Abstract
Background: Evidence increasingly indicates that poor sleep quality is a major public health concern. Household food insecurity (HFI) disproportionately affects Latinos and is a novel risk factor for poor sleep quality. Psychological distress may be a potential mechanism through which HFI affects sleep quality. Sleep, food insecurity, and distress are linked to type 2 diabetes mellitus.
Objectives: We examined the relations between HFI, psychological distress, and sleep quality and tested whether psychological distress mediates the relation between HFI and sleep in people with diabetes mellitus.
Methods: Latinos with type 2 diabetes mellitus (n = 121) who completed baseline assessments for the CALMS-D (Community Health Workers Assisting Latinos Manage Stress and Diabetes) stress management intervention trial completed the US Household Food Security Survey, and measures of depressive symptoms [Personal Health Questionnaire Depression Scale (PHQ-8)], anxiety symptoms [Patient-Reported Outcomes Measurement Information System (PROMIS)-short], diabetes distress [Problem Areas in Diabetes Questionnaire (PAID-5)], and sleep quality [Pittsburgh Sleep Quality Index (PSQI)]. Psychological distress was operationalized with the PHQ-8, PROMIS-short, and PAID-5 scales. We used unadjusted and adjusted indirect effect tests with bias-corrected bootstrapped 95% CIs on 10,000 samples to test both relations between variables and potential mediation.
Results: Mean age was 61 y, 74% were women, and 67% were food insecure. Experiencing HFI was associated with both greater psychological distress and worse sleep quality (P < 0.05). Depressive symptoms (adjusted R2: 2.22, 95% CI: 1.27, 3.42), anxiety symptoms (adjusted R2: 1.70, 95% CI: 0.87, 2.85), and diabetes mellitus distress (adjusted R2: 0.60, 95% CI: 0.11, 1.32) each mediated the relation between HFI and worse sleep quality with and without adjustment for age, education, income, marital status, and employment status.
Conclusions: Household food insecurity is a common and potent household stressor that is associated with suboptimal sleep quality through psychological distress. Efforts to improve food security and decrease psychological distress may yield improved sleep in this high-risk population. The CALMS-D stress management trial was registered at clinicaltrials.gov as NCT01578096.
Keywords: psychological distress, household food insecurity, sleep quality, Latinos, diabetes
Introduction
Evidence increasingly indicates that poor sleep quality is a major public health concern. Sleep is a basic biological need that, when disturbed, is associated with metabolic disease risk (1–6), including diabetes mellitus (7, 8). The present guidelines recommend 7–8 h of sleep within a 24-h period for adults to maintain good health (9); however, an estimated 35% of people report <7 h of sleep during a typical 24-h period during the day ≥1 time in the past month (10). In addition, the amount of sleep differs between ethnic groups, with Latinos reporting an average sleep time of 6 h 34 min (11). Latinos also are more likely than other racial/ethnic groups to report that they are kept awake by financial, employment, and personal relationship and/or health-related concerns. Overall, 38% of Latinos report that these concerns disturb their sleep at least a few nights per week, compared with 28% of non-Hispanic whites (11).
Food insecurity is a novel risk factor for the development of sleep problems and, subsequently, chronic disease, both of which affect Latinos disproportionately (12–14). Food insecurity is the limited or uncertain availability of nutritionally adequate and safe foods or the limited or uncertain ability to acquire acceptable foods in socially acceptable ways (e.g., without resorting to emergency food supplies, scavenging, stealing, or other coping strategies) (15). In 2014, 14.0% (17.4 million) of all US households were food insecure and the prevalence was higher for Latinos (22.4%) than for non-Hispanic white households (10.5%) (16). Food insecurity is associated with an increased risk of developing type 2 diabetes mellitus (T2DM).9 T2DM, once diagnosed, also is associated with a person being less adherent to recommended self-care activities (17) and, in turn, suboptimal glycemic control (18–20).
Psychological distress may be a mechanism through which food insecurity affects sleep quality. Household food insecurity (HFI) is a major stressor (21) that is associated with depression and diabetes distress (21) and anxiety (22, 23). Sleep and wakefulness are disrupted by a variety of factors, including those that are physiologic, behavioral, and environmental (24). It also is well documented that psychological distress disturbs sleep (25–28).
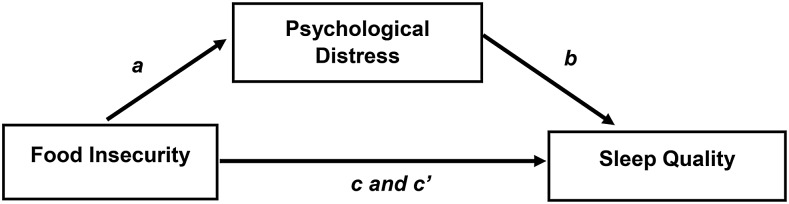
To understand the relations between HFI, psychological distress, and suboptimal sleep quality and predicted pathways, we used baseline data from the CALMS-D (Community Health Workers Assisting Latinos Manage Stress and Diabetes) randomized controlled trial (20, 29) in Latinos with T2DM. We hypothesized that food insecurity would be associated with poor sleep quality, and psychological distress would mediate this relation (Figure 1).
FIGURE 1.
