Abstract
A pure leiomyoma of the prostate is a rare tumor. Less than 30 cases about prostatic leiomyoma have been reported. Pathologic anatomy examination is the only medium for definitive diagnosis and is important to rule out malignancies such as leiomyosarcoma. We describe an accidental finding of a tumor in the right prostate lobe of a 54 year old man, who was diagnosed with prostatic leiomyoma and treated with open radical prostatectomy.
Keywords: Leiomyoma, Prostate, Radical prostatectomy
A 54-year old man presented at the office for a routine check-up since his father had recently been diagnosed with prostate cancer. The patient had no medical history and did not take any medications. He had little to no lower urinary tract symptoms.
Serum PSA level was within normal ranges (0.9 μg/l). Urinalysis revealed no abnormalities.
On digital rectal examination an enlarged, atypical right prostate lobe was palpated. Transrectal ultrasonography confirmed a suspicious, hypervascularized mass located in the right prostate lobe (Fig. 1).
Figure 1.

Transrectal ultrasonography shows an atypical mass located in the right prostate lobe.
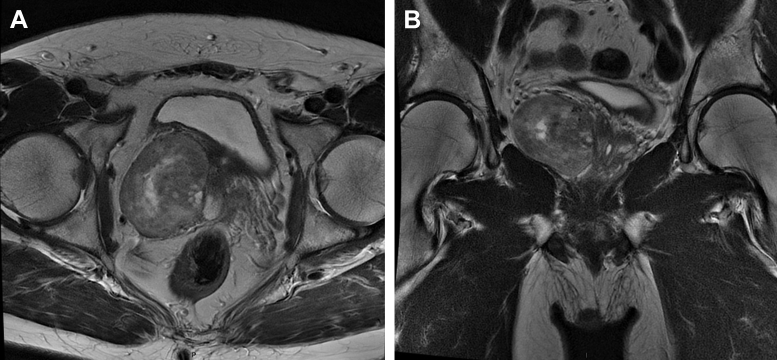
Further investigation with MRI showed a heterogenous mass with cystic and solid components in the right prostate lobe (Fig. 2). There was a mass effect on the surrounding tissue, though there was no sign of invasion of the seminal vesicles. A clear fat plane between prostate and rectum excluded a tumor of rectal origin.
Figure 2.
MRI shows a heterogenous mass located in the right prostate lobe.
CT scan did not detect any lymphadenopathy or distant metastasis.
Prostate biopsy was performed. Histopathological examination showed proliferating cells with monomorph round to fusiform nuclei. These cells showed only rare mitotic activity and mild cellular atypia. A strong vascularization was seen. There were no signs of necrosis.
Immunohistochemical analysis showed no expression of CD34. Proliferation rate of Ki67 was only 1%-2%. Expression of bcl-2, CD99, b-catenin and c-kit was not checked. The lesion showed a positive staining for the myogenic markers desmin and actin. S-100 and cytokeratin staining were negative. The suspect diagnosis was a stromal tumor of uncertain malignant potential (STUMP) or a low-grade leiomyomatous tumor.
The patient was treated with an open radical prostatectomy and extended lymphadenectomy. No frozen sections were taken.
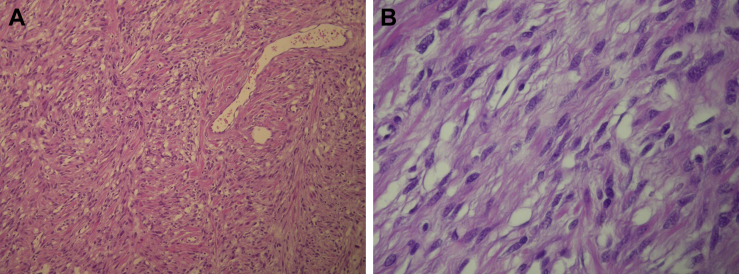
Microscopical examination showed complete resection of a low grade mesenchymal tumor at the right prostate lobe with a diameter of 5.5 cm There were less than 5 mitose figures per 50 high power fields. Resection margins were clear. There was no invasion of the capsule or seminal vesicles (Fig. 3). All eighteen resected lymph nodes were reactive and showed no malignancy.
Figure 3.
A. HE-staining 100× with bundles of elongated cells. Note the absence of normal prostatic glands. B. HE-staining 400× showing elongated leiomyocytes with spindle shaped nuclei and inconspicuous nucleolus. Top right a leiomyocyte with slight anisocytosis and anisonucleosis.
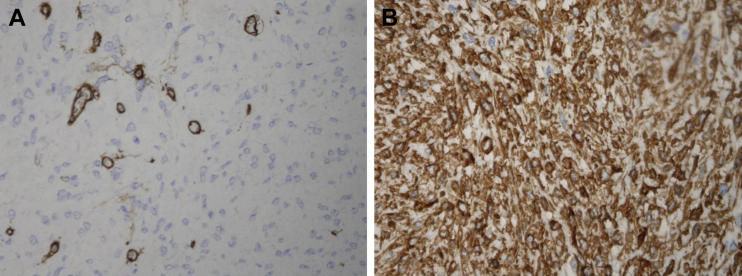
There was a strong immunoreactivity of the proliferating cells for smooth muscle cell markers desmin and actin. No immunoreactivity for CD117, CD34 and S100 was detected (Fig. 4). The proliferation fraction of Ki67 was about 2 percent.
