Abstract
Neurofibromatosis type 1 (NF1) is associated with systemic vascular disease, and it can also affect intracranial vasculature in a small percentage of patients. Very rarely, NF1 may co-present with hypoplasia of the internal carotid artery (ICA). Prior reports have documented NF1 with bilateral optic gliomas and a unilateral hypoplastic internal carotid artery; however, we report a case with the aforementioned findings in addition to a right-sided lentiform mass. This case report further suggests a common congenital pathway related to neurofibromin loss of function resulting in both nerve sheath tumors and cerebrovascular anomalies.
Keywords: neurofibromatosis, optic glioma, hypoplastic internal carotid artery, lentiform mass, nerve sheath tumor, neurovascular abnormalities, intracranial vascular malformations, aplastic internal carotid artery, intracranial mass, neurofibromin
Introduction
Neurofibromin loss of function can result in systemic malignancies and vascular abnormalities [1]. Neurofibromatosis type 1 (NF1) affects one in three thousand people and can be associated with systemic vascular disease and malformations affecting the aortic, renal, and mesenteric arteries [2-3]. On the other hand, hypoplasia or aplasia of the internal carotid artery (ICA) not secondary to mass effect or compression is another very rare congenital anomaly that may lead to neurologic deficits or life threatening intracranial vascular abnormalities such as aneurysm formation [4-6].
Case series have demonstrated NF1 with non-specific cerebrovascular dysplasia in as few as two percent of patients [7-9]. Moreover, in a case series reviewing NF1 and a hypoplastic ICA, the presence of optic gliomas was found in only a third of patients [10]. Here we discuss an extremely rare case that demonstrates a hypoplastic ICA, NF1, bilateral optic gliomas, and an additional lentiform mass. Informed consent was obtained from the patient for this study.
Case presentation
Our patient is an 18-year-old female with known NF1 and bilateral optic gliomas who presented to the neurology department for evaluation of a hypoplastic left ICA demonstrated on a prior CT angiogram at an outside hospital. Given the rarity of a hypoplastic ICA in NF1 patients, workup was initiated with particular attention given to alternate etiologies such as Moyamoya syndrome. The patient had a long-standing history of headaches, chronic left-greater-than-right vision loss, intermittent vertigo, numbness, tingling, and pain. A physical exam confirmed her visual symptoms and demonstrated 4+/5 right upper extremity weakness, hyporeflexia of the left triceps reflex, and diffuse café au lait spots. The patient underwent magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) imaging of the brain (Figures 1-3).
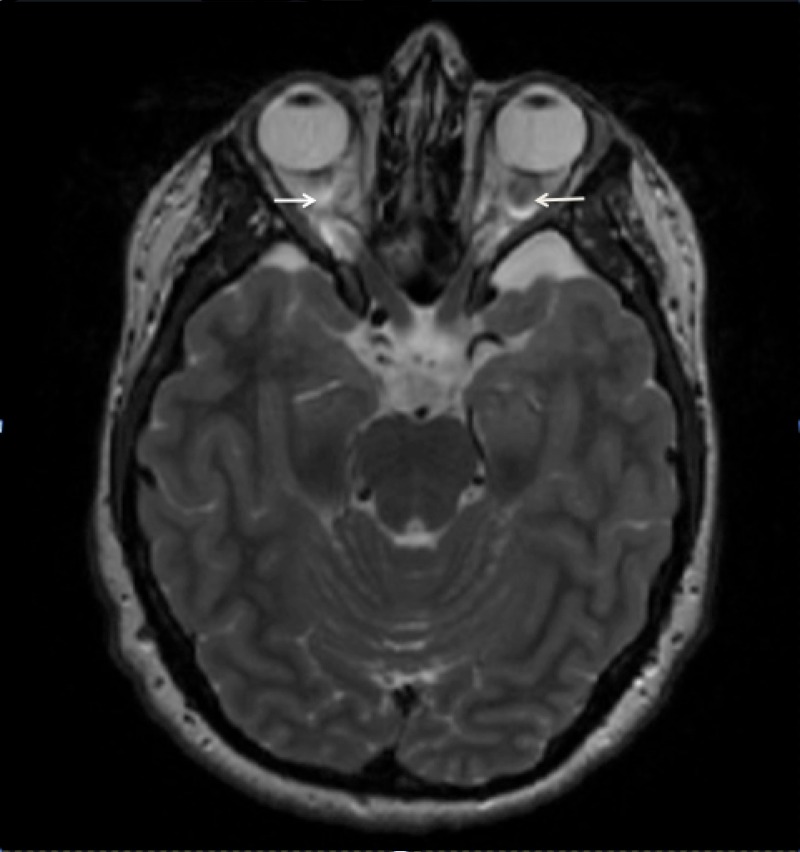
Figure 1. T2 weighted axial MRI through the suprasellar cistern.
Bilateral optic nerve enlargement consistent with optic nerve gliomas. No significant mass effect on adjacent vasculature.
Figure 3. Axial CT.
The right carotid canal and left hypoplastic carotid canal are demarcated by arrows.
