Abstract
Introduction:
Artificial models can be useful at approximate and qualitative research, which should give the preliminary results. Artificial models are usually made of photo-elastic plastic e.g.. juvidur, araldite in the three-dimensional contour shape of the bone. Anatomical preparations consist of the same heterogeneous, structural materials with extremely anisotropic and unequal highly elastic characteristics, which are embedded in a complex organic structure.
The aim of the study:
Examine the budget voltage and deformation of: dynamic compression plate (DCP), locking compression plate (LCP), Mitkovic internal fixator (MIF), Locked intramedullary nailing (LIN) on the compressive and bending forces on juvidur and veal bone models and compared the results of these two methods (juvidur, veal bone).
Material and Methods:
For the experimental study were used geometrically identical, anatomically shaped models of Juvidur and veal bones diameter of 30 mm and a length of 100 mm. Static tests were performed with SHIMADZU AGS-X testing machine, where the force of pressure (compression) increased from 0 N to 500 N, and then conducted relief. Bending forces grew from 0 N to 250 N, after which came into sharp relief.
Results:
On models of juvidur and veal bones studies have confirmed that uniform stability at the site of the fracture MIF with a coefficient ranking KMIF=0,1971, KLIN=0,2704, KDCP=0,2727 i KLCP=0,5821.
Conclusion:
On models of juvidur and veal bones working with Shimadzu AGS-X testing machine is best demonstrated MIF with a coefficient of 0.1971.
Keywords: osteosynthesis material, veal bone, juvidur, SHIMADZU AGS-X
1. INTRODUCTION
Artificial models can be useful at approximate and qualitative research, which should give the preliminary results. Artificial models are usually made of photo-elastic plastic e.g.. juvidur, Araldite in the three-dimensional contour shape of the bone. The good side of this method is greater possibility of repeating the experiment, changes of certain conditions of the experiment, good control and reproducibility of measurements (1). Anatomical preparations consist of the same heterogeneous, structural materials with extremely anisotropic and unequal highly elastic properties, which are embedded in a very complex organic structure. Anatomical preparations are commonly used as models for the testing of deformation, strength and stiffness of some parts of the musculoskeletal system (1).
Immobilization of bone fractures is one of the most complex problems in modern traumatology. Preserved vascularization of peristalsis, surrounding soft tissue and timely reposition and immobilization of broken bones forms the basis of restitution fractures (1). Repositioned bone fragments, to keep and maintain the resulting repositioning should have adequate biomechanical stabilization of bone fragments which ensures callus formation (1).
Today there are many internal and external methods of stabilization of fractures. The implants are made of special bioinert metal that does not lead to complications due to incompatibilities with the tissue. Today it is used so designed implants, its construction minimum damage vascularization of bone and minimally disrupt the integrity of the periosteum (2).
The most common osteosynthesis materials used today, are used for internal fixation of fractures include: dynamic compression plate (DCP), locking compression plate (LCP), Mitković internal fixator (MIF) and locked intramedullary nailing (LIN).
DCP has a specially designed shape Hole Circle, whose tightening approaching fragments to each other, allowing you to achieve axial compression. Hole for screw implantation can enable a screw to 25 ° (2).
LCP plate has screw holes similar DCP plate, but with one side threaded hole for the screw does not allow the application of the same angle. LCP plate lets you set how the standard screw with a spherical head, as well as newly developed safety screw with a head that is notched and is binding in the screw holes in the plate (3). LCP plate allows the combination of standard screw with a spherical head and screw with a head that is notched which prevents loosening between the screw and the plate better than the DCP. Screw trapped in the plate gives stability and no need to top rests on the bone. The free space between the periosteum and the plate allows the free circulation through the periosteum (2, 3).
