Abstract
Objective:
To show the place and role of continuous electrocardiographic twenty-four-hour ECG monitoring in daily clinical practice of pediatric cardiologists.
Methods:
According to protocol, 2753 patients underwent dynamic continuous ECG Holter monitoring (data collected from the “Register of ECG Holter monitoring” of Pediatric Clinic, UCC Sarajevo in period April 2003- April 2015).
Results:
There were 50,5% boys and 49,5% girls, aged from birth to 19 years (1,63% - neonates and infants, 2,6% - toddlers, 9,95% - preschool children, 35,5% - gradeschoolers and 50,3% children in puberty and adolescence). In 68,1% of patients Holter was performed for the first time. Indications for conducting Holter were: arrhythmias in 42,2% cases, precordial pain in 23,5%, suspicion of pre-excitation and/or pre-excitation in 10%, crisis of consciousness in 8%, uncorrected congenital/acquired heart defects in 4,2%, operated heart defects in 3,7%, hypertension in 3,1% cases, control of the pacemaker in 1,63% and other causes in 3,5% cases. Discharge diagnosis after ECG Holter monitoring were: insignificant arrhythmias in 47,1% cases, wandering pacemaker in 21,3%, pre-excitation in 16,2%, benign ventricular premature beats in 6,3%, atrioventricular block in 3%, sinus pause in 2.2% cases and other arrhythmias in 3,5%. In mentioned period 57 cases of Wolf Parkinson White syndrome were registered, in 4,5% of patients antiarrhythmic therapy was administered. Radiofrequent ablation was performed in 23 cases.
Conclusion:
The development of pediatric cardiac surgery has initiated development of pediatric arrhythmology as imperative segment of pediatric cardiology. Continuous ECG Holter monitoring has become irreplaceable method in everyday diagnostics and therapy of arrhythmias in children.
Keywords: 24 hour ECG Holter monitoring, arrhythmia, postoperative arrhythmia, antiarrhythmic therapy
1. INTRODUCTION
Pediatric arrhythmology which studies arrhythmias (dysrhythmias) in children, is still insufficiently explored area of pediatric cardiology/cardiac surgery, whose development is the main parameter of evaluation of development of medicine, primarily in order to reduce perinatal mortality. The incidence of significant arrhythmias in children is 2%, and if talked about all insignificant rhythm disorders up to 25%. The basic mechanism for creation of arrhythmia is caused by instability of the membrane potential of the cells of the heart, which increases automatism and they become ectopic centers that alter the normal order of creation and implementation of stimulus in other parts of the heart. Pathophysiologically, there are three mechanisms of formation of dysrhythmias: occurrence of circulation in some part of the heart, occurrence of subsequent potentials or unusual occurrence of automatism. In children, dysrhythmias are most often linked to the occurrence of circular mechanisms, and the causes can be different: intracardiac and extracardiac. Studies of cell disorders are probably right path for understanding the genesis of arrhythmias. There are numerous possibilities for classification of cardiac arrhythmias which are based on clinical and electrocardiographic criteria. They are divided into rhythm disturbances in the sinus node (abnormal formation or impulse disclosure), rhythm disturbances due to the creation of ectopic impulses and rhythm disturbances due to damage in the conduction system. In relation to the place of origin they can be atrial and ventricular, and when clinically divided, they can be disturbances in heart rate (bradyarrhythmias and tachyarrhythmias), rhythm disturbances (extrasystoles) and conduction disorders (blocks). They can be acute or chronic and may occur in any life period of the child. The most common arrhythmia in children’s age is sinus tachycardia, and the most important is paroxysmal supraventricular tachycardia. The main symptoms of dysrhythmias are: sense of general weakness, fatigue, palpitations, hypotension, dizziness, nausea, pallor, cold sweat, redness of the face (flushing), although the most difficult dysrhythmia can remain asymptomatic for years. Dysrhythmias can be suspected if the aforementioned medical history occurred, in case of positive physical clinical findings (venous pulsations of the neck, pulse changes, dysrhythmic actions). Diagnosis is based on a series of diagnostic tests: electrocardiography (ECG), continuous electrocardiographic twenty-four-hour Holter monitoring, permanent methods of monitoring of the heart rate (transtelephonic ECG and loop recorder), echocardiography (and even fetal echocardiography), scintigraphy, tilt-table test, ergometry, esophageal electrophysiology, cardiac electrophysiologic studies (EPS) with programmed electrical stimulation (PES), intracardiac electrophysiology. The sensitivity of particular methods for different arrhythmias is different. Therapeutically the most important aspect of treatment is based on the use of antiarrhythmic drugs and the application of electrotherapy (electro-stimulation, electrical cardioversion, defibrillation, implantation, radiofrequent ablation). The therapeutic approach is often unfortunately individual. Continuous electrocardiographic twenty-four-hour ECG monitoring is a sovereign diagnostic method (gold standard) of arrhythmias in children.
