Abstract
AIM
To examine patient knowledge and factors influencing knowledge about pregnancy in British women with inflammatory bowel disease (IBD).
METHODS
This is a post hoc analysis of a study of female members of Crohn’s and Colitis United Kingdom, aged 18-45 years who were sent an online questionnaire recording patient demographics, education, employment, marital status, and disease characteristics. Disease related pregnancy knowledge was recorded using Crohn’s and colitis pregnancy knowledge score (CCPKnow).
RESULTS
Of 1324 responders, 776 (59%) suffered from Crohn’s disease, 496 (38%) from ulcerative colitis and 52 (4%) from IBD-uncategorised. CCPKnow scores were poor (0-7) in 50.8%, adequate (8-10) in 23.6%, good (11-13) in 17.7% and very good (≥ 14) in 7.8%. Multiple linear regression analysis revealed that higher CCPKnow scores were independently associated with higher educational achievement (P < 0.001), younger age at diagnosis (P = 0.003) and having consulted a health care professional about pregnancy and IBD (P = 0.001).
CONCLUSION
Knowledge was poor in 50%. Speaking with health-care professionals was a modifiable factor associated with better knowledge. This illustrates the importance of disease related pregnancy education
Keywords: Inflammatory bowel disease, Ulcerative colitis, Crohn’s disease, Patient knowledge, Pregnancy, Reproduction
Core tip: Inflammatory bowel disease (IBD) affects many women of childbearing age and knowledge of IBD and pregnancy related issues, is key to enable patients to make informed decisions. In this large study of British women with IBD, knowledge was poor in over half of participants. Speaking with health care professionals about pregnancy was identified as a modifiable factor associated with better knowledge. This study illustrates first the importance of disease related education for female patients with IBD and second highlights that health professionals should seek opportunities to educate patients about pregnancy and IBD early in their disease course.
INTRODUCTION
Inflammatory bowel disease (IBD) is a chronic disease and includes ulcerative colitis (UC), Crohn’s disease (CD) and IBD-unclassified (IBD-U). Severity of disease can differ and the impact upon the quality of life for individual patients can vary dramatically, with one study reporting that up to 48% of patients feel IBD symptoms significantly affect their lives even whilst in remission[1]. As the age of onset for IBD is usually around the reproductive years, questions about having children and being pregnant are common for many women who have IBD[2]. Decision-making regarding IBD and pregnancy is complex and requires weighing the benefits and risks of treatments.
Fertility in female patients with IBD is generally equal or only marginally reduced when compared to the general population[3-6]. Nevertheless, 42.7% of women with IBD fear infertility[7] and studies have shown that voluntary childlessness is more common in women with IBD than the general population[8].
Recently, the role of IBD and pregnancy related patient knowledge has been scrutinized. The Crohn’s and colitis pregnancy knowledge score (CCPKnow) is a validated self-report tool that has been developed for use in clinical practice as well as research[9]. Its use has shown that whilst women with children are more likely to have higher CCPKnow scores[9,10], those who are voluntarily childless tend to have lower scores[11]. Importantly, poor knowledge has also been correlated with views about IBD medication that contradict medical guidelines[12]. Making uninformed choices on IBD medication could lead to disease flares and potentially adverse pregnancy outcomes. Good disease pregnancy related knowledge is therefore key to women having a safe and successful pregnancy.
Average CCPknow scores have been demonstrated to be between 5.4-7.47, with between 44.8%-65% scoring “poor” (CCPKnow < 8) in British and Australian cohorts[9,11,13]. Previous studies have revealed some of the factors associated with higher CCPKnow scores including Caucasian ethnicity, higher income, having a partner, being a member of Crohn’s and Colitis Patient Association and longer disease duration[9]. However, these studies sampled a relatively small cohort of patients (< 250) and showed limited evidence into what modifiable factors might affect knowledge levels. The extent of IBD and pregnancy related patient knowledge in British women has so far not been investigated.