Mitković internal fixator (MIF) is placed along the bone without no periostal of fragments with minimal damage to soft tissue. There are four mobile terminals that glide along the carrier. The carrier is 1 mm away from the periosteum. Terminals are fixed with screws in multiple planes. In these locations, only internal fixator is in contact with periosteum diaphysis. Proximal and distal carrier are screwed. Distally placed screw allows spontaneous dynamization (4). Such stability is achieved by fragments and peace the focus of the fracture. With the verticalization of patients, the proximal fragment travels to the distal performing compression among the fragments of the focus of the fracture and thus enhancing the process of osteogenesis.
Locked intramedullary nailing (LIN)) should be thick enough to achieve stable osteosynthesis, and screw on the end of the nail secure the same to the cortex, preventing rotational and torsional movements between bone fragments.
In addition to biological factors in the rehabilitation of fracture, biomechanical impact is critical in histogenesis and maturation of the callus. The broken bone is exposed to very complex sets of gravity, inerational and muscle strength. Therefore, the location of the fracture is exposed to constant forces of compression, decompression, bending and torsion. This is the reason that in the area of the fracture crack there are different strains. What is the exact size of the dilatation of healing is not yet clearly defined, but most authors believe that it does not exceed 1 mm (1, 5). Selection of osteosynthesis material for stabilization the fracture is one of the important conditions for bone repair (5, 6).
2. THE AIM OF THE STUDY
Compare the biomechanical stability of osteosynthesis materials (LIN, DCP, LCP and MIF) to compressive forces and bending on models of juvidur and veal bones. Through research come to the knowledge of which tested osteosynthesis material has better biomechanical characteristics to stabilize the fracture, which is crucial for bone repair.
3. MATERIAL AND METHODS
For the experimental study were used geometrically identical, anatomically shaped models of Juvidur diameter of 30 mm, length 100 mm. “Bone” is represented by two juvidurs with a gap of 10 mm between them, which are stabilized with tested osteosynthesis material. Through the juvidar bar using 10mm drill “medullary cavity” was established. Models have been produced in the same controlled conditions. Such models of juvidur allow identical biochemical conditions for all tests of the tested osteosynthesis materials (Figure 1).
Figure 1.

Testing on a Shimadzu Ags-X testing machine of DCP models of juvidur to lateral forces
This experimental study was using the veal bone length of 100 mm and a diameter of 30 mm with the medullary cavity of 16mm. Under the same conditions the osteosynthesis material was set on bones (DCP, LCP, MIF and LIN), with 10 mm distance between the two veal bones length of 100 mm (Figure 2). The same producer was for DCP, and LCP, LIN, while the MIF was produced by another manufacturer.
Figure 2.

Mitković internal fixator testing of veal bone at Shimadzu Ags-X testing machine
We set up on models of juvidur and veal bones trialed osteosynthesis material; DCP without locking and LCP locking plate with 10 holes. The plates are juvidur or veal bone fastened with three screws on each side “of the fracture crack”, making a total of six screws on the board. LIN length of 200 mm is set in the “medullary cavity” model of juvidur, as well as the medullary cavity of veal bones with one screw placed distally and proximally. The same technique was appointed to MIF on juvidur and veal bone models (Figure 2). In order to more accurately position and strengthen the model on the testing machine, were created for this occasion, special grips for proximal and distal part of the model juvidur and veal bones. Static tests were performed by SHIMADZU AGS-X testing machine, where the force of pressure (compression) increased from 0 N to 500 N, and then conducted relief. Bending forces grew from 0 N to 250 N, after which came into sharp relief. For software that is an integral part of the testing machine SHIMADZU AGS-X data are written and recorded the change in deflection diagram in seconds depending on the increase in the force. By dividing the maximum force with the total time we get an increase in force per unit of time.
Ranking DCP, the LCP, LIM, MIF was done specifically for testing in juvidur and veal bones. The ranking was done by determining the minimum coefficient ranking, prepared on the basis of the arithmetic mean (mean) dilatation (stroke) in millimeters. The ranking was determined for two cases. First, equal weights of the arithmetic mean (mean) dilatation for each type of load. Second, different weights arithmetic means including: weight coefficient for the pressure Kp = 0.5; weighting coefficient for bending in one plane K1 = 0.25; weighting coefficient for bending in the second plane K2 = 0.25.
