Abstract
Legionella pneumophila is, by far, the species most frequently associated with Legionnaires’ disease (LD). Human infection occurs almost exclusively by aerosol inhalation which places the bacteria in juxtaposition with alveolar macrophages. LD risk management is based on controlling water quality by applying standardized procedures. However, to gain a better understanding of the real risk of exposure, there is a need (i) to investigate under which conditions Legionella may be aerosolized and (ii) to quantify bacterial deposition into the respiratory tract upon nebulization. In this study, we used an original experimental set-up that enables the generation of aerosol particles containing L. pneumophila under various conditions. Using flow cytometry in combination with qPCR and culture, we determined (i) the size of the aerosols and (ii) the concentration of viable Legionella forms that may reach the thoracic region. We determined that the 0.26–2.5 μm aerosol size range represents 7% of initial bacterial suspension. Among the viable forms, 0.7% of initial viable bacterial suspension may reach the pulmonary alveoli. In conclusion, these deposition profiles can be used to standardize the size of inoculum injected in any type of respiratory tract model to obtain new insights into the dose response for LD.
Legionella are facultative intracellular pathogens that cause Legionnaires’ disease (LD), although some species are strictly intracellular1. Epidemiological studies unambiguously identified water as the main reservoir of Legionella. Man-made ecosystems (e.g., hot water and air conditioning systems, shower heads, humidifiers, cooling towers, and whirlpool baths) have been the source of several outbreaks of LD2,3,4,5. In particular, hospital water distribution systems serve as the primary reservoir for nosocomial legionellosis. Respiratory therapeutic devices (including oxygen humidifiers, medical aerosol-producing devices such as nebulizers and face masks) filled or rinsed with tap water may serve as secondary reservoirs for LD infection6,7,8. LD may also occur after inhalation of amoeba vacuoles containing Legionella9.
A bioaerosol is defined as a collection of biological particles (including bacteria and fungi in addition to viruses and fragments of organisms) dispersed in the air10. It is generally composed of single cells or aggregates of cells (e.g., bacterial cells, spores, actinomycetes, endotoxins, and amoebae vacuoles) but can also be composed of cell conglomerations with small dust particles or water droplets. For instance, LD is a high-profile pathogenic bioaerosol-transmitted infection11,12,13.
The ability of Legionella to cause disease is associated with their ability to enter the respiratory system through respirable-size droplets as transporting particles. The conditions under which Legionella may be aerosolized and how they enter the respiratory tract upon aerosol generation remain poorly documented10,14.
Droplet generation is thought to be a key step in the transmission of Legionella4; water is as an excellent transporting medium for the bacterium. However, the effectiveness of the process by which water in the reservoir is transferred to the air and then to the human respiratory tract remains poorly investigated. Both processes seem to depend mainly on the interdependence of the sizes of transporting and transported particles15. The geometric and aerodynamic sizes of the water droplets with respect to microbial survival and lung deposition are critical factors in the delivery of viable bacteria to the human respiratory system. In addition, the process at the origin of water droplet generation can induce enrichment of bacterial concentration in the airborne liquid droplets relative to the bulk concentration in the reservoir15. This bacterial enrichment is a complex phenomenon. As a result, measurement of the size distribution of liquid aerosols correlated with an infectious dose remains challenging. Infectious doses for humans can be extrapolated only from animal inhalation studies (e.g., guinea pigs) in the CFU range of 8,000–17,00016. Of the mechanisms by which human infection may occur, we decided to focus on medical nebulization because it has been less studied in comparison with other environmental exposures, such as aerosols generated from spa pools or industrial cooling towers4,17. Our study benefits from the newest technology available on the nebulizer market for droplet generation, vibrating-mesh nebulizers, rather than the common jet nebulizers commonly used to infect animals during inhalation experiments14. The main advantages of vibrating-mesh nebulizers include consistent aerosol generation efficiency, a high fine-particle fraction reaching the peripheral lung and a low residual volume in the reservoir. It is commonly accepted that mesh nebulizers are more efficient than jet nebulizers and can provide higher drug doses to patients18.
In addition to investigating the effectiveness of the L. pneumophila transfer from the water in the reservoir to the air and then to the human respiratory tract, we evaluated the viability of the inoculum within the generated droplets. At least 14 physiological forms of L. pneumophila have been described according to the various environments they may colonize19. Among them, the presence in water samples of viable but not culturable (VBNC) forms contributes to underestimation of the number of potentially pathogenic Legionella detected by standard methods. Our preliminary studies on anthropic reservoirs have demonstrated the presence of VBNC forms of Legionella after water disinfection treatments (heat20 and chlorine21). Finally, the role of Legionella intracellular forms (intra-amoebic) has been little investigated in environmental samples22 even though these forms are considered more infectious19. VBNC cells can be detected and quantified by a flow cytometric assay (FCA)23. Assessment of their presence is important because they are able to infect amoebas as well as macrophage-like and epithelial cells from human respiratory mucosa after resuscitation on amoebas21,24.