In light of the established correlation being between IBD patients’ level of knowledge on pregnancy matters and their subsequent decisions on family planning one can highlight the importance of identifying factors affecting women’s knowledge. The aim of this study is to ascertain the extent of low levels of knowledge amongst a sample of British women and to determine which factors, particularly which modifiable factors, influence knowledge of IBD and pregnancy.
MATERIALS AND METHODS
This study is a post hoc analysis of a recently published paper examining factors affecting voluntary childlessness in IBD[11]. We contacted all 4300 female members of Crohn’s and Colitis United Kingdom (the national charity providing support and patient education in addition to funding research for patients affected by IBD in the United Kingdom) aged 18-45 years by email. These women were then invited to complete our online questionnaire using an online survey system (Bristol Online Surveys, United Kingdom). Each received two invitation reminders and submission of the completed questionnaire was taken as informed consent.
The study collected self reported data on patients’ demographics, educational achievements, employment status, marital status and sexual orientation. Furthermore, questions related to disease characteristics consisted of diagnosis, duration of illness, and number of hospitalisations, surgical resections, and current as well as previous exposure to IBD medication. For the purpose of this post-hoc analysis each participant’s child status was analysed as a dichotomous variable. As such, child status group 1 consisted of women who either had children after diagnosis of IBD or those who were planning to have children at some stage after diagnosis. Child status group 2 consisted of women who only had children prior to diagnosis, those who were experiencing infertility and those who decided to remain voluntarily childless.
The validated CCPKnow was used to assess disease-related pregnancy knowledge[9]. This 17-item self-report questionnaire classifies knowledge as poor (0-7), adequate (8-10), good (11-13), and very good (14-17).
Data analysis was performed using SPSS 22.0 (IBM, Armonk, United States). We conducted ANOVAs and student t-tests for continuous data and chi-square tests for categorical data at a P-value < 0.05. To determine independent predictors of CCPKnow independence of variables was determined by entering any significant variables from the univariate analysis into multiple linear regression analysis. The study was approved by the National Research Ethics Service Committee North West - Preston (14/NW/1391).
RESULTS
A total of 1324 women completed the survey (response rate 31%) with a mean age of 33 years. Of these 1009 (76.2%) were in a long-term relationship, 259 (19.6%) were single and 44 (3.3%) were separated/divorced. Over half of patients had university level education with 577 (43.6%) having a bachelors degree and 204 (15.4%) having a masters or doctorate. Over three quarters were in employment, with 697 (52.6%) in full time employment, 337 (25.5%) in part time employment and only 80 (6%) unemployed. For further details on demographic variables please see Table 1.
Table 1.
Patient demographics n (%)
| Patient demographics | Value |
| Age (yr) | Mean 33.5 (18-45) |
| Ethnicity | |
| White | 1258 (95.0) |
| Asian | 34 (2.6) |
| Black | 6 (0.5) |
| Other | 26 (1.9) |
| Highest educational achievement | |
| Secondary school | 157 (11.9) |
| Apprenticeship/guild/NVQ | 386 (29.1) |
| Bachelor | 577 (43.6) |
| Master/PhD | 204 (15.4) |
| Employment status | |
| Full time employment | 697 (52.6) |
| Part time employment | 337 (25.5) |
| Full time education | 102 (7.7) |
| Unemployed | 80 (6.0) |
| House person | 108 (8.2) |
| Relationship status | |
| Single | 259 (19.6) |
| Separated/divorced | 44 (3.3) |
| Long term relationship/married/civil partnership | 1009 (76.2) |
| Other | 12 (0.9) |
| Same sex relationship | |
| Yes | 66 (5.0) |
| No | 1250 (94.4) |
| Chose not to answer | 8 (0.6) |
Of the 1324 responders 776 (59%) suffered from CD, 496 (38%) from UC and 52 (4%) from IBD-U. Ninehundredtwentythree (69.3%) had been admitted to hospital due to their disease and 437 (32.3%) had undergone bowel resection surgery. Fourhundredseventysix (35.9%) were either currently taking or had previously been on biologic medications, 965 (72.8%) for immunomodulators and 1136 (85.8%) for 5-aminosalicylic acid medication with current or previous steroid use 1123 (84.8%). Detailed information regarding disease characteristics and medication history is available in Table 2.