Conceptual framework used to examine the relations and predicted pathways between HFI, psychological distress, and suboptimal sleep quality in Latinos with type 2 diabetes mellitus. HFI to psychological distress (a path); psychological distress to suboptimal sleep quality (b path); total effect of HFI on suboptimal sleep quality (c path). Direct effect of HFI on suboptimal sleep quality (c′ path). Indirect and standardized effects of HFI on suboptimal sleep quality via psychological distress (a and b paths) and 95% bootstrapped CI. HFI, household food insecurity.
Methods
Setting and sample
The CALMS-D study was a research collaboration between Yale University School of Public Health, UConn (University of Connecticut) Health, Hartford Hospital, and the Hispanic Health Council, a nonprofit, community-based research, service, training, and advocacy organization. This study was approved by the institutional review boards of all of the involved institutions and was registered at clinicaltrials.gov as NCT01578096.
Participants were recruited from the Brownstone Clinic, an outpatient clinic at Hartford Hospital, serving low-income patients with diabetes mellitus, ∼80% of whom are Latino. Participants were adult residents of Hartford, Connecticut, self-identifying as Latino or Hispanic, Spanish speaking, ambulatory, with T2DM for ≥6 mo, and most-recent-past-year glycated hemoglobin concentrations ≥7.0%. Glycated hemoglobin reflects blood glucose concentrations during the previous 6–12 wk and is the gold standard indicator of glycemic control (30). The chart review excluded patients for medical instability or intensive medical treatment, bipolar or thought disorder, or suicide attempt or psychiatric hospitalization in the past 2 y. Face-to-face screening excluded patients with substance use problems or those who were enrolled in another research study.
Clinic patients were referred to the Hispanic Health Council to learn about the study, provide written informed consent, and participate in the intervention. The Hispanic Health Council is a community-based organization headquartered in a large Latino neighborhood in Hartford. A total of 121 Latinos with T2DM were recruited, consented, and completed face-to-face baseline interviews with trained bilingual or bicultural interviewers. Self-reported information was entered into remote electronic data capture databases (31).
Measures
Demographic and socioeconomic characteristics.
Demographic information included age, sex, marital status (partnered compared with not partnered), number of years living in the United States, language spoken (English only, Spanish only, or English and Spanish). Socioeconomic information included income (≤$1000/mo or ≥$1001/mo), education (high school graduate or General Educational Development diploma, or less than high school graduate or General Educational Development diploma), and participation in Supplemental Nutrition Assistance Program (SNAP) benefits (yes or no).
Food security status.
Food security status was assessed by using the 6-item US Household Food Security Survey short form (32, 33). Sample items are the following: “The food that (I/we) bought just didn’t last, and (I/we) didn’t have money to get more” and “Were you ever hungry but didn’t eat because there wasn’t enough money for food?” Items referenced the previous 12 mo. Response options were “yes,” “every month or almost every month,” “some months but not every month,” and “only one month.” The sum of affirmative responses produces a scale score (0–6). Higher scores indicate greater HFI. Recent evidence indicates that people in households with “marginal food security,” usually classified as food secure in the US government’s prevalence estimates, also may face an increased likelihood of impaired health and nutrition (34). For this reason, we defined scores = 0 as food secure and scores ≥1 as food insecure, including marginal, low, and very low food security levels. In our sample, Cronbach’s α = 0.89.
Depressive symptoms.
The validated Spanish version of the Personal Health Questionnaire Depression Scale (PHQ-8, i.e., the PHQ-9 without the suicidality item) (35, 36) measures depressive symptoms during the past 2 wk, with higher scores indicating more depressive symptoms. We omitted the suicidality item so that community health workers performing assessments in the field would not be placed in a position of responding to suicidality. In our sample Cronbach’s α = 0.79.
Anxiety symptoms.
The validated Spanish version of the Patient-Reported Outcomes Measurement Information System (PROMIS) emotional distress/anxiety scale (Short Form 8a) assesses anxiety symptoms during the past 7 d (37, 38). The 8-item scale contains response options from 1 = never to 5 = always, with higher scores indicating more anxiety symptoms (37); in our sample, Cronbach’s α = 0.91.
Diabetes distress.
The 5-item validated-US Spanish-language version of the Problem Areas in Diabetes Questionnaire (PAID-5) scale assesses current emotional distress from living with diabetes mellitus (39). Each item is scored 0 = not a problem to 4 = serious problem, with higher scores indicating more distress (39); in our sample, Cronbach’s α = 0.92.
Sleep outcome.
Sleep quality was measured with the 3-factor version of the Pittsburgh Sleep Quality Index (PSQI), which assesses sleep quality during a 1-mo period (40, 41). As validated by Tomfohr et al. (40), we used 6 of the 7 PSQI subscales (Subjective Sleep Quality, Sleep Duration, Sleep Disturbance, Sleep Efficiency, Daytime Dysfunction, and Sleep Latency). The 6-subscale version is a more reliable assessment of sleep quality among English- and Spanish-speaking Latinos than the 7-subscale version. The subscale Sleep Medication was omitted because of low confirmatory factor loading. In distinguishing good and poor sleepers, a global PSQI score >5 yields a sensitivity of 89.6% and a specificity of 86.5%. We used a score of >5 to indicate inadequate and poor sleep quality (24, 41). In our sample, Cronbach’s α = 0.82.
