Highlights
-
•
Blunt trauma can result in rupture IVC in the setting of multiple injuries.
-
•
IVC injury is rare and fatal. We report an patient survived conservative management.
-
•
IVC pseudoaneurysm can result from traumatic blunt injury to IVC.
-
•
Non-operative management of blunt IVC injury can be established in setting of hemodynamic stability.
-
•
Follow up for pseudoaneurysm and IVC disruption is needed to ensure non expansion.
Keywords: Accidents, traffic; IVC/injuries; Pseudoaneurysm; Management
Abstract
Introduction
Injuries to the inferior vena cava (IVC) secondary to blunt trauma are rare and occurs in less than 1% of all blunt trauma patients. Mortality rates for IVC injuries reported in the literature range from 34% to 70%. Inferior vena cava (IVC) pseudoaneurysms resulting from these injuries are also rare clinical entities with an uncertain natural history due to limited follow-up information.
Case presentation
This case report describes a 23-year-old woman with traumatic IVC dissection resulting in pseudoaneurysms. It also details our treatment plan, with follow-up through radiographic resolution of the pseudoaneurysms.
Discussion
Due to rarity of these injuries, management of these injuries has not been subjected to major studies, but several case reports and small retrospective studies have demonstrated that management can be tailored to the hemodynamic status of the patient. Stable patients whose injuries have achieved local venous tamponade have been successfully treated without surgical intervention, while unstable patients require operative management.
Conclusion
Of all incoming patients, IVC injuries are highly fatal with mortality rates between 70 and 90%. Management of these injuries should be tailored based on hemodynamic stability of such patients.
1. Introduction
Blunt injury to the inferior vena cava (IVC) is rare, occurring in less than 1% of blunt trauma patients. Deceleration causes shear forces on vessels which can quickly produce rapid uncontrollable hemorrhage. The IVC is anatomically divided into five segments: infra-renal (IRIVC), para-renal (PRIVC), supra-renal (SRIVC), retro-hepatic (RHIVC), and supra-hepatic (SHIVC). Overall, the most frequently injured segment is the IRIVC (39%), followed by the RHIVC (19%), SRIVC (18%), PRIVC (17%), and the SHIVC. Aneurysms and pseudoaneurysms of the inferior vena cava (IVC) can result from such injuries. A pseudoaneurysm is a pulsatile hematoma with disruption of one or more vessel layers and is always acquired. A small tear of the IVC leads to slow extravasation of blood, allowing the areolar tissue to form a sac, thus creating an unstable environment with a high rate of rupture. Despite these anatomic differences, aneurysms and pseudoaneurysms of the IVC are discussed similarly because they behave in the same way.
Factors predictive of mortality reported include level of the IVC injury, hemodynamic status on arrival, number of associated injuries, blood loss and transfusion requirements, among others. Recent work by Huerta el al described Glasgow Coma Scale (GCS) as an independent predictor of mortality in IVC trauma. Only 39 instances of IVC aneurysms and pseudoaneurysms have been reported in the world literature. Of these, only a few were in a suprahepatic location and most were managed surgically. We present a case of an IVC pseudoaneurysm (contained traumatic supra-hepatic rupture of the IVC and associated pericaval hematoma) without involvement of the pericardium is reported, which required no surgical intervention.
2. Case report
A 23-year-old woman presented to our level 1 trauma center after a head-on motor vehicle crash. The patient was in shock with a heart rate of 122 and a systolic blood pressure (SBP) of 92. A massive transfusion protocol was initiated. Patient received 4 units of packed red blood cells(PRBC) and her blood pressure stabilized. Focus abdominal sonographic test (FAST) was negative. With hemodynamic stability established a completion trauma computed tomography (CT) was performed. Injuries included grade IV liver laceration, grade I splenic laceration, unstable C2 fracture, right knee arthrotomy, left lower mid shaft femur fracture, left open distal tibia-fibula fracture, right posterior hip dislocation. Also revealed is an irregularity of the suprahepatic IVC with contained contrast extravasation consistent with an IVC pseudoaneurysm at the hepatic confluence of the IVC (Fig. 1). Observation of these lesions was felt to be the safest course of action in this severely injured polytrauma patient who, at the time of diagnosis, was hemodynamically stable. Her fluid management was closely monitored preoperatively using the end points of urine output, heart rate, and blood pressure. A central venous catheter was not initially placed due to concerns of further injury to the pseudoaneurysms. On hospital day 3(HD3) MRI of the brain indicated multiple punctate lesions consistent with fat emboli; subsequent TTE with bubble study found evidence of patent foramen ovale(PFO) with moderate right left shunting. On HD6, the patient was noted to be tachypneic; A CT angiogram of the chest was performed which showed a pulmonary embolism. Patient was placed on heparin drip. An IVC filter was also placed. Venogram performed at the time revealed no active extravasation.
