Abstract
Objective
Psychiatric hospitalization is essential in the clinical management of suicidal adolescents, and a considerable number of hospitalized adolescents are rehospitalized, yet little is known about how this experience may influence postdischarge outcomes. This study examined the association between rehospitalization within three months of index hospitalization and subsequent suicide attempts and suicidal ideation among adolescents.
Methods
Participants were 373 youths (13–17 years old) hospitalized because of suicide risk, and they were followed for one year. Using Cox regression, the investigators examined rehospitalization within three months of index hospitalization as a predictor of time to suicide attempt during the subsequent nine months. Using latent-class growth modeling, they also examined whether rehospitalization predicted a change in the nine-month course of three suicidal ideation trajectories (subclinical, elevated but fast declining, and chronically elevated).
Results
Rehospitalization was associated with greater risk of suicide attempts, above the effects of key covariates. Rehospitalization also predicted distinct changes in suicidal ideation trajectories: Within the elevated–fast declining and chronically elevated groups, rehospitalization predicted increases in ideation during the follow-up, with larger magnitude for the chronic group. In contrast, rehospitalization was associated with a decrease in follow-up suicidal ideation in the subclinical group.
Conclusions
Rehospitalization predicted a more severe course of suicide ideation for most of the adolescents, but it was protective for only a smaller subgroup with subclinical levels of ideation at index hospitalization. Our findings also suggest that rehospitalization is a strong indicator of future risk of suicide attempt. These findings have important implications for intervening with rehospitalized adolescents.
During the adolescent years, there is a significant increase in the prevalence of suicidal thoughts and behaviors (1). Approximately 16% and 8% of high school students surveyed nationally reported serious suicidal thoughts and suicide attempts, respectively, in the prior year (2). Psychiatric hospitalization can provide critical services that facilitate safety and stabilization for managing acute psychiatric symptoms and elevated suicide risk. However, a significant number of adolescents continue to experience suicide-related outcomes after discharge, including rehospitalizations, emergency department visits (3), persistent suicidal ideation, and repeated suicidal behavior (4–7). Adolescent rehospitalization rates are high: 19%–28% are rehospitalized within six months (3,8), 38% within one year (9), and up to 43% within 2.5 years after discharge (10). The risk of rehospitalization is especially elevated during the first three months after discharge (9–11). Although our understanding of the correlates of rehospitalization has expanded (8–13), less is known about the implications of this experience for the subsequent course of suicide-related outcomes, such as suicidal ideation and suicide attempts. Consequently, further attention is warranted to examine whether rehospitalization is associated with chronic or remitting clinical trajectories among youths at high risk of suicide.
High rates of rehospitalization, particularly among suicide-related admissions (3), highlight the chronicity of psychiatric crises after discharge and raise questions about the effectiveness of hospitalization and existing aftercare interventions. Although most adolescents receive outpatient services postdischarge (14), receiving these services does not appear to be linked with significantly improved suicide-related outcomes, such as reduced likelihood of suicide attempts or decreases in suicidal ideation (6,14–16). More generally, these findings are consistent with a paucity of efficacious interventions for suicidal adolescents (17,18). Past work examining the impact of aftercare services on risk of rehospitalization has also yielded mixed findings (10,12,19). In light of the challenge of intervening with high-risk youths and the facts that hospitalization is not intended to resolve long-standing difficulties and that premature discontinuation of outpatient treatment is common (6,20), it is not surprising that a substantial number of previously hospitalized adolescents continue to experience difficulties after being discharged (4,21).
Inpatient hospitalization is considered essential in the clinical management of acutely suicidal adolescents (22), and recent estimates indicate that inpatient admission rates for youths have been increasing (23). However, empirical data are lacking in regard to the impact on postdischarge suicide-related outcomes (18,24). We are aware of two studies examining hospitalization in relation to suicide-related outcomes (25,26); however, their findings were inconclusive. Moreover, the costs associated with psychiatric hospitalization may include financial strain, enduring stigma, and negative impact on the hospitalized individual’s identity and hope for the future (27). On a broader level, hospitalization of adolescents for self-inflicted injuries costs the U.S. health care system $615 million annually (28), necessitating an examination of these services.
The purpose of this study was to examine the extent to which rapid rehospitalization (that is, within three months of discharge) predicts suicide attempts and influences the course of suicidal ideation within a subsequent nine-month period. With the challenges of intervening with suicidal adolescents and the brevity of hospitalizations, we anticipated that rehospitalization would be associated with modest reductions in suicidal ideation and suicide attempts.
