Abstract
Introduction:
Recently, multidetector computed tomography (MDCT) has been introduced into clinical practice. MDCT has become the noninvasive diagnostic test of choice for detailed evaluation of biliary obstruction.
Aim:
the main objective of the present study was to evaluate the diagnostic value of MDCT compared to invasive procedures for detecting biliary obstruction causes.
Material and Methods:
Since February 2009 until May 2011 fifty biliary obstruction patients based on clinical, laboratory or ultrasonographic findings, were evaluated by Multidetector-row computed tomography. The causes of biliary obstruction, which was identified using. MDCT were classified into three categories: calculus, benign stricture, and malignancy. Final diagnosis was conducted based on percutaneous transhepatic cholangiography (PTC), endoscopic retrograde cholangiopancreatography, biopsy, or surgery. The MDCT diagnosis and were compared with the final diagnosis.
Results:
A correct diagnosis of causes of biliaryobstruction was made on the basis of MDCT findings for 44 of the total 50 patients. Two patients with chronic pancreatitis were incorrectly diagnosed with a pancreatic head adenocarcinoma on the basis of MDCT findings. One patient with biliary stone was incorrectly diagnosed with a periampullary adenocarcinoma on the basis of MDCT findings. The Sensitivity, specificity and accuracy of MDCT in the diagnosis of causes of biliary obstruction were 94.12% and87.87% and94.6% respectively.
Conclusion:
Based on the findings of this study MDCT has an excellent image quality, providing valuable information about the biliary tree and other abdominal organs. The use of advanced image processing, including maximum intensity projection and multiplanar reconstruction (especially coronal or sagittal reformatted images), allows superior visualization of the biliary tree and vascular structures. Three-dimensional reconstruction images complement axial images by providing a more anatomically meaningful display of the lesion and its relationship to adjacent structures, and accurate determining the craniocaudal extent of the lesion. High accuracy, wide availability and ease of use, make the MDCT the imaging modality of choice for evaluation of biliary obstruction.
Keywords: Biliary obstruction, Diagnosis, Multidetector-row computed tomography, Accuracy, Sensitivity
1. INTRODUCTION
Jaundice is classified into three categories: Pre-hepatic, Hepatocellular (hepatic) and Post-hepatic (1, 2). Post-hepatic jaundice (obstructive jaundice) is caused by an interruption to the drainage of bile in the biliary system. Gallstones in the common bile duct, and pancreatic cancer in the head of the pancreas are the most common causes for the obstructive jaundice. There are other causes such as strictures of the common bile duct, biliary atresia, ductal carcinoma, Mirizzi’s syndrome, pancreatitis and pancreatic pseudocysts (3, 4). Direct Cholangiography methods are the gold standard techniques for evaluation the biliary obstruction. Endoscopic retrograde cholangiopancreatography (ERCP) allow both: a direct visualization of biliary tree and therapeutic intervention. When ERCP is not effective, percutaneous transhepatic cholangiography (PTC) can be performed, due to luminal obliteration by tumor tissue. Even so, they are invasive. Moreover the surrounding organs cannot be demonstrated with these techniques (5, 6). Imaging had some advantages and applications such as (a) noninvasive diagnosis and characterization of biliary obstruction (b) confirmation of diagnosis, (c) pretherapeutic staging, and (d) screening of high-risk patients. Ultrasonography (US) is the initial screening imaging modality for evaluating biliary dilatation in patients with biliary obstruction because it is inexpensive and widely available. However the sensitivity of US in detecting the cause of biliary obstruction is as low as 33% (7,8). Despite the all advantages of MR cholangiography as a noninvasive tool for evaluating the biliary and as an alternative to ERCP, reliable differentiation of a malignant from a benign stricture is not always possible at MR imaging. In addition, MR imaging is a relatively poor method in the evaluation of intraductal lesions following stent placement (9). Axial conventional CT could not provide adequate information of biliary abnormalities since the orientation of these ducts was not suitable for evaluation in axial planes (1). Nowadays, with development of multidetector scanners, MDCT has become the noninvasive diagnostic test of choice for detailed evaluation of biliary obstruction. Multidetector CT can be used as a versatile and available method. Multiphase scanning with the use of advanced image processing, including maximum intensity projection and multiplanar reconstruction (especially coronal or sagittal reformatted images). It provides insights on the level and cause of biliary obstruction and helps survey the entire abdomen for disease staging (3, 10).
