Abstract
Introduction:
Positron emission tomography/computed tomography (PET-CT) is very sensitive for diagnosis of recurrent NSCLC and has a significant impact on change of management. Preliminary data suggest superiority of PET-CT comparing to CT alone for lung cancer restaging.
Materials and methods:
This is a retrospective study which aim is to validate usage of PET-CT in suspected non-small cell lung carcinoma recurrence and its impact on further patient management. Total number of 31 patients with non-small cell lung carcinoma and uncertain diagnosis of recurrent disease or its extent after routine clinical and CT work-up were enrolled in this study.
Discussion:
We found in our study that PET-CT diagnosed recurrent disease in 65% of patients who were previously presented with an indeterminante CT. In 85% of patients there were change in further management.
Conclusion:
We suggest that PET should be performed on patients who have suspected relapse after potentially curative treatment, particularly if active treatment is being considered. PET-CT improved the diagnosis of recurrent NSCLC and this resulted in a significant impact and change in further patient management.
Keywords: NSCLC, PET-CT, impact, post-treatment, management
1. INTRODUCTION
When we are discussing the post-treatment management of patients with non-small cell lung carcinoma (NSCLC) it is important to point out that there are different opinions regarding tests used for monitoring of the disease. Controversy exists about diagnostic tests which should be used during surveillance and how often they should be used. The main reason for this is that there is, at the moment, no evidence that earlier treatment of recurrent disease leads to a better effect. Certain scientific societies recommend in their guidelines only physical examination every 3 months (ASCO), and other societies like the American College of Radiology, NCCN and ACCP suggest annual CT scan as stated in their guidelines. Still, there are many questions in the post-treatment period that should be answered, like complication of treatment, disease recurrence, or new primary tumors (1).
There are different studies about PET-CT used for early diagnosis of recurrence, which reports better sensitivity, specificity and accuracy for PET-CT comparing to other tests used during surveillance period. But this diagnostic tool is not yet recommended in guidelines, mostly because of the lack of evidence that earlier diagnosis of recurrence have significant survival benefit. The other important thing is that more intensive monitoring is certainly much more expensive (1).
Follow up of patients with NSCLC is based on early detection of recurrence and also control of complications due to treatment (2-3). Despite curative resection 30% to 55% of patients with NSCLC evolve recurrence and eventually die of their disease (4). Therefore, many patients die of their disease related to recurrence after surgery (5-6).
Very often patients complain of residual symptoms or diagnostic imaging display abnormalities. That precipitate evaluation for residual or recurrent disease. CT is currently the standard diagnostic imaging tool for reevaluation of previously treated NSCLC patients, particularly if symptoms persist or surveillance suggest disease relapse. But computed tomography (CT) based differentiation of necrotic tissue induced by therapy and residual or recurrent carcinoma is very difficult, sometimes impossible leading to many equivocal CT results. Valid and timely diagnosis of recurrence is extremely significant for initiating therapy sooner and shortening the period of patient anxiety or to avoid unnecessary treatment.
Positron emission tomography/computed tomography (PET-CT) is very sensitive for diagnosis of recurrent NSCLC and has a significant impact on change of management (7). Preliminary data suggest superiority of PET-CT comparing to CT alone for lung cancer restaging (8-9) and a markedly poorer prognosis for patients with positive PET-CT findings than for those with negative PET-CT findings (10).
FDG-PET imaging can depict local recurrence of NSCLC after surgical resection, chemotherapy, or radiotherapy, and this is possible before anatomic changes are visible on conventional imaging (11-14). Some patients with localized relapsed lung cancer may be cured with appropriate aggressive therapy and preliminary data suggest that PET-CT can identify such patients better than other diagnostic methods (15).
2. MATERIALS AND METHODS
Total number of 31 patients with non-small cell lung carcinoma and uncertain diagnosis of recurrent disease or its extent after routine clinical and CT work-up in the period of March 2014 to February 2016, were enrolled in this study. Patients were eligible for this study if they had a confirmed histologic diagnosis of NSCLC and had been treated with curative intent 6 months before referral for a PET-CT scan.
This is a retrospective study which aim is to validate usage of PET-CT in suspected non-small cell lung carcinoma recurrence and its impact on further patient management.
All patients had indeterminante CT findings. All of them performed PET-CT study and findings are recorded with confirmation or exclusion of recurrent disease. Patients were classified as negative if imaging showed no abnormality suggestive of recurrence. Positive PET-CT scans were classified as localised relapse or distant disease. We used medical histories from Clinic for Oncology and recorded all changes in patient management after PET-CT study. Treatment intent was categorized by an oncologist experienced in lung cancer management, who synthesized the available pre-PET clinical and imaging information. Any change in patient further management was noted. All interventions and procedures that were supposed to be done before PET-CT study and were canceled after, were recorded.
3. RESULTS
In our study were included 58% males and 42% females. Patients have a hystologycal type of NSCLC as follows: 19 (%) patients had adenocarcinoma, 11 (%) patients were diagnosed as squamocellular carcinoma and 1 (%) had large cell undifferentiated carcinoma (Chart 1).