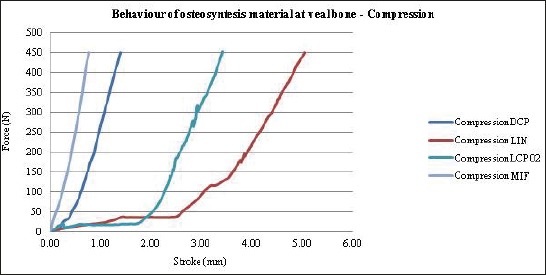
The coefficient ranking for each of the test method (juvidur; veal tibia) was determined according to the algorithm:
where:
Ki – coefficient ranking each osteosynthesis materials;
i – LIN; DCP; LCP; MIF osteosynthesis material designation;
– Arithmetic average of dilatation (mm) for the pressure force;
Kp – Coefficient of pressure force;
– The arithmetic mean of dilatation (mm) for the force bending in one plane;
K1 – coefficient of bending forces on one plane;
– The arithmetic mean of dilatation (mm) for the force bending in the second plane;
K2 – coefficient of bending forces in the second plane;
Models of juvidur and veal bones were exposed under the same conditions the forces of compression and lateral bending.
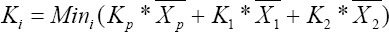
Graph 1.
The distribution of the force (N) in relation to the dilatation (mm) – juvidur on compression force
Results of the study was mechanical stability of tested osteosynthesis material, models of juvidur when the weights of forces: pressure Kp=0,5; Bending in one plane K1=0,25; Bending the second plane K2=0,25, show that in the first rank of MIF with a coefficient ranking KMIF=0,1971, followed with a LIN with KLIN=0,2704, DCP with KDCP=0,2727 and LCP with KLCP=0,5821 (Table 1).
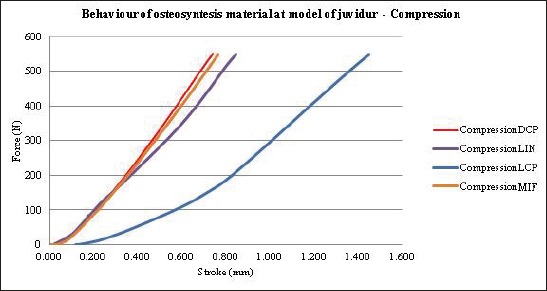
Table 1.
Rank of investigated osteosyntesis materials on juvidur model
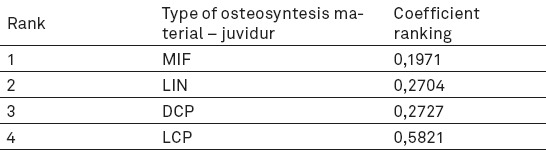
Graph 2.
The distribution of the force (N) in relation to the dilatation (mm) – veal bone on compression force
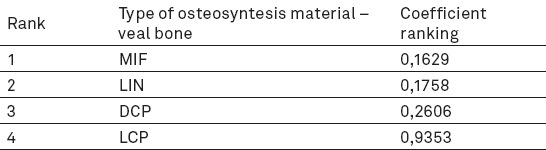
Results of research on veal bones with weight coefficient forces: Pressure Kp=0,5; Bending in one plane K1=0,25; Bending the second plane K2=0,25, MIF had the weight coefficient KMIF-TT=0,1629, then follows LIN with KLIN-TT=0,1758, DCP with KDCP-TT=0,2606 and KLCP-TT=0,9353 (Table 2).
Table 2.