METHODS
Participants and Procedures
Participants were 373 adolescents, ages 13 to 17, who were psychiatrically hospitalized at two Midwestern hospitals because of acute suicidal ideation or a recent suicide attempt and who were followed for one year. The sample was drawn from data from a randomized clinical trial of a psychosocial intervention (29). Adolescents were eligible for inclusion if they or a parent reported on the Diagnostic Interview Schedule for Children (DISC-IV; 30) a past-month suicide attempt or suicidal ideation that was either unrelenting or accompanied by a specific plan. Exclusion criteria included cognitive impairment, transfer to other inpatient services, residence more than an hour away from study site, and absent legal guardian. Study eligibility criteria were determined on the basis of hospital admission records, and eligible adolescents were approached to participate. Legal guardians provided written informed consent, and adolescents provided informed assent to a protocol approved by the participating university’s institutional review board. Data collection took place between November 2002 and December 2006. Participants were assessed within one week of hospitalization, and follow-up data were collected three, six, and 12 months later. Retention of participants was as follows: 342 (76%) participants at three months, 314 (70%) at six months, and 346 (77%) at 12 months. A more detailed description of participant recruitment and retention has been reported previously (29).
The analytic sample consisted of participants with data on mental health services obtained within three months of discharge and at least one subsequent assessment. The analytic sample (83% of the original sample of 448, for a final sample of N=373) did not differ from excluded adolescents with regard to sex, age, race, use of public assistance, the predictors of interest, and suicide attempt history.
Measures
Suicidal ideation and suicide attempts
Lifetime multiple attempt status, assessed at baseline, and suicide attempts as of each of the follow-up points were assessed with suicide attempt items from the DISC-IV (30). Severity of suicidal ideation was assessed at each follow-up point with the self-reported 15-item Suicidal Ideation Questionnaire–Junior (SIQ-JR) scale (31).
Baseline psychiatric symptoms
Depressive symptoms were assessed with the Children’s Depression Rating Scale—Revised (32). Hopelessness was assessed with the 20-item Beck Hopelessness Scale (33). Externalizing symptoms were assessed with the external problems subscale from the Youth Self-Report (34), which measures delinquent and aggressive behaviors. Substance use was assessed with the 18-item problem severity scale from the Personal Experience Screening Questionnaire (35,36), which measures the frequency of behaviors related to alcohol and drug abuse.
Baseline connectedness
Perception of family connectedness was measured with items from the Perceived Emotional/Personal Support Scale (37), which assesses perception of relationships as being close, confiding, satisfying, and supportive.
Psychiatric rehospitalization
A dichotomous variable was created (yes-no) based on two questions inquiring whether a participant was in a psychiatric hospital or a general hospital for psychiatric or emotional problems. Rehospitalization was measured within three months of index hospitalization.
Data Analysis
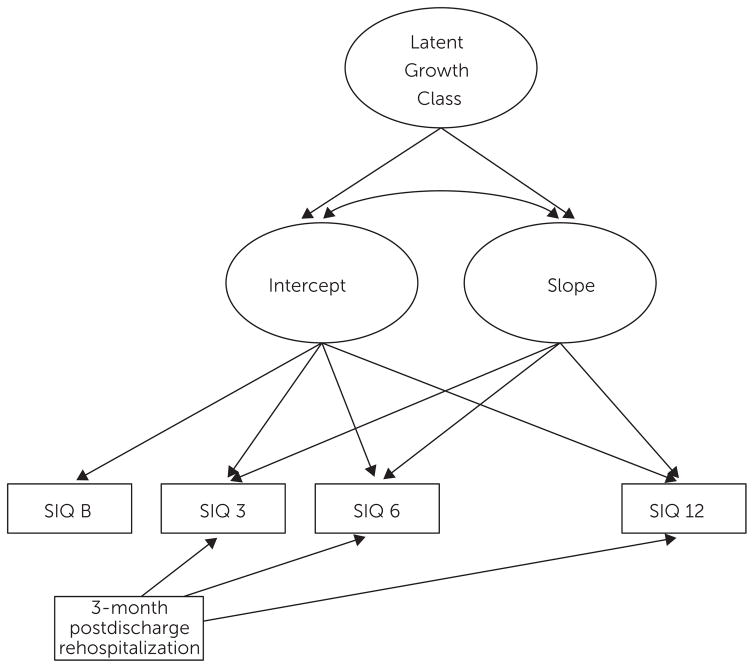
We used latent-class growth modeling (LCGM) and implemented it with a PROC TRAJ procedure (38) in SAS (version 9.2). We extend previous findings in which LCGM identified three suicidal ideation trajectory groups (subclinical, elevated but rapidly declining, and chronically elevated) by using the SIQ score obtained at baseline and the SIQ score at three, six, and 12 months after hospitalization (4). Using a modeling approach proposed by Jones and Nagin (39,40), we extended these analyses to examine whether rehospitalization within three months of discharge enhanced or attenuated the subsequent course of suicidal ideation trajectories, that is, SIQ assessed after the rehospitalization. The hypothesized model is shown in Figure 1.
