Abstract
Legal and ethical issues form an important component of modern research, related to the subject and researcher. This article seeks to briefly review the various international guidelines and regulations that exist on issues related to informed consent, confidentiality, providing incentives and various forms of research misconduct. Relevant original publications (The Declaration of Helsinki, Belmont Report, Council for International Organisations of Medical Sciences/World Health Organisation International Guidelines for Biomedical Research Involving Human Subjects, World Association of Medical Editors Recommendations on Publication Ethics Policies, International Committee of Medical Journal Editors, CoSE White Paper, International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use-Good Clinical Practice) form the literature that are relevant to the ethical and legal aspects of conducting research that researchers should abide by when conducting translational and clinical research. Researchers should note the major international guidelines and regional differences in legislation. Hence, specific ethical advice should be sought at local Ethics Review Committees.
Key words: Confidentiality, ethics, informed consent, legal issues, plagiarism, professional misconduct
INTRODUCTION
The ethical and legal issues relating to the conduct of clinical research involving human participants had raised the concerns of policy makers, lawyers, scientists and clinicians for many years. The Declaration of Helsinki established ethical principles applied to clinical research involving human participants. The purpose of a clinical research is to systematically collect and analyse data from which conclusions are drawn, that may be generalisable, so as to improve the clinical practice and benefit patients in future. Therefore, it is important to be familiar with Good Clinical Practice (GCP), an international quality standard that is provided by the International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH),[1] or the local version, GCP of the Central Drugs Standard Control Organization (India's equivalent of US Food and Drug Administration)[2] and local regulatory policy to ensure that the research is conducted both ethically and legally. In this article, we will briefly review the legal and ethical issues pertaining to recruitment of human subjects, basic principles of informed consent and precautions to be taken during data and clinical research publications. Some of the core principles of GCP in research include defining responsibilities of sponsors, investigators, consent process monitoring and auditing procedures and protection of human subjects.[3]
ISSUES RELATED TO THE RESEARCH PARTICIPANTS
The main role of human participants in research is to serve as sources of data. Researchers have a duty to ‘protect the life, health, dignity, integrity, right to self-determination, privacy and confidentiality of personal information of research subjects’.[4] The Belmont Report also provides an analytical framework for evaluating research using three ethical principles:[5]
Respect for persons – the requirement to acknowledge autonomy and protect those with diminished autonomy
Beneficence – first do no harm, maximise possible benefits and minimise possible harms
Justice – on individual and societal level.
Mistreatment of research subjects is considered research misconduct (no ethical review approval, failure to follow approved protocol, absent or inadequate informed consent, exposure of subjects to physical or psychological harm, exposure of subjects to harm due to unacceptable research practices or failure to maintain confidentiality).[6] There is also scientific misconduct involving fraud and deception.
Consent, possibility of causing harm
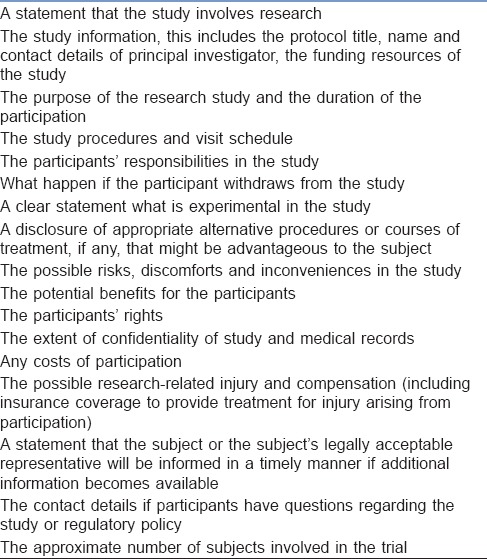
Based on ICH definition, ‘informed consent is a process by which a subject voluntarily confirms his or her willingness to participate in a particular trial, after having been informed of all aspects of the trial that are relevant to the subject's decision to participate’. As for a standard (therapeutic) intervention that carries certain risks, informed consent – that is voluntary, given freely and adequately informed – must be sought from participants. However, due to the research-centred, rather than patient-centred primary purpose, additional relevant information must be provided in clinical trials or research studies in informed consent form. The essential components of informed consent are listed in Table 1 [Adapted from ICH Harmonised Tripartite Guideline, Guideline for Good Clinical Practice E6(R1)].[1] This information should be delivered in the language and method that individual potential subjects can understand,[4] commonly in the form of a printed Participant Information Sheet. Informed consent is documented by means of written, signed and dated informed consent form.[1] The potential subjects must be informed of the right to refuse to participate or withdraw consent to participate at any time without reprisal and without affecting the patient–physician relationship. There are also general principles regarding risk assessment, scientific requirements, research protocols and registration, function of ethics committees, use of placebo, post-trial provisions and research publication.[4]
Table 1.