Table 2.
Disease and treatment characteristics n (%)
| Characteristics | Value |
| Diagnosis | |
| CD | 776 (58.6) |
| UC | 496 (37.5) |
| IBD-U | 48 (3.6) |
| Unknown | 4 (0.3) |
| Age at diagnosis | Mean 25 yr |
| Median 24 yr | |
| Duration of disease | Mean 8.5 yr |
| Median 7 yr | |
| Hospital admissions | |
| Yes | 923 (69.3) |
| No | 401 (30.3) |
| Median 2 admissions | |
| Bowel resection surgery | |
| Yes | 437 (32.3) |
| No | 897 (67.7) |
| Median 2 resections | |
| 5-ASA medication | |
| Current | 615 (46.4) |
| Previous | 521 (39.4) |
| Never | 188 (14.2) |
| Corticosteroids | |
| Current | 175 (13.2) |
| Previous | 948 (71.6) |
| Never | 201 (15.2) |
| Immunomodulators | |
| Current | 597 (45.1) |
| Previous | 368 (27.7) |
| Never | 359 (27.2) |
| Anti-TNF agents | |
| Current | 280 (21.1) |
| Previous | 196 (14.8) |
| Never | 848 (64.1) |
CD: Crohn’s disease; IBD-U: Inflammatory bowel disease-unclassified; UC: Ulcerative colitis; TNF: Tumor necrosis factor.
CCPKnow scores were poor (0-7) in 673 participants (50.8%), adequate (8-10) in 313 participants (23.6%), good (11-13) in 235 participants (17.7%) and very good (≥ 14) in 103 participants (7.8%). Higher CCPKnow scores were associated with higher educational achievement, particularly postgraduate achievements vs high school achievements (Masters/PhD 8.67 vs Secondary school degree 5.99, P < 0.001). Working full time and being in a long-term relationship was respectively associated with better scores compared to being unemployed and being single (full time employment 7.18 vs unemployed 6.12, P = 0.03; long-term relationship 7.60 vs single 6.26, P < 0.001). Having children after being diagnosed with IBD or planning to have children was associated (group 1, CCPKnow = 7.71) with significantly better CCPKnow scores than having children prior to diagnosis, being infertile or planning to remain childless (group 2, CCPKnow = 7.05, P = 0.007). Patients with CD compared to UC patients, as well as (7.51 vs UC 6.97, P = 0.026) patients with markers of more severe disease (hospital admission 7.59 vs none 6.66, P < 0.001; surgery 7.71 vs none 7.12, P = 0.018; current biological therapy 8.30 vs none 7.05, P < 0.001) had higher knowledge scores. Ethnicity and same sex relationships had no influence on CCPKnow scores. We found significant but modest negative correlations between age and CCPKnow (Pearson correlation -0.131, P < 0.001) and between age at diagnosis and CCPKnow (Pearson correlation -0.212, P < 0.001). Participants of younger age and participants with younger age at diagnosis had better CCPKnow scores. See Table 3 for further details regarding CCPKnow scores.
Table 3.