FIGURE 1. Hypothesized 12-month rehospitalization model for adolescents with suicidal ideationa.
aThe model depicts latent growth classes of Suicidal Ideation Questionnaire–Junior (SIQ) scores. Rehospitalization between baseline (SIQ B) and month 3 (SIQ 3) is included as a predictor of the course of each trajectory after rehospitalization. For graphic simplicity, only the intercept and one slope are shown.
An advantage of examining the influence of rehospitalization within multiple trajectory groups—rather than across averaged suicidal ideation for the whole sample—is the simultaneous accounting for ideation severity at hospitalization and follow-up such that differences between rehospitalized and nonrehospitalized adolescents within trajectories are minimized. We also controlled for covariates that may influence the likelihood of rehospitalization and trajectory group membership. Thus the analysis allowed for examining whether rehospitalization is associated with a different course of ideation within an otherwise similar group. [Additional details concerning data-analytic procedures are provided in an online supplement to this article.] Because the sample was drawn from an intervention study, we controlled for intervention effects; however, because it was nonsignificant and did not alter the results, intervention assignment was removed from the final model.
We examined whether rehospitalization within the first three months after baseline served to predict time to suicide attempt in the subsequent nine-month period. We controlled for key covariates and estimated a Cox proportional hazards regression in the SPSS (version 21). Number of days to suicide attempt was used as a continuous measure of time. This analysis maximizes use of data by censoring participants lost to follow-up at the last nonmissing assessment. The proportional hazards assumption was examined with the time-dependent covariates test; the interaction between the time variable and rehospitalization was not significant, suggesting that the assumption was met.
RESULTS
Sample Characteristics
Participants were predominantly female (72%, N=269) with a mean age of 15.6±1.3 years. The racial-ethnic sample composition was 83% (N=308) Caucasian, 7% (N=26) African American, 1% (N=2) Asian American/Pacific Islander, 2% (N=8) Hispanic, 1% (N=3) Native American, and 7% (N=26) “other” or not identified.
A total of 80 (21%) adolescents were rehospitalized within the first three months of index hospitalization. Rehospitalized participants tended to score higher on baseline measures of psychopathology (Table 1). Although these differences were not statistically significant, a greater proportion of boys than girls (24% versus 20%) and a greater proportion of youths with multiple suicide attempt history versus those without (25% versus 19%) were rehospitalized.
TABLE 1.
Characteristics of adolescents with suicidal ideation who were or were not rehospitalized within one year of discharge
| Baseline characteristic | Overall sample
|
Rehospitalization
|
pa | ||||
|---|---|---|---|---|---|---|---|
| Yes
|
No
|
||||||
| M | SD | M | SD | M | SD | ||
| Suicidal ideation (SIQ-JR)b | 46.43 | 20.73 | 53.70 | 18.03 | 44.44 | 21.01 | <.001 |
| Depressive symptoms (CDRS-R)c | 60.80 | 12.80 | 64.85 | 10.69 | 59.71 | 13.11 | <.001 |
| Hopelessness (BHS)d | 8.74 | 5.79 | 10.41 | 6.07 | 8.29 | 5.64 | .004 |
| Substance abuse (PESQ)e | 27.99 | 11.52 | 27.22 | 11.11 | 28.21 | 11.63 | ns |
| Externalizing problems (YSR–external problems)f | 21.38 | 9.71 | 23.08 | 11.16 | 20.91 | 9.23 | .077 |
| Family connectedness (PEPSS–Family)g | 8.30 | 2.10 | 8.15 | 2.25 | 8.34 | 2.05 | ns |
Two-sample t test (two-sided). The Ns varied between 369 and 372 for the overall sample, between 289 and 293 for youths who were not rehospitalized, and between 79 and 80 for youths who were rehospitalized.
Suicidal Ideation Questionnaire–Junior. Possible scores range from 0 to 90, with higher scores indicating more severe suicidal ideation.
Children’s Depression Rating Scale–Revised. Possible scores range from 17 to 113, with higher scores indicating more severe depressive symptoms.
Beck Hopelessness Scale. Possible scores range from 0 to 20, with higher scores indicating greater hopelessness.