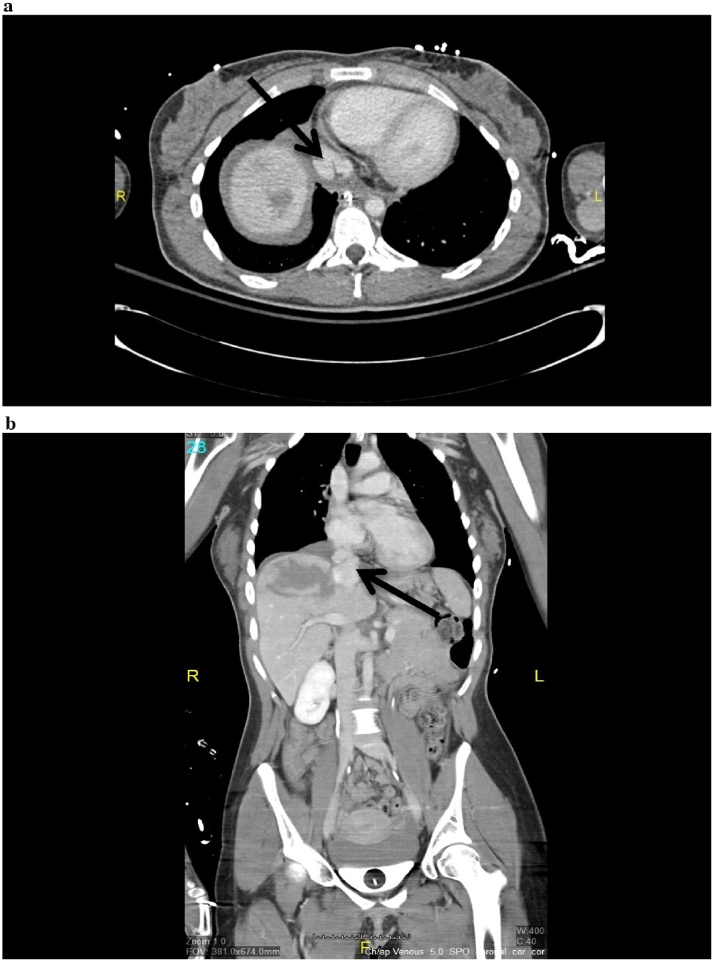
Fig. 1.
a. An axial image from the patient’s initial computed tomography study demonstrates a pseudoaneurysm along the posterior aspect of the suprahepatic inferior vena cava (IVC). b. Coronal image demonstrates focal irregularity of the IVC at the confluence with the right hepatic vein.
She was transferred out of the surgical intensive care unit (SICU). A repeat CT venogram on HD 9, 14 (Fig. 2), and 21 after injury demonstrated stability of the IVC pseudoaneurysms. Owing to her continued hemodynamic stability and the lack of pseudoaneurysm growth, a nonoperative approach was maintained, with planned CT venogram 4 weeks later. The repeat CT scan showed a decrease in size of the IVC pseudoaneurysm from 1.5 to _1 cm. After this decrease in size, it was decided to perform repeat imaging in 6 months with a plan for surgical intervention only in the presence of clinical symptoms or enlargement. She was subsequently discharged to home after a 26-day hospital stay. A repeat abdominal CT, obtained 6 month (Fig. 3) later, demonstrated resolution of IVC pseudoaneurysms.