Patient demographics, disease characteristics and impact of speaking to healthcare professionals on Crohn’s and colitis pregnancy knowledge score
| Factor | Groups | CCPKnow score | Significance |
| Age | N/A | Pearson correlation -0.131 | P < 0.001 |
| Age at diagnosis | N/A | Pearson correlation -0.212 | P < 0.001 |
| Ethnicity | White | 7.32 | P = 0.773 |
| Mixed | 8.00 | ||
| Asian | 6.59 | ||
| Black | 6.33 | ||
| Other | 7.43 | ||
| Education | Secondary school | 5.99 | P < 0.001 |
| NVQ/diploma | 6.08 | ||
| Bachelors degree | 8.02 | ||
| Masters/PhD | 8.67 | ||
| Relationship status | Single | 6.26 | P < 0.001 |
| Separated/divorced | 6.82 | ||
| Long term relationship | 7.60 | ||
| Not stated | 7.67 | ||
| Employment status | Full-time | 7.18 | P = 0.30 |
| Part-time | 7.73 | ||
| Full-time education | 7.46 | ||
| Unemployed | 6.12 | ||
| House person | 7.59 | ||
| Same-sex relationship | Yes | 6.71 | P = 0.451 |
| No | 7.35 | ||
| Chose not to answer | 6.63 | ||
| Diagnosis | CD | 7.51 | P = 0.051 |
| UC | 6.97 | ||
| IBD-U | 7.85 | ||
| Unknown | 4.25 | ||
| Children | Group 1 | 7.71 | P = 0.007 |
| Group 2 | 7.05 | ||
| Partner with IBD | Yes | 8.64 | P = 0.241 |
| No | 7.30 | ||
| Hospital admissions | Admission | 7.59 | P < 0.001 |
| None | 6.66 | ||
| Resection surgery | Yes | 7.71 | P = 0.018 |
| No | 7.12 | ||
| Current 5-ASA prescription | Yes | 7.06 | P = 0.048 |
| No | 7.53 | ||
| Current immunomodulatory | Yes | 7.67 | P = 0.006 |
| prescription | No | 7.02 | |
| Current anti-TNF | Yes | 8.30 | P < 0.0001 |
| prescription | No | 7.05 | |
| Spoken to HCP | Yes | 8.75 | P < 0.001 |
| No | 5.82 | ||
| Spoken to GP | Yes | 8.44 | P < 0.001 |
| No | 6.98 | ||
| Spoken to gastroenterologist | Yes | 9.18 | P < 0.001 |
| No | 6.25 | ||
| Spoken to IBD nurse | Yes | 9.27 | P < 0.001 |
| No | 6.83 |
CD: Crohn’s disease; IBD-U: Inflammatory bowel disease-unclassified; UC: Ulcerative colitis.
Speaking to health care professionals about IBD and pregnancy, was also associated with better CCPKnow scores (spoken to a healthcare professional 8.75 vs not 5.82, P < 0.001). This significant difference persisted even when data was divided into specific types of healthcare professionals. Thus, talking to any healthcare professional significantly correlated with higher knowledge (Gastroenterologist 9.18 vs no 6.25, P < 0.001), (GP 8.44 vs no 6.98, P < 0.001), (Specialist IBD nurse 9.27 vs 6.83, P < 0.001; see Figure 1).
Figure 1.
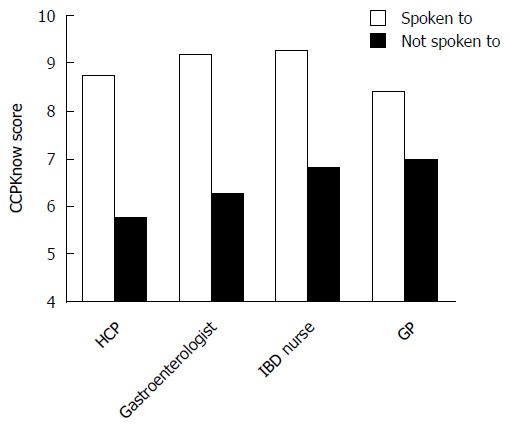
Demonstrates effect of talking to healthcare professionals on Crohn’s and colitis pregnancy knowledge scores.
Multiple linear regression analysis revealed that university level education (β = 0.292, P < 0.0001), having spoken to a health care professional (β = 0.317, P < 0.0001) and younger age at diagnosis (increasing age β = -0.274, P = 0.003) were independently associated with higher CCPKnow scores (Table 4).