Statistical analyses
Statistical analyses were performed by using SPSS version 23.0 (IBM SPSS Statistics) and process (42), with P < 0.05 considered statistically significant. We used descriptive statistics to characterize the demographic factors of the full sample, followed by separate factors for participants who were food secure and those who were food insecure. ANOVAs were conducted to determine the differences between continuous sociodemographic characteristics and household food security status. Chi-square tests were conducted to determine the differences between categorical socioeconomic characteristics and household food security status. Fisher’s exact test and the Mann-Whitney U test were used to examine group differences (food secure compared with food insecure) on the variables listed in Table 1.
TABLE 1.
Sample characteristics by HFI status in Latinos with T2DM1
| Characteristics | Total (n = 121) | Food secure (n = 40) | Food insecure (n = 81) | P |
| Age,2 y | 61 ± 12 | 61 ± 12 | 60 ± 12 | 0.65 |
| Sex3 | 0.15 | |||
| Females | 90 (74.4) | 33 (36.7) | 57 (63.3) | |
| Males | 31 (25.6) | 7 (22.6) | 24 (77.4) | |
| Education3 | 0.57 | |||
| <High school | 93 (76.9) | 32 (34.4) | 61 (65.6) | |
| ≥High school | 28 (23.1) | 8 (28.6) | 20 (71.4) | |
| Employment status3 | 0.61 | |||
| Unemployed | 109 (90.1) | 36 (33.0) | 73 (67.0) | |
| Employed | 12 (9.9) | 4 (33.3) | 8 (66.7) | |
| Monthly income,3 US$ | 0.82 | |||
| 0–1000 | 80 (66.1) | 27 (33.8) | 53 (66.3) | |
| ≥1001 | 41 (33.9) | 13 (31.7) | 28 (68.3) | |
| Persons in household, including participant2 | 2.2 ± 1.4 | 2.2 ± 1.1 | 2.2 ± 1.5 | 0.99 |
| Marital status3 | 0.86 | |||
| Single | 83 (68.6) | 27 (32.5) | 56 (67.5) | |
| Partnered | 38 (31.4) | 13 (34.2) | 25 (65.8) | |
| Time living in the United States,2 y | 35 ± 14 | 35 ± 16.7 | 36 ± 13.2 | 0.77 |
| SNAP participation3 | 0.98 | |||
| No | 18 (14.9) | 6 (33.3) | 12 (66.7) | |
| Yes | 103 (85.1) | 34 (33.0) | 69 (67.0) | |
| Psychological distress2 | ||||
| Depressive symptoms | 6 ± 5.5 | 3 ± 3.8 | 8 ± 5.6 | <0.001 |
| Anxiety symptoms | 15 ± 7.6 | 12 ± 6.2 | 17 ± 7.7 | <0.001 |
| Diabetes distress | 8 ± 6.4 | 5 ± 8.5 | 9 ± 6.5 | 0.01 |
| Sleep quality2 | 6 ± 4.7 | 4 ± 4.3 | 7 ± 4.6 | <0.001 |
Values are means ± SDs or n (%). Percentages for Food secure and Food insecure columns are calculated horizontally within each row. HFI, household food insecurity; SNAP, Supplemental Nutrition Assistance Program; T2DM, type 2 diabetes mellitus.
ANOVAs were conducted to determine differences between continuous sociodemographic characteristics and household food security status. The Mann-Whitney U test was used to determine the differences between continuous variables and household food security status.
Chi-square tests were conducted to determine differences between categorical socioeconomic characteristics and household food security status. Fisher’s exact test was used for cell counts of <5.
The statistical significance of the indirect effect (IE) was tested through use of bootstrapping. Bootstrapping is used to generate an approximation of the sampling distribution to obtain a more accurate CI while making no assumptions about the shape of the sampling distribution (43). Bootstrapping is a preferred method because it is the only test that does not violate assumptions of normality (and it is recommended for small sample sizes), as compared with the Sobel test assumption of a normal sampling distribution. Preacher and Hayes’s (42) bootstrap PROCESS Macros method was used to assess the direct relation between HFI and sleep quality and the potential mediating effects of psychological distress on that relation. We used a series of IE tests (42) with bootstrapped CIs (10,000 samples) to test whether dichotomous food insecurity was associated with suboptimal sleep quality (continuous) via each measure of distress (e.g., depressive symptoms, anxiety symptoms, diabetes distress).
IE tests assess whether the ab path is significant according to the distribution of ab paths generated via bootstrapping Figure 1). For each mediator, we examined IEs with 2 models. The first model was unadjusted and the second model was adjusted for age, sex, education, employment status, income, and marital status.
Results
The respondents’ mean age was 61 y, 74% were women, 77% had a high school education or less, 90% were unemployed, 66% had a monthly income of ≤$1000, and 31% were married or had an intimate partner. The majority (86%) of the respondents identified themselves as Puerto Rican or Puerto Rican American, and 93% indicated their preferred language as Spanish. More than 85% participated in SNAP, and 67% were classified as HFI (Table 1).