Very few studies have sought to quantify the presence of all viable forms of Legionella and size of Legionella-containing droplets25,26. Thus, in this paper, we propose a methodology for determining airborne particle distribution and the number of Legionella cells in airborne droplets of a given size. More specifically, new insights are provided into the size characterization of Legionella bioaerosols, including assessment of the number of viable (culturable (VC) or not (VBNC)) bacterial cells in respirable droplet size fractions. The secondary objectives were (i) to improve our knowledge of the role of aerosols in the transmission of Legionella using vibrating-mesh nebulization and (ii) to fully characterize an experimental set-up that enables determination of aerosol deposition profiles under laboratory conditions within an animal respiratory tract.
Results and Discussion
Validation of the experimental set-up
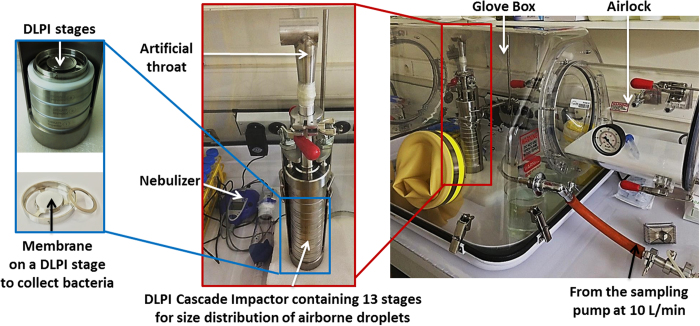
Aerosol generation by an e-Base® vibrating-mesh nebulizer was performed in a glove box (Fig. 1). Briefly, the Legionella-calibrated suspension was introduced into the nebulizer reservoir. The nebulizer was connected to the low-pressure impactor (DLPI) by an artificial throat. A pump-simulating inspiration was used during nebulization to collect aerosols on the 13-DLPI stages. The size classification in DLPI was set at up to 10 μm, with evenly distributed impactor stages.
Figure 1. Experimental set-up for the generation and characterization of aerosols.
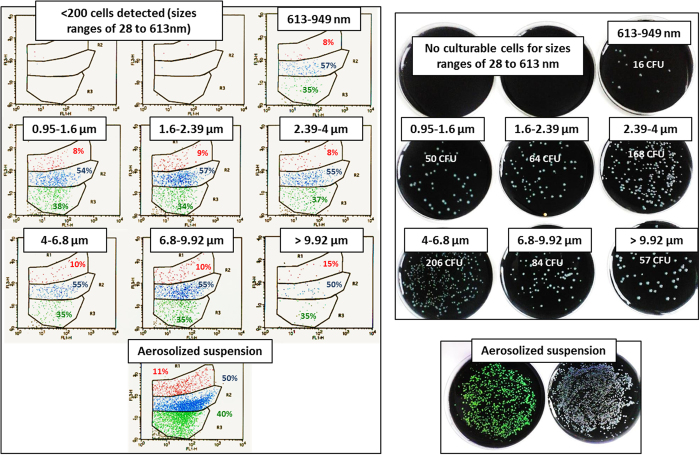
Bacterial detection and viability before and after aerosolization were assessed using culture, qPCR and FCA on Lp1 008 suspensions of different concentrations and stages: exponential phase forms (EPFs) and stationary phase forms (SPFs) according to a procedure described by Faulkner and Garduno27. As determined by qPCR, only 15.8 ± 2.4% of the initial total inoculum (in genomic units (GU)) was recovered from the 13-DLPI stages after aerosolization. The remaining part of the inoculum was either kept in the nebulizer reservoir or disseminated in the artificial throat. The percentage recovered was the same for both suspensions at both concentrations, indicating good reproducibility of the nebulization process. As shown by FCA analysis and cultivability on BCYE media, the percentages of VC (35.7 ± 1.3%), VBNC (55.7 ± 1.1%) and dead cells (DC; 8.7 ± 0.9%) were the same for both aerosolized suspensions and those recovered at each DLPI stage (Fig. 2).
Figure 2. Representative experimental results obtained with FCA and culture for different aerodynamic size ranges of airborne particles (n = 3, repeated twice).
Left: FCA results in percentages. Cells are distributed according to propidium iodide fluorescence intensity versus GFP fluorescence intensity. Green: VC, blue: VBNC, red: DC. Right: culture in colony-forming units (CFU). Aerosolized suspension of Lp1 008 EPF cells at 2.107 CFU/mL.
Validation of bacterial suspension prior to aerosolization
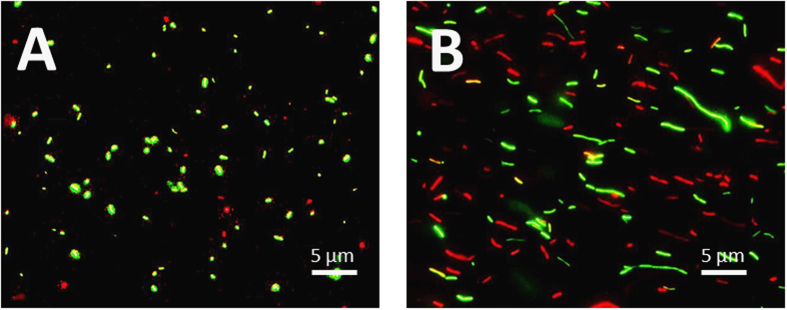
Figure 3 shows that Lp1 008 EPF cells were composed mostly of cells approximately 1 μm long whereas Lp1 008 SPF cells consisted of polymorphic bacilli ranging from 1 μm to >5 μm. It is known that Legionella become highly polymorphic with age27. Because the size of the contaminating bacteria may be a critical factor with respect to both bioaerosol infection and access to the respiratory tract and small bacilli 1 μm long are often encountered within environmental samples as planktonic cells28,29, the use of Lp1 008 EPF cell suspensions seemed more pertinent for further testing.