Personal Experience Screening Questionnaire. Possible scores range from 18 to 72, with higher scores indicating more severe substance abuse.
Youth Self-Report–Externalizing. Possible scores range from 0 to 64, with higher scores indicating more severe externalizing problems.
Perceived Emotional/Personal Support Scale. Possible scores range from 1 to 12, with higher scores indicating greater family connectedness.
There were no differences in symptom severity between rehospitalized and nonrehospitalized adolescents within each ideation trajectory group, suggesting that clinical differences were minimized. However, rehospitalized adolescents in the elevated–fast declining trajectory (group 2) had higher externalizing scores (mean±SD=25.84±12.07) than those not hospitalized (22.13±8.61) (p=.05). Rehospitalized adolescents in the chronically elevated trajectory (group 3) had lower externalizing scores (19.33±7.57) than adolescents who were not rehospitalized (26.10±11.79) (p=.04).
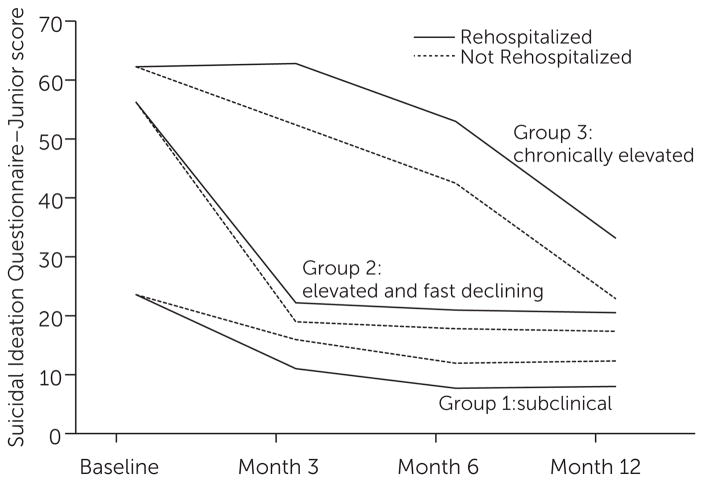
Rehospitalization and Course of Suicidal Ideation
Approximately 9% (N=11) of adolescents in the subclinical ideation trajectory (group 1; N=118), 24% (N=51) in the elevated but rapidly declining ideation trajectory (group 2; N=213), and 46% (N=18) in the chronically elevated ideation trajectory (group 3; N=39) were rehospitalized within the first three months of discharge. Table 2 describes the effects of rehospitalization as a predictor of suicidal ideation course and accounts for baseline covariates (depressive symptoms, hopelessness, externalizing problems, sex, and whether they had made multiple suicide attempts) as well as suicidal ideation severity at baseline and follow-up (ideation trajectory). Rehospitalization had a significant moderating effect for all groups. Rehospitalization was associated with significantly increasing suicidal ideation for the elevated–fast declining (group 2) and the chronic (group 3) trajectories during follow-up, with larger effects for the chronic group. Conversely, for the subclinical trajectory (group 1), the effect of rehospitalization was associated with less severe suicidal ideation during follow-up (Figure 2).
TABLE 2.
Effect of rehospitalization on latent suicidal ideation trajectories of adolescentsa
| Trajectory | B (rehospitalization) | SE(B) | p |
|---|---|---|---|
| Group 1: subclinical ideation | −6.08 | 2.89 | .036 |
| Group 2: elevated and fast declining | 3.45 | 1.62 | .034 |
| Group 3: chronically elevated | 10.52 | 2.85 | <.001 |
N=370. Analyses adjusted for sex, multiple-attempt history, depressive symptoms, hopelessness, and externalizing problems. Controlling for number of previous hospitalizations did not change the pattern of results.
FIGURE 2. Impact of rehospitalization on trajectories of suicidal ideation among adolescentsa.
aPossible scores range from 0 to 90, with a published clinical cutoff score of 31. The analysis adjusted for baseline depressive symptoms, hopelessness, externalizing problems, history of multiple suicide attempts, and sex. Controlling for number of previous hospitalizations did not change the pattern of the results.