There were no substantial differences between participants who were food secure and those who were food insecure regarding age, sex, education, income, number of people in the household, number of years living in the United States, preferred language, and marital status (Table 1). Participants who were food insecure had significantly more depressive symptoms, anxiety symptoms, and diabetes distress, and worse sleep quality than participants who were food secure (Table 1).
We tested the unadjusted IE of HFI on suboptimal sleep quality via each measure of distress (Figure 1) and then tested each of these IEs adjusted for age, sex, education, employment status, income, and marital status. As shown in Tables 2–4, across all models distress was associated with suboptimal sleep quality (b path), HFI was associated with suboptimal sleep quality (c path), and there was an IE of HFI on suboptimal sleep quality via each measure of distress. The adjusted standardized IE through depression was 0.06 (95% CI: 0.01, 0.13), through anxiety was 0.18 (95% CI: 0.09, 0.28), and through diabetes distress was 0.23 (95% CI: 0.14, 0.34).
TABLE 2.
Test of IE of food insecurity on suboptimal sleep quality via depressive symptoms in Latinos with T2DM1
| Model 12 | Model 23 | |
| Food insecurity to depressive symptoms (a path) | 4.53* | 4.71* |
| Depressive symptoms to suboptimal sleep quality (b path) | 0.51* | 0.47* |
| Total effect of food insecurity on suboptimal sleep quality (c path) | 2.97* | 3.23* |
| Direct effect of food insecurity on suboptimal sleep quality (c׳ path) | 0.68 | 1.01 |
| IE of food insecurity on suboptimal sleep quality via depressive symptoms (a and b paths) (95% bootstrapped CI) | 2.31 (1.36, 3.44) | 2.22 (1.27, 3.42) |
| Completely standardized IE (95% bootstrapped CI) | 0.07 (0.01, 0.14) | 0.06 (0.01, 0.13) |
| Adjusted R2 | 0.09 | 0.22 |
| F | 10.97* | 4.20* |
Bootstrapped 95% CIs on 10,000 sample. *P < 0.001. IE, indirect effect; T2DM, type 2 diabetes mellitus.
Model 1 was unadjusted.
Model 2 was adjusted for age, sex, education, employment status, income, and marital status.
TABLE 4.
Test of IE of food insecurity on suboptimal sleep quality via diabetes distress in Latinos with T2DM1
| Model 12 | Model 23 | |
| Food insecurity to diabetes distress (a path) | 2.94* | 2.93* |
| Diabetes distress to suboptimal sleep quality (b path) | 0.22*** | 0.21*** |
| Total effect of food insecurity on suboptimal sleep quality (c path) | 2.89*** | 3.16*** |
| Direct effect of food insecurity on suboptimal sleep quality (c׳ path) | 2.23** | 2.56** |
| Indirect effect of food insecurity on suboptimal sleep quality via diabetes distress (a and b paths) (95% bootstrapped CI) | 0.66 (0.15, 1.42) | 0.60 (0.11, 1.32) |
| Completely standardized IE (95% bootstrapped CI) | 0.23 (0.14, 0.33) | 0.23 (0.14, 0.34) |
| Adjusted R2 | 0.04 | 0.08 |
| F | 5.37* | 1.38 |
Bootstrapped 95% CIs on 10,000 sample. *P < 0.05, **P < 0.01, ***P < 0.001. IE, indirect effect; T2DM, type 2 diabetes mellitus.
Model 1 was unadjusted.
Model 2 was adjusted for age, sex, education, employment status, income, and marital status.
TABLE 3.
Test of IE of food insecurity on suboptimal sleep quality via anxiety symptoms in Latinos with T2DM1
| Model 12 | Model 23 | |
| Food insecurity to anxiety symptoms (a path) | 4.99*** | 5.40** |
| Anxiety symptoms to suboptimal sleep quality (b path) | 0.34*** | 0.31*** |
| Total effect of food insecurity on suboptimal sleep quality (c path) | 3.02*** | 3.27*** |
| Direct effect of food insecurity on suboptimal sleep quality (c׳ path) | 1.31§ | 1.57* |
| Indirect effect of food insecurity on suboptimal sleep quality via anxiety symptoms (a and b paths) (95% bootstrapped CI) | 1.72 (0.79, 2.79) | 1.70 (0.87, 2.85) |
| Completely standardized IE (95% bootstrapped CI) | 0.17 (0.08, 0.27) | 0.18 (0.09, 0.28) |
| Adjusted R2 | 0.09 | 0.19 |
| F | 11.77*** | 3.52** |
Bootstrapped 95% CIs on 10,000 sample. §P < 0.10, *P < 0.05, **P < 0.01, ***P < 0.001. IE, indirect effect; T2DM, type 2 diabetes mellitus.
Model 1 was unadjusted.
Model 2 was adjusted for age, sex, education, employment status, income, and marital status.
Discussion
We found that HFI is associated with suboptimal sleep quality and that psychological distress mediates the relation between HFI and suboptimal sleep quality. In this sample of low-income Latinos with T2DM, we found HFI to be significantly associated with each measure of psychological distress (i.e., depressive symptoms, anxiety symptoms, and diabetes distress) and with suboptimal sleep quality.