Fig. 2.
A sagittal image from the patient’s repeat computed tomography study demonstrates stable pseudoaneurysm along the confluence of the suprahepatic inferior vena cava (IVC).
Fig. 3.
a. Axial computed tomography image taken approximately 6 month after the initial caval injury demonstrates interval resolution of the traumatic pseudoaneurysm of the suprahepatic inferior vena cava (IVC); b. Coronal image demonstrates resolution of the IVC at the confluence with the hepatic veins.
3. Discussion
Injuries to the IVC are relatively uncommon in the setting of blunt abdominal trauma and are rarely isolated. In one study of 10 patients who presented with IVC injury secondary to blunt trauma, there was a 70% mortality rate. Depending on the location of injury, death is due to exsanguination or cardiac tamponade. Typically, trauma to the IVC is associated with liver injury and the liver is the second most commonly injured abdominal organ in blunt trauma. Damage to juxtahepatic veins constitutes a small proportion of all liver injuries, but the mortality rate is between 50 and 80% with most deaths caused by exsanguination. There are few studies that scrutinize the repair of injuries to the vena cava and juxtahepatic veins, as these injuries are rare and usually fatal before treatment can be initiated. IVC aneurysms are also a rare clinical entity. A review of the limited cases available in the literature shows patient presentation and pathogenesis of the aneurysms are diverse. In search of some predictability, it seems as though location of the aneurysms can be tied to the mechanism in traumatic caval injury. Caval injury caused by blunt abdominal trauma results in injury of the IVC at the retrohepaticor-intrapericardial regions of the IVC.
Decision to repair an IVC injury is based on the location, extent of injury and on the hemodynamic status of the patient. Patients who are stable or whose caval injuries have reached spontaneous vascular tamponade, typically through containment by the liver capsule, diaphragm or suspensory ligaments, have been successfully managed with conservative treatment. Operative strategies have been employed for unstable patients, patients with large defects of the IVC and for patients whose caval hematomas are not contained. The suprahepatic region of the IVC is challenging for surgical intervention, as it requires dividing the falciform ligament, cross clamping, mobilizing the damaged IVC segment and extending the abdominal incision into a full sternotomy. Intervention is associated with high perioperative mortality and morbidity rates and long-term complications, including IVC stenosis and thrombosis. Nearly, all case reports describing the repair of these lesions involve the use of cardio-pulmonary bypass and grafting the damaged vessels and have a high mortality rate between 70 and 90%. There is one recent report, however, which described the successful reconstruction of an extra pericardial rupture of the IVC using a cross-clamping technique and a Gore-Tex prosthesis. In hemodynamically stable patients with symptoms, IVC aneurysms or pseudoaneurysms can be treated by endovascular methods, including stents, balloon occlusion, and electrothrombosis. In light of the clinical and hemodynamic stability of our patient, imaging findings of a contained suprahepatic IVC pseudoaneurysm, challenging operative region for intervention and risk of morbidity associated with operative treatment, the decision was made for conservative management. Close follow- up is required to reduce the chance for an adverse event.11 We would submit that in a patient with an asymptomatic IVC aneurysm, even at a precarious location such as the cavoatrial junction, serial imaging should be used and intervention should be limited to those patients with symptoms or those aneurysms that demonstrate growth on serial imaging. We would recommend a venography or CT venogram at 30 days, 6 months, and a year or until resolution occurs.
4. Conclusions
IVC blunt injuries resulting in pseudoaneurysms are an unusual clinical phenomenon with different etiologies. Owing to the paucity of reports and lack of data, consensus is lacking on the management of these patients. Because of the success reported here and by others, we believe that a nonoperative approach in asymptomatic aneurysms can be undertaken, given close radiographic follow-up and clinical stability.
Conflicts of interest
None.
Funding
None.
Ethical approval
Approval has been given.
Consent
No consent was needed as this was a case report and it did not include any patient identifiers.
A written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the consent is available on request.
Author contribution
Ali Cheaito is responsible for design, data collection, and writing of paper.