Rehospitalization and Time to Suicide Attempt
After the initial three-month period in which rehospitalization was tracked after the index hospitalization, 45 adolescents (12%) attempted suicide at least once in the subsequent nine-month period. Twenty-six (9%) of those who were not rehospitalized (N=284) attempted suicide compared with 19 (26%) of those who were rehospitalized (N=74) and who attempted suicide during this period. Rehospitalization was significantly associated with increased risk of postdischarge suicide attempts during this nine-month period (hazard ratio=3.13, p<.001), even after we controlled for baseline depressive symptoms, suicidal ideation, hopelessness, externalizing problems, multiple suicide attempt history, and sex (Table 3). In additional analysis, we explored whether the effect of rehospitalization was moderated by any of the covariates. Significant interaction effects identified involved baseline suicidal ideation (B=−.03, SE[B]= .02, p=.048) and externalizing problems (B=−.09, SE[B]=.04, p=.01), suggesting that the association between rehospitalization and suicide attempts was stronger for those with more severe ideation and externalizing problems at index hospitalization.
TABLE 3.
Cox regression model predicting time to suicide attempt among adolescentsa
| Variable | B | SE(B) | Hazard ratio | 95% CI | p |
|---|---|---|---|---|---|
| Male (reference: female) | −.050 | .36 | .95 | .47–1.91 | ns |
| Multiple attempts (reference: no) | .560 | .31 | 1.75 | .95–3.22 | .074 |
| Suicidal ideation | .002 | .01 | 1.00 | .98–1.02 | ns |
| Depressive symptoms | .010 | .01 | 1.01 | .98–1.03 | ns |
| Hopelessness | −.010 | .03 | .99 | .94–1.06 | ns |
| Externalizing problems | −.020 | .02 | .98 | .95–1.02 | ns |
| Rehospitalization (reference: no) | 1.140 | .32 | 3.13 | 1.66–5.89 | <.001 |
N=352. Controlling for number of previous hospitalizations did not change the pattern of results.
DISCUSSION
This prospective study considered the extent to which psychiatric rehospitalization within the critical three-month period after discharge predicted suicide-related outcomes among acutely suicidal adolescents. Specifically, we examined whether there was an enduring relationship between rehospitalization and severity of suicidal ideation as well as time to suicide attempt in the subsequent nine months. We had identified three distinct profiles of adolescents characterized by differing patterns of suicidal ideation over a 12-month period after discharge wherein some adolescents followed a subclinical course of ideation, others experienced highly elevated but rapidly declining ideation, and another group had chronically elevated ideation (4). Our study extends previous findings by conducting a finer-grained examination of the influence of rehospitalization on the course of suicidal ideation while accounting for suicidal ideation severity at index hospitalization and throughout the follow-up, thus minimizing potentially confounding differences. We found that rehospitalization altered the course of suicidal ideation in these three groups in distinct ways. Within the chronically elevated and elevated–fast-declining trajectory groups, rehospitalization—relative to no rehospitalization—was associated with significant increases in suicidal ideation over the follow-up. The magnitude of this effect was much larger for adolescents in the chronically elevated trajectory. In contrast, rehospitalization was associated with a decrease in suicidal ideation in the subclinical group.
These findings highlight the importance of recognizing that acutely suicidal adolescents, although vulnerable to suicidal crises as a group, comprise a heterogeneous population where treatment decisions may interact with individual differences to yield distinct outcomes. Furthermore, for the overall sample, we found that rehospitalization was uniquely associated with earlier recurrence of suicide attempts even after taking into account baseline levels of depressive symptoms, hopelessness, externalizing behaviors, suicidal ideation, history of multiple suicide attempts, and sex. Significant interactions suggested that this association was stronger for those with more severe ideation and externalizing problems at index hospitalization. Whether cause or consequence, rehospitalization in this population is a clinical indicator of the severity and chronicity of suicide risk. It was strongly associated with recurrence of suicide risk in the form of elevated suicidal ideation as well as suicide attempts.
There are a number of potential explanations for the relationships found here. First, results are consistent with past findings highlighting the chronic nature of suicide risk (5,7) as well as the limited efficacy of interventions to prevent severe suicidal ideation and suicide attempts (17,18,41). A recent nationally representative study found that a majority of suicidal adolescents were receiving mental health services before the onset of suicidal behavior (1). With these findings in mind, it is less surprising that rehospitalization was not uniformly associated with lower risk among acutely suicidal youths after discharge.