Essential components of an informed consent
Special populations
Informed consent may be sought from a legally authorised representative if a potential research subject is incapable of giving informed consent[4] (children, intellectual impairment). The involvement of such populations must fulfil the requirement that they stand to benefit from the research outcome.[4] The ‘legally authorised representative’ may be a spouse, close relative, parent, power of attorney or legally appointed guardian. The hierarchy of priority of the representative may be different between different countries and different regions within the same country; hence, local guidelines should be consulted.
Special case: Emergency research
Emergency research studies occur where potential subjects are incapacitated and unable to give informed consent (acute head trauma, cardiac arrest). The Council for International Organisations of Medical Sciences/World Health Organisation guidelines and Declaration of Helsinki make exceptions to the requirement for informed consent in these situations.[4,7] There are minor variations in laws governing the extent to which the exceptions apply.[8]
Reasonable efforts should have been made to find a legal authority to consent. If there is not enough time, an ‘exception to informed consent’ may allow the subject to be enrolled with prior approval of an ethical committee.[7] Researchers must obtain deferred informed consent as soon as possible from the subject (when regains capacity), or their legally authorised representative, for continued participation.[4,7]
Collecting patient information and sensitive personal information, confidentiality maintenance
The Health Insurance Portability and Accountability Act has requirements for informed consent disclosure and standards for electronic exchange, privacy and information security. In the UK, generic legislation is found in the Data Protection Act.[9]
The International Committee of Medical Journal Editors (ICMJE) recommendations suggest that authors must ensure that non-essential identifying information (names, initials, hospital record numbers) are omitted during data collection and storage wherever possible. Where identifying information is essential for scientific purposes (clinical photographs), written informed consent must be obtained and the patient must be shown the manuscript before publication. Subjects should also be informed if any potential identifiable material might be available through media access.
Providing incentives
Cash or other benefits ‘in-kind’ (financial, medical, educational, community benefits) should be made known to subjects when obtaining informed consent without emphasising too much on it.[7] Benefits may serve as appreciation or compensation for time and effort but should not result in the inducement to participation.[10] The amount and nature of remuneration should be compared to norms, cultural traditions and are subjected to the Ethical Committee Review.[7]
ISSUES RELATED TO THE RESEARCHER
Legal issues pertaining to regulatory bodies
Various regulatory bodies have been constituted to uphold the safety of subjects involved in research. It is imperative to obtain approval from the appropriate regulatory authorities before proceeding to any research. The constitution and the types of these bodies vary nation-wise. The researchers are expected to be aware of these authorities and the list of various bodies pertinent to India are listed in the article “Research methodology II” of this issue.
Avoiding bias, inappropriate research methodology, incorrect reporting and inappropriate use of information
Good, well-designed studies advance medical science development. Poorly conducted studies violate the principle of justice, as there are time and resources wastage for research sponsors, researchers and subjects, and undermine the societal trust on scientific enquiry.[11] The Guidelines for GCP is an international ethical and scientific quality standard for designing, conducting, recording and reporting trials.[1]
Fraud in research and publication
De novo data invention (fabrication) and manipulation of data (falsification)[6] constitute serious scientific misconduct. The true prevalence of scientific fraud is difficult to measure (2%–14%).[12]
Plagiarism and its checking
Plagiarism is the use of others' published and unpublished ideas or intellectual property without attribution or permission and presenting them as new and original rather than derived from an existing source.[13] Tools such as similarity check[14] are available to aid researchers detect similarities between manuscripts, and such checks should be done before submission.[15]
Overlapping publications
Duplicate publications violate international copyright laws and waste valuable resources.[16,17] Such publications can distort evidence-based medicine by double-counting of data when inadvertently included in meta-analyses.[16] This practice could artificially enlarge one's scientific work, distorting apparent productivity and may give an undue advantage when competing for research funding or career advancement.[17] Examples of these practices include:
Duplicate publication, redundant publication
Publication of a paper that overlaps substantially with one already published, without reference to the previous publication.[11]
Salami publication
Slicing of data from a single research process into different pieces creating individual manuscripts from each piece to artificially increase the publication volume.[16]
Such misconduct may lead to retraction of articles. Transparent disclosure is important when submitting papers to journals to declare if the manuscript or related material has been published or submitted elsewhere, so that the editor can decide how to handle the submission or to seek further clarification. Further information on acceptable secondary publication can be found in the ICMJE ‘Recommendations for the Conduct, Reporting, Editing, and Publishing of Scholarly Work in Medical Journals’.