Table 4.
Multiple linear regression analysis
| Factors | Beta-coefficient | Significance |
| Current 5-ASA (yes/no) | -0.490 | P = 0.603 |
| Current immunomodulators (yes/no) | -0.380 | P = 0.663 |
| Current biologics (yes/no) | 0.111 | P = 0.201 |
| Educational achievement (university/no university) | 0.292 | P = 0.001 |
| Work status (employed/unemployed) | -0.075 | P = 0.369 |
| Martial status (relationship/single) | 0.120 | P = 0.147 |
| Child status (group 1/group 2) | -0.142 | P = 0.157 |
| Diagnosis (CD/UC) | 0.090 | P = 0.336 |
| Surgery (yes/no) | -0.084 | P = 0.426 |
| Hospital admission (yes/no) | 0.038 | P = 0.676 |
| Spoken to HCP (yes/no) | -0.317 | P < 0.0001 |
| Age | -0.211 | P = 0.053 |
| Age at diagnosis | -0.274 | P = 0.003 |
DISCUSSION
The importance of IBD and pregnancy related patient knowledge (as measured by CCPKnow) has been demonstrated in a number of key studies over the last 5 years. As discussed, poorer patient knowledge has been associated with inaccurate opinions about medications, which if acted upon could increase the risk of adverse IBD and potentially pregnancy outcomes[12]. Importantly, poor IBD and pregnancy related patient knowledge is also associated with voluntary childlessness[10,11]. Studies examining CCPKnow have so far reported on medium size cohorts only and data from the United Kingdom have previously been lacking. This is the largest study of CCPKnow so far and the first to study a cohort of British women with IBD. We have demonstrated that knowledge was poor in over half of patients.
While the number of studies examining IBD related pregnancy knowledge is still limited, the relationship between general patient knowledge in IBD patients and their physical and mental health outcomes has been investigated in a number of studies. Poor general IBD knowledge has been linked to patients having less adaptive coping strategies[14]. It has also been hypothesised that better knowledge of general IBD issues might be associated with fewer disease complications, yet, Eaden et al[15] found no significant difference in knowledge between those who developed colorectal cancer as a complication of IBD and those patients who did not. However, as they discuss, their results may be skewed by the theory that having colorectal cancer itself may increase knowledge late in the disease course and perhaps comparing CCPKnow scores between patients who take up screening colonoscopies and those who do not would have demonstrated a difference.
Interestingly, better IBD knowledge has not always been associated with positive patient outcomes. Selinger et al[16] showed that better knowledge was associated with higher anxiety levels. Whilst it was not clear whether this was because more anxious patients sought out more knowledge, it is worth bearing in mind that by educating patients, we might potentially cause anxiety.
It is important to examine potential factors associated with poor IBD related patient knowledge. Such factors may help identify those patients most in need of disease education, increase our understanding how patient knowledge is formed and in turn establish which interventions show potential to improve knowledge for women with IBD. Our study demonstrates that non-modifiable factors including education, employment and being in a relationship had a positive influence on CCPKnow score. It is not surprising that higher educational achievement was an independent predictor of higher CCPKnow scores and that pregnancy related knowledge is more relevant for women in a relationship compared to single women. This has been supported by previous studies[9]. Patients with CD and higher disease burden also had better knowledge. While the exact reason for this cannot be determined from our data, the increased contact with healthcare professionals associated with more severe disease may have led to increased knowledge. Patients with more severe disease may also have a vested interest in knowing more, as it is likely that it will take more personal and professional effort to control their symptoms than someone with mild disease.