2. MATERIALS AND METHODS
Since February 2009 until May 2011, we conducted a prospective study on 50 patients – 21 males and 29 females (in the old range 8 to 87 years). Institutional review committee approval and patient’s written informed consent were obtained. All patients had symptoms and signs of biliary obstruction including jaundice, total bilirubin level > 1.2 mg/dl T, direct bilirubin level > 0.5 mg/dl, alkaline phosphatase level >100 IU/L. All the patients were evaluated by Multidetector-row computed tomography. MDCT examinations were performed with a 16- channel Somatom sensation MDCT (Siemens Medical. Systems, Germany) using the following parameters: collimation, 4 x 1mm; slice width, 1.25 mm; reconstruction interval, 1 mm; 120mAs; and 140 kV. Scanning was performed from the hepatic dome to the level of the L3 vertebra. First, pre-contrast abdominal CT scans were performed to screen for calculi. Then, arterial Phase CT scans were obtained 35 seconds after initiation of intravenous injection of contrast and finally portovenous phase CT scans were obtained 70 seconds after initiation of intravenous injection of 100 ml of nonionic contrast agent at a flow rate of 2.0 to 4.0 ml/sec. All images obtained were transferred to a work station system. With the use of post processing techniques, coronal and sagittal multiplanar reconstruction images were produced. Also minimum intensity projection views (for the study of dilated bile ducts), Maximum intensity projection views (for the study of blood vessels) and volume Rendering views (for a review of three-dimensional biliary tree anatomy) were created. All images obtained were analyzed by an experienced radiologist. He evaluated the presence, the level and the cause of the obstruction. He was also asked to determine whether the obstruction is regular or irregular, and estimate the degree of biliary tree dilatation above the level of obstruction,(mild 7-11 mm, moderate 12-16 mm, or severe greater than 17mm).
The causes of biliary obstruction were identified using MDCT and were classified into three categories: calculus, benign stricture, and malignancy. On MDCT, biliary stone was suggested by the appearance of a high-density material surrounded by hypodense bile in the bile duct
A malignant tumor was suggested by the visualization of an abrupt irregular narrowing or obstruction in the bile duct (Figure 2) (11). A benign stricture was suggested by the presence of smooth narrowing in a short segment of the bile duct (12). Final diagnosis was based on endoscopic retrograde cholangiopancreatography (ERCP), percutaneous transhepatic cholangiography (PTC), biopsy, or surgery. On the basis of MDCT findings, 27 patients underwent ERCP, 17 patients underwent surgery, percutaneous biopsy was performed in 5 patients, and one patient underwent PTC. Sensitivity, specificity, and accuracy of MDCT were calculated by comparing the MDCT data with the data obtained with invasive procedures (7, 13).
Figure 1.
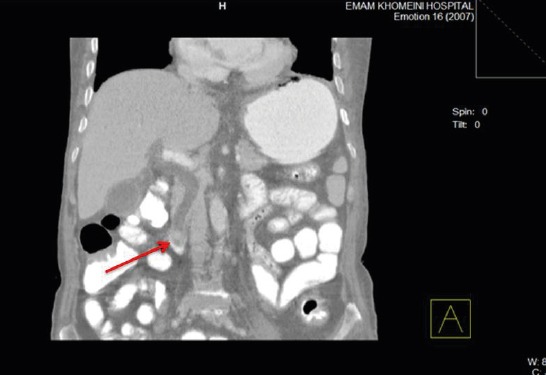
A 48-year-old woman with biliary obstruction. MDCT image shows dilatation of common bile duct and oval hyper dense material (arrow) surrounded by hypodense bile in distal common bile duct, suggesting the presence of biliary stone.
