Highlights
-
•
Cancer developing from more than one origin is called multiple primary cancer (MPC) and is a rare situation.
-
•
We report a male case presenting to the Emergency Clinic with symptoms of ileus who was diagnosed with synchronous colon and breast cancer.
-
•
Synchronous colorectal cancer is recognized as an important clinical entity, its clinical and pathological properties as well as prognosis are still undetermined.
Keywords: Breast, Case report, Colon, Ileus, Male, Synchronous
Abstract
Introduction
Cancer developing from more than one origin is called multiple primary cancer (MPC) and is a rare situation. In this article, we report a case presenting to the Emergency Clinic with symptoms of ileus who was diagnosed with synchronous colon and breast cancer.
Presentation of case
A 57 year old male patient presented to the Emergency Clinic with abdominal pain, vomiting, constipation and lack of flatulence. The patient was taken to the operating room for emergency surgery with the diagnosis of intestinal obstruction. While still hospitalized, breast ultrasound was performed, revealing a mass lesion in the right breast measuring 2 cm. The core biopsy result was suggestive of invasive ductal adenocarcinoma. Right modified radical mastectomy with removal of the level 2 axillary lymph nodes was performed. The result of the histopathological investigation of the right hemicolectomy specimen was reported as moderately differentiated adenocarcinoma, while that of the mastectomy material was invasive ductal adenocarcinoma.
Discussion
Synchronous colorectal cancer is recognized as an important clinical entity, its clinical and pathological properties as well as prognosis are still undetermined. A family history of cancer might be a significant factor in synchronous cancers. Many of the theories about the etiology of multiple primary malignant neoplasia suggest the role of genetic, hormonal, environmental and immunological factors as well as iatrogenic causes.
Conclusion
Especially for patients whose treatment begins in the emergency settings, meticulous systemic physical examination is recommended to initiate treatment of a possible synchronous tumor at an earlier stage.
1. Introduction
Cancer is a serious health problem worldwide, being responsible from ¼ of all deaths. Among newly diagnosed cancer cases in males, the most common are the cancers of the prostate (25%), lung (15%), colon and rectum (10%) and bladder (7%). Breast cancer in males is a rare disease accounting for less than 1% of all organ cancers in males. Its proportion among all cases of breast cancer is equally minuscule [1]. Cancer developing from more than one origin is called multiple primary cancer (MPC) and is a rare situation. MPC can be classified as synchronous and metachronous. Two or more primary tumors diagnosed simultaneously or within six months to each other are called “synchronous”, whereas tumors developing more than six months after the detection of a primary tumor are called “secondary” or “metachronous” cancer [2]. The frequency of multiple primary malignant neoplasia (MPMN) is reported as 0.73% to 11.7% [3], [4].
In this article, we report a case presenting to the Emergency Clinic with symptoms of ileus who was diagnosed with synchronous colon and breast cancer.
2. Presentation of case
A 57 year old male patient presented to the Emergency Clinic with abdominal pain, vomiting, constipation and lack of flatulence. Physical examination revealed distension and widespread tenderness of the abdomen. Rectal ampulla was empty. A palpable mass was detected in the right breast. Systemic examination yielded no other pathological findings. Of the laboratory results, the white blood cell count was 1500/mm3, urea 92 mg/dL, creatinine 1.15 mg/dL, alpha-fetoprotein 3.1, carcinoembrionic antigen (CEA) 1.28, CA 125 15.4, CA 15-3 12.2, CA 19-9 13.1. An abdomen plain X-ray showed multiple air-fluid levels (Fig. 1). A contrast-enhanced computed tomography (oral and IV contrast) of the abdomen revealed a sigmoid colon mass with proximal dilatation and air-fluid levels (Fig. 2)
Fig. 1.
Abdomen plan X-ray.
Fig. 2.
A contrast-enhanced computed tomography (oral and IV contrast) of the abdomen.
The patient was taken to the operating room for emergency surgery with the diagnosis of intestinal obstruction. Intraoperative exploration revealed a mass lesion with a diameter of 5 cm at the level of the splenic flexure. No sign of metastasis was observed on other intraabdominal organs. Left sided hemicolectomy with Hartmann's procedure was performed. The patient was transferred to the ward after the operation. On the first postoperative day, the patient had flatulence and fecal discharge from the colostomy. Oral intake was allowed.
While still hospitalized, breast ultrasound was performed, revealing a mass lesion in the right breast measuring 2 cm. Magnetic resonance imaging demonstrated a mass lesion not invading the pectoralis muscle with a 2.5 cm diameter and a BI-RADS score of 5 (Fig. 3). The core biopsy result was suggestive of invasive ductal adenocarcinoma. Right modified radical mastectomy with removal of the level 2 axillary lymph nodes was performed before discharge. On the third postoperative day after the breast surgery the patient was discharged as clinically stable.
Fig. 3.
Magnetic resonance imaging of the left breast.