Not surprisingly having children after being diagnosed with IBD or planning to have children was associated with better CCPKnow scores. Some of the effects are likely related to the information provided during pregnancy care or sought out by the patients in the process of considering pregnancy. The effects of disease type, severity and child status on CCPKnow scores disappear on regression analysis suggesting that the most important factors influencing CCPKnow relate to general education achievement, age at diagnosis and having spoken to health care professionals. Child status was not an independent predictor of CCPKnow scores as there were clear connections between child status and age at diagnosis (older women were less likely to have children post diagnosis).
Speaking with health care professionals about pregnancy was identified as a strong and independent modifiable factor associated with better knowledge. Optimistically, perhaps this is largely due to the education patients receive during each consultation, however it is worth considering that more knowledgeable patients may also demonstrate better attendance or seek more contacts with professionals. Indeed a single education seminar can improve CCPKnow score significantly[13]. It is likely that pregnancy related IBD education can have positive effects on child planning, maternal and foetal outcomes as recently demonstrated in a Dutch study[17]. Patients exposed to pre-conceptual counselling had better outcomes than those without such counselling[17].
The positive contribution of patient education on clinical outcomes has been clearly demonstrated in other diseases. A study of an educational intervention for patients with diabetes showed not only increased knowledge scores, but also improved HbA1c levels and improved self-care and dietary practice[18]. Similar results have been demonstrated following a patient education intervention for asthmatics; as knowledge increased, antibiotic use, steroid use and unplanned visits to the doctor all reduced[19]. However, whilst patient education programmes almost universally show better knowledge levels, a study by Waters et al[20] was grossly underpowered and hence failed to show that an education programme for IBD patients influences medication adherence or quality of life.
Our study has a number of strength and weaknesses. This large sample of British women with IBD has a similar distribution of disease compared to other UK IBD cohorts; however more women were in long-term relationships and had university level education than in the United Kingdom adult population[21,22]. As we have shown, higher educational level equates with higher CCPKnow scores, it is likely that the study samples’ CCPKnow scores are actually a slight overestimation rather than underestimation compared to the general IBD population.
There are several limitations to this study. Firstly, all patients are members of Crohn’s and Colitis United Kingdom, and membership has been shown to increase knowledge and specifically CCPKnow scores[9]. We may have, therefore, overestimated CCPKnow scores somewhat. However, whilst this makes it likely that all studied patients had higher knowledge levels than found in non-members, our results showing differences in knowledge level still remain valid as we compared patients like for like and analysis focussed on differences influenced by other patient and disease characteristics.
Additionally, data collected regarding disease characteristics was self-reported and the anonymous study design did not allow for independent verification of such self reported data.
In conclusion we have demonstrated poor knowledge pregnancy related IBD patient knowledge in over half of this cohort. The positive impact speaking to a healthcare professional has on CCPKnow score is highly significant. This study therefore illustrates the importance of disease related education for female patients with IBD. Health professionals, of any vocation, should seek opportunities to educate women of reproductive age about pregnancy and IBD early in their disease course in an effort to try reduce voluntary childlessness due to limited knowledge and/or incorrect assumptions and improve maternal and foetal outcomes.
COMMENTS
Background
Inflammatory bowel disease (IBD) affects many women of childbearing age and knowledge of IBD and pregnancy related issues, is key to enable patients to make informed decisions. This study examined knowledge and factors influencing knowledge about pregnancy in British women with IBD.
Research frontiers
The effects of patient knowledge on decision making regarding pregnancy, adherence to medical treatment during pregnancy and on foetal and maternal outcomes are all being studied currently. It is likely that patient knowledge plays a vital role in all of them.
Innovations and breakthroughs
This study demonstrates for the first time in a very large study that knowledge is poor in 50% of patients. The study has shown that speaking with health care professionals is associated with improved knowledge.
Applications
Women with IBD should be educated about pregnancy related issues early in their disease course to avoid voluntary childlessness. Pre-conceptual counselling should be available for women with IBD during their reproductive years.
Terminology
IBD are chronic inflammatory bowel diseases comprising Crohn’s disease and ulcerative colitis.