2. AIM
The aim of this paper was to show the place and role of continuous electrocardiographic twenty-four-hour ECG monitoring in daily clinical practice of pediatric cardiologists. In early development of pediatric cardiac surgery in Bosnia and Herzegovina, which started in April 1997, the development of arrhythmology has proved to be necessary, and without continuous Holter monitoring it was unthinkable to seriously approach this problem.
3. METHODS
The research had prospective-retrospective and analytical character, and included the period April 2003- April 2015 (data collected from the “Register of ECG Holter monitoring” of Pediatric Clinic, UCC Sarajevo). According to the protocol, 2753 patients underwent dynamic continuous ECG Holter monitoring. All registrations were made during hospitalization by keeping records of activities and including records of subjective symptoms, lasting an average of 24 hours with the registration of most often between one hundred and two hundred thousand beats (or QRS complexes). Attempts in conducting methods at home did not prove applicable under our conditions. The device itself is a battery-powered tape recorder with a built-in clock, and electrodes for recording precordial leads on the chest of the patient. In general at any time they register three leads. Activity Log during registration records patient, child or parent to allow the determination of the correlation of the patient’s symptoms and the patient’s activity with the occurrence of possible arrhythmias. Keeping of activity log, dosing activities (running up the stairs, the use of test strips, etc.), control of subjective problems and checking of the electrodes, monitors competent pediatric nurse, who transferres the tape to the software system, where a pediatric cardiologist conducts the reading. Electronic processing rate, registration and presented results can be disturbed by the device malfunction, improper placement of the electrode, wetting of the device, nearness of the magnetic field, high-voltage appliances, metals and etc. On recording then are present higher number of artifacts, bizarre images, which should not be misinterpreted.
4. RESULTS
There were 1392 (50,5%) boys and 1361 (49,5%) girls and the patients were aged from birth to 19 years of life. There were 45 (1,63%) registered neonates and infants, 74 toddlers (2,6%), 274 (9,95%) preschool children, 978 (35,5%) gradeschoolers and 1385 (50,3%) children in puberty and adolescence (Figure 1).
Figure 1.
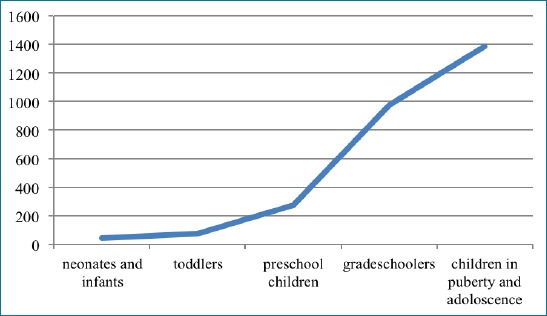
Age distribution of patients
In 1876 patients (68,1%) Holter was performed for the first time, a control ECG Holter monitoring was done in 877 (31,9%) cases. Indications for conducting Holter were: arrhythmias in 1164 (42,2%) cases, precordial pain in 648 (23,5%), suspicion of pre-excitation and/or pre-excitation in 278 (10%), crisis of consciousness in 220 (8%), uncorrected congenital/acquired heart defects in 116 (4,2%), operated heart defects in 102 (3,7%), hypertension in 85 (3,1%) cases, control of the pacemaker in 45 (1,63%), and other causes in 95 (3,5%) cases (Figure 2).
Figure 2.
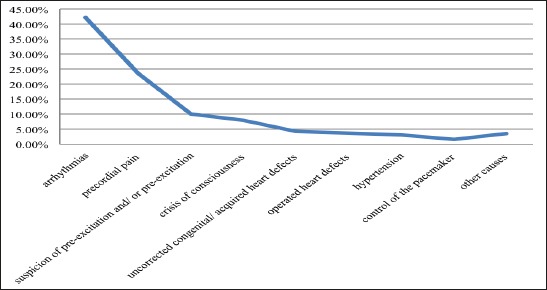
Indications for conducting ECG Holter monitoring
Discharge diagnosis after ECG Holter monitoring are: insignificant arrhythmias in 1297 (47,1%) cases, wandering pacemaker–in 588 (21,3%), pre-excitation in 448 (16,2%), benign ventricular premature beats in 175 (6,3%), atrioventricular block in 84 (3%), sinus pause in 63 (2.2%) cases and other arrhythmias in 98 (3,5%) (Figure 3).