Chart 1.
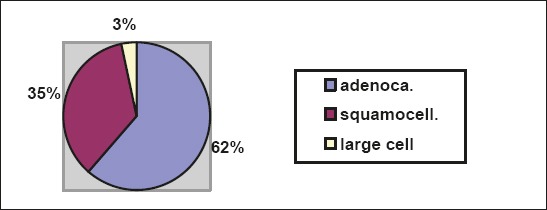
Patient distribution according to hystologycal type of NSCLC
PET-CT analysis found recurrent disease in 20 patients, and 11 patients did not have PET-CT confirmation of recurrence (Table 1).
Table 1.
Patient distribution according to PET-CT findings

All patients with PET-CT confirmed relapse of disease were classified based on PET-CT findings as locally relapsed or distant disease (Chart 2).
Chart 2.
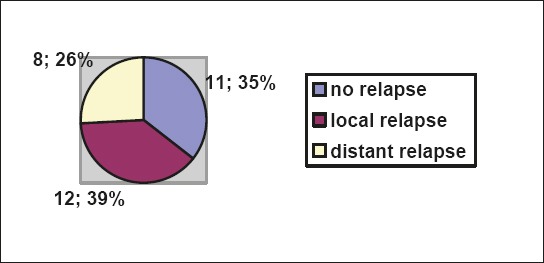
Patient distribution (n=31) according to PET-CT findings of relapsed disease
Medical histories of patients with PET-CT confirmed recurrent disease were analyzed and we found that in 17 (85%) patients there were change in further management. For the rest of 3 patients we did not found any data (Table 2).
Table 2.
Patients distribution (n=20) according to PET CT diagnosis of recurrent disease and impact on further management
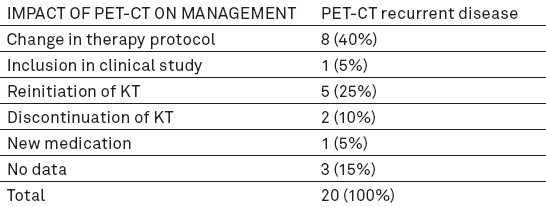
Table 3.
Patients distribution (n=11) according to PET CT diagnosis of non- recurrent disease and impact on further management

In the group of patients without diagnosis of recurrent disease there were mostly no any further changes in management (64% of patients). PET-CT findings suggestive for non- recurrent disease show also impact on further management in 4 (36%) patients.
4. DISCUSSION
We found in our study that PET-CT diagnosed recurrent disease in 65% patients who were previously presented with an indeterminante CT. In the study of Bury et all., PET, for the detection of recurrent carcinoma in patients who have been treated with early apparent curative result, has a sensitivity of 100%, a specificity of 97%, a PPV of 93%, an NPV of 100% and a diagnostic accuracy of 98% (95% CI 90±99%). By comparison, the accuracy of CT in this analysis was 91% (95% CI 81±97%) (15). We could not calculate sensitivity, specificity, PPV and NPV as there were no possibilities to have histology confirmation - gold standard.
Further change in therapy management in our study was observed in 85% of patients with PET-CT confirmed recurrent disease. In a study performed by Hicks et all. published in The Journal of Nuclear Medicine the PET results had a high impact on management in 40 patients (63%) (16).
PET-CT showed no signs of recurrent disease in 35% patients. In this group of patients 36% still have change in further management after exclusion of recurrent disease.
Of potential economic and clinical importance in previously mentioned study by Hicks et all. was the observation that 15 patients (24%) in this group who were suspected to have relapsed by conventional imaging subsequently received no active treatment after a negative PET-CT. Only 1 of these patients had relapse confirmed on follow-up. By preventing treatment in these patients, PET is likely to have reduced expenditure but also spared these patients unwarranted toxicity (17, 18).
We found in our study that 64% of patients who were PET-CT negative and had suspicious of relapse on CT, that way consequently avoided planned KT.
5. CONCLUSION
We suggest that PET should be performed on patients who have suspected relapse after potentially curative treatment, particularly if active treatment is being considered. PET-CT improved the diagnosis of recurrent NSCLC and this resulted in a significant impact and change in further patient management.
Footnotes
• Conflict of interest: none declared.