Figure 3. Microscopic epifluorescent image (Gx400) of aerosolized Legionella suspension.
(A) Lp1 008 EPF cells. (B) Lp1 008 SPF cells.
After FCA, more Legionella DC were observed in Lp1 008 SPF cell than in Lp1 008 EPF cell suspensions at the two concentrations tested (2 × 106 and 2 × 107/mL). Because the detection limit of FCA is 103 cells/mL, the use of a calibrated suspension at 2 × 106 CFU/mL was not appropriate. These results validated our choice to use Lp1 008 EPF cell suspensions at 2 × 107 CFU/mL for the characterization of Legionella aerosols.
Size distribution of transporting droplets
To determine whether sodium fluoride (NaF) and Legionella nebulization generate distinctive aerosols, they were compared with respect to cumulative distribution (NaF cumulative mass distribution versus Legionella cumulative distribution in % of genomic units). Figure 4 shows aerodynamic diameters, which, for unit density spheres such as water droplets, are the same as physical diameters.
Figure 4. Typical cumulative distribution of airborne droplets characterized by a low-pressure impactor (DLPI).
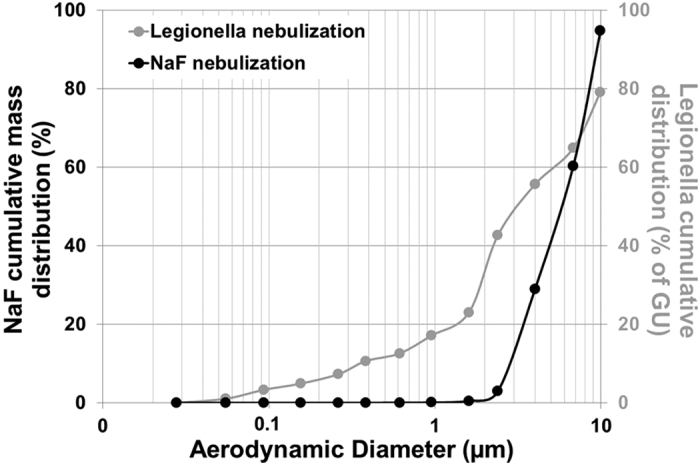
NaF quantification by an electrochemical method (expressed in % of mass reaching each stage of the DLPI, i.e., in % of total mass of NaF aerosolized). Legionella quantification by qPCR (expressed in % of genetic units reaching each stage of the DLPI, i.e., in % of total airborne Legionella). Particles larger than 10 μm were not plotted.
The aerosols produced using NaF as a chemical marker for size distribution of transporting droplets demonstrated a mass median aerodynamic diameter (MMAD) of 6.1 μm ± 0.4 with a geometric standard deviation (GSD) of 1.7 μm ± 0.1. Thus, the size distribution of transporting droplets generated by the vibrating-mesh nebulizer can be considered to be monodispersed. In addition, the distribution of airborne Legionella showed an MMAD of 3.4 μm ± 0.4 with a GSD of 4.1 μm ± 1.2. The particle size distribution of Legionella generated by the nebulizer is highly polydispersed in comparison with the transporting droplets. This difference in the polydispersity index should be due to different compositions of the aerosols (e.g., bacteria packaged or not in droplets), as measured during nebulization using the vibrating mesh technology.
Characterization of Legionella aerosols
Particles with aerodynamic diameters in the submicron range cannot transport Legionella bacteria, which are several times larger than the water-transporting particles. Moreover, a liquid environment appears to be necessary for the bacteria to remain viable while airborne. Thus, we assumed that the bacterial spread that may cause LD requires the generation of water droplets small enough to be deposited in the thoracic region but large enough to contain viable and virulent Legionella. The size distribution of airborne droplets is critical for delivering viable bacteria to the respiratory tract, and the mass of droplets of this given size is related to the number of bacteria contained within. A specific size range of droplets (2–10 μm) is required for the bacteria to be delivered to the thoracic region30. Overall, one can admit that the minimum droplet diameter that may contain bacteria is between 1 and 2 μm14,15. However, depending on the way by which aerosols are inhaled (mouth versus nose inhalation of aerosols), results may vary. Indeed, several studies have shown that nose-inhalation aerosols of more than 2.5 μm in diameter cannot reach the pulmonary alveoli31,32. Mouth inhalation of aerosols may propose different results, showing the possibility for aerosols of 1–10 μm to reach the pulmonary tract33.
In the present study, 93.4% of the total amount of airborne Legionella DNA was in a particle size range of 1.6–9.92 μm (Fig. 4, Tables 1 and 2). This result indicates that 93.4% of the airborne Legionella DNA detected were compatible with efficient aerosolization of bacteria entrapped in water-transporting particles. The particles were large enough to contain Legionella in viable and pathogenic conditions and to allow droplet deposition in the thoracic region.