Rank of investigated osteosyntesis materials on veal bone
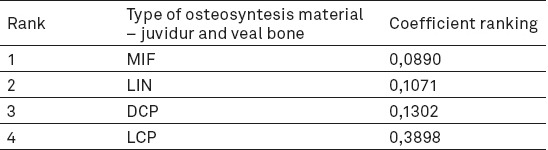
The overall result of the biomechanical stability study of the osteosynthesis material on models of juvidur and veal bones, taking into account that the weight coefficients of the test methods (juvidur = 0.4; cadaver = 0.6), and weight coefficients of forces: Pressure Kp=0,5; Bending in one plane K1=0,25; Bending the second plane K2=0,25, shows that MIF is first in ranking with minimum coefficient rank KU-MIF=0,0890, then follows KU-MIF=0,0890, and LIN with KU-LIN=0,1071, DCP with KU-DCP=0,1302 and LCP with KU-LCP=0,3898 (Table 3).
Table 3.
The overall result of the osteosynthesis material on models of juvidur and veal bones
4. DISCUSSION
Absolute stability leads to a small stress when connecting between fragments of bone cells, which creates favorable conditions for primary bone healing. Relative stability results in the creation of suitable conditions for secondary bone healing, while a high level of stress leads to elongation of the bone gap above the level of resistance of the tissue, which leads to rupture of the cellular integrity and the inability of fracture healing (4, 5, 6). It used to be internal fixation with a plate which achieved absolute stability of the broken bone fragments which did not allow micro-movements between fragments. Such stabilization of the fracture knew to result with loosening the implant and result in postponement healing or not healing of bones (7).
One of the problems of a dynamic-compression plate, a loss of stability between the plate and the screw at the site of the fracture (8). Contact compound head screws and plates realized cross-linking of the screw head and the lip of the plate. The strength of this compound depends on the size of the tightening force screws and friction factor of metal on metal (8).
Maximum load which cortical bone of the femur adults before the occurrence of fractures endure, according to Reilly, with the effect of compression force is 205 ± 17,3 Mpa or shearing forces 71 ± 2,6 Mpa. The maximum force that the femur can withstand that does not lead to fracture of the same is forces of tension with 53 ± 10,7 Mpa or compression forces 131 ± 20,7 Mpa (9).
Energy spreads like a wave through the bone and the speed of the wave burdens bones about 3000 m/s. It takes 15 J of energy for fracture of the tibia diaphysis or femur fractures in adults.
The energy released when a person weighing 70 kg in the fall to the ground from a standing position is about 500 J. The ability to absorb energy have eccentric muscle contraction and deformation of soft tissue that prevent bone fractures in the insignificant, small declines in younger, because the absorbed energy. That same energy muscles, ligaments are unable to resorb in older people (10). Today osteosynthesis construction material is not intended to provide absolute peace between bone fragments after the surgical setting. Rigid osteosynthesis carries two potential drawbacks to the place of fracture: bone resorption, and the lack of micro-movements at the site of the fracture prevents the formation of callus (11).
Mitkovich preferred internal fixator that allows a minimally invasive surgical technique, no rough handling, minimal blood loss, and provides excellent biomechanical conditions for healing (12). Surgical treatment of locked intramedullary nailing is the surest and quickest way to bone repair, if timely provide favorable biomechanical conditions on the level of the fracture (13).
“Biological” novelties AO groups in Davos is the LCP panel, made according to the principles of limited contact with the surface of the cortex (14). For newly designed plate is typical double hole shape and the ability to use two types of screws. Classical screws and openings are achieving dynamic compression osteosynthesis. Next to the classic, are set and sliced open. The extraction of new screws in them, the plate becomes internal fixator, and the fragments are fixed according to the principle of elastic stable osteosynthesis. LCP-plate fixator, can be applied to the location of the fracture classical or with minimal invasive osteosynthesis (14). Top new screws of LCP plate in fact is a drill that bores time in the cortex. The neck screw makes part which is cut into the tray in the cortex. The head screw is conical with coils that are used for screwing in notches opening in the plate, as is equal to the diameter of the screw head and the thread holes in the board. So screw the board realizes rigid contact, and the plate is not pressing the bone surface. It can be deposited in the subcutaneous layer and to maintain the role of elastic stable osteosynthesis without compromising periosteum and circulation bones (15).