In mediation models, HFI was associated with suboptimal sleep quality through these 3 indicators of psychological distress. These mediational relations remained after we controlled for a range of clinical and demographic characteristics, including income. Overall, income levels in this sample were low. Our results suggest that HFI may predict distress and sleep uniquely, independent of more traditional socioeconomic indicators, including income. Worry over providing food, feeding children, and experiencing hunger may be uniquely distressing, contributing to why HFI is associated consistently with maternal depression, children’s psychoemotional development, and adults’ mental health (44–46). To our knowledge, no previous study has examined the associations between household food insecurity, psychological distress and sleep quality in Latinos with T2DM.
Our results are consistent with previous studies indicating that HFI is associated with suboptimal sleep outcomes (e.g., short sleep duration, poor sleep quality) (14, 47). Ding et al. (47) found a link between HFI and habitual short sleep duration, long sleep latency, and frequent sleep complaints. They hypothesized that mental health may be a mechanism underlying the relation between HFI and sleep; however, their study did not explicitly test this hypothesis (47). Our results support mental health as a mechanism linking HFI to sleep in Latinos with T2DM.
Studies also have documented the association between psychological distress and suboptimal sleep (48–50). To our knowledge, few studies, however, have used mediation models to explore direct and indirect associations between HFI, psychological distress, and sleep quality (51). Liu et al. (48) examined the associations between housing and food insecurity with insufficient sleep in adults in 12 US states and found the prevalence of insufficient sleep and mental distress to be substantially greater in those who reported HFI than in those who did not. Further adjustment for respondents’ mental distress reduced the magnitude of the relation, and HFI remained highly associated with frequently experiencing insufficient sleep (PR = 1.54; 95% CI: 1.42, 1.67) (48). That study used only a single item to assess sleep and 1 item to assess distress. Our study extends the findings of Liu et al. by using a more sophisticated self-reported assessment of sleep and distress and by using PROCESS, the current state-of-the-art analysis, for testing mediation (42).
Among low-income families in the United States, HFI is associated with a diagnosis of diabetes mellitus (52). Once a person is diagnosed with diabetes, his or her level of HFI is associated with being depressed and having greater emotional distress and suboptimal glycemic control (18, 53–55). Our findings suggest that the relation between HFI and sleep quality is complex and seems to be mediated by psychological distress. Participants who experienced HFI reported more symptoms of depression, anxiety, and higher diabetes distress, and they were more likely to have suboptimal sleep quality.
Our study has several important limitations. First, we used cross-sectional data and thus cannot establish temporal precedence or causality. Prospective studies would further this line of research in 2 important ways: 1) they would better describe the sequencing of HFI, psychological distress, and sleep (ideally, microlongitudinal designs would be used that would track the temporal unfolding of food abundance and scarcity, psychological symptoms, and sleep), and 2) they would allow for testing causal mechanisms underlying relations between HFI (and the extent to which respondents experienced hunger) on psychological distress and sleep quality.
Second, our analyses of sleep quality relied on self-report data that are potentially subject to several sources of bias. Participants may not correctly recall their sleep patterns, and it is possible that participants with psychological distress have a negative reporting bias, thus underreporting sleep quality. Objective measures of sleep such as actigraphy (56) would provide more reliable indexes of sleep.
Third, other mechanisms linking HFI and sleep, such as nutritional intake, were not assessed. Future studies should examine multiple classes of putative mediators.
In general, the aforementioned limitations are outweighed by the study’s strengths, which include a vulnerable and hard-to-reach clinical sample, measurement of multiple domains of psychological distress, use of a validated and widely used measure of HFI, and state-of-the-art mediation modeling.
Social determinants of health (e.g., food security, financial stability), mental health, diabetes mellitus, and sleep health are among the 42 public health areas of concern outlined in Healthy People 2020 (56). In our previous work, HFI was a powerful mental stressor and was a social determinant of health (57, 58). These findings also have clinical implications for patients with T2DM. Sleep is a basic human need that is important for good health (1, 59). Suboptimal sleep is prevalent in patients with T2DM (60). Because poor sleep quality may have a negative effect on glucose regulation, it is important for health care providers to promote better sleep quality in patients with T2DM.
According to Healthy People 2020, “Mental health is a state of successful performance of mental function, resulting in productive activities, fulfilling relationships with other people, and the ability to adapt to change and to cope with challenges” (56). In our sample, participants who experienced HFI reported more symptoms of psychological distress. These results may point to important intervention opportunities for improving sleep quality in individuals with T2DM, specifically, facilitating access to healthful diets and providing affected individuals with the skills to better cope with mental distress associated with poverty-related stressors, including HFI.
Community health workers meet important needs of individuals with T2DM that are not addressed by private or public health care and social assistance systems (61). The Patient Protection and Affordable Care Act (Public Law 111-148) may represent an opportunity to formalize the role of community health workers as members of a multidisciplinary T2DM health care team. As such, further prospective cohort studies are needed to help delineate the impact of such food assistance programs as SNAP, and the role of community health workers in helping affected individuals better cope with poverty- and disease-related stressors should be prioritized.
