Abstract
Excess weight gain tends to occur in young adulthood. However, research examining effective weight-related interventions for this age group has been limited. As one of seven trials in the EARLY Trials consortium (Early Adult Reduction of weight through LifestYle intervention), the CHOICES Study (Choosing Healthy Options in College Environments and Settings) tested effects of a technology-integrated, young adult weight gain prevention intervention. It was a randomized controlled trial with assessments at baseline (2011) and 4-, 12- and 24-months post-intervention initiation and included 441 participants (ages 18-35) who were students at three Minnesota community colleges. The 24-month intervention included a 1-credit academic course and social networking and support online intervention. This analysis examined effects on 12 secondary behavioral outcomes across three domains: diet (fast food, sugary beverages, breakfast, at-home meal preparation), physical activity/screen time (minutes and energy expenditure in leisure time physical activity, television viewing, leisure time computer use) and sleep (hours of sleep, time required to fall asleep, days not getting enough rest, difficulty staying awake). The intervention resulted in significant reductions in fast food (p=0.007) but increases in difficulty staying awake (p=0.015). There was limited evidence of other behavior changes at 4 months (0.05<p<0.1) in the expected direction but differences by treatment condition dissipated over time. Analyses examining summary treatment effects (i.e., modeling effects on all behavioral outcomes simultaneously) indicated significant overall effects (p=0.014), largely driven by 4-month results (p=0.005). Additional research is needed to understand effective obesity prevention among young adults, particularly when addressing multiple weight-related outcomes.
Introduction
Obesity is a public health concern,1, 2 and young adults (e.g., ages 18–35) are especially at risk for unhealthy weight gain.3, 4 The young adult years represent a critical transition period when many young people move out of their family's home, relocate, and establish independent lifestyles. These transition years may also involve other landmark life events, like entering post-secondary education, beginning new jobs, shifting social networks, and childbearing. Despite the importance of this age, research examining effective weight gain prevention strategies for young adults has been limited.3, 4
There is a particular need for research in at-risk young adult populations, including those in understudied and non-traditional post-secondary settings, like 2-year community colleges.5, 6 Nearly 8 million young adults in the U.S. attend 2-year community and technical colleges. These institutions serve a large proportion of students from lower-income and/or minority communities.7 Previous research has demonstrated that, compared to their counterparts attending 4-year universities, 2-year college students are at significantly greater risk for adverse weight-related factors, including overweight/obesity, physical inactivity, excessive television viewing, and high intakes of soda and fast food.6 To our knowledge, there have been no randomized controlled weight gain prevention trials conducted on 2-year college campuses; thus this represents an important setting for future research, partnership and outreach.
Several recent reviews 4, 8-10 have identified a limited number of interventions addressing young adult weight gain prevention, with very few specifically addressing at-risk or underserved populations. Many of these studies yielded favorable short-term effects on weight status and/or body composition, but were small-scale pilot studies and lacked data from fully powered randomized trials. Other young adult interventions targeting specific weight-related behaviors, including 19 interventions focusing exclusively on diet-related factors and 7 focusing on physical activity only, have yielded encouraging findings for dietary behaviors, but mixed results for physical activity.4 This literature thus suggests behavioral interventions targeting young adults may yield a more consistent impact on some types of weight-related behaviors versus others. In addition, some behaviors related to weight have been poorly examined in intervention studies. Specifically, numerous studies show inverse associations between short sleep duration and obesity, particularly among young people.11-18 but weight gain prevention studies attempting to intervene on sleep remain relatively rare.
