Sir,
Surgical excision is the most effective treatment for glomus tumors of nail unit. Sometimes this can be a difficult task because, despite being a well-defined tumor, its visualization can be difficult. The use of intraoperative nail bed and matrix dermoscopy helps in the diagnosis and localization of the tumor from surrounding tissue.
A 35-year-old female presented to us with a history of severe episodic pain in the distal part of left thumb for the last 7 years, exacerbating factors being minor trauma and exposure to cold. She received courses of topical steroids and analgesics with temporary relief. No apparent swelling or deformity of the nail was present on visual examination. Point tenderness was elicited on applying pressure with a blunt object over the proximal nail fold of the affected thumb. X-ray of the hand was normal and magnetic resonance imaging (MRI) showed a tumor of size 9.5 × 6.2 mm at the subungual aspect of distal phalanx which was isointense on T1 and hyperintense on T2 weighted images [Figure 1]. No bony deformity was present. In view of typical clinical presentation and imaging, provisional diagnosis of glomus tumor was made. Surgical excision of the tumor by transungual approach was planned under local anesthesia after taking informed consent. One millilitre of 2% lignocaine hydrochloride injection without adrenaline was injected at the base of the thumb bilaterally followed by application of tourniquet. Careful avulsion of nail plate was done with the help of nail spatula. An ill-defined bluish swelling was visible over the proximal nail bed extending under the proximal and lateral nail folds. On naked eye examination, delineation of the tumor margin from the surrounding tissue was difficult. After retraction of nail folds, polarized light, non-contact dermoscopy (Dermlite DL3 with attached IPhone 6S) of nail bed and matrix was done. On dermoscopy, ramified telangiectasias over blue background were present at the site of the tumor [Figure 2]. Excision of mass was done considering that tumor margin corresponded to an abrupt loss of ramified telengiectesias. After careful excision of the tumor mass, closure was done with help of absorbable 4.0 vicryl sutures and hemostatic dressing [Figure 3]. Postoperative antibiotics and analgesics were given. No recurrence of pain occurred after healing in follow-up visits (indirect evidence of complete surgical excision). Histopathology of the excised mass showed collection of monomorphic cells with eosinophilic cytoplasm (glomus cells) around dilated vascular channels consistent with the diagnosis of glomus tumor.
Figure 1.

Magnetic resonance imaging showing a tumor at the subungual aspect of distal phalanx which is hyperintense on T2 weighted images
Figure 2.
On dermoscopy, ramified telangiectasias over blue background were present at the site of the tumor; notice abrupt loss of telengiectesias at periphery of mass
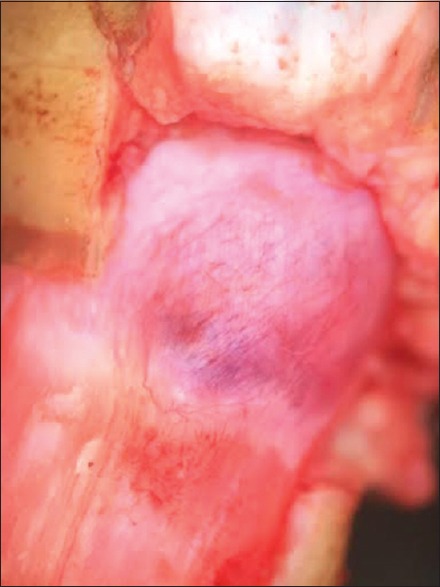
Figure 3.

Excised tumor mass
Diagnosis of nail unit glomus tumor can be established by clinical and imaging techniques.[1] Clinical methods include elicitation of local tenderness with help of pinhead (Love sign) or exposure to cold water. Clinical examination is not sufficient in many cases for localization of tumor because of small size and lack of visible deformity.[2,3] Imaging provides accurate location and size of tumor. Ultrasound usually shows a hypoechoic mass but it is an operator dependent procedure. MRI is the most sensitive imaging method but high cost and low specificity (difficult to differentiate from mucous cyst, epithelial inclusion cyst, etc.) are the limiting factors.[4]
Complete surgical excision is a definitive treatment because incomplete excision of tumor results in relapse of pain within few days of surgery. Intraoperative localization of tumor is a difficult task in many cases. Intraoperative dermoscopy of nail bed and matrix is an easy, rapid, and noninvasive method for proper localization of tumor. It shows presence of ramified telengiectesias over blue background at the site of tumor. Tumor margin can be considered corresponding to abrupt loss of telengiectesias at the periphery of mass. Proper pressure of tourniquet is important to create a bloodless field for successful intraoperative dermoscopy. We suggest that intraoperative dermoscopy should be performed in every case of nail bed and matrix glomus tumor. It will help in complete excision of tumor as well as decrease the damage to the surrounding nail matrix.[5,6,7]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.McDermott EM, Weiss AP. Glomus tumors. Hand Surg. 2006;31:1397–400. doi: 10.1016/j.jhsa.2006.05.018. [DOI] [PubMed] [Google Scholar]
- 2.Takemura N, Fujii N, Tanaka T. Subungual glomus tumor diagnosis based on imaging. J Dermatol. 2006;33:389–93. doi: 10.1111/j.1346-8138.2006.00092.x. [DOI] [PubMed] [Google Scholar]
- 3.Chen SH, Chen YL, Cheng MH, Yeow KM, Chen HC, Wei FC. The use of ultrasonography in preoperative localization of digital glomus tumors. Plast Reconstr Surg. 2003;112:115–9. doi: 10.1097/01.PRS.0000066163.81401.05. [DOI] [PubMed] [Google Scholar]
- 4.Drapé JL, Idy-Peretti I, Goettmann S, Guérin-Surville H, Bittoun J. Standard and high resolution magnetic resonance imaging of glomus tumors of toes and fingertips. J Am Acad Dermatol. 1996;35:550–5. doi: 10.1016/s0190-9622(96)90678-7. [DOI] [PubMed] [Google Scholar]
- 5.Hirata SH, Yamada S, Almeida FA, Enokihara MY, Rosa IP, Enokihara MM, et al. Dermoscopic examination of the nail bed and matrix. Int J Dermatol. 2006;45:28–30. doi: 10.1111/j.1365-4632.2004.02335.x. [DOI] [PubMed] [Google Scholar]
- 6.Hirata SH, Yamada S, Almeida FA, Tomomori-Yamashita J, Enokihara MY, Paschoal FM, et al. Dermoscopy of the nail bed and matrix to assess melanonychia striata. J Am Acad Dermatol. 2005;53:884–6. doi: 10.1016/j.jaad.2005.07.032. [DOI] [PubMed] [Google Scholar]
- 7.Maehara Lde S, Ohe EM, Enokihara MY, Michalany NS, Yamada S, Hirata SH. Diagnosis of glomus tumor by nail bed and matrix dermoscopy. An Bras Dermatol. 2010;85:236–8. doi: 10.1590/s0365-05962010000200018. [DOI] [PubMed] [Google Scholar]