In mentioned period 57 cases of WPW (Wolf Parkinson White) syndrome were registered, which was in most cases associated with paroxysmal supraventricular tachycardia and make the most of the discharge diagnoses of pre-excitations. In 126 (4,5%) patients antiarrhythmic therapy was administered. 29 pacemakers were implanted (of this number, 6 were congenital) and radiofrequent ablation was performed in 23 cases.
5. DISCUSSION
Registrations of dynamic 24h ECG Holter monitoring in average of about 220 pediatric patients annually is representative and good for gaining experience and knowledge, but the question remains on its rationality, better cooperation with pediatric cardiologists in the Federation of B&H, specifying indication registration, period between check ups and so on. There is no significant difference in gender structure and preponderance of children in the age over 50% during puberty and adolescence is the result of neurohormonal events is known and consistent to results of other authors. Movement of registration rhythm disturbances that is present in early neonatal and infant period (1.7%), which will with development of fetal echocardiography result in detection of fetal arrhythmia with intrauterine diagnosis and treatment (fetal echocardiography, direct intrauterine delivery of the drug in the fetal circulation or application of medication through the mother), will be even more present (1, 2). There are several open issues that are in the foreground. The most intriguing question is incisional arrhythmia, that occur after operative correction of congenital heart defects (CHD) and on which are based today’s and future research in this area. Modern pediatric cardiology today mainly deals with congenital heart defects. The incidence of congenital heart defects is 0.8-1% and represent 23% of all congenital anomalies, and they are the most common congenital anomalies (3, 4). In recent years we have witnessed an intensive development of pediatric cardiac surgery (improvement in diagnosis, interventional diagnostics, neonatal care, perfusion, anesthesia, cardiac surgery techniques, etc.) and growing possibilities of surgical treatment of most congenital heart defects, and even the most complex (5). In most cases, congenital heart anomalies require surgical treatment (60%), and sometimes in several occasions. Toll to the development and success of pediatric cardiac surgery is the appearance of numerous postoperative (incisional) arrhythmias (6). Postoperative arrhythmia is a major cause of morbidity and mortality after cardiac surgery for congenital heart disease (7). Hemodynamically CHDs are divided into congenital anomalies of the heart without the shunt (obstructive), congenital anomalies of the heart with the shunt and complex congenital heart anomalies. Anomalies with shunt are divided on the ones with left-to-right shunt and cyanogen with right-to-left shunt.
The process of creating postoperative arrhythmias occur around the scars of the surgical incision on the atrium or ventricle, around the conduits, patches and similar artifacts. Postoperative arrhythmias are usually permanent although they may be transient, but they are progressively evolving (8). Some congenital heart defects have dysrhythmia that is often associated with them, or even part of the anomalies, such as Ebstein’s anomaly, transposition of the great arteries, tricuspid atresia, total anomalous pulmonary venous return (TAPVR), atrial septal defect, atrioventricular septal defect, etc. After operative correction of congenital heart anomalies, the most common postoperative arrhythmias are right bundle branch block, atrioventricular block second degree (Mobitz type 2), atrioventricular block grade III, left bundle branch block, paroxysmal supraventricular tachycardia, and in older children atrial fibrillation (9). The hardest dysrhythmia occur after replacing the valve, and in the postoperative valvular anomalies incidence of postoperative complete block is 60-80% with thrombosis, hypovolemia and dehydration especially in young children (10). Considering that congenital heart defects have evolving character, their early diagnosis is imperative, and complete objectification due to the complex anatomy and hemodynamics, association with other anomalies have crucial importance for the pediatric cardiac surgeon. In children whose surgical treatment of congenital heart defects is postponed there is an increased risk of incisional arrhythmias (11). Empirically it was found that a higher frequency of arrhythmias after surgery of congenital heart defects are primarily a complex type, in transposition of the great arteries, ventricular septal defect, coarctation of the aorta, aortic stenosis, atrioventricular septal defect, including atrial septal defect and congenital heart defects where interventions are performed around aortic valve or at the interventricular septum (12). The surgical technique of congenital heart defects affects the type of incisional arrhythmias (12). Incisional arrhythmias are particularly common cause of sudden cardiac death in children, and even adults, especially after operated congenital aortic stenosis, tetralogy of Fallot, transposition of the great arteries so these operated congenital anomalies need special attention (12, 13). Often a decision on the treatment of certain congenital heart defects (intervention catheterization, a hybrid operation, palliative corrections, radical correction) is made by the overall occurrence of vitally threatening arrhythmias (14). At this moment occurrence of incisional arrhythmias is one of the decisive parameters for the preference of certain operational techniques. Unrecognized and inadequately treated incisional dysrhythmia can be immediate and more often, later the cause of death (15). This always has to be viewed through the prism of growth and development of the child as specificum for itself, and whose interaction with congenital heart defects and incisional arrhythmias have many factors (16). This is one reason for the dynamic development of pediatric arrhythmology. On the other hand, diagnosis and treatment of incisional arrhythmias follow this trend mainly through invasive procedures and new drugs (17). Our 116 records of ECG Holter monitoring from not operated CHDs and 102 tracks of operated heart defects and 29 implanted pacemakers often after the appearance of total AV block after surgery of CHD, suggests the size of the problem. On the other hand therapy, not only of incisional arrhythmias, is complex. The recent technical developments of electrotherapy with the discovery of new drugs has failed to resolve a number of dilemmas. From the number of implanted pacemakers, in over 50% of cases, implantation occur due to total AV block after operative correction of CHD or after block, including the SA node disease. Radiofrequency ablation was found in 23 patients, with satisfactory results in 75% of patients. 4,5% of our records were made in order to administrate treatment or therapy control from total of 21,4 % registered significant arrhythmias (pre-excitation, sinus pauses, AV blocks).