The need for targeting multiple weight-related behaviors within an intervention is also important because weight behaviors cluster together,19, 20 and interventions targeting multiple behaviors may have a greater public health impact than those focusing on singular behavioral targets, particularly given that behavior change, even in the absence of weight change, may have beneficial health effects.21, 22 However, to date, few young adults obesity prevention studies have used a multiple behavior approach. One study conducted on 13 large university campuses used online mini-educational lessons to promote a non-diet approach to healthy weight maintenance; the 10-week intervention focused on eating, physical activity and stress and also included sleep content.23 Overall, the intervention did not have an impact on BMI or weight status, but did yield small, immediate post-intervention improvements in diet, activity and sleep. Another 12-week study of 155 university students evaluated a multiple component intervention requiring participants to complete a contract identifying at least one behavior to improve in the next week (e.g., physical activity, alcohol misuse, sleep) in addition to behavioral self-monitoring; intervention results indicated favorable changes across several health behaviors.24 More research using multiple behavior intervention approaches is needed, particularly to understand the possible impact of interventions that are sustained for longer durations. Furthermore, interventions utilizing innovative technologies, such as social networking technologies, may be particularly relevant to young adults; to date, early work on such technologies has shown mixed effects on various behavioral outcomes but may have a high degree of relevance to this age group, particularly as the field advances.25, 26
To address these gaps in the literature, the Choosing Healthy Options in College Environments and Settings (CHOICES) Study was designed to test an intervention to reduce unhealthy weight gain among 2-year college students;27 body mass index (BMI) was the primary outcome of the CHOICES study. This study was one of seven randomized, controlled trials funded as part of the EARLY Trials consortium (Early Adult Reduction of weight through LifestYle intervention, earlytrials.org). The purpose of this paper is to describe the impact of the CHOICES intervention on weight-related behaviors intervened upon and assessed as secondary outcomes including dietary, physical activity/screen time and sleep behaviors.
Methods
The CHOICES Study
The CHOICES Study had a randomized, controlled, parallel-group design with a 1:1 randomization ratio. The study tested a 24-month active intervention to prevent excess weight gain in participants 18-35 years of age, including 441 participants from three community colleges in the Twin Cities area of Minnesota (2011-2014).27 Eligibility requirements were: being 18-35 years old; BMI=20-34.9kg/m2; and planning to be in the geographic area for ≥2 years. Original study eligibility requirements were BMI=20-29.9kg/m2; due to challenging participant enrollment in this population and initial interest from students with BMI ≥30kg/m2, investigators expanded the BMI inclusion criteria to 20-34.9kg/m2 after enrollment began. This change brought CHOICES into alignment with inclusion criteria for other EARLY trials. Individuals with BMI≥35kg/m2 were ineligible because (a) CHOICES was a weight gain prevention trial and (b) individuals with BMI≥35kg/m2 have different intervention needs for weight loss.28, 29
Additional EARLY trial criteria excluded participants with significant health problems that are described elsewhere.27, 30 Study protocols were approved by the University of Minnesota Institutional Review Board.
Intervention and control conditions
The CHOICES intervention consisted of two overlapping components: an academic course and a social network and support website. The intervention focused on several content areas, including diet/nutrition, physical activity, screen time, and sleep. These areas and the intervention-targeted behaviors were identified from previous evidence of leading contributors to weight gain and formative research with 2-year college students.6, 31, 32 Intervention development was informed by ecological theories of health behavior, social cognitive theory, and social network theory, suggesting weight-related behaviors are influenced by various personal and socio-environmental factors.27 More detail on the CHOICES intervention is available elsewhere.27
Students randomized to the intervention condition participated in a one-credit course offered through the college in which they were enrolled. The course was developed and delivered by CHOICES research staff and focused on eating, activity, sleep habits, and stress management as mechanisms for maintaining and/or achieving a healthy weight. Participants chose between three course sections (online, face-to-face, or hybrid) to meet scheduling needs and learning preferences.