Second, psychiatric hospitalization may have iatrogenic effects for a subset of suicidal adolescents. As has been argued by Linehan (42), the attentive responsiveness to reported suicidal ideation or self-injury that characterizes hospitalization may act as an unintended reinforcement of self-harmful behaviors. Moreover, hospitalization may disrupt the positive aspects of some suicidal adolescents’ lives, such as positive peer or family relationships and age-appropriate engagement in social activities. At the same time, acknowledging that interpersonal factors may also serve as risk factors is important. For example, disengaged parent-child relationships have been identified as a contributor to rehospitalization (11). Hospitalization may also unintentionally exacerbate hopelessness (failed outpatient treatment) or contribute to an identity as an “ill” person or someone with low self-efficacy for coping and benefiting from treatment. However, given that this was a naturalistic study, drawing conclusions about iatrogenic effects would be premature; instead, it may be more fitting to describe rehospitalization as a marker of chronicity of risk. In addition, although psychiatric hospitalization is critical to the treatment of acutely suicidal adolescents (22), its goals are often constrained to maintaining safety and facilitating linkage to appropriate outpatient services rather than to remission of psychopathology and significant modification of the environmental context. Consequently, some of the relevant precipitants of crisis may be too long-standing to be addressed within the course of hospitalization.
Nevertheless, the fact that rehospitalization was prospectively associated with a more severe course of suicide ideation and a more imminent risk of suicide attempts is of concern. Moreover, because rehospitalization was associated with a more pronounced increase in suicidal ideation in the chronically elevated ideation group, it is possible that rehospitalization may especially negatively affect adolescents at chronic risk of self-harm. This is consistent with the hypothesis that hospitalization may be clinically contraindicated for some forms of psychopathology, such as borderline personality disorder, because it may unintentionally reinforce suicide-related behaviors (42). However, we did not assess personality disorders in our study, and thus this inference warrants caution.
The predominantly female and Caucasian sample has limited generalizability to other adolescent groups. The strength of our conclusions is especially tempered by the fact that examining the relationship between rehospitalization and suicide-related outcomes in a naturalistic study does not allow for ruling out the possibility that findings may be influenced by factors for which we were not able to account (including health insurance coverage, outpatient providers’ risk management practices, readmission psychiatric status, emotional liability, and impulsive aggression). Although controlling for key covariates in this study minimized this possibility, future work should consider other factors. Another factor that warrants closer consideration is the role of aftercare services. Specifically, we were not able to establish the temporal relationship between rehospitalization and delivery of aftercare services.
However, participation in services was high during the first three months after discharge (only 4% of the sample did not attend any sessions), and controlling for number of sessions attended did not affect results reported here. Rehospitalized youths generally attended more sessions within this period compared with youths who were not rehospitalized. Future studies should examine aftercare services in greater detail to assess their impact on posthospitalization trajectories, including youths’ adherence to these services. Finally, the retrospective recall of dates of attempts at follow-up assessments is another important limitation. Despite these limitations, this study has addressed an important gap in the literature and has important strengths, including a large sample of acutely suicidal adolescents and prospective design.
CONCLUSIONS
To our knowledge, this is the first prospective study examining the link between rehospitalization and suicide-related outcomes among suicidal adolescents. Our findings suggest that rehospitalization shortly after discharge is a significant event. For most adolescents, rehospitalization was associated with a more severe course of suicidal ideation; for a smaller subgroup reporting subclinical ideation at index hospitalization, it was protective. Rehospitalization may be a significant vulnerability factor, signaling increased suicide attempt risk. Although these results raise questions about possible iatrogenic effects of rehospitalization, without understanding the mechanisms accounting for the associations found here, firm conclusions are premature. Given the exploratory nature of the analytic approach utilized (LCGM) and the inability to consider all possibly pertinent covariates (including adequately accounting for the role of aftercare services), cross-validation and replication of findings are necessary. However, our findings have implications for intervening with readmitted adolescents, including the need for posthospitalization services, addressing potentially self-defeating cognitions about hospitalization, and addressing realistic expectations with adolescents and families. More studies are needed to investigate further how and why rehospitalization influences these youths’ posthospitalization functioning. Studying adolescents’ subjective experiences may help clarify why rehospitalization is associated with increased vulnerability to suicidal crises.
Acknowledgments
Support for this project was provided by grant R01 MH63881 and Mid-career Investigator Award K24MH77705 from the National Institute of Mental Health to Dr. King. The authors thank Sanjeev Venkataraman, M.D., and Paul Quinlan, M.D., for administrative and risk management support and Anne Kramer, M.S.W., A.C.S.W., Barbara Hanna, Ph.D., and Lois Weisse, R.N., for project management. The authors also thank the research staff, participating inpatient staff, and the adolescent participants and their parents and guardians.
Footnotes
The authors report no financial relationships with commercial interests.