REFERENCES
- 1.Crino L, Weder W, van Meerbeeck J, Felip E On behalf of the ESMO Guidelines Working Group. Early stage and locally advanced (non-metastatic) non-small-cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Annals of Oncology. 2010;21(Supplement 5):v103–v115. doi: 10.1093/annonc/mdq207. [DOI] [PubMed] [Google Scholar]
- 2.Keidar Z, Haim N, Guralnik L, Wollner M, Bar-Shalom R, Ben-Nun A, Israel O. PET/CT using 18F-FDG in Suspected Lung Cancer Recurrence: Diagnostic Value and Impact on Patient Management. The Journal of Nuclear Medicine. 2004;45:10. [PubMed] [Google Scholar]
- 3.Colice GL, Rubins J, Unger M. Follow up and surveillance of the lung cancer patient following curative-intent therapy. Chest. 2003;123:272S–283S. doi: 10.1378/chest.123.1_suppl.272s. [DOI] [PubMed] [Google Scholar]
- 4.Carnio S, Novello S, Papotti M, et al. Prognostic and predictive biomarkers in early stage non small-cell lung cancer: tumor based approaches including gene signatures. Transl Lung Cancer Res. 2013;2:372–81. doi: 10.3978/j.issn.2218-6751.2013.10.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yamashita T, Uramoto H, Onitsuka T, et al. Association between lymphangiogenesis-/micrometastasis- and adhesion-related molecules in resected stage I NSCLC. Lung Cancer. 2010;70:320–8. doi: 10.1016/j.lungcan.2010.02.013. [DOI] [PubMed] [Google Scholar]
- 6.Uramoto H, Tanaka F. Prediction of recurrence after complete resection in patients with NSCLC. Anticancer Res. 2012;32:3953–60. [PubMed] [Google Scholar]
- 7.Frank A, Lefkowitz D, Jaeger S, et al. Decision logic for retreatment of asymptomatic lung cancer recurrence based on positron emission tomography findings. Int J Radiat Oncol Biol Phys. 1995;32:1495–512. doi: 10.1016/0360-3016(94)00622-R. [DOI] [PubMed] [Google Scholar]
- 8.Patz EF, Lowe V, Hoffman JM, Paine SS, Harris LK, Goodman PC. Persistent or recurrent bronchogenic carcinoma: detection with PET and 2-[F-18]-2-deoxy-Dglucose. Radiology. 1994;191:379–82. doi: 10.1148/radiology.191.2.8153309. [DOI] [PubMed] [Google Scholar]
- 9.Inoue T, Kim EE, Komaki R, et al. Detecting recurrent or residual lung cancer with FDG-PET. J Nucl Med. 1995;36:788–93. [PubMed] [Google Scholar]
- 10.Patz EF, Connolly J, Herndon J. Prognostic value of thoracic FDG PET imaging after treatment for non-small cell lung cancer. AJR. 2000;174:769–74. doi: 10.2214/ajr.174.3.1740769. [DOI] [PubMed] [Google Scholar]
- 11.Frank A, Lefkowitz D, Jaeger S, et al. Decision logic for retreatment of asymptomatic lung cancer recurrence based on positron emission tomography. Int J Radiat Oncol Biol Phys. 1995;32:1495–512. doi: 10.1016/0360-3016(94)00622-R. [DOI] [PubMed] [Google Scholar]
- 12.Hicks RJ, Kalff V, MacManus MP, Ware RE, McKenzie AF, Matthews JP, Ball DL. The utility of 18F-FDG PET for suspected recurrent non–small cell lung cancer after potentially curative therapy: impact on management and prognostic stratification. J Nucl Med. 2001;42:1605–13. [PubMed] [Google Scholar]
- 13.Ryu JS, Choi NC, Fischman AJ, Lynch TJ, Mathisen DJ. FDG-PET in staging and restaging non-small cell lung cancer after neoadjuvant chemoradiotherapy: correlation with histopathology. Lung Cancer. 2002;35:179–87. doi: 10.1016/s0169-5002(01)00332-4. [DOI] [PubMed] [Google Scholar]
- 14.Keidar Z, Haim N, Guralnik L, Wollner M, Bar-Shalom R, Ben-Nun A, Israel O. PET/CT using 18F-FDG in suspected lung cancer recurrence: diagnostic value and impact on patient management. J Nucl Med. 2004;45:1640–6. [PubMed] [Google Scholar]
- 15.Hellwig D, Groschel A, Graeter TP, Hellwig AP, Nestle U, Schäfers HJ, Sybrecht GW, Kirsch CM. Diagnostic performance and prognostic impact of FDG-PET in suspected recurrence of surgically treated non-small cell lung cancer. Eur J Nucl Med Mol Imaging. 2006;33:13–21. doi: 10.1007/s00259-005-1919-4. [DOI] [PubMed] [Google Scholar]
- 16.Bury T, Corhay JL, Duysinx B, et al. Value of FDG-PET in detecting residual or recurrent nonsmall cell lung cancer. Eur Respir J. 1999;14:1376177–1380. doi: 10.1183/09031936.99.14613769. [DOI] [PubMed] [Google Scholar]
- 17.Hicks RJ, Kalff V, et al. The Utility of 18F-FDG PET for Suspected Recurrent Non–Small Cell Lung Cancer After Potentially Curative Therapy: Impact on Management and Prognostic Stratification. J Nucl Med. 2001;42:1605–13. [PubMed] [Google Scholar]
- 18.Beslic N, Sadija A, Milardovic R, Ceric T, Ceric S, Beganovic A, Kristic S, Cavaljuga S. Advantages of Combined PET-CT in Mediastinal Staging in Patients with Non-small Cell Lung Carcinoma. Acta Inform Med. 2016 Apr;24(2):99–102. doi: 10.5455/aim.2016.24.99-102. doi: 10.5455/aim.2016.24.99.102. [DOI] [PMC free article] [PubMed] [Google Scholar]