Copyright
Usually, sponsors and authors are required to sign over certain publication rights to the journal through copyright transfer or a licensing agreement; thereafter, authors should obtain written permission from the journal/publisher if they wish to reuse the published material elsewhere.[6]
Authorship and its various associations
The ICMJE recommendation lists four criteria of authorship:
Substantial contributions to the conception of design of the work, or the acquisition, analysis or interpretation of data for the work
Drafting the work or revising it critically for important intellectual content
Final approval of the version to be published
Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Authors and researchers have an ethical obligation to ensure the accuracy, publication and dissemination of the result of research,[4] as well as disclosing to publishers relevant corrections, retractions and errata, to protect scientific integrity of published evidence. Every research study involving human subjects must be registered in a publicly accessible database (e.g., ANZCTR [Australia and NZ], ClinicalTrials.gov [US and non-US], CTRI [India]) and the results made publicly available.[4] Sponsors of clinical trials must allow all study investigators and manuscript authors access to the full study data set and the right to use all study data for publication.[5] Source documents (containing trial data) and clinical study report (results and interpretation of trial) form part of the essential documentation that must be retained for a length of time prescribed by the applicable local legislation.[1] The ICMJE is currently proposing a requirement of authors to share with others de-identified individual patient data underlying the results presented in articles published in member journals.[18]
Those who have contributed to the work but do not meet all four criteria should be acknowledged; some of these activities include provision of administrative support, writing assistance and proofreading. They should have their written permission sought for their names to be published and disclose any potential conflicts of interest.[6] The Council of Scientific Editors has identified several inappropriate types of authorship, such as guest authorship, honorary or gift authorship and ghost authorship.[6] Various interventions should be put in place to prevent such fraudulent practices in research.[19] The list of essential documents for the conduct of a clinical trial is included in other articles of the same issue.
SUMMARY
The recent increase in research activities has led to concerns regarding ethical and legal issues. Various guidelines have been formulated by organisations and authorities, which serve as a guide to promote integrity, compliance and ethical standards in the conduct of research. Fraud in research undermines the quality of establishing evidence-based medicine, and interventions should be put in place to prevent such practices. A general overview of ethical and legal principles will enable research to be conducted in accordance with the best practices.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use. [monograph on the Internet] Geneva: 1996. [Last updated on 1996 Jun 10; Last cited on 2016 May 25]. ICH Harmonised Tripartite Guideline, Guideline for Good Clinical Practice E6(R1), Current Step 4 Version. Available from: http://www.ich.org/products/guidelines/efficacy/efficacy-single/article/goodclinical-practice.html . [Google Scholar]
- 2.Cdsco.nic.in [homepage in the Internet]. India 2014. Ministry of Health and Family Welfare, Government of India online resources. Central Drugs Standard Control Organization. [Last cited on 2016 Aug 11]. Available from: http://www.cdsco.nic.in/html/GCP1.html ; http://www.cdsco.nic.in/forms/list.aspx?lid=1843&Id=31 .