Figure 4.
A. Strong cytoplasmic smooth muscle actine reactivity (200×). B. CD34 staining. Only reactivity in vascular endothelium and not in the proliferating cells (200×).
Based on the immunohistochemical findings, the diagnosis of a pure leiomyoma of the prostate was made.
The postoperative course of the patient was uneventful. The transurethral catheter was removed after 8 days and the patient regained complete continence after eighteen sessions of pelvic floor rehabilitation.
Discussion
A pure leiomyoma of the prostate is a rare tumor. It was first described by Kaufman and Berneike in 1951. Less than 30 cases about prostatic leiomyoma have been reported ever since.1 A leiomyoma is a benign tumor, arising from smooth muscle fibers. Occasionally it can be located in the genitourinary system, including the kidney, ureter, bladder, urachus, prostate, urethra and the seminal vesicles.2 More common locations for leiomyomas are the gastrointestinal and the female genital tract.2, 3, 4
Chronic inflammatory and infectious processes have been proposed as possible pathogenic mechanisms, whereas embryonic remnants of the Müllerian tube would lie at the origin of a true leiomyoma of the prostate.2, 4 Periglandular prostate smooth muscle and the prostate capsule are other possible locations of origin. The exact mechanism is however still unknown.2, 5
Symptoms are similar to those of benign prostatic hyperplasia and include lower urinary tract symptoms, acute urinary retention, etc.2 Two cases reported macroscopic hematuria.4, 5 Less frequently, compression of the tumor can cause rectal symptoms.5
Imaging techniques are valuable tools in diagnosing various tumors of the prostate. A leiomyoma on transrectal ultrasound can be seen as a hyperechogenic or hypoechogenic well defined mass. CT images can be very diverse, going from heterogenous to homogenous masses with or without contrast captation related to the amount of necrotic tissue.5
Magnetic resonance imaging can differentiate glandular from leiomyomatous tissue. In general, leiomyomata show a homogenous sign after gadolinium administration. Images can still be very diverse, related to the amount of histological degenerations within the lesion.5
Pathologic anatomy examination is the only medium for definitive diagnosis and is important to rule out malignancies such as leiomyosarcoma.3, 5 Immunohistochemical examination of a leiomyoma shows strong positivity for myogenic markers such as desmin and actin.2, 4, 5 The cells can present immunoreactivity against androgen receptors, variable reactivity to progesterone receptors but usually no reactivity for estrogen receptors and Ki-67.5 The presence of atypia can implicate a possible risk for malignant transformation. Atypical cells typically have multinucleate giant cells with vacuoles.5
A distinction must be made between a true leiomyoma of the prostate, which is a very rare entity, and another, more frequent form where nodules of leiomyomatosis are associated with benign hyperplasia. A true leiomyoma of the prostate has no glandular component, no capsule and no pseudocapsule of more than 1 g.2, 5 The smooth muscle cells of a pure leiomyoma replace the entire prostatic tissue. The recognition of leiomyoma is important because of the potential of malignancy in some cases, especially in those with nuclear atypia.2, 5
Due to the risk of malignant transformation, especially when cellular atypia is found, all studies in literature conclude that a complete resection of the tumor is the preferred approach.2, 3, 5 Transurethral resection, open adenomectomy and radical prostatectomy as a treatment for leiomyomas have all been reported. Due to the rarity of the tumor, no comparative studies about its treatment are available. No data about the percentage of malignant transformation were found.
Leiomyoma of the prostate has an excellent prognosis due to its benign nature and the very low recurrence rate after complete removal.2, 5
Conclusion
Leiomyoma of the prostate is a rare tumor and it should be included in the differential diagnosis when an atypical mass of the prostate is detected. Histopathological examination is essential for the definitive diagnosis. A true leiomyoma of the prostate shows no glandular prostatic tissue, whereas the presence of cellular atypia implicates a risk for malignant transformation. When complete resection is performed and no cellular atypia is found, this tumor has an excellent prognosis.
Conflicts of interest
None.
References
- 1.Hossain D., Meiers I., Qian J. Prostatic leiomyoma with atypia: follow-up study of 10 cases. Ann Diagn Pathol. 2008 Oct;12(5):328–332. doi: 10.1016/j.anndiagpath.2008.02.009. [DOI] [PubMed] [Google Scholar]
- 2.Mellas S., Bouchikhi A.A., Tazi M.F. Prostatic leiomyoma: a case report. Case Rep Urol. 2012;2012:702762. doi: 10.1155/2012/702762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oderda M., Mondaini N., Bartoletti R. Leiomyomata of the genitourinary tract: a case series from the “rare urological neoplasm” registry. Scand J Urol. 2013 Apr;47(2):158–162. doi: 10.3109/00365599.2012.727466. [DOI] [PubMed] [Google Scholar]
- 4.Van Ulden-Bleumink W.M., Dom P.G.B., Ramakers B.P.M., Van Adrichem N.P.H. A rare prostatic diagnosis of an old man: a pure prostatic leiomyoma. Case Rep Urol. 2013;2013:741235. doi: 10.1155/2013/741235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barba J., Tolosa E., Panizo A.F., Berian J.M. Prostatic leiomyoma, case report. Arch Esp Urol. 2011;64(7):631–635. [PubMed] [Google Scholar]