A, Martin NG. Pathological gambling recovery in the absence of abstinence. Addiction. 2010;105(12):2169–2175. doi: 10.1111/j.1360-0443.2010.03080.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline Follow-back: A technique for assessing self-reported alcohol consumption. In: Litten R, Allen J, editors. Measuring Alcohol Consumption. New York: Humana Press; 1992. pp. 41–71. [Google Scholar]
- Stinchfield R. Reliability, validity, and classification accuracy of the South Oaks Gambling Screen (SOGS) Addictive Behaviors. 2002;27:1–19. doi: 10.1016/s0306-4603(00)00158-1. [DOI] [PubMed] [Google Scholar]
- Stout RL, Wirtz RW, Carbonari J, Del Boca FK. Ensuing balanced distribution of prognostic factors in treatment outcome research. Journal of Studies on Alcohol. 1994;12:70–75. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- Sullivan S, McCormick R, Lamont M, Penfold A. Problem gambling: Patients affected by their own or another’s gambling may approve of help from general practitioners. New Zealand Medical Journal. 2007;120:U2605. [PubMed] [Google Scholar]
- Toneatto T, Gunaratne M. Does the treatment of cognitive distortions improve clinical outcomes for problem gambling? Journal of Contemporary Psychotherapy. 2009;39:221–229. [Google Scholar]
- Walker M, Toneatto T, Potenza MN, Petry N, Ladouceur R, Hodgins DC, … Blaszczynski A. A framework for reporting outcomes in problem gambling treatment research: The Banff, Alberta consensus. Addiction. 2006;101:504–511. doi: 10.1111/j.1360-0443.2005.01341.x. [DOI] [PubMed] [Google Scholar]
- Welte J, Barnes G, Wieczorek W, Tidwell MC, Parker J. Alcohol and gambling pathology among U.S. adults: Prevalence, demographic patterns and comorbidity. Journal of Studies on Alcohol. 2001;62:706–712. doi: 10.15288/jsa.2001.62.706. [DOI] [PubMed] [Google Scholar]
- Weinstock J, Whelan JP, Meyers AW. Behavioral assessment of gambling: An application of the Timeline Followback Method. Psychological Assessment. 2004;16:72–80. doi: 10.1037/1040-3590.16.1.72. [DOI] [PubMed] [Google Scholar]
- Wulfert E, Hartley J, Lee M, Wang N, Franco C, Sodano R. Gambling screens: Does shortening the time frame affect their psychometric properties? Journal of Gambling Studies. 2005;21:521–536. doi: 10.1007/s10899-005-5561-7. [DOI] [PubMed] [Google Scholar]