Peer-review
The present manuscript reports the results of online survey regarding disease-related pregnancy knowledge in a relatively large sample of women with IBD from across the United Kingdom. They concluded disease-related education is important and health care professional should try to educate patients earlier. The manuscript is interesting and well written. Study methods and conclusion is clear. It will be helpful for readers.
Footnotes
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
Institutional review board statement: The study was approved by the National Research Ethics Service Committee North West - Preston (14/NW/1391).
Informed consent statement: Patients provided informed consent by completing the anonymous online questionnaire.
Conflict-of-interest statement: Selinger CP has received unrestricted research grants from Warner Chilcott, and Abbvie, has provided consultancy to Warner Chilcott, Dr Falk, Abbvie and Takeda, and had speaker arrangements with Warner Chilcott, Dr Falk, Abbvie, MSD and Takeda. The other authors report no relevant conflict of interest.
Data sharing statement: Data are available on request from the lead author.
Peer-review started: June 17, 2016
First decision: July 29, 2016
Article in press: August 30, 2016
P- Reviewer: Cho YS, Doherty GA, Ingle SB S- Editor: Gong ZM L- Editor: A E- Editor: Wang CH
References
- 1.Lönnfors S, Vermeire S, Greco M, Hommes D, Bell C, Avedano L. IBD and health-related quality of life -- discovering the true impact. J Crohns Colitis. 2014;8:1281–1286. doi: 10.1016/j.crohns.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 2.van der Woude CJ, Ardizzone S, Bengtson MB, Fiorino G, Fraser G, Katsanos K, Kolacek S, Juillerat P, Mulders AG, Pedersen N, et al. The second European evidenced-based consensus on reproduction and pregnancy in inflammatory bowel disease. J Crohns Colitis. 2015;9:107–124. doi: 10.1093/ecco-jcc/jju006. [DOI] [PubMed] [Google Scholar]
- 3.Dubinsky M, Abraham B, Mahadevan U. Management of the pregnant IBD patient. Inflamm Bowel Dis. 2008;14:1736–1750. doi: 10.1002/ibd.20532. [DOI] [PubMed] [Google Scholar]
- 4.Hudson M, Flett G, Sinclair TS, Brunt PW, Templeton A, Mowat NA. Fertility and pregnancy in inflammatory bowel disease. Int J Gynaecol Obstet. 1997;58:229–237. doi: 10.1016/s0020-7292(97)00088-x. [DOI] [PubMed] [Google Scholar]
- 5.Mayberry JF, Weterman IT. European survey of fertility and pregnancy in women with Crohn’s disease: a case control study by European collaborative group. Gut. 1986;27:821–825. doi: 10.1136/gut.27.7.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khosla R, Willoughby CP, Jewell DP. Crohn’s disease and pregnancy. Gut. 1984;25:52–56. doi: 10.1136/gut.25.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mountifield R, Bampton P, Prosser R, Muller K, Andrews JM. Fear and fertility in inflammatory bowel disease: a mismatch of perception and reality affects family planning decisions. Inflamm Bowel Dis. 2009;15:720–725. doi: 10.1002/ibd.20839. [DOI] [PubMed] [Google Scholar]
- 8.Marri SR, Ahn C, Buchman AL. Voluntary childlessness is increased in women with inflammatory bowel disease. Inflamm Bowel Dis. 2007;13:591–599. doi: 10.1002/ibd.20082. [DOI] [PubMed] [Google Scholar]
- 9.Selinger CP, Eaden J, Selby W, Jones DB, Katelaris P, Chapman G, McDonald C, McLaughlin J, Leong RW, Lal S. Patients’ knowledge of pregnancy-related issues in inflammatory bowel disease and validation of a novel assessment tool (‘CCPKnow’) Aliment Pharmacol Ther. 2012;36:57–63. doi: 10.1111/j.1365-2036.2012.05130.x. [DOI] [PubMed] [Google Scholar]