Table 1. Quantification of Legionella by qPCR (expressed as percentages of genomic units) reaching each stage of the DLPI.
| Range of aerodynamic diameter | Legionella in % of the initial bacterial suspension | Legionella in % of the total airborne bacteria |
|---|---|---|
| 28–55 nm | 0.01 ± 0.02 | 0.10 ± 0.80 |
| 55–93 nm | 0.04 ± 0.05 | 0.25 ± 1.30 |
| 93–155 nm | 0.11 ± 0.05 | 0.65 ± 0.70 |
| 155-262 nm | 0.02 ± 0.05 | 0.10 ± 1.50 |
| 262–382 nm | 0.07 ± 0.05* | 0.45 ± 1.60* |
| 382–613 nm | 0.11 ± 0.15* | 0.70 ± 2.70* |
| 613–949 nm | 0.09 ± 0.10* | 0.55 ± 2.20* |
| 949–1600 nm | 0.60 ± 0.20* | 3.80 ± 5.40* |
| 1.6–2.39 μm | 5.85 ± 2.20* | 37.15 ± 8.20* |
| 2.39–4 μm | 1.20 ± 0.40* | 7.80 ± 1.85* |
| 4–6.8 μm | 0.85 ± 0.70* | 5.40 ± 7.55* |
| 6.8–9.92 μm | 2.40 ± 0.90* | 15.15 ± 5.40* |
| >9.92 μm | 4.40 ± 1.70* | 27.90 ± 9.15* |
Total (VC, VBNC and DC) Lp1 008 Legionella was quantified by qPCR. The results from three independent experiments are expressed as percentages of genomic units (GU) compared to the quantity of total Legionella in bacterial suspension initially introduced into the nebulizer to generate the bioaerosol or compared to the total aerosolized Legionella (i.e., the sum of the bacteria deposited in the 13 stages of the DLPI). Sizes of aerosols that may reach the pulmonary region are highlighted in bold.
*Culturable cells.
Table 2. Main features of Legionella bioaerosols depending on the transporting droplet size distribution.
| |
0–0.262 | 0.262–0.949 | 0.949–1.6 | 1.6–9.92 | |
|---|---|---|---|---|---|
| Droplet range (μm) | Possibility of cellular fragments entrapped or not in droplets | ||||
| Mode of bacterial transportation | Cellular fragments (entrapped or not) in droplets | Airborne bacteria not entrapped in droplets | Airborne bacteria (entrapped or not) in droplets | Airborne bacteria packaged in droplets | |
| Total Legionella quantification by qPCR | in % of the initial bacterial suspension | 0.2 ± 0.1 | 0.3 ± 0.1 | 0.6 ± 0.3 | 14.7 ± 2.1 |
| in % of the total airborne bacteria | 1.1 ± 0.3 | 1.7 ± 0.1 | 3.8 ± 0.4 | 93.4 ± 14.2 | |
| Detection of culturable cells | No | Yes | Yes | Yes | |
| Viable cells in CFU | Not detectable | 2 × 104 ± 1.4 × 103 | 4.5 × 104 ± 1.8 × 104 | 1.1 × 106 ± 1.6 × 105 | |
Total Legionella (VC, VBNC, DC) results are expressed as percentages (see Table 1). Viable cells (VC, VBNC) results from three independent experiments are expressed in colony-forming Units (CFU).
We suggest two possible explanations why the particle size of the remaining 6.6% (1.1%, 1.7% and 3.8% in the 28–262 nm, 262–949 nm and 0.949–1.6 μm ranges, respectively) of the total airborne Legionella DNA was 55 nm-1.6 μm (Fig. 4, Table 1). One is that the Legionella DNA detected might come from cellular fragments that are entrapped or not in droplets. This phenomenon can occur for all particle sizes, but it seems uncommon; approximately 1.1% of the total airborne Legionella DNA could be attributed to cellular fragments of 28–262 nm because no culturable cells were detected (Fig. 2, Tables 1 and 2). The second possible explanation is that the orientation of bacteria against the flow direction during sampling in the DLPI cascade impactor resulted in the presence of 1.7% of total airborne Legionella DNA, with the detection of culturable cells of 0.262–0.949 μm (Fig. 2, Tables 1 and 2). This seems to indicate that some airborne and viable Legionella cells were not packaged in spherical liquid droplets (because it is sterically impossible to entrap a viable Legionella cell in a sphere 0.3 μm in diameter). Indeed, the gravitational settling speed of a particle is determined by the opposing effects of the gravitational force and the aerodynamic resistance. The aerodynamic drag force depends on the shape and orientation of the particle with respect to its direction of motion. Thus, a cylindrical particle settles under gravity with an orientation parallel to its direction of motion. This phenomenon was observed with inhalation of fibrous particles such as asbestos34.