- 3.Devine S, Dagher RN, Weiss KD, Santana VM. Good clinical practice and the conduct of clinical studies in pediatric oncology. Pediatr Clin N Am. 2008;55:187–209. doi: 10.1016/j.pcl.2007.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–4. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 5.hhs.gov [homepage on the Internet] Rockville: U.S. Department of Health & Human Services Online Resource; [updated on 1979 Apr 18; cited on 2016 Aug 10]. Available from: http://www.hhs.gov/ohrp/regulations-and-policy/belmont-report/index.html . [Google Scholar]
- 6.Scott-Lichter D. CSE's White Paper on Promoting Integrity in Scientific Journal Publications, 2012 Update. 3rd Revised Edition. Wheat Ridge, CO; 2012. [Last accessed on 2016 Aug 08]. the Editorial Policy Committee, Council of Science Editors. Available from: http://www.councilscienceeditors.org/wp.content/uploads/entire_whitepaper.pdf . [Google Scholar]
- 7.International Ethical Guidelines for Biomedical Research Involving Human Subjects. [monograph on the Internet] Geneva: 2002. [cited on 2016 Aug 10]. Council for International Organizations of Medical Sciences (CIOMS) in Collaboration with the World Health Organization (WHO) Available from: http://www.cioms.ch/publications/layout_guide2002.pdf . [Google Scholar]
- 8.van Belle G, Mentzelopoulos SD, Aufderheide T, May S, Nichol G. International variation in policies and practices related to informed consent in acute cardiovascular research: Results from a 44 country survey. Resuscitation. 2015;91:76–83. doi: 10.1016/j.resuscitation.2014.11.029. [DOI] [PubMed] [Google Scholar]
- 9.Data Protection Act United Kingdom [monograph on the Internet] Norwich, UK: 1998. [updated on 1998 Jul 16; cited on 2016 Aug 14]. Her Majesty's Stationery Office and Queen's Printer of Acts of Parliament. Available from: http://www.legislation.gov.uk/ukpga/1998/29/introduction . [Google Scholar]
- 10.Njue M, Molyneux S, Kombe F, Mwalukore S, Kamuya D, Marsh V. Benefits in cash or in kind? A community consultation on types of benefits in health research on the Kenyan Coast. PLoS One. 2015;10:e0127842. doi: 10.1371/journal.pone.0127842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mutch WA. Academic fraud: Perspectives from a lifelong anesthesia researcher. Can J Anaesth. 2011;58:782. doi: 10.1007/s12630-011-9523-5. [DOI] [PubMed] [Google Scholar]
- 12.George SL. Research misconduct and data fraud in clinical trials: Prevalence and causal factors. Int J Clin Oncol. 2016;21:15–21. doi: 10.1007/s10147-015-0887-3. [DOI] [PubMed] [Google Scholar]
- 13.Recommendations on Publication Ethics Policies for Medical Journals: World Association of Medical Editors. [monograph on the Internet] Winnetka, IL, USA: 2016. [Last cited on 2016 May 17]. WAME Publication Ethics Committee. Available from: http://www.wame.org/about/recommendations-on-publication-ethicspolicie#Plagiarism . [Google Scholar]
- 14.Crossref.org [homepage on Internet] Oxford Centre for Innovation, UK: 2016. [updated on 2016 Apr 26; cited on 2016 Aug 06]. Available from: http://www.crossref.org/crosscheck/index.html . [Google Scholar]
- 15.Shafer SL. Plagiarism is ubiquitous. Anesth Analg. 2016;122:1776–80. doi: 10.1213/ANE.0000000000001344. [DOI] [PubMed] [Google Scholar]
- 16.Abraham P. Duplicate and salami publications. J Postgrad Med. 2000;46:67–9. [PubMed] [Google Scholar]
- 17.Supak Smolcic V. Salami publication: Definitions and examples. Biochem Med (Zagreb) 2013;23:237–41. doi: 10.11613/BM.2013.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Taichman DB, Backus J, Baethge C, Bauchner H, de Leeuw PW, Drazen JM, et al. Sharing clinical trial data: A proposal from the international committee of medical journal editors. JAMA. 2016;315:467–8. doi: 10.1001/jama.2015.18164. [DOI] [PubMed] [Google Scholar]
- 19.Marusic A, Wager E, Utrobicic A, Rothstein HR, Sambunjak D. Interventions to prevent misconduct and promote integrity in research and publication. Cochrane Database Syst Rev. 2016;4:MR000038. doi: 10.1002/14651858.MR000038.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]