Figure 2.
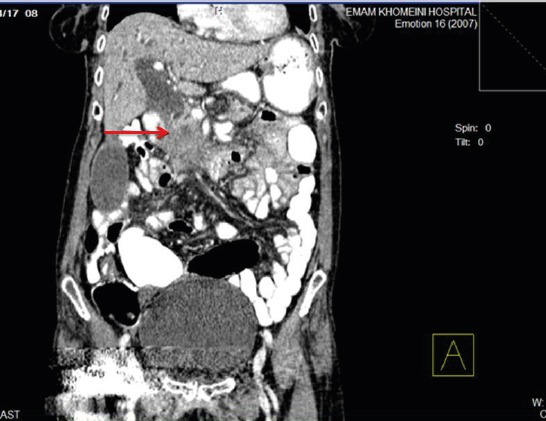
56-year-old woman with biliary obstruction secondary to tumor in pancreatic head. MDCT image shows irregular narrowing (arrow) and dilatation in common bile duct.
3. RESULTS
In this study based on MDCT findings in 50 patients, 27 patients (54%) with malignant obstruction of the biliary ducts, 17 patients (34%) with obstruction by biliary stone and in 6 patients (12%), obstruction by benign factors were reported. Finally, 27 patients of 50 patients undergoing ERCP, Surgery and tissue sampling was performed in 17 patients. Five patients underwent percutaneous biopsy, and PTC was performed in one patient. According to the above reference, In 24 patients (48%), obstruction of the bile ducts with malignant agents, in 18 patients (36%) obstruction of biliary ducts with biliary stone, and in 8 patients (16%) obstruction of biliary ducts with benign causes were confirmed. The Sensitivity, specificity and accuracy of MDCT in the diagnosis of causes of biliary obstruction were 94.12% and 87.87% and 94.6% respectively. Findings of MDCT compared with the final diagnoses are summarized in Table 1.
Table 1.
MDCT Versus Reference Examination in Diagnosis of Biliary Obstruction. a Includes ERCP, percutaneous transhepatic cholangiography, endoscopic and percutaneous biopsy, and surgery.
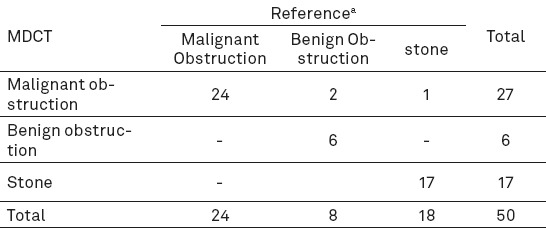
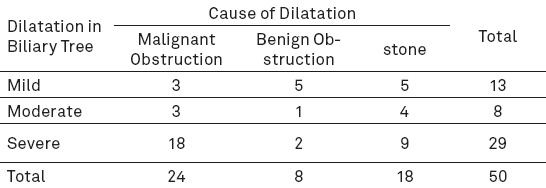
In the evaluation of 50 patients using MDCT, malignant obstruction of the bile ducts was diagnosed in 27 patients. In a survey conducted by the reference methods, in the 24 cases of 50 patients, malignant obstruction was confirmed. Pancreatic head Adenocarcinoma in 2 cases diagnosed by MDCT, eventually diagnosed with chronic pancreatitis. Also one patient with diagnosis of periampulary adenocarcinoma in MDCT, eventually diagnosed with biliary stone. Also, a total of 5 cases of peripheral cholangiocarcinoma and a Klatskin tumor (or hilar cholangiocarcinoma) was diagnosed using MDCT (Figure 3). In all cases with a diagnosis of cholangiocarcinoma, the final diagnosis was approved by the reference methods. Sensitivity, specificity and accuracy of MDCT in the diagnosis of malignant biliary obstruction were 95.8% and 84.6% and 90% respectively. Sensitivity, specificity and accuracy of MDCT in the diagnosis of benign causes of biliary obstruction were 62.5% and 95.8% and 87.5% respectively. In this study, the rate of biliary dilation at the proximal site of obstruction, on the MDCT images were measured in millimeters. Degree of biliary duct dilatation was classified as mild (7-11mm), moderate (12-16mm), and severe (Higher than 17mm). There was no significant relationship between degree of biliary duct dilatation and the cause of obstruction. However the presence of severe biliary dilatation without detectable stones should raise a concern of malignancy. The degree of biliary dilatation seen on MDCT and the final diagnosis is summarized in Table 2.