The detection of culturable cells from the 262 nm cut-off diameter of the DLPI cascade impactor clearly shows that viable bacteria that were not entrapped in droplets were aerosolized in the 262–949 nm range. Specifically, the detection of culturable cells of 262 nm is to be expected if we consider the orientation of the bacteria with respect to their direction of motion in the cascade impactor, given the bacteria’s rod-like shape and their size (approximately 1–2 μm long and 0.3–0.9 μm wide). Finally, the 3.8% of the total airborne Legionella DNA that were detected in the size range of 0.949–1.6 μm can be attributed to airborne Legionella in transporting droplets (entrapped or not) because the droplet diameter that may contain these bacteria is between 1 and 2 μm14,15.
Thus, we can identify 4 modes of transportation during the aerosolization of Legionella (Table 2): cellular fragments of Legionella (entrapped or not) in droplets (28–262 nm), airborne bacteria not entrapped in droplets and oriented by the air flow direction during the respiration process (0.262–0.949 μm), airborne bacteria (entrapped or not) in droplets (0.949–1.6 μm), and airborne bacteria packaged in droplets (1.6–9.92 μm).
In our study, 44% of total airborne Legionella DNA or 7% of initial bacterial suspension in the 0.26–2.5 μm range reached pulmonary alveoli. Among viable forms (VC and VBNC) as determined by FCA and cultivability, 43% of total airborne viable Legionella or 0.7% of initial viable bacterial suspension reached the pulmonary alveoli (Tables 1 and 2). As shown in microscopic epifluorescent images (Gx400) of aerosolized Legionella suspensions (Fig. 3), Lp1 008 EPF cells were composed mostly of cells approximately 1 μm long, whereas Lp1 008 SPF cells consisted of polymorphic bacilli ranging from 1 μm to >5 μm in size. Consequently, only Lp1 008 EPF cells could reach the pulmonary alveoli.
Few attempts have been made to investigate the sizes of liquid aerosols that have disease potential. Insights into the human dose response for LD are determined by quantitative microbial risk assessment (QMRA) techniques that animal model data may provide35. However, injected Legionella concentrations were determined as culturable cells (VC) only36,37,38, although real concentrations of total viable cells (VC and VBNC) can be determined by FCA23. Under our experimental conditions, 0.7% of initial viable bacterial suspensions might reach the pulmonary alveoli. Thus, it is possible to standardize the size of inoculum injected in animal models by reducing the high dispersion of the LD50% (lethal dose) values35 and focusing on all viable forms (VC and VBNC).
Animals are infected via intratracheal, nasal, intraperitoneal injections or tracheal instillation. This study is the first investigation of the aerosolization of Legionella by vibrating-mesh technology, which enables delivery of Legionella aerosol to a laboratory animal model.
Methods
Experimental design
Results presented in the tables and figures are for a bacterial concentration of 2.107 CFU/mL (2–3 days with Lp1 008 EPF cells). The aerosol experiments were performed in triplicate (3*13-DLPI stages, i.e., 39 analyzed samples). The biological analysis of each 13-DLPI stage was performed in duplicate (i.e., 78 samples for culture, FCA and qPCR).
Bacterial culture and suspension preparation
A Legionella pneumophila serogroup 1 GFP (green fluorescent protein)-modified strain was used39,40. This LP1 008-GFP strain was stored at −80 °C in Cryobank tubes (Mast Diagnostic, Amiens, France). After thawing, the strain was plated onto BCYE agar (Buffered Charcoal Yeast Extract, Oxoid, France) supplemented with chloramphenicol (Sigma Aldrich, France) at 8 mg/mL for 72 h at 37 °C (for plasmid selection) and then re-plated onto the same medium and incubated at 37 °C for another 2–3 days to obtain Lp1 008 EPF cells or for 5–6 days to obtain Lp1 008 SPF cells. These cultures were then used to achieve 5 mL suspensions in sterile normal saline (0.9% NaCl) water at a final concentration of 2.106 or 2.107 CFU/mL. An optical density of 0.2 at 600 nm (Biomate TM3; Avantec, Illkirch, France) was taken as a reference for a suspension containing 108 CFU/mL. The 5 mL suspensions were immediately placed in the nebulizer for cascade impactor experiments to determine the size distribution of airborne particles.
Generation of aerosols
Nebulizers for medical applications are usually employed to generate bioaerosols with small-particles (1–3 μm)14. In this study, the nebulizer used to aerosolize bacterial suspensions, or sodium fluoride solution (used as a usual chemical tracer for aerosol according to the NF EN 13544-1 standard), was an e-Base® Nebulizer System (PARI GmbH, Stanberg, Germany). The mechanism of aerosol generation was based on a perforated oscillating membrane technology. It consists of the high-frequency vibration of a very thin membrane with a multitude of micrometric holes. The holes allow very fine nebulization from the liquid in the device’s reservoir (Fig. 1).
Size distribution of airborne particles
Low-pressure cascade impactor set-up
The airborne particle size distribution was assessed using a 13-stage cascade low-pressure impactor (DLPI, Dekati, Finland). At an airflow of 10 L min−1, particles were impacted depending on their inertia-related aerodynamic diameter in one of the 13 size fraction stages. The size classification in DLPI was set at up to 10 μm, with evenly distributed impactor stages. In each size fraction, the particles were collected on collection substrates to obtain their gravimetric size distribution. Specifically, the mass median aerodynamic diameter (MMAD) and the geometric standard deviation (GSD) were calculated. The MMAD was defined as the median of the distribution of the airborne particle mass with respect to the aerodynamic diameter. The GSD was used to characterize the dispersion of aerosols. When the GSD was lower than 2, aerosols were considered to be monodispersed; when it was higher than 2, the particle size distribution was polydispersed32,41,42.