In addition to the course, students randomized to the intervention participated in a social networking and support website, introduced as part of the course and continued as the primary intervention channel for 20 months. The website was password-protected and open only to intervention participants and a limited number of their invited guests. It was designed to reinforce, inform and encourage exchange and support between participants. Students were encouraged to track their weight and up to 10 weight-related behaviors (i.e., sugary beverages, fast food, fruits/vegetables or breakfast consumption; eating mindfully; TV/movie viewing; computer and internet use, physical activity, sleep duration or stress management) on the website. Trained interventionists primarily interacted with participants through the website, but occasionally used texting and telephone calls to offer encouragement and help problem solve. The website included articles, recipes, quizzes, videos and ways to accumulate points for prizes.
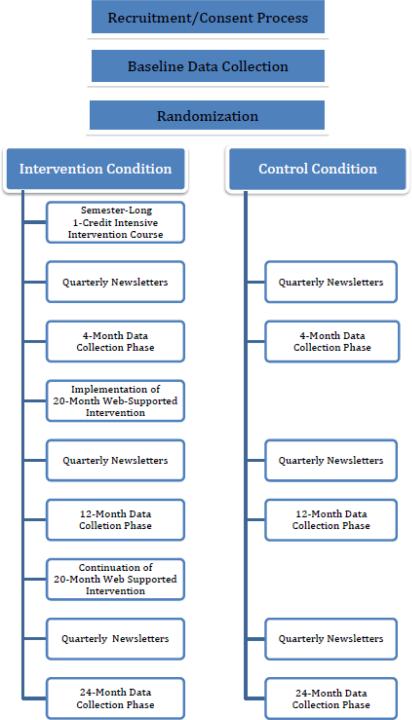
Students randomized to the control condition received health assessments per the study measurement schedule as well as basic health promotion information on a quarterly basis. Students in the control condition were not allowed to enroll in the course and were not granted access to the website. Figure 1 summarizes the study design and activities included in intervention and control conditions.
Figure 1.
Study Design, Measurement Periods and Intervention Elements: The CHOICES Study
Blocked randomization was determined using computer-generated randomization. Following baseline measures, the team blocked students on college, weight status and gender, and randomly assigned participants within block into the intervention or control condition. The randomization sequence was generated by the study programmer. Participants were enrolled and notified of randomization assignment by the study coordinator.
Evaluation
Outcome evaluation measures were collected at baseline and 4-, 12- and 24-months post intervention initiation. These included measures of demographic characteristics (e.g., gender, race/ethnicity, education, participant income, relationship status), weight-related behaviors (e.g., diet, physical activity, media use), and other related factors. Self-reported income did not include income from other family members, but rather only income from the individual participant. Participants received $100 in gift cards for participating in each outcome assessment.
In this analysis we focused on secondary intervention outcomes in three behavioral domains: dietary factors, physical activity/screen time and sleep. Behavioral outcomes were self-reported by participants at the four measurement time points, and were assessed via survey items included as common elements across all seven EARLY Trials. Objectively assessed height and weight were documented by trained data collectors; these details and results of the primary outcome evaluation are reported elsewhere.33 (Lytle et al, under review)
Outcome measures
Eating behaviors targeted by the intervention and assessed included: fast food purchasing, sugary beverage and breakfast consumption and frequency of home meal preparation.33 To assess fast food, participants were asked: “Over the past 30 days, how many times did you buy food at a fast food restaurant, such as McDonald's, Burger King, Arby's, Wendy's, Hardee's, Taco Bell, Taco Johns, Chipotle, KFC, Pizza Hut, Panera, Quiznos, Noodles & Company, Bruegger's Bagels?”34 Four questions selected from the National Cancer Institute's Diet History Questionnaire (DHQ)35 asked about past 30-day consumption of soda/pop, fruit drinks, sports drinks and energy drinks. As in the DHQ, two additional questions were included to quantify how often soda/pop and/or fruit drink consumption was diet/sugar-free. Finally, breakfast was assessed by asking “in a typical week, how many times do you eat breakfast?,” and home food preparation was assessed via a summary score of responses to three items: “over the past week, how many times did you eat the following meals that were prepared in your home or the place where you live” (breakfast, lunch, dinner; days/week).