Figure 3.

Klatskin tumor in a 57-year-old man with weight loss, jaundice and abdominal pain. Coronal minimum-intensity-projection image indicates the dilated biliary tree in both hepatic lobes and obstruction by a hilar cholangiocarcinoma (arrow).
Table 2.
Degree of biliary dilatation seen on MDCT in patients with biliary obstruction
In this study, a significant relationship was found between the pattern of obstruction and obstructive agents. In this regard, obstructive pattern was classified as sudden and regular, or gradually and irregular. Many benign conditions cause a short segment and regular obstruction; however, obstruction by malignant causes was often long segment and irregular.
4. DISCUSSION
Ultrasonography is the first-line imaging modality in patients with biliary obstruction. The ultrasonography as non-invasive, rapid and inexpensive technique is very operator dependent. In the literature, a sensitivity range of 20 to 80% is often documented (3, 7). Our results for US diagnostic accuracy, sensitivity and specificity are in accordance with those reported in the other literature, 33.4% and 13.3% and 33.3% respectively. MRCP refers to selective MRI of the pancreatic and biliary ducts. MRCP offers a high diagnostic accuracy in evaluation of biliary duct pathology, however, the limited availability, high cost, and long examination time limit its use (7, 9). ERCP is both an endoscopic and a radiological procedure. It is one of several invasive direct cholangiography techniques, along with percutaneous trans-hepatic cholangiography (PTC). ERCP is currently the “gold standard” for the diagnosis of pancreatic and biliary ductal pathology. ERCP has some advantages over other noninvasive techniques since it provides both diagnosis and therapeutic intervention in the same setting. Biopsy can also be performed to establish tissue diagnosis. However, ERCP does not provide extra-luminal information. Moreover, it has a failure rate of 3-10% and 0.5-5% rate of complications, including adverse reaction from sedatives, pancreatitis, and perforation of the gastrointestinal tract, bleeding, cholangitis, sepsis, and death (6, 14). On the use of MDCT in the evaluation of biliary obstruction limited research has been done. Ahmetoghlo A. ET al. were reviewed the use of MDCT in patients with biliary obstruction. In this prospective study, 34 patients with biliary obstruction have been evaluated. The accuracy of MDCT in the diagnosis of biliary obstruction has been estimated at 83.3%. Also in this study the sensitivity and specificity of MDCT in the diagnosis of gallstones, respectively 93% and 89% have been reported (3). In research conducted in 2010 by Tongdee et al. the accuracy of MDCT in determining the cause of biliary obstruction in 50 patients was calculated. In this study, the sensitivity, specificity and accuracy of MDCT in the diagnosis of gallstones, respectively, 91.7%, 100%, 96%, was calculated (7).
In our study of 18 patients with gallstones, 17 patients were diagnosed correctly by MDCT. Sensitivity, specificity and accuracy of MDCT in the diagnosis of gallstones, respectively 94.5% and 100% and 94.12% were calculated. In previous studies conducted on the sensitivity and specificity, and accuracy of MRCP in the diagnosis of gallstones in this way amounts to between 81-100%, 84-100%, 90-96% have been calculated (9, 12-18). The results indicate that both methods are comparable in this way. Our results show high sensitivity, specificity and accuracy of MDCT in the diagnosis of malignant biliary obstruction (Respectively 95.8%, 84.6%, 90%). These results significantly from the results of axial CT in the diagnosis of malignant biliary obstruction (sensitivity 77% and specificity 63%) are better (4). In our study correct diagnosis of biliary obstruction in 44 patients of 50 patients were given. The sensitivity, specificity and accuracy of MDCT in the diagnosis of biliary obstruction in comparison with other invasive methods, respectively, 94.12%, 87.87% and 94.6% was calculated. These results are comparable with the results in the study by Choi et al. with an accuracy calculated of 90% and the study by Tongdee et al. with an accuracy calculated of 88.5% (7).