The authors recommend individual (dynamic compression or elastic stable osteosynthesis), and the combined application of these new boards. To accomplish dynamic compression board role, it is sufficient tightening a one screw through the location of fractures, and one classic screw on each side of the fracture. For fixation of other parts of the panels can be used screwed the new generation. In the osteotomy and more fracture fragments of diaphyses and metaphysis fractures of the long bones, the board is used as a fixator. Then its surface does not necessarily have to be in contact with the periosteum. In this way the elastic stable osteosynthesis is accomplished with internal fixator. Micro-movements fragments are desirable and as consequently healing with stimulus periosteum callus (15).
OnurBaşcı had at twenty one left femur from cadaver examined the biomechanical stability of the femur diaphyses fractures by AO classification type A1, A2, A3 with IML and LCP plate. Twenty-left cadaver femur divided into three groups: A, B, C. In each group there were seven left cadaver femur. Group A has been stabilized with an LCP and was relatively resistant to torsional load test (p = 0.949) compared to the group B stabilized IML, that is relatively more resistant to the axial compression rate (p = 0.225) compared to the group with the stabilized LCP. Group C is significantly more resistant in relation to groups B in the axial (p = 0.003), a torsional (p = 0.008). Thanks to its high biomechanical stability that allows early mobility LCP and IML in combination could be the treatment of choice in complicated A3 osteoporotic fractures of the distal femur in young people and adults (16).
On the tibia sheep of Bunyamin A and associates examined the biomechanical stability properties of longitudinal and oblique fractures. Fractures stabilized with straight and spiral DCP. Statistically there is a significant difference, which confirms that straight DCP plane provides better stabilization. Spiral plate during the effect of torsion forces has greater strength and resilience of the DCP plate. Recent biomechanical analysis may encourage, in the near future, the use of spiral DCP to stabilize the fracture (17).
Experimental research on the model of the femur on the impact loads and moving bone fragments stabilized wrinkled and not wrinkled Kuncher. Group A has been stabilized with not wrinkled Kuncher, while in group B and C is set with wrinkled Kuncher in which the free space below the trochanter major between the wedge and the cortex was 100 mm. Based on the tests, there was a realization that the maximum value of displacement in the frontal plane of the distal femur 1,86 mm while minimum is in the sagittal plane of the proximal femur 0,08 mm. Achieved values in any level, does not exceed the acceptable movement up to 3 mm in order to prevent bone consolidation (18).
The fracture healing is conditioned by controlled axial load and micro movements. How much is the axial load, and how much micro-movements are still not clearly defined. How fracture healing, it would be ideal to grow load the bone and reduces the load on the osteosynthesis material. This gradual change of axial load and micro movements can be achieved by using timely dynamics of the LCP, MIF and LIN (18).
5. CONCLUSION
Locked intramedullary nailing and Mitkovich internal fixator provide physiological biochemical conditions that would give an advantage in the treatment of diaphyseal transverse comminuted fracture in relation to the dynamic compression and dynamic compression locked plate.
Footnotes
• Conflict of interest: none declared.