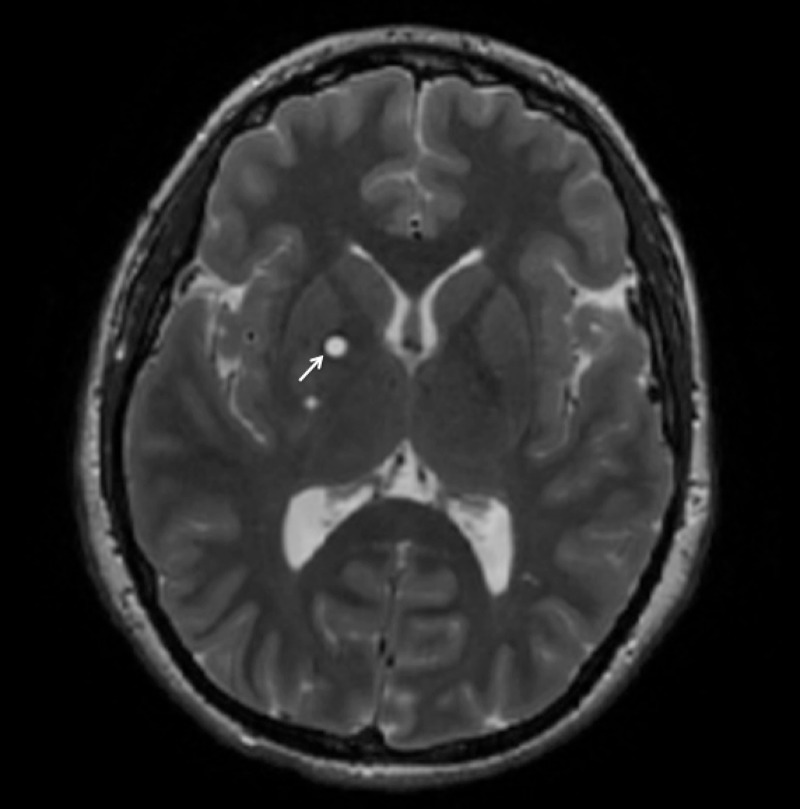
Figure 2. Axial T2 FLAIR MRI.
Hyperintense lesions within the right lentiform nucleus concerning for glioma.
The patient then underwent a diagnostic six-vessel cerebral angiogram (DCA) that demonstrated a complete left internal carotid occlusion distal to the branch of the ophthalmic artery. In addition, the entire left middle cerebral artery (MCA) and anterior cerebral artery (ACA) vascular territories were supplied by the right internal carotid via a robust anterior communicating artery (Figures 4-5).
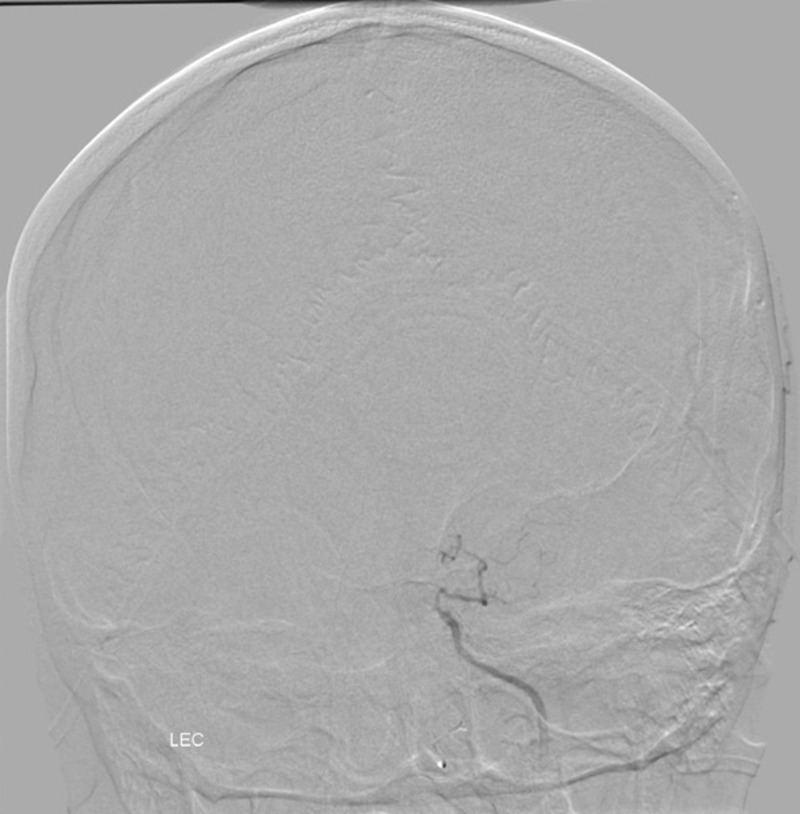
Figure 4. Posterior anterior (PA) angiogram of the anterior circulation.
Left ICA demonstrates absence of the intracranial left ICA distal to ophthalmic branch consistent with hypoplasia of the left ICA.
Figure 5. PA angiogram of the anterior circulation.