“Low-cost” psychological interventions for Latinos with T2DM have been reported, including the CALMS-D randomized controlled trial. Evidence from the CALMS-D trial demonstrated that stress management delivered by a community health worker can decrease the symptoms of depression and anxiety in the Latinos with T2DM population (29). Until public policy can redirect resources toward ending HFI, efforts must be made to mitigate the deleterious effects of HFI on health outcomes. Future studies that compare the cost-effectiveness of community health worker–led interventions to typical care in SNAP recipients with T2DM on household food security, sleep quality, and other diabetes-related outcomes should be prioritized.
Acknowledgments
RP-E and JW designed the research; JC coordinated the recruitment; SS-P and GD conducted the research; AB-M, CYO, and JW analyzed the data; AB-M drafted the manuscript; AB-M, RP-E, CYO, and JW critically revised the manuscript; and AB-M had primary responsibility for the final content. All of the authors read and approved the final manuscript.
Footnotes
Abbreviations used: CALMS-D, Community Health Workers Assisting Latinos Manage Stress and Diabetes; HFI, household food insecurity; IE, indirect effect; PAID-5, Problem Areas in Diabetes; PHQ-8, Personal Health Questionnaire; PROMIS, Patient Reported Outcomes Measurement Information System; PSQI, Pittsburgh Sleep Quality Index; SNAP, Supplemental Nutrition Assistance Program; T2DM, type 2 diabetes mellitus.
References
- 1.Knutson KL. Sociodemographic and cultural determinants of sleep deficiency: implications for cardiometabolic disease risk. Soc Sci Med 2013;79:7–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Knutson KL, Van Cauter E. Associations between sleep loss and increased risk of obesity and diabetes. Ann N Y Acad Sci 2008;1129:287–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med 2010;71:1027–36. [DOI] [PubMed] [Google Scholar]
- 4.Grandner MA, Perlis ML. Short sleep duration and insomnia associated with hypertension incidence. Hypertens Res 2013;36:932–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grandner MA, Buxton OM, Jackson N, Sands-Lincoln M, Pandey A, Jean-Louis G. Extreme sleep durations and increased C-reactive protein: effects of sex and ethnoracial group. Sleep 2013;36:769–779E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grandner MA, Chakravorty S, Perlis ML, Oliver L, Gurubhagavatula I. Habitual sleep duration associated with self-reported and objectively determined cardiometabolic risk factors. Sleep Med 2014;15:42–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ferrie JE, Kivimaki M, Akbaraly TN, Tabak A, Abell J, Davey Smith G, Virtanen M, Kumari M, Shipley MJ. Change in sleep duration and type 2 diabetes: the Whitehall II Study. Diabetes Care 2015;38:1467–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lou P, Zhang P, Zhang L, Chen P, Chang G, Zhang N, Li T, Qiao C. Effects of sleep duration and sleep quality on prevalence of type 2 diabetes mellitus: a 5-year follow-up study in China. Diabetes Res Clin Pract 2015;109:178–84. [DOI] [PubMed] [Google Scholar]
- 9.National Institutes of Health, National Heart, Lung and Blood Institute, US Department of Health and Human Services. Your guide to healthy sleep.. Publication no. 11–5271; 2011.
- 10.Centers for Disease Control and Prevention. Unhealthy sleep-related behaviors—12 states, 2009. MMWR Morb Mortal Wkly Rep 2011;60:233–8. [PubMed] [Google Scholar]
- 11.National Sleep Foundation. 2010 Sleep in America poll. Washington (DC): National Sleep Foundation; 2010. [Google Scholar]
- 12.Laraia BA. Food insecurity and chronic disease. Adv Nutr 2013;4:203–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Perez-Escamilla R, Ferris AM, Drake L, Haldeman L, Peranick J, Campbell M, Peng YK, Burke G, Bernstein B. Food stamps are associated with food security and dietary intake of inner-city preschoolers from Hartford, Connecticut. J Nutr 2000;130:2711–7. [DOI] [PubMed] [Google Scholar]
- 14.Jordan ML, Perez-Escamilla R, Desai MM, Shamah-Levy T. Household food insecurity and sleep patterns among Mexican adults: results from ENSANUT-2012. J Immigr Minor Health 2015 Jul 11 (Epub ahead of print; DOI: 10.1007/s10903-015-0246-5). [DOI] [PubMed] [Google Scholar]
- 15.Anderson SE. Core indicators of nutritional state for difficult-to-sample populations. J Nutr 1990;120:1559–660. [DOI] [PubMed] [Google Scholar]
- 16.Coleman-Jensen A, Gregory C, Singh A. Household food security in the United States in 2013. Report No.: ERR-173. Washington (DC): US Department of Agriculture, Economic Research Service; 2014.