REFERENCES
- 1.Grubor P, Grubor M. Results of Application of Eexternal Fixation with Different Types ofFixators. Srp Arh Celok Lec. 2012 May-Jun;140(5-6):332–8. doi: 10.2298/sarh1206332g. [DOI] [PubMed] [Google Scholar]
- 2.Müller ME, Allgöwer M, Schneider R, Willenegger H. Udžbenik osteosinteze. Vol. 24. Zagreb: Jugoslavenska medicinska naklada; 1981. [Google Scholar]
- 3.Korner J, et al. A biomechanical evaluation of methods of distal humerus fracture fixation using locking compression plates versus conventional reconstruction plates. J Orthop Trauma. 2004;18(5):286–93. doi: 10.1097/00005131-200405000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Mitkovic M, Bumbasirevic M, Golubovic Z, Mladenovic D, Milenkovic S, Micic I. New biological method of internal fixation of the femur. Acta Chir Jugosl. 2005;52(2):113–6. doi: 10.2298/aci0502113m. [DOI] [PubMed] [Google Scholar]
- 5.Wali MG, Baba AN, Latoo IA, Bhat NA, Baba OK, Sharma S. Internal fixation of shaft humerus fractures by dynamic compression plate or interlocking intramedullary nail: a prospective, randomised study. Strategies Trauma Limb Reconstr. 2014 Nov;9(3):133–40. doi: 10.1007/s11751-014-0204-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sabalić S, Kodvanj J, Pavić A. Comparative study of three models of extra-articular distal humerus fracture osteosynthesis using the finite element method on an osteoporotic computational model. Injury Int. 2013;44:S54–S61. doi: 10.1016/S0020-1383(13)70200-6. [DOI] [PubMed] [Google Scholar]
- 7.Bruce CW, Gibson TW, Runciman RJ. A comparison of conventional compression plates and locking compression plates using cantilever bending in an ilial fracture model. Vet Comp Orthop Traumatol. 2014;27(6):430–5. doi: 10.3415/VCOT-14-01-0001. [DOI] [PubMed] [Google Scholar]
- 8.Alexander J, Morris RP, Kaimrajh D, Milne E4, Latta L, Flink A, Lindsey RW. Biomechanical evaluation of periprosthetic refractures following distal femur locking platefixation. Injury. 2015 Dec;46(12):2368–73. doi: 10.1016/j.injury.2015.09.033. [DOI] [PubMed] [Google Scholar]
- 9.Reilly DT, Burstein AH. The elastic and ultimate properties of compact bone tissue. J Biomech. 1975;8:393–405. doi: 10.1016/0021-9290(75)90075-5. [DOI] [PubMed] [Google Scholar]
- 10.Gautier E, Perren SM, Cordey J. Effect of plate position relative to bending direction on the rigidity of a plate osteosynthesis. A theoretical analysis. Injury. 2000;31(Suppl 3):C14–20. doi: 10.1016/s0020-1383(00)80027-3. [DOI] [PubMed] [Google Scholar]
- 11.Perren SM, Botzy J. Cellular diferentiation and bone biomechanics during the consolidation of a fracture. Anat Clin. 1978;1:13–28. [Google Scholar]
- 12.Mitković M. Nova biološka metoda unutrašnje fiksacije femura, Facta universitatis - series: Medicine and Biology. 2001;8(1):50–3. [Google Scholar]
- 13.Grubor P, Grubor M, Asotic M. Comparison of Stability of Different types of External Fixation. Med Arh. 2011;65(3):157–9. doi: 10.5455/medarh.2011.65.157-159. [DOI] [PubMed] [Google Scholar]
- 14.Frigg R. Locking Compression Plate (LCP). An osteosynthesis plate based on the Dynamic Compression Plate and the Point Contact Fixator (PC-Fix) Injury. 2001;32(Suppl2):63–6. doi: 10.1016/s0020-1383(01)00127-9. [DOI] [PubMed] [Google Scholar]
- 15.Aksakal B, Gurger M, Yakupsay, Erhan Yilmaz. Biomechanical comparison of straight DCP and helical plates for fixation of transverse and oblique bone fractures. Acta of Bioengineering and Biomechanics. 2014;16(4) [PubMed] [Google Scholar]
- 16.Başcı O, Karakaşlı A, Kumtepe E, Güran G, Havıtçıoğlu H, Başc ıO, Karakaşl ıA, et al. Combination of anatomical locking plate and retrograde intramedullary nail in distal femoral fractures: comparison of mechanical stability. Eklem Hastalık Cerrahisi. 2015;26(1):21–6. doi: 10.5606/ehc.2015.06. [DOI] [PubMed] [Google Scholar]
- 17.Kajzer A, Kajzer W, Marciniak J. Expandable intramedullary nail - experimental biomechanical evaluation. Archives of Materials Science and Engineering. 2010;41(1):45–52. [Google Scholar]
- 18.Grubor P. Treetment of War Wounds the Extremities. New York, USA: Nova Science Publishers; 2014. pp. 65–9. [Google Scholar]