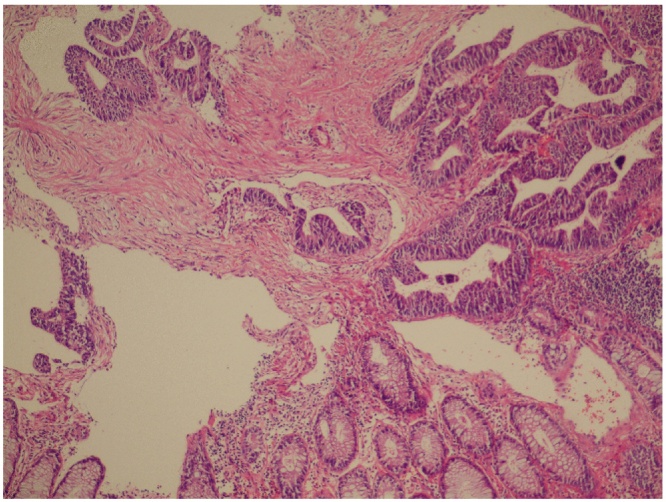
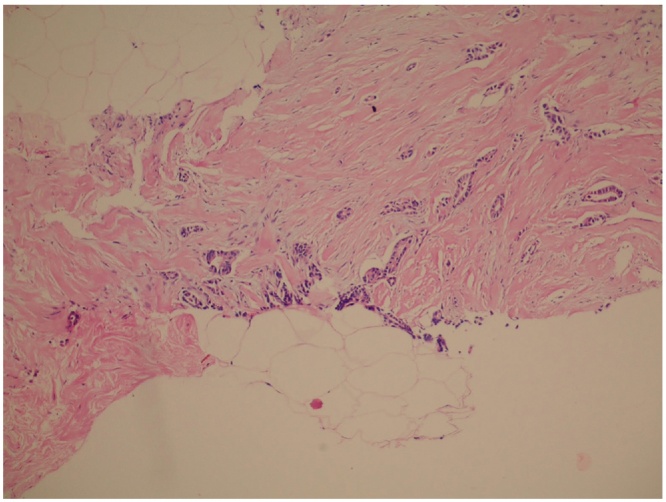
The result of the histopathological investigation of the right hemicolectomy specimen was reported as moderately differentiated adenocarcinoma, while that of the mastectomy material was invasive ductal adenocarcinoma (Fig. 4, Fig. 5). Estrogen receptor (ER) was 100% ++, progesterone receptor (PR) 95% ++, cerb2 was negative and the Ki 67 index was 40% +++. The patient was referred to the Medical Oncology clinic.
Fig. 4.
Colonic type malignant invasive glandular structures (Hematoxylin and eosin ×200).
Fig. 5.
Malignant breast invasive ductal carcinoma glandular structures (hematoxylin and eosin ×200).
3. Discussion
The incidence of breast cancer in men is 1 in 100,000; mostly presenting as ER and PR positive invasive ductal carcinomas [5], [6]. Our patient too had ER +, PR + invasive ductal carcinoma. Synchronous colorectal cancer for patients with primary colorectal cancer is reported between 2.3% and 12.4%, whereas synchronous breast cancer in men is less than 2% [7], [8]. Data regarding the incidence of coexisting breast and colon tumors in men is scarce.
Although synchronous colorectal cancer is recognized as an important clinical entity, its clinical and pathological properties as well as prognosis are still undetermined. A family history of cancer might be a significant factor in synchronous cancers. Kimura et al. [9] have demonstrated a positive correlation between the frequency of synchronous cancer and family history. Based on a series of 42 cases, Oya et al. [10], reported that synchronous colon cancer is more often located in the left colon and that synchronous tumors are smaller in size than solitary tumors. In the same study, they found the male to female ratio for synchronous colon cancer as 3.67:1 and concluded that distant metastases were more frequent in synchronous cancer cases than for solitary tumors.
Of the hereditary colorectal cancer syndromes, Lynch syndrome is associated with colon, endometrium, stomach, ovary, hepatobiliary, urinary tract, pancreas, small bowel cancers and glioblastoma. However, an increase in the risk of breast cancer has not been demonstrated fort his syndrome. Familial adenomatous polyposis carries increased risk for the malignancies of the pancreas, thyroid and liver in addition to the gastrointestinal tract. Peutz − Jeghers syndrome is associated with both breast and colon cancer, but the diagnosis requires multiple characteristic hamartomatous polyps in the small bowel, mucocutaneous hyperpigmentation and a family history of the syndrome. [11]. None of the diagnostic criteria for Peutz − Jeghers syndrome was applicable to our patient. Many of the theories about the etiology of MPMN suggest the role of genetic, hormonal, environmental and immunological factors as well as iatrogenic causes [12]. An increased risk in colorectal, urinary bladder, lung and breast cancer has been associated with endometrial cancer [13]. One study has determined a specific genetic mutation in synchronous breast and colon cancer. The CHECK2*1100delC mutation was proposed as a tool to detect synchronous tumors [14]. Our patient had no family history of cancer and no genetic tests were performed.