5. CONCLUSION
Our study confirms that MDCT with the use of advanced image processing, including maximum intensity projection and multiplanar reconstruction (especially coronal or sagittal reformatted images), allows superior visualization of the biliary tree and vascular structures. Three-dimensional reconstruction images complement axial images by providing a more anatomically meaningful display of the lesion and its relationship to adjacent structures, and accurate determining the craniocaudal extent of the lesion. In this method also a full view of the relevant adjacent organs including the liver, pancreas and the duodenum are shown. Compared with MRCP, MDCT procedures are easier to apply, imaging speed and spatial resolution of the images is up, and interpret the resulting images is easier. MDCT is noninvasive and fast for the diagnosis of benign and malignant causes of biliary obstruction. High accuracy, wide availability and ease of use, make the MDCT the imaging modality of choice for evaluation of biliary obstruction.
Footnotes
• Conflict of interest: none declared.
REFERENCES
- 1.Varghese JC, Farrell MA, Courtney G, Osborne H, Murray FE, Lee MJ. A prospective comparison of magnetic resonance cholangiopancreatography with endoscopic retrograde cholangiopancreatography in the evaluation of patients with suspected biliary tract disease. Clin Radiol. 1999;54:513–20. doi: 10.1016/s0009-9260(99)90848-6. [DOI] [PubMed] [Google Scholar]
- 2.Freeny PC, Ball TJ. Endoscopic retrograde cholangiopancreatography (ERCP) and percutaneous transhepatic cholangiography (PTC) in the evaluation of suspected pancreatic carcinoma: diagnostic limitations and contemporary roles. Cancer. 1981;47:1666–78. doi: 10.1002/1097-0142(19810315)47:6+<1666::aid-cncr2820471435>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 3.Ahmetoğlu A, Koşucu P, Kul S, Dinç H, Sari A, Arslan M, Alhan E. MDCT cholangiography with volume rendering for the assessment of patients with biliary obstruction. AJR Am J Roentgenol. 2004;183:1327–32. doi: 10.2214/ajr.183.5.1831327. [DOI] [PubMed] [Google Scholar]
- 4.Rösch T, Meining A, Frühmorgen S, Zillinger C, Schusdziarra V, Hellerhoff K, Classen M, Helmberger H. A prospective comparison of the diagnostic accuracy of ERCP, MRCP, CT, and EUS in biliary strictures. Gastrointest Endosc. 2002;55:870–6. doi: 10.1067/mge.2002.124206. [DOI] [PubMed] [Google Scholar]
- 5.Pasanen PA, Partanen KP, Pikkarainen PH, Alhava EM, Janatuinen EK, Pirinen AE. A comparison of ultrasound, computed tomography and endoscopic retrograde cholangiopancreatography in the differential diagnosis of benign and malignant jaundice and cholestasis. Eur J Surg. 1993;159:23–9. [PubMed] [Google Scholar]
- 6.Kim MJ, Mitchell DG, Ito K, Outwater EK. Biliary dilatation: differentiation of benign from malignant causes-value of adding conventional MR imaging to MR cholangiopancreatography. Radiology. 2000;214:173–81. doi: 10.1148/radiology.214.1.r00ja35173. [DOI] [PubMed] [Google Scholar]
- 7.Tongdee T, Amornvittayachan O, Tongdee R. Accuracy of multidetector computed tomography cholangiography in evaluation of cause of biliary tract obstruction. J Med Assoc Thai. 2010;93:566–73. [PubMed] [Google Scholar]