Pharmacological treatment is primarily based on the use of five groups of drugs; Group I Sodium-channel blockers with its three subgroups: quinidine, procainamide, disopyramide or lidocaine, mexiletine, tocainide, phenytoin, flecainide, propafenone, encainide, cibenzoline and lorcainide; Group II–β1 adrenergic receptor antagonists–propranolol, ormidol, atenolol, metoprolol and nadalol; Group III–Potassium channel blockers–amiodarone, sotalol, bretylium; Group IV–Calcium channel blockers-digoxin, verapamil, adenosine, diltiazem and Unclassified antiarrhythmic agents- atropine, adrenaline, isoprenaline, calcium chloride, magnesium chloride (18). In daily practice the most commonly used are calcium channel blockers and beta-blockers, while in the intensive care unit, the most often used are Calcium channel blockers and unclassified antiarrhythmics. Sotalol Hydrochloride is most used drug with satisfactory success. Treatment is usually given as monotherapy as well as combination of antiarrhythmic therapy and other therapies. Especially the application of combined treatment with metformin and sotalol in obese should be emphasized, and therapy with antihypertensives like ACE inhibitors. Disadvantages of medicamentous therapy of arrhythmias are burden of taking regular medications, recurrent arrhythmias, psychological consequences of awareness about the disease, medication side effects, risk of interaction, the need for ongoing supervision of patients, frequent specialist examinations, as well as the use of diagnostic methods, and occasional hospitalizations for arrhythmias recurrence and/or their evaluation. Criticism, self-criticism in the form of treatment therapies prognosis should be our imperative, not forgetting our social and social frameworks.
Anamnestic data should be carefully taken considering prenatal, perinatal, postnatal period, family medical history has to have special reference to the habits during pregnancy, association with other diseases, preferences to respiratory infections, poor tolerance to the stress as well as the subjective feeling of the general situation, particularly on the main symptoms of heart disease (heart failure, signs of heart failure, cyanosis, and syncope) (19).
6. CONCLUSION
The development of pediatric cardiac surgery has initiated the development of pediatric arrhythmology as imperative segment of pediatric cardiology. Continuous ECG Holter monitoring has become irreplaceable method in everyday diagnostics and therapy of arrhythmias in children.
Incisional arrhythmias will be still an open question and the subject of future research. Children arrhytmology is not an extension of adult arrhytmology and raises a lot of questions, instead of giving absolute answers at this point.
Footnotes
• Conflict of interest: none declared.