- 10.Huang VW, Chang HJ, Kroeker KI, Goodman KJ, Hegadoren KM, Dieleman LA, Fedorak RN. Does the level of reproductive knowledge specific to inflammatory bowel disease predict childlessness among women with inflammatory bowel disease? Can J Gastroenterol Hepatol. 2015;29:95–103. doi: 10.1155/2015/715354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Selinger CP, Ghorayeb J, Madill A. What Factors Might Drive Voluntary Childlessness (VC) in Women with IBD? Does IBD-specific Pregnancy-related Knowledge Matter? J Crohns Colitis. 2016 doi: 10.1093/ecco-jcc/jjw078. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 12.Selinger CP, Eaden J, Selby W, Jones DB, Katelaris P, Chapman G, McDondald C, McLaughlin J, Leong RW, Lal S. Inflammatory bowel disease and pregnancy: lack of knowledge is associated with negative views. J Crohns Colitis. 2013;7:e206–e213. doi: 10.1016/j.crohns.2012.09.010. [DOI] [PubMed] [Google Scholar]
- 13.Mountifield R, Andrews JM, Bampton P. It IS worth the effort: Patient knowledge of reproductive aspects of inflammatory bowel disease improves dramatically after a single group education session. J Crohns Colitis. 2014;8:796–801. doi: 10.1016/j.crohns.2013.12.019. [DOI] [PubMed] [Google Scholar]
- 14.Moradkhani A, Kerwin L, Dudley-Brown S, Tabibian JH. Disease-specific knowledge, coping, and adherence in patients with inflammatory bowel disease. Dig Dis Sci. 2011;56:2972–2977. doi: 10.1007/s10620-011-1714-y. [DOI] [PubMed] [Google Scholar]
- 15.Eaden JA, Abrams K, Mayberry JF. Does patient knowledge affect the colorectal cancer risk in ulcerative colitis? Postgrad Med J. 2002;78:615–618. doi: 10.1136/pmj.78.924.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Selinger CP, Lal S, Eaden J, Jones DB, Katelaris P, Chapman G, McDonald C, Leong RW, McLaughlin J. Better disease specific patient knowledge is associated with greater anxiety in inflammatory bowel disease. J Crohns Colitis. 2013;7:e214–e218. doi: 10.1016/j.crohns.2012.09.014. [DOI] [PubMed] [Google Scholar]
- 17.de Lima A, Zelinkova Z, van der Ent C, Steegers EA, van der Woude CJ. Tailored anti-TNF therapy during pregnancy in patients with IBD: maternal and fetal safety. Gut. 2016;65:1261–1268. doi: 10.1136/gutjnl-2015-309321. [DOI] [PubMed] [Google Scholar]
- 18.Tan AS, Yong LS, Wan S, Wong ML. Patient education in the management of diabetes mellitus. Singapore Med J. 1997;38:156–160. [PubMed] [Google Scholar]
- 19.Boulet LP, Boulay MÈ, Gauthier G, Battisti L, Chabot V, Beauchesne MF, Villeneuve D, Côté P. Benefits of an asthma education program provided at primary care sites on asthma outcomes. Respir Med. 2015;109:991–1000. doi: 10.1016/j.rmed.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 20.Waters BM, Jensen L, Fedorak RN. Effects of formal education for patients with inflammatory bowel disease: a randomized controlled trial. Can J Gastroenterol. 2005;19:235–244. doi: 10.1155/2005/250504. [DOI] [PubMed] [Google Scholar]
- 21.Office for National Statistics. 2015. Population Estimates by Marital Status and Living Arrangements – England and Wales, 2002 to 2014, London, UK. [Online] Available from: http://www.ons.gov.uk. [Google Scholar]
- 22.Office for National Statistics. 2014. 2011 Census Analysis: Local Area Analysis of Qualifications Across England and Wales Release London, UK. [Online] Available from: http://www.ons.gov.uk. [Google Scholar]