References
- 1.Nock MK, Green JG, Hwang I, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70:300–310. doi: 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Youth Risk Behavior Surveillance—United States, 2013. Morbidity and Mortality Weekly Report. 2014;63(4):1–168. [Google Scholar]
- 3.Yen S, Weinstock LM, Andover MS, et al. Prospective predictors of adolescent suicidality: 6-month post-hospitalization follow-up. Psychological Medicine. 2013;43:983–993. doi: 10.1017/S0033291712001912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Czyz EK, King CA. Longitudinal trajectories of suicidal ideation and subsequent suicide attempts among adolescent inpatients. Journal of Clinical Child and Adolescent Psychology. 2015;44:181–193. doi: 10.1080/15374416.2013.836454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goldston DB, Daniel SS, Reboussin DM, et al. Suicide attempts among formerly hospitalized adolescents: a prospective naturalistic study of risk during the first 5 years after discharge. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:660–671. doi: 10.1097/00004583-199906000-00012. [DOI] [PubMed] [Google Scholar]
- 6.King CA, Segal H, Kaminski K, et al. A prospective study of adolescent suicidal behavior following hospitalization. Suicide and Life-Threatening Behavior. 1995;25:327–338. [PubMed] [Google Scholar]
- 7.Prinstein MJ, Nock MK, Simon V, et al. Longitudinal trajectories and predictors of adolescent suicidal ideation and attempts following inpatient hospitalization. Journal of Consulting and Clinical Psychology. 2008;76:92–103. doi: 10.1037/0022-006X.76.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arnold EM, Goldston DB, Ruggiero A, et al. Rates and predictors of rehospitalization among formerly hospitalized adolescents. Psychiatric Services. 2003;54:994–998. doi: 10.1176/appi.ps.54.7.994. [DOI] [PubMed] [Google Scholar]
- 9.Fontanella CA. The influence of clinical, treatment, and healthcare system characteristics on psychiatric readmission of adolescents. American Journal of Orthopsychiatry. 2008;78:187–198. doi: 10.1037/a0012557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.James S, Charlemagne SJ, Gilman AB, et al. Post-discharge services and psychiatric rehospitalization among children and youth. Administration and Policy in Mental Health and Mental Health Services Research. 2010;37:433–445. doi: 10.1007/s10488-009-0263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blader JC. Symptom, family, and service predictors of children’s psychiatric rehospitalization within one year of discharge. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:440–451. doi: 10.1097/00004583-200404000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Foster EM. Do aftercare services reduce inpatient psychiatric readmissions? Health Services Research. 1999;34:715–736. [PMC free article] [PubMed] [Google Scholar]
- 13.Romansky JB, Lyons JS, Lehner RK, et al. Factors related to psychiatric hospital readmission among children and adolescents in state custody. Psychiatric Services. 2003;54:356–362. doi: 10.1176/appi.ps.54.3.356. [DOI] [PubMed] [Google Scholar]
- 14.Daniel SS, Goldston DB, Harris AE, et al. Review of literature on aftercare services among children and adolescents. Psychiatric Services. 2004;55:901–912. doi: 10.1176/appi.ps.55.8.901. [DOI] [PubMed] [Google Scholar]
- 15.Asarnow JR, Baraff LJ, Berk M, et al. An emergency department intervention for linking pediatric suicidal patients to follow-up mental health treatment. Psychiatric Services. 2011;62:1303–1309. doi: 10.1176/appi.ps.62.11.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pfeffer CR, Peskin JR, Siefker CA. Suicidal children grow up: psychiatric treatment during follow-up period. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:679–685. doi: 10.1097/00004583-199207000-00015. [DOI] [PubMed] [Google Scholar]
- 17.Brent DA, McMakin DL, Kennard BD, et al. Protecting adolescents from self-harm: a critical review of intervention studies. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52:1260–1271. doi: 10.1016/j.jaac.2013.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gould MS, Greenberg T, Velting DM, et al. Youth suicide risk and preventive interventions: a review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:386–405. doi: 10.1097/01.CHI.0000046821.95464.CF. [DOI] [PubMed] [Google Scholar]
- 19.Carlisle CE, Mamdani M, Schachar R, et al. Aftercare, emergency department visits, and readmission in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51:283–293. doi: 10.1016/j.jaac.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 20.King CA, Hovey JD, Brand E, et al. Suicidal adolescents after hospitalization: parent and family impacts on treatment follow-through. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:85–93. doi: 10.1097/00004583-199701000-00021. [DOI] [PubMed] [Google Scholar]