Physical activity/screen time behaviors included: energy expenditure for leisure time physical activity (LTPA), total LTPA in minutes, television viewing and leisure time computer use. The Paffenbarger Questionnaire36 was used to estimate calories expended in leisure activity based on number of stairs climbed and blocks walked, amount of time spent doing light (5 kcal/min), medium (7.5 kcal/min), and high (10 kcal/min) intensity activity, and weekly minutes of LTPA (excluding flights of stairs). Television and leisure time computer use were assessed using weekday and weekend specific items from the CARDIA Study (http://www.cardia.dopm.uab.edu). Daily hours were reported in response to the questions: “on a typical [weekday/weekend day] how much time do you spend sitting while watching TV (including videos on VCR/DVDs)” and “sitting while using the computer for non-work/non-school activities or playing video games.”
Finally, four outcomes were used to assess sleep. Daily hours of sleep were calculated based on two items, “What time do you usually go to bed in the evening (turn out the lights in order to go to sleep)?” and “What time do you usually get out of bed in the morning?”.37 Participants were also asked, “on average, how often has it taken you more than 30 minutes to fall asleep after lights out?,” “during the past 30 days, for about how many days have you felt you did not get enough rest or sleep?,” and “in the past week, how many days have you had trouble staying awake while driving, eating meals, in class or engaging in social activity?.” These items were adapted from the Pittsburgh Sleep Quality Index.38
Sample size determination
Sample size was calculated based on power to detect changes in the primary outcome, change in BMI. A sample size of 441 participants provided power to detect <3% change in BMI between treatment conditions using a 2-sided test at 5% Type I error rate with greater than 80% power, an ICC of 0.005, and dropout rate of 20%.
Statistical Analysis
Summary statistics were calculated for overall descriptive and demographic characteristics of the sample, comparing characteristics of the intervention and control condition, as well as the characteristics of those completing 24-month assessments versus those who did not. Behavioral outcomes distributions were examined and transformed, when necessary. This involved log-transformation of several outcomes, and square-root transformation when zeros were present in the data. In some cases, it was not possible to approximate a Gaussian distribution through transformations; thus, three variables (eating breakfast, trouble staying awake, and trouble falling asleep) were dichotomized, and logistic regression was used.
Second, repeated measures analysis was used to examine possible different trajectories over four time periods by condition (3 degrees of freedom (Df) test). Models were adjusted for age, sex, racial category, parental education level, data collection wave, and intervention course section with school as a random effect. Also included were tests (1 Df, each) for differences at each time point, and tests for net differences from baseline per ensuing time period.
Finally, to give a comprehensive view of the intervention, as well as to reflect the flexible structure of allowing participants to select any targeted behavior(s) on which to focus during the intervention (which they could also change throughout the intervention), additional analyses were conducted. To examine summary treatment effects both within and across the three domains (diet, physical activity/screen time, and sleep), the four target behavioral outcomes in each domain were analyzed as repeated outcomes on the same underlying complex, as well as by all twelve outcomes per student marking a global complex of healthy life-style behaviors. In these hierarchical mixed models,39 the input variables were standardized and modeled as repeated measures using compound symmetry as the covariance matrix.
Results
The average age of participants was 22.8 years. A majority of the sample was female (67.6%), white (72.6%), with an income <$12,000 (66.2%). Approximately 16% of the sample was Black/African American and 7.6% were Hispanic. The only marginally significant sociodemographic or behavioral difference between the intervention and control conditions was for percent of participants identifying as white (intervention: 76.3%, control: 68.7%, p=0.07). (Table 1)
Table 1.