REFERENCES
- 1.Rubart M, Zipes DP. Arrhythmias, Sudden Death and Syncope. In: Bonow RO, Mann DL, Zipes DP, Libby P, editors. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 9th ed. Philadelphia: Saunders Elsevier; 2011. pp. 660–9. [Google Scholar]
- 2.Hanash CR, Crosson JE. Emergency diagnosis and management of pediatric arrhythmias. J Emerg Trauma Shock. 2010:251–60. doi: 10.4103/0974-2700.66525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jovanović I, Ðukić M, Parezanović V, Ilić S. Ostojić M, Kanjuh V, Beleslin B, editors. Urođene srčane mane. Kardiologija. Beograd, Zavod za udžbenike. 2011:588. [Google Scholar]
- 4.Massin M, Malekzadeh-Milani SG, Demanetz H, Wauthy P, Deuvaert FE, Dessy H, Verbeet T. Prevalence of early postoperative arrhythmias in children with delayed open-heart surgery for severe congenital heart disease. Acta Clin Belg. 2010:386–91. doi: 10.1179/acb.2010.65.6.003. [DOI] [PubMed] [Google Scholar]
- 5.Pflaumer A. Perspectives in ablation of arrhythmias in children and patients with congenital heart disease. Intern Med J. 2012:70–6. doi: 10.1111/j.1445-5994.2012.02899.x. [DOI] [PubMed] [Google Scholar]
- 6.Malčić I. Begovac M, editor. Osobitosti aritmija u dječjoj dobi.i sur. Aritmije u liječničkoj praksi. Zagreb, Školska knjiga. 2010:94. [Google Scholar]
- 7.Lan YT, Lee JC, Wetzel G. Postoperative arrhythmia. Curr Opin Cardiol. 2003;18(2):73–8. doi: 10.1097/00001573-200303000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Prijić S, Ađić O, Košutić J, Stajević M, Ninić S, Kuburović V, et al. Značaj magnetne rezonancije u praćenju bolesnika sa Tetralogijom Fallot. In: Zdravković D, Ðorđević M, editors. Problemi u pedijatriji 2012. Beograd: Zavod za udžbenike; 2013. pp. 132–47. [Google Scholar]
- 9.Grujić M, Mrđa S, Mujović N, Kocijančić A. In: Tahikardije. Grujić M, editor. Kosmos, Beograd: Srčane aritmije; 2010. p. 166. [Google Scholar]
- 10.Prijić S, Košutić J, Vukomanović V, Stajević M, Ninić S. In: Savremeni pristup dijagnostici i liječenju aortne stenoze kod djece. Problemi u pedijatriji 2010. Zdravković D, editor. Beograd: Zavod za udzbenike; 2011. pp. 419–32. [Google Scholar]
- 11.Alp H, Narin C, Baysal T, Sarıgül A. The prevalence of and risk factors for early postoperative arrhythmias in children after cardiac surgery [Online] 2013:85. doi: 10.1111/ped.12209. [DOI] [PubMed] [Google Scholar]
- 12.Gist KM, Erickson BA, Schuchardt EL, Morose M, Kaufman J, Da Cruz E, Mitchell MB, et al. Tachyarrhythmia following Norwood Operation: A Single Center Experience. Cardiology in the Young–46th Annual Meeting of the Association for European Paediatric and Congenital Cardiology, AEPC with joint sessions with the Japanese Society of Pediatric Cardiology and Cardiac Surgery, Istanbul, May 23-26. 2012, Cambridge University Press, May. 2012;22(1):4. [Google Scholar]
- 13.Buljević B. Uzroci i intrauterino liječenje fetalnih aritmija. U: MalčićI, Škrablin-KučićS. i sur. Fetalna i neonatalna kardiologija. Zagreb: Medicinska naklada; 2011. pp. 182–200. [Google Scholar]
- 14.Baumgartner H. i sur. ESC Guidelines for the management of grown-up congenital heart disease (new version. 2010): The Task Force on the Management of Grown-up Congenital Heart Disease of the European Society of Cardiology (ESC) Eur Heart J. 2010;31(23):2915–57. doi: 10.1093/eurheartj/ehq249. [DOI] [PubMed] [Google Scholar]
- 15.Košutić J, Stajević M, Šehić I, Ugrinović B, Vukomanović V, Rakić S. i sur. Indikacije i optimalan uzrast za hiruršku korekciju izolovanog otvora međukomorske pregrade. U: ZdravkovićD. Problemi u pedijatriji 2010. Beograd: Zavod za udžbenike; 2011. pp. 321–8. [Google Scholar]
- 16.Ofori-Amanfo G, Cheifetz IM. Pediatric postoperative cardiac care. Crit Care Clin. 2013;29(2):185–202. doi: 10.1016/j.ccc.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 17.Bagatin J, Carević V. Novi lijekovi u kardiologiji. Medicus. 2010;19(2):225–9. [Google Scholar]
- 18.Begić Z. Poremećaji srčanog ritma dječije dobi (preporuke-algoritmi dijagnostike i tretmana) Sarajevo: PECS, VIII Ljetna pedijatrijska škola; 2010. pp. 75–99. [Google Scholar]
- 19.Begic Z, Dinarevic SM, Pesto S, Begic E, Dobraca A, Masic I. Evaluation of Diagnostic Methods in the Differentiation of Heart Murmurs in Children. Acta Inform Med. 2016;24(2):94–98. doi: 10.5455/aim.2016.24.94-98. doi: 10.5455/aim.2016.24.94-98. [DOI] [PMC free article] [PubMed] [Google Scholar]