- 21.Halliday-Boykins CA, Henggeler SW, Rowland MD, et al. Heterogeneity in youth symptom trajectories following psychiatric crisis: predictors and placement outcome. Journal of Consulting and Clinical Psychology. 2004;72:993–1003. doi: 10.1037/0022-006X.72.6.993. [DOI] [PubMed] [Google Scholar]
- 22.American Academy of Child and Adolescent Psychiatry. Practice parameter for the assessment and treatment of children and adolescents with suicidal behavior. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(suppl):24S–51S. doi: 10.1097/00004583-200107001-00003. [DOI] [PubMed] [Google Scholar]
- 23.Blader JC. Acute inpatient care for psychiatric disorders in the United States, 1996 through 2007. Archives of General Psychiatry. 2011;68:1276–1283. doi: 10.1001/archgenpsychiatry.2011.84. [DOI] [PubMed] [Google Scholar]
- 24.National Strategy for Suicide Prevention. Goals and Objectives for Action. Washington, DC: US Department of Health and Human Services, Office of the Surgeon General and National Action Alliance for Suicide Prevention; 2012. [PubMed] [Google Scholar]
- 25.Waterhouse J, Platt S. General hospital admission in the management of parasuicide: a randomised controlled trial. British Journal of Psychiatry. 1990;156:236–242. doi: 10.1192/bjp.156.2.236. [DOI] [PubMed] [Google Scholar]
- 26.Huey SJ, Jr, Henggeler SW, Rowland MD, et al. Multisystemic therapy effects on attempted suicide by youths presenting psychiatric emergencies. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:183–190. doi: 10.1097/00004583-200402000-00014. [DOI] [PubMed] [Google Scholar]
- 27.Comtois KA, Linehan MM. Psychosocial treatments of suicidal behaviors: a practice-friendly review. Journal of Clinical Psychology. 2006;62:161–170. doi: 10.1002/jclp.20220. [DOI] [PubMed] [Google Scholar]
- 28.Olfson M, Gameroff MJ, Marcus SC, et al. National trends in hospitalization of youth with intentional self-inflicted injuries. American Journal of Psychiatry. 2005;162:1328–1335. doi: 10.1176/appi.ajp.162.7.1328. [DOI] [PubMed] [Google Scholar]
- 29.King CA, Klaus N, Kramer A, et al. The Youth-Nominated Support Team–Version II for suicidal adolescents: a randomized controlled intervention trial. Journal of Consulting and Clinical Psychology. 2009;77:880–893. doi: 10.1037/a0016552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shaffer D, Fisher P, Lucas C, et al. Diagnostic Interview Schedule for Children (Youth Informant and Parent Informant Interviews): Epidemiologic Version. New York: Columbia University, Division of Child Psychiatry, Joy and William Ruane Center to Identify and Treat Mood Disorders; 1998. DISC–IV. [Google Scholar]
- 31.Reynolds WM. Suicidal Ideation Questionnaire: Professional Manual. Odessa, Fla: Psychological Assessment Resources; 1988. [Google Scholar]
- 32.Poznanski EO, Mokros HB. Children’s Depression Rating Scale–Revised (CDRS-R) Los Angeles: Western Psychological Services; 1996. [Google Scholar]
- 33.Beck AT, Steer RA. Beck Hopelessness Scale Manual. San Antonio, Tex: Psychological Corp; 1988. [Google Scholar]
- 34.Achenbach TM. Manual for the Youth Self-Report and 1991 Profile. Burlington, Vt: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- 35.Winters KC. Personal Experience Screen Questionnaire (PESQ) Manual. Los Angeles: Western Psychological Services; 1991. [Google Scholar]
- 36.Winters KC. Development of an adolescent alcohol and other drug abuse screening scale: Personal Experience Screening Questionnaire. Addictive Behaviors. 1992;17:479–490. doi: 10.1016/0306-4603(92)90008-j. [DOI] [PubMed] [Google Scholar]
- 37.Slavin LA. Validation studies of the PEPSS, a measure of perceived emotional support for use with adolescents. Journal of Adolescent Research. 1991;6:316–335. [Google Scholar]
- 38.Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociological Methods and Research. 2001;29:374–393. [Google Scholar]
- 39.Jones BL, Nagin DS. Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociological Methods and Research. 2007;35:542–571. [Google Scholar]
- 40.Nagin DS, Pagani L, Tremblay RE, et al. Life course turning points: the effect of grade retention on physical aggression. Development and Psychopathology. 2003;15:343–361. doi: 10.1017/s0954579403000191. [DOI] [PubMed] [Google Scholar]
- 41.Corcoran J, Dattalo P, Crowley M, et al. A systematic review of psychosocial interventions for suicidal adolescents. Children and Youth Services Review. 2011;33:2112–2118. [Google Scholar]
- 42.Linehan M. Cognitive-Behavioral Treatment of Borderline Personality Disorder. New York: Guilford; 1993. [Google Scholar]