Size distribution of transporting droplets
We used NaF as a molecular tracer for aerosols in order to determine the aerodynamic size distribution of the droplets according to the NF EN 13544-1 standard. For this purpose, 4 mL of NaF (2.5 wt%) was introduced into the nebulizer reservoir. The nebulizer was connected to the DLPI via an artificial throat (according to the United States Pharmacopeia: height 112 mm, width 42 mm, internal diameter 19 mm) (Fig. 1). The NaF solution initially introduced in the reservoir was aerosolized for 10 min. Then, each DLPI stage was rinsed with 5 mL of deionized water to collect the NaF deposited on each size-fraction stage. The NaF concentration of samples was assayed using an electrochemical method (PerfectIONTM combined with a SevenGo proTM F− electrode, Mettler Toledo, France). Finally, the MMAD and the GSD of the nebulized droplets were calculated32,41,42.
Size distribution of airborne-transported bacteria
A bacterial analysis of the size-classified particles was performed when a bacterial suspension was introduced into the nebulizer reservoir. Indeed, transporting water droplets must be large enough to contain Legionella in viable conditions. Thus, the concentration of Legionella bacteria depending on the water droplet inertia-related aerodynamic diameter should also be determined. These experiments were conducted inside a Glove Box (815-PGB GLOVE BOX, Fisher Scientific) to prevent infection of the experimenters. The same DLPI protocol as that used for the NaF aerosol experiments was employed, except that each stage of the cascade impactor was covered with a specific membrane for Legionella collection (polycarbonate membrane–membrane filters Nuclepore™ track etched, Whatman, GE Healthcare). After nebulization, each membrane potentially retaining bacteria was collected in 5 mL of physiological water. After 30 sec of sonication (Bransonic 32 sonicator bath, Branson Instruments, Danbury, CT USA), the bacterial suspension of each 13-DLPI stage was analyzed by culture (viable and culturable cells—VC), flow cytometry (percentage of VBNC cells) and qPCR (VC, VBNC and dead cells—DC).
Biological characterization of Legionella bacteria
Quantification by qPCR
The bacteria were quantified using a GFP mut2 sequence43 expressed by Lp1 008-GFP cells. The forward and reverse primers were 5′-AGAGTGCCATGCCCGAAGGT-3′ and 5′-AAGGACAGGGCCATCGCCAA-3′, respectively. Plasmid DNA was extracted from all samples with the NuCleoSpin Plasmid kit (Macherey-Nagel) according to a procedure described by Cormack et al. Real-time quantitative PCR (qPCR) was carried out on an ABI Prism 7500 automate (Applied Biosystems), using the 2X Power SYBR® Green PCR Master Mix (Life Technologies) under the following conditions: initial denaturation for 15 min at 95 °C, 50 cycles consisting of 15 s denaturation at 95 °C, and 1 min annealing and elongation at 60 °C. At the end of every elongation step, the fluorescence of the incorporated SYBR green dye was measured. After 50 cycles of amplification, a melting curve program was incorporated to check for any primer dimers or other non-specific amplifications. For each experiment, three independent extractions, on the initial calibrated suspension and on each 13-DLPI stage, were performed, and each extraction was run in duplicate. The results were analyzed using Sequence Detection Software version 1.4 (ABI 7500 System Software, Applied Biosystems). The results were expressed in genomic units (GU) of amplified GFP sequence.
Cultivability
Cultivability assessment (determination of the number of viable and culturable cells—VC) was performed on initial bacterial suspensions and on bacterial suspensions collected from each 13-DLPI stage. Experiments were performed in duplicate. Each bacterial suspension (100 μL) was plated on two BCYE agar samples with or without chloramphenicol supplementation and incubated at 37 °C for 72 h. All BCYE plates were observed under UV at 366 nm to enumerate Legionella colonies (CFU) expressing GFP.
Percentage of VBNC Legionella by flow cytometric assay (FCA)
As previously described20,23,24, FCA profiles were obtained using a combination of GFP green fluorescence (viable cells expressing GFP) and propidium iodide (PI) red fluorescence for cells with damaged membranes. One milliliter of bacterial suspension (prior aerosolization or collected from each 13-DLPI stages) was labeled with 5 μL PI at 1 mg/mL. Flow cytometric measurements were performed using a BD FACSCalibur instrument (Becton Dickinson Biosciences) equipped with an air-cooled argon laser (488 nm emission; 20 mW). The green fluorescent emission from GFP was collected in the FL1 channel (500 to 560 nm), and the red fluorescence from PI was collected in the FL3 channel (670 nm). A threshold was applied to the FL1 channel to eliminate background signals. Analysis was performed at a low-flow-rate setting. The results were analyzed using Cell Quest Pro software (Becton Dickinson Biosciences).
Additional Information
How to cite this article: Allegra, S. et al. Characterization of aerosols containing Legionella generated upon nebulization. Sci. Rep. 6, 33998; doi: 10.1038/srep33998 (2016).