Opacification of the bilateral middle cerebral and anterior cerebral arteries via enlarged anterior communicating artery.
The findings on the DCA excluded the diagnosis of Moyamoya syndrome and further characterized the complete occlusive disease of her left carotid artery with total perfusion of her anterior circulation via the right ICA through a very robust anterior communicating artery. Moreover, a computerized tomography (CT) of her head revealed hypoplasia of the internal carotid canal suggesting a long-standing congenital lesion. The additional lentiform mass was radiographically determined as not exerting mass effect and warranted scheduled surveillance imaging without further intervention. The patient has since been conservatively followed by the neurology service.
Discussion
This case demonstrates the presence of an intracranial mass in addition to a hypoplastic ICA and optic gliomas in an NF1 patient. This constellation of findings is extremely rare and further demonstrates a clinical example in which loss of function in neurofibromin results in both intracranial and systemic nerve sheath tumors and congenital vascular anomalies. This clinical presentation highlights the importance of further understanding the genetic pathways leading to neurologic tumors and vascular abnormalities. Moreover, this case suggests that further screening for intracranial or congenital malformations in the setting of neurofibromatosis is warranted to optimize management of vascular risk factors to minimize vascular neurologic injury.
Conclusions
Although neurofibromatosis is exceedingly rare, this disease can co-present with vascular manifestations, and this case report suggests the workup of congenital and acquired intracranial vascular disease for this patient population.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
issued approval Informed consent was obtained from the patient for this study.
References
- 1.Neurofibromin is a novel regulator of RAS-induced signals in primary vascular smooth muscle cells. Li F, Munchhof AM, White HA, et al. http://www.ncbi.nlm.nih.gov/pubmed/16644864. Hum Mol Genet. 2006;15:1921–1930. doi: 10.1093/hmg/ddl114. [DOI] [PubMed] [Google Scholar]
- 2.Vascular abnormalities in patients with neurofibromatosis syndrome type I: clinical spectrum, management, and results. Oderich GS, Sullivan TM, Bower TC, et al. http://www.ncbi.nlm.nih.gov/pubmed/17681709. J Vasc Surg. 2007;46:475–484. doi: 10.1016/j.jvs.2007.03.055. [DOI] [PubMed] [Google Scholar]
- 3.Noninvasive evaluation of arterial abnormalities in young patients with neurofibromatosis type 1. Tedesco MA, Ratti G, Di Salvo G, et al. http://www.ncbi.nlm.nih.gov/pubmed/10999614. Angiology. 2000;51:733–741. doi: 10.1177/000331970005100905. [DOI] [PubMed] [Google Scholar]
- 4.Congenital absence or hypoplasia of the carotid artery: radioclinical issues. Taşar M, Yetişer S, Taşar A, Uğurel S, Gönül E, Sağlam M. http://www.ncbi.nlm.nih.gov/pubmed/15334399. Am J Otolaryngol. 2004;25:339–349. doi: 10.1016/j.amjoto.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 5.Aplasia of the internal carotid artery. Lee JH, Oh CW, Lee SH, Han DH. http://www.ncbi.nlm.nih.gov/pubmed/12601459. Acta Neurochir (Wien) 2003;145:117–125. doi: 10.1007/s00701-002-1046-y. [DOI] [PubMed] [Google Scholar]
- 6.Major congenital anomalies of the internal carotid artery: agenesis, aplasia and hypoplasia. Claros P, Bandos R, Gilea I, Claros A, Capdevila A, Garcia Rodriguez J, Claros A. http://www.ncbi.nlm.nih.gov/pubmed/10428407. Int J Pediatr Otorhinolaryngol. 1999;49:69–76. doi: 10.1016/s0165-5876(99)00012-9. [DOI] [PubMed] [Google Scholar]
- 7.Vascular neurofibromatosis affecting the internal carotid artery: a case report. Steel TR, Bentivoglio PB, Garrick R. http://www.ncbi.nlm.nih.gov/pubmed/7917100. Br J Neurosurg. 1994;8:233–237. doi: 10.3109/02688699409027975. [DOI] [PubMed] [Google Scholar]
- 8.Ocular ischaemia with hypoplasia of the internal carotid artery associated with neurofibromatosis type 1. Shuto T, Yamamoto I. http://www.ncbi.nlm.nih.gov/pubmed/10819269. Acta Neurochir (Wien) 2000;142:353–354. doi: 10.1007/s007010050047. [DOI] [PubMed] [Google Scholar]
- 9.Cerebrovascular dysplasia in neurofibromatosis type 1. Cairns AG, North KN. http://www.ncbi.nlm.nih.gov/pubmed/18469031. J Neurol Neurosurg Psychiatry. 2008;79:1165–1170. doi: 10.1136/jnnp.2007.136457. [DOI] [PubMed] [Google Scholar]
- 10.Neurofibromatosis and intracranial arterial occlusive disease. Tomsick TA, Lukin RR, Chambers AA, Benton C. Neuroradiology. 1976;11:229–234. doi: 10.1007/BF00328378. [DOI] [PubMed] [Google Scholar]