- 8.Choi JY, Lee JM, Lee JY, Kim SH, Lee MW, Han JK, Choi BI. Navigator-triggered isotropic three-dimensional magnetic resonance cholangiopancreatography in the diagnosis of malignant biliary obstructions: comparison with direct cholangiography. J Magn Res Imaging. 2008;27:94–101. doi: 10.1002/jmri.21038. [DOI] [PubMed] [Google Scholar]
- 9.Alcaraz MJ, De la Morena EJ, Polo A, Ramos A, De la Cal MA, González Mandly A. A comparative study of magnetic resonance cholangiography and direct cholangiography. Rev Esp Enferm Dig. 2000;92:427–38. [PubMed] [Google Scholar]
- 10.Khan SA, Davidson BR, Goldin R, Pereira SP, Rosenberg WM, Taylor-Robinson SD, Thillainayagam AV. Guidelines for the diagnosis and treatment of cholangiocarcinoma: consensus document. Gut. 2002;51:I1–9. doi: 10.1136/gut.51.suppl_6.vi1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zandrino F, Benzi L, Ferretti ML, Ferrando R, Reggiani G, Musante F. Multislice CT cholangiography without biliary contrast agent: technique and initial clinical results in the assessment of patients with biliary obstruction. EurRadiol. 2002;12:1155–61. doi: 10.1007/s00330-001-1188-y. [DOI] [PubMed] [Google Scholar]
- 12.Soto JA, Alvarez O, Munera F, Velez SM, Valencia J, Ramirez N. Diagnosing bile duct stones: comparison of unenhanced helical CT, oral contrast-enhanced CT cholangiography, and MR cholangiography. AJR Am J Roentgenol. 2000;175:1127–34. doi: 10.2214/ajr.175.4.1751127. [DOI] [PubMed] [Google Scholar]
- 13.Baron RL, Tublin ME, Peterson MS. Imaging the spectrum of biliary tract disease. Radiol Clin North Am. 2002;40:1325–54. doi: 10.1016/s0033-8389(02)00045-3. [DOI] [PubMed] [Google Scholar]
- 14.Taylor AC, Little AF, Hennessy OF, Banting SW, Smith PJ, Desmond PV. Prospective assessment of magnetic resonance cholangiopancreatography for noninvasive imaging of the biliary tree. Gastrointest Endosc. 2002;55:17–22. doi: 10.1067/mge.2002.120324. [DOI] [PubMed] [Google Scholar]
- 15.Fleischmann D, Ringl H, Schöfl R, Pötzi R, Kontrus M, Henk C, Bankier AA, Kettenbach J, Mostbeck GH. Three-dimensional spiral CT cholangiography in patients with suspected obstructive biliary disease: comparison with endoscopic retrograde cholangiography. Radiology. 1996;198:861–8. doi: 10.1148/radiology.198.3.8628884. [DOI] [PubMed] [Google Scholar]
- 16.Choi JY, Lee JM, Lee JY. Assessment of hilar and extrahepatic bile duct cancer using multi-detector CT: value of adding multiplanar reformations to standard axial images. EurRadiol. 2007;17:3130–8. doi: 10.1007/s00330-007-0658-2. [DOI] [PubMed] [Google Scholar]
- 17.Ghimire R, Lohani B, Pradhan S. Accuracy of ultrasonography in evaluation of level and cause of biliary obstruction: a prospective study. Kathmandu Univ Med J (KUMJ) 2005;3:17–21. [PubMed] [Google Scholar]
- 18.Cho ES, Park MS, Yu JS, Kim MJ, Kim KW. Biliary ductal involvement of hilarcholangiocarcinoma: multidetector computed tomography versus magnetic resonance cholangiography. J Comput Assist Tomogr. 2007;31:72–8. doi: 10.1097/01.rct.0000230013.24091.8e. [DOI] [PubMed] [Google Scholar]