Acknowledgments
We thank Dr. C. Ginevra and Dr. S. Jarraud from the French Reference Center for Legionella for providing us with the GFP-modified strains. We also thank Mathilde Landraud for qPCR analysis during her Master 1 training. This study was supported by a grant from Jean Monnet University, Saint-Etienne, France and by the Agence Nationale de Sécurité Sanitaire (ANSES), France.
Footnotes
Author Contributions S.A. and J.P. designed experiments. S.A., L.L. and P.A.M. conducted the experiments. All authors analyzed the data and wrote and reviewed the manuscript.
References
- La Scola B. et al. Legionella drancourtii sp. nov., a strictly intracellular amoebal pathogen. Int. J. Syst. Evol. Microbiol. 54, 699–703 (2004). [DOI] [PubMed] [Google Scholar]
- Bouwknegt M., Schijven J. F., Schalk J. A. C. & de Roda Husman A. M. Quantitative risk estimation for a Legionella pneumophila infection due to whirlpool use. Risk Anal. Off. Publ. Soc. Risk Anal. 33, 1228–1236 (2013). [DOI] [PubMed] [Google Scholar]
- Chaabna Z. et al. Molecular diversity and high virulence of Legionella pneumophila strains isolated from biofilms developed within a warm spring of a thermal spa. BMC Microbiol. 13, 17 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore G., Hewitt M., Stevenson D., Walker J. T. & Bennett A. M. Aerosolization of respirable droplets from a domestic spa pool and the use of MS-2 coliphage and Pseudomonas aeruginosa as markers for Legionella pneumophila. Appl. Environ. Microbiol. 81, 555–561 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falkinham J. O., Hilborn E. D., Arduino M. J., Pruden A. & Edwards M. A. Epidemiology and ecology of opportunistic premise plumbing pathogens: Legionella pneumophila, Mycobacterium avium, and Pseudomonas aeruginosa. Environ. Health Perspect. 123, 749–758 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnow P. M., Chou T., Weil D., Shapiro E. N. & Kretzschmar C. Nosocomial Legionnaires’ disease caused by aerosolized tap water from respiratory devices. J. Infect. Dis. 146, 460–467 (1982). [DOI] [PubMed] [Google Scholar]
- Woo A. H., Goetz A. & Yu V. L. Transmission of Legionella by respiratory equipment and aerosol generating devices. Chest 102, 1586–1590 (1992). [DOI] [PubMed] [Google Scholar]
- Bou R. & Ramos P. Outbreak of nosocomial Legionnaires’ disease caused by a contaminated oxygen humidifier. J. Hosp. Infect. 71, 381–383 (2009). [DOI] [PubMed] [Google Scholar]
- Cateau E., Delafont V., Hechard Y. & Rodier M. H. Free-living amoebae: what part do they play in healthcare-associated infections? J. Hosp. Infect. 87, 131–140 (2014). [DOI] [PubMed] [Google Scholar]
- Górny R. L., Dutkiewicz J. & Krysińska-Traczyk E. Size distribution of bacterial and fungal bioaerosols in indoor air. Ann. Agric. Environ. Med. AAEM 6, 105–113 (1999). [PubMed] [Google Scholar]
- Campèse C. et al. Legionnaires’ disease in France. Med. Mal. Infect. doi: 10.1016/j.medmal.2015.01.015 (2015). [DOI] [PubMed] [Google Scholar]
- Parr A., Whitney E. A. & Berkelman R. L. Legionellosis on the Rise: A Review of Guidelines for Prevention in the United States. J. Public Health Manag. Pract. JPHMP (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Legionella and the prevention of legionellosis. (Bartram Jamie, Chartier Yves, Lee John V., Pond Kathy & Surman-Lee Susanne, 2007).