- 17.Heerman WJ, Wallston KA, Osborn CY, Bian A, Schlundt DG, Barto SD, Rothman RL. Food insecurity is associated with diabetes self-care behaviours and glycaemic control. Diabet Med 2016;33:844–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Seligman HK, Jacobs EA, Lopez A, Tschann J, Fernandez A. Food insecurity and glycemic control among low-income patients with type 2 diabetes. Diabetes Care 2012;35:233–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Silverman J, Krieger J, Kiefer M, Hebert P, Robinson J, Nelson K. The relationship between food insecurity and depression, diabetes distress and medication adherence among low-income patients with poorly-controlled diabetes. J Gen Intern Med 2015;30:1476–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Perez-Escamilla R, Bermudez-Millan A, Segura-Perez S, Damio GCJ, Wagner J. Household food insecurity and higher blood glucose concentrations among Latinos with type 2 diabetes. 142nd APHA Annual Meeting and Exposition; 2014 Nov 18; New Orleans, LA; 2014. [Google Scholar]
- 21.Kollannoor-Samuel G, Wagner J, Damio G, Segura-Perez S, Chhabra J, Vega-Lopez S, Perez-Escamilla R. Social support modifies the association between household food insecurity and depression among Latinos with uncontrolled type 2 diabetes. J Immigr Minor Health 2011;13:982–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chilton M, Booth S. Hunger of the body and hunger of the mind: African American women's perceptions of food insecurity, health and violence. J Nutr Educ Behav 2007;39:116–25. [DOI] [PubMed] [Google Scholar]
- 23.Hadley C, Patil CL. Seasonal changes in household food insecurity and symptoms of anxiety and depression. Am J Phys Anthropol 2008;135:225–32. [DOI] [PubMed] [Google Scholar]
- 24.Buysse DJ, Yu L, Moul DE, Germain A, Stover A, Dodds NE, Johnston KL, Shablesky-Cade MA, Pilkonis PA. Development and validation of patient-reported outcome measures for sleep disturbance and sleep-related impairments. Sleep 2010;33:781–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gregory AM, Buysse DJ, Willis TA, Rijsdijk FV, Maughan B, Rowe R, Cartwright S, Barclay NL, Eley TC. Associations between sleep quality and anxiety and depression symptoms in a sample of young adult twins and siblings. J Psychosom Res 2011;71:250–5. [DOI] [PubMed] [Google Scholar]
- 26.Franzen PL, Buysse DJ. Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications. Dialogues Clin Neurosci 2008;10:473–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van Mill JG, Hoogendijk WJ, Vogelzangs N, van Dyck R, Penninx BW. Insomnia and sleep duration in a large cohort of patients with major depressive disorder and anxiety disorders. J Clin Psychiatry 2010;71:239–46. [DOI] [PubMed] [Google Scholar]
- 28.Seixas AA, Nunes JV, Airhihenbuwa CO, Williams NJ, Pandi-Perumal SR, James CC, Jean-Louis G. Linking emotional distress to unhealthy sleep duration: analysis of the 2009 National Health Interview Survey. Neuropsychiatr Dis Treat 2015;11:2425–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wagner J, Bermudez-Millan A, Segura-Perez S, Damio G, Chhabra J, Perez-Escamilla R. Group stress management delivered by community health workers: effects on emotional functioning among Latinos with type 2 diabetes. 142nd APHA Annual Meeting and Exposition; 2014 Nov 18; New Orleans, LA; 2014. [Google Scholar]
- 30.National Institute of Diabetes and Digestive and Kidney Diseases. The A1C test and diabetes [Internet]. c2014 [cited 2016 May 1]. Available from: https://www.niddk.nih.gov/health-information/health-topics/diagnostic-tests/a1c-test-diabetes/Documents/A1C_Test_DM_508.pdf.
- 31.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to measuring household food security, revised 2000. Alexandria (VA): US Department of Agriculture, Food and Nutrition Service; 2000.
- 33.Blumberg SJ, Bialostosky K, Hamilton WL, Briefel RR. The effectiveness of a short form of the Household Food Security Scale. Am J Public Health 1999;89:1231–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cook JT, Black M, Chilton M, Cutts D, Ettinger de Cuba S, Heeren TC, Rose-Jacobs R, Sandel M, Casey PH, Coleman S, et al. Are food insecurity’s health impacts underestimated in the U.S. population? Marginal food security also predicts adverse health outcomes in young U.S. children and mothers. Adv Nutr 2013;4:51–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gilmer TP, Walker C, Johnson ED, Philis-Tsimikas A, Unutzer J. Improving treatment of depression among Latinos with diabetes using project Dulce and IMPACT. Diabetes Care 2008;31:1324–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Merz EL, Malcarne VL, Roesch SC, Riley N, Sadler GR. A multigroup confirmatory factor analysis of the Patient Health Questionnaire-9 among English- and Spanish-speaking Latinas. Cultur Divers Ethnic Minor Psychol 2011;17:309–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Irwin DE, Stucky B, Langer MM, Thissen D, Dewitt EM, Lai JS, Varni JW, Yeatts K, DeWalt DA. An item response analysis of the pediatric PROMIS anxiety and depressive symptoms scales. Qual Life Res 2010;19:595–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Craig BM, Reeve BB, Cella D, Hays RD, Pickard AS, Revicki DA. Demographic differences in health preferences in the United States. Med Care 2014;52:307–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Welch G, Schwartz CE, Santiago-Kelly P, Garb J, Shayne R, Bode R. Disease-related emotional distress of Hispanic and non-Hispanic type 2 diabetes patients. Ethn Dis 2007;17:541–7. [PubMed] [Google Scholar]
- 40.Tomfohr LM, Schweizer CA, Dimsdale JE, Loredo JS. Psychometric characteristics of the Pittsburgh Sleep Quality Index in English speaking non-Hispanic whites and English and Spanish speaking Hispanics of Mexican descent. J Clin Sleep Med 2013;9:61–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989; 28:193–213. [DOI] [PubMed] [Google Scholar]
- 42.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput 2004;36:717–31. [DOI] [PubMed] [Google Scholar]
- 43.Hayes A, Preacher K. Quantifying and testing indirect effects in simple mediation models when the constituent paths are nonlinear. Multivariate Behav Res 2010;45:627–60. [DOI] [PubMed] [Google Scholar]
- 44.Leung CW, Epel ES, Willett WC, Rimm EB, Laraia BA. Household food insecurity is positively associated with depression among low-income supplemental nutrition assistance program participants and income-eligible nonparticipants. J Nutr 2015;145:622–7. [DOI] [PubMed] [Google Scholar]
- 45.Corman H, Curtis MA, Noonan K, Reichman NE. Maternal depression as a risk factor for children’s inadequate housing conditions. Soc Sci Med 2016;149:76–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Perez-Escamilla R, Pinheiro de Toledo Vianna R. Food insecurity and the behavioral and intellectual development of children: a review of the evidence; 2012 [Internet]. [cited 2016 Feb 9]. Available from: http://digitalcommons.library.tmc.edu/childrenatrisk/vol3/iss1/9.