Sample characteristics at baseline: The CHOICES Study.
| Total (n=441) | Intervention (224) | Control (n=217) | P-value1 | |
|---|---|---|---|---|
| Gender, Female (%) | 67.6 | 67.0 | 68.2 | 0.78 |
| Race/ethnicity | ||||
| White (%) | 72.6 | 76.3 | 68.7 | 0.07 |
| Hispanic or Latino origin (%) | 7.5 | 7.6 | 7.4 | 0.93 |
| Current relationship status | ||||
| Single or casually dating (%) | 54.6 | 53.8 | 53.3 | 0.75 |
| Age at randomization, years | 22.8 | 22.9 | 22.8 | 0.84 |
| Income | ||||
| Less than $12,000 (%) | 66.2 | 67.9 | 64.5 | 0.46 |
| Dietary factors | ||||
| Fast food (times/week) | 1.7 | 1.7 | 1.8 | 0.45 |
| Sugary beverages (times/day) | 0.9 | 0.8 | 1.0 | 0.13 |
| Breakfast 5-7 days/week (%) | 51.5 | 51.8 | 51.2 | 0.89 |
| Weekly meals prepared at home (total) | 13.5 | 13.5 | 13.4 | 0.86 |
| Activity | ||||
| Energy expenditure: Leisure time physical activity (kcals) | 2076.2 | 2169.3 | 1979.2 | 0.51 |
| Leisure time physical activity (weekly minutes) | 270.8 | 295.5 | 245.5 | 0.20 |
| Television (hours/day) | 1.5 | 1.6 | 1.5 | 0.58 |
| Leisure-time computer use (hours/week) | 1.2 | 1.2 | 1.2 | 0.63 |
| Sleep | ||||
| Total daily sleep (hours) | 8.4 | 8.4 | 8.3 | 0.36 |
| Days/month not getting enough rest | 9.1 | 9.4 | 8.8 | 0.37 |
| Difficulty staying awake >2 days/week (%) | 7.7 | 6.2 | 9.2 | 0.24 |
| ≥30 minutes to fall asleep 3-7 nights/week (%) | 28.8 | 32.1 | 25.4 | 0.11 |
There were no sociodemographic differences between those retained in the study and those who were lost to follow-up, ineligible and/or dropped out, with the exception of race; more non-white than white participants were lost by the 24-month follow-up (p=0.03) (data not shown). In addition, there was no differential retention by eating, activity and/or sleep-related outcomes, except for sugary beverage consumption; those who were lost by the 24-month follow-up reported higher baseline sugary beverage consumption versus those retained (p=0.001) (data not shown).
During the course of the trial, 23 serious adverse events were reported by participants across both conditions. Only one was determined to be possibly, though not probably, related to study participation. All adverse events were reviewed by the study's Data Safety Monitoring Board.
Behavior change over time by treatment group is presented in Table 2. At 24-months, results suggest that the intervention resulted in decreases in fast food consumption (p=0.007) but increases in difficulty staying awake during more than 2 days in the past week (p=0.015), compared to the control condition. In addition, differences in days in the past month not getting enough rest was marginally significant between treatment groups at 24-months (p=0.061). For the 4-month follow-up assessment period only, several behaviors also yielded intervention effects of borderline significance (0.05<p<0.10) in the expected direction including: fast food, breakfast, meals prepared at home; only one yielded statistically significance differences at the p<0.05 level (days in the past month not getting enough rest). Few differences were observed at 12- and 24-month follow-up time points.
Table 2.
Treatment effects on secondary weight-related outcome variables: The CHOICES Study.