- Thomas R. J. et al. Characterization and deposition of respirable large- and small-particle bioaerosols. Appl. Environ. Microbiol. 74, 6437–6443 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron P. A. & Willeke K. Respirable droplets from whirlpools: measurements of size distribution and estimation of disease potential. Environ. Res. 39, 8–18 (1986). [DOI] [PubMed] [Google Scholar]
- Armstrong T. W. & Haas C. N. Quantitative microbial risk assessment model for Legionnaires’ disease: assessment of human exposures for selected spa outbreaks. J. Occup. Environ. Hyg. 4, 634–646 (2007). [DOI] [PubMed] [Google Scholar]
- Ishimatsu S., Miyamoto H., Hori H., Tanaka I. & Yoshida S. Sampling and detection of Legionella pneumophila aerosols generated from an industrial cooling tower. Ann. Occup. Hyg. 45, 421–427 (2001). [PubMed] [Google Scholar]
- Ari A. Jet, Ultrasonic, and Mesh Nebulizers: An evaluation of nebulizers for better clinical outcomes. Eurasian J. Pulmonol. 16, 1–7 (2014). [Google Scholar]
- Robertson P., Abdelhady H. & Garduño R. A. The many forms of a pleomorphic bacterial pathogen-the developmental network of Legionella pneumophila. Front. Microbiol. 5, 670 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allegra S. et al. Longitudinal evaluation of the efficacy of heat treatment procedures against Legionella spp. in hospital water systems by using a flow cytometric assay. Appl. Environ. Microbiol. 77, 1268–1275 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustapha P. et al. Monitoring of Legionella pneumophila viability after chlorine dioxide treatment using flow cytometry. Res. Microbiol. Press (2015). [DOI] [PubMed] [Google Scholar]
- Corsaro D. et al. Novel Chlamydiales strains isolated from a water treatment plant. Environ. Microbiol. 11, 188–200 (2009). [DOI] [PubMed] [Google Scholar]
- Allegra S. et al. Use of flow cytometry to monitor Legionella viability. Appl. Environ. Microbiol. 74, 7813–7816 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epalle T. et al. Viable but not culturable forms of Legionella pneumophila generated after heat shock treatment are Infectious for macrophage-like and alveolar epithelial cells after resuscitation on Acanthamoeba polyphaga. Microb. Ecol. 69, 215–224 (2015). [DOI] [PubMed] [Google Scholar]
- Blatny J. M. et al. Airborne Legionella bacteria from pulp waste treatment plant: aerosol particles characterized as aggregates and their potential hazard. Aerobiologia 27, 147–162 (2010). [Google Scholar]
- Blatny J. M. et al. Dispersion of Legionella-containing aerosols from a biological treatment plant, Norway. Front. Biosci. Elite Ed. 3, 1300–1309 (2011). [DOI] [PubMed] [Google Scholar]
- Faulkner G. & Garduño R. A. Ultrastructural analysis of differentiation in Legionella pneumophila. J. Bacteriol. 184, 7025–7041 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mampel J. et al. Planktonic replication is essential for biofilm formation by Legionella pneumophila in a complex medium under static and dynamic flow conditions. Appl. Environ. Microbiol. 72, 2885–2895 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abdel-Nour M., Duncan C., Low D. E. & Guyard C. Biofilms: the stronghold of Legionella pneumophila. Int. J. Mol. Sci. 14, 21660–21675 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO | Hazard prevention and control in the work environment: Airborne dust (WHO, 1999). WHO Available at: http://www.who.int/occupational_health/publications/airdust/en/. (Accessed: 17th January 2016).
- Pourchez J. et al. Generation and characterization of radiolabelled nanosized carbonaceous aerosols for human inhalation studies. J. Aerosol Sci. 55, 1–11 (2013). [Google Scholar]
- Leclerc L. et al. Impact of airborne particle size, acoustic airflow and breathing pattern on delivery of nebulized antibiotic into the maxillary sinuses using a realistic human nasal replica. Pharm. Res. 31, 2335–2343 (2014). [DOI] [PubMed] [Google Scholar]
- Schlesinger R. B. In McClellan R. O., Henderson R. F. (Eds), Concepts in Inhalation Toxicology 163–192 (Hemisphere Publishing Corp 1989). [Google Scholar]
- Bernstein D. M., Rogers R. & Smith P. The biopersistence of brazilian chrysotile asbestos following inhalation. Inhal. Toxicol. 16, 745–761 (2004). [DOI] [PubMed] [Google Scholar]
- Armstrong T. W. & Haas C. N. A quantitative microbial risk assessment model for Legionnaires’ disease: animal model selection and dose-response modeling. Risk Anal. Off. Publ. Soc. Risk Anal. 27, 1581–1596 (2007). [DOI] [PubMed] [Google Scholar]
- Brieland J. K., Loebenberg D., Menzel F. & Hare R. S. Efficacy of SCH27899 in an animal model of Legionnaires’ disease using immunocompromised A/J mice. Antimicrob. Agents Chemother. 44, 1333–1336 (2000). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edelstein P. H. In Legionella (eds Buchrieser C. & Hilbi H.) 954, 521–540 (Humana Press, 2013). [Google Scholar]
- Hori J. I. & Zamboni D. S. The mouse as a model for pulmonary Legionella infection. Methods Mol. Biol. Clifton NJ 954, 493–503 (2013). [DOI] [PubMed] [Google Scholar]
- Chen D., Zheng X. & Lu Y. Identification and characterization of novel ColE1-type, high-copy number plasmid mutants in Legionella pneumophila. Plasmid 56, 167–178 (2006). [DOI] [PubMed] [Google Scholar]
- Köhler R. et al. Expression and use of the green fluorescent protein as a reporter system in Legionella pneumophila. Mol. Gen. Genet. MGG 262, 1060–1069 (2000). [DOI] [PubMed] [Google Scholar]
- Durand M. et al. Impact of acoustic airflow nebulization on intrasinus drug deposition of a human plastinated nasal cast: new insights into the mechanisms involved. Int. J. Pharm. 421, 63–71 (2011). [DOI] [PubMed] [Google Scholar]
- Leclerc L. et al. Assessing sinus aerosol deposition: benefits of SPECT-CT imaging. Int. J. Pharm. 462, 135–141 (2014). [DOI] [PubMed] [Google Scholar]
- Cormack B. P., Valdivia R. H. & Falkow S. FACS-optimized mutants of the green fluorescent protein (GFP). Gene 173, 33–38 (1996). [DOI] [PubMed] [Google Scholar]