- 47.Ding M, Keiley MK, Garza KB, Duffy PA, Zizza CA. Food insecurity is associated with poor sleep outcomes among US adults. J Nutr 2015;145:615–21. [DOI] [PubMed] [Google Scholar]
- 48.Liu Y, Croft JB, Wheaton AG, Perry GS, Chapman DP, Strine TW, McKnight-Eily LR, Presley-Cantrell L. Association between perceived insufficient sleep, frequent mental distress, obesity and chronic diseases among US adults, 2009 behavioral risk factor surveillance system. BMC Public Health 2013;13:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sariarslan HA, Gulhan YB, Unalan D, Basturk M, Delibas S. The relationship of sleep problems to life quality and depression. Neurosciences (Riyadh) 2015;20:236–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Grandner MA, Petrov ME, Rattanaumpawan P, Jackson N, Platt A, Patel NP. Sleep symptoms, race/ethnicity, and socioeconomic position. J Clin Sleep Med 2013;9:897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Liu Y, Njai RS, Greenlund KJ, Chapman DP, Croft JB. Relationships between housing and food insecurity, frequent mental distress, and insufficient sleep among adults in 12 US states, 2009. Prev Chronic Dis 2014;11:E37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fitzgerald N, Hromi-Fiedler A, Segura-Perez S, Perez-Escamilla R. Food insecurity is related to increased risk of type 2 diabetes among Latinas. Ethn Dis 2011;21:328–34. [PMC free article] [PubMed] [Google Scholar]
- 53.Bawadi HA, Ammari F, Abu-Jamous D, Khader YS, Bataineh S, Tayyem RF. Food insecurity is related to glycemic control deterioration in patients with type 2 diabetes. Clin Nutr 2012;31:250–4. [DOI] [PubMed] [Google Scholar]
- 54.Berkowitz SA, Baggett TP, Wexler DJ, Huskey KW, Wee CC. Food insecurity and metabolic control among U.S. adults with diabetes. Diabetes Care 2013;36:3093–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Marino M, Li Y, Rueschman MN, Winkelman JW, Ellenbogen JM, Solet JM, Dulin H, Berkman LF, Buxton OM. Measuring sleep: accuracy, sensitivity, and specificity of wrist actigraphy compared to polysomnography. Sleep 2013;36:1747–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.US Department of Health and Human Services. Healthy people 2020 [Internet]. [cited 2016 Feb 9]. Available from: https://www.healthypeople.gov; 2011.
- 57.Bermudez-Millan A, Damio G, D'Angelo K, Segura-Perez S, Perez-Escamilla R. Social Determinants of Stress and its Effects on Maternal and Child Health. 137th American Public Health Association; 2009 Nov 10.
- 58.Bermudez-Millan A, Damio G, Cruz J, D'Angelo K, Segura-Perez S, Perez-Rivera K, Stratton A, Perez-Escamilla R. Power of community dialogue as a community-based participatory research strategy and approach to make systemic changes. 138th American Public Health Association; 2010 Nov 9. [Google Scholar]
- 59.Buxton OM, Broussard JL, Zahl AK, Hall M. Effects of sleep deficiency on hormones, cytokines, and metabolism. In: Redline S, editor. Impact of sleep and sleep disturbances on obesity and cancer. New York: Springer; 2014. [Google Scholar]
- 60.Lou P, Qin Y, Zhang P, Chen P, Zhang L, Chang G, Li T, Qiao C, Zhang N. Association of sleep quality and quality of life in type 2 diabetes mellitus: a cross-sectional study in China. Diabetes Res Clin Pract 2015;107:69–76. [DOI] [PubMed] [Google Scholar]
- 61.Perez-Escamilla R, Damio G, Chhabra J, Fernandez ML, Segura-Perez S, Vega-Lopez S, Kollannor-Samuel G, Calle M, Shebl FM, D’Agostino D. Impact of a community health workers-led structured program on blood glucose control among Latinos with type 2 diabetes: the DIALBEST trial. Diabetes Care 2015;38:197–205. [DOI] [PMC free article] [PubMed] [Google Scholar]