| Domain | Outcome | Analysis using available data | Overall Effect | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 4 months | 12 months | 24 months | P(df=3) | ||||||
| N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | |||
| Dietary factors | Fast food (times/week) | |||||||||
| Intervention (I) | 212 | 1.6 (0.2) | 194 | 1.3 (0.1) | 188 | 1.5 (0.2) | 179 | 1.3 (0.1) | 0.007 | |
| Control (C) | 209 | 1.9 (0.2) | 194 | 1.9 (0.1) | 184 | 1.4 (0.2) | 174 | 1.4 (0.1) | ||
| I-C difference | −0.3 | −0.6 | 0.1 | −0.1 | ||||||
| p-net | — | 0.059 | 0.157 | 0.504 | ||||||
| Sugary beverages (times/day) | ||||||||||
| Intervention | 212 | 0.7 (0.1) | 194 | 0.7 (0.1) | 188 | 0.6 (0.1) | 179 | 0.6 (0.1) | 0.608 | |
| Control | 209 | 0.8 (0.1) | 194 | 0.7 (0.1) | 184 | 0.6 (0.1) | 174 | 0.7 (0.1) | ||
| I-C difference | −0.1 | 0.00 | 0.0 | −0.1 | ||||||
| p-net | — | 0.652 | 0.254 | 0.890 | ||||||
| Eat breakfast 5-7 days/week | ||||||||||
| Intervention | 212 | 50.9% (3.8) | 194 | 56.7% (3.9) | 188 | 59.3% (4.0) | 179 | 62.5% (4.2) | 0.299 | |
| Control | 209 | 54.1% (3.9) | 194 | 49.9% (4.0) | 184 | 57.6% (4.1) | 174 | 59.5% (4.2) | ||
| I-C difference | −3.2% | 6.8% | 1.7% | 3.0% | ||||||
| p-net | — | 0.057 | 0.413 | 0.318 | ||||||
| Weekly meals prepared at home (total) | ||||||||||
| Intervention | 211 | 13.3 (0.4) | 194 | 13.2 (0.4) | 188 | 13.2 (0.4) | 179 | 13.9 (0.4) | 0.284 | |
| Control | 209 | 13.7 (0.4) | 193 | 12.7 (0.4) | 184 | 13.3 (0.4) | 174 | 13.6 (0.4) | ||
| I-C difference | −0.4 | −0.5 | −0.1 | 0.3 | ||||||
| p-net | — | 0.070 | 0.591 | 0.257 | ||||||
| Physical activity and screen time | Energy expenditure for leisure time physical activity (weekly kcals) | |||||||||
| Intervention | 212 | 2289.0 (216.2) | 194 | 2128.7 (178.3) | 188 | 1712.9 (171.9) | 179 | 1700.3 (166.8) | 0.343 | |
| Control | 208 | 1989.8 (218.2) | 194 | 1750.6 (178.4) | 184 | 1659.8 (173.3) | 173 | 1766.8 (167.5) | ||
| I-C difference | 299.2 | 378.1 | 53.1 | −66.5 | ||||||
| p-net | — | 0.083 | 0.277 | 0.726 | ||||||
| Leisure time physical activity (minutes) | ||||||||||
| Intervention | 212 | 310.0 (29.3) | 194 | 282.2 (24.5) | 188 | 234.9 (21.8) | 178 | 212.5 (21.9) | 0.538 | |
| Control | 209 | 245.4 (29.5) | 192 | 208.5 (24.6) | 183 | 202.5 (22.1) | 174 | 220.7 (21.9) | ||
| I-C difference | 64.6 | 73.7 | 32.4 | −8.2 | ||||||
| p-net | — | 0.165 | 0.733 | 0.622 | ||||||
| Television (hours/day) | ||||||||||
| Intervention | 212 | 1.5 (0.1) | 194 | 1.4 (0.1) | 188 | 1.4 (0.1) | 179 | 1.3 (0.1) | 0.570 | |
| Control | 209 | 1.5 (0.1) | 194 | 1.5 (0.1) | 184 | 1.3 (0.1) | 173 | 1.2 (0.1) | ||
| I-C difference | 0.0 | −0.1 | 0.1 | 0.1 | ||||||
| p-net | — | 0.470 | 0.584 | 0.574 | ||||||
| Leisure-time computer use (hours/day) | ||||||||||
| Intervention | 212 | 1.2 (0.1) | 194 | 1.3 (0.1) | 188 | 1.2 (0.1) | 179 | 1.2 (0.1) | 0.605 | |
| Control | 209 | 1.3 (0.1) | 194 | 1.3 (0.1) | 184 | 1.