4. Conclusion
As a conclusion, for any patient with a newly diagnosed colon tumor, the possibility of a synchronous tumor should be remembered. Especially for patients whose treatment begins in the emergency settings, meticulous systemic physical examination is recommended to initiate treatment of a possible synchronous tumor at an earlier stage.
Conflict of interest
None.
Funding
No.
Ethical approval
None.
Consent
Written informed consent was obtained from the patient’s and his first degree relatives for publication of this case and involving images.
Author contribution
AA, KB, SA, contributed in the study concept, data acquisition and data analysis. CT and CC contributed in the data analysis. CT, AA, OS wrote the paper. All authors read and approved the final version of the submitted manuscript.
Registration of research studies
None.
Guarantor
Cihad Tatar.
Disclaimer
The case report is compliant and has been reported in line with the CARE Guidelines [15].
Contributor Information
Aziz Ari, Email: azizari02@hotmail.com.
Cihad Tatar, Email: tatarcihad@gmail.com.
Kenan Buyukasik, Email: op_dr_kenan@hotmail.com.
Ozgur Segmen, Email: ozgursegmen@gmail.com.
Coskun Cakir, Email: c_cakir@hotmail.com.
Soykan Arikan, Email: soykanarikan@yahoo.com.
References
- 1.Gradishar W.J. Male breastcancer. In: Harris J.R., Lippman M.E., Morrow M., Osborn C.K., editors. Disease of the Breast. Lippincott Williams and Wilkins; Philedelphia: 2000. pp. 661–667. [Google Scholar]
- 2.Martini N., Melamed M.R. Multiple primary lung cancers. J. Thorac. Cardiovasc. Surg. 1975;70:606–612. [PubMed] [Google Scholar]
- 3.Spratt J.S., Hoag M.G. Incidence of multiple primary cancers per man −year of followup: 20- year review from the Ellis Fischel State Cancer Hospital. AnnSurg. 1966;164:775–784. doi: 10.1097/00000658-196611000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aydiner A., Karadeniz A., Uygun K. Multiple primary neoplasms at a single institution: differences between synchronous and metachronous neoplasms. Am. J. Clin. Oncol. 2000;23:364–370. doi: 10.1097/00000421-200008000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Goss P.E., Reid C., Pintilie M. Male breast carsinoma: a review of 229 patients who presented to the Princess Margaret Hospital during 40 years: 1995–1996. Cancer. 1999;85:629–639. doi: 10.1002/(sici)1097-0142(19990201)85:3<629::aid-cncr13>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 6.Tatar C., Erözgen F., Akıncı M., Benek S., Kizilkaya C. Erkek Meme Kanserinde Prevalans ve Klinik Deneyimlerimiz. Med. Bull. Haseki. 2013;51:99–101. [Google Scholar]
- 7.Welch J.P. Multiple colorectal tumors: an appraisal of natural history and therapeutic options. Am. J. Surg. 1981;142:274–280. doi: 10.1016/0002-9610(81)90292-0. [DOI] [PubMed] [Google Scholar]
- 8.Agrawal A., Ayantunde A.A., Rampaul R., Robertson J.F. Male breastcancer: a review of clinical management. Breast Cancer Res. Treat. 2007;103:11–21. doi: 10.1007/s10549-006-9356-z. [DOI] [PubMed] [Google Scholar]
- 9.Kimura T., Iwagaki H., Fuchimoto S. Synchronous colorectal carcinomas. Hepatogastroenterology. 1994;41:409–412. [PubMed] [Google Scholar]
- 10.Oya M., Takahashi S., Okuyama T. Synchronous colorectal carcinoma: clinico-pathological features and prognosis. Jpn. J. Clin. Oncol. 2003;33:38–43. doi: 10.1093/jjco/hyg010. [DOI] [PubMed] [Google Scholar]
- 11.Jasperson K.W., Tuohy T.M., Neklason D.W., Burt R.W. Hereditary and familial colon cancer. Gastroenterology. 2010;138(6):2044–2058. doi: 10.1053/j.gastro.2010.01.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ray P., Sharifi R., Ortolano V. Involvement of the genitourinary system in multipleprimarymalignantneoplasms: a review. J. Clin. Oncol. 1983;1:574–581. doi: 10.1200/JCO.1983.1.9.574. [DOI] [PubMed] [Google Scholar]
- 13.Markakis C., Marinis A., Dikeakos P. Multiple synchronous primary neoplasms of the breast, colon and rectum after surgery for endometrial cancer: a case report. Int. J. Surg. Case Rep. 2013;4(5):493–495. doi: 10.1016/j.ijscr.2013.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meijers- Heijboer H., Wijnen J., Vasen H. The CHECH 1100C mutation identifies families with a hereditary breast and colorectal cancer phenotype. Am. J. Hum. Genet. 2003;72:1304–1308. doi: 10.1086/375121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gagnier J., Kienle G., Altman D.G., Moher D., Sox H., Riley D.S., the CARE group The CARE guidelines: consensus-based clinical case report guideline development. J. Clin. Epidemiol. 2014;67(1):46––51. doi: 10.1016/j.jclinepi.2013.08.003. [DOI] [PubMed] [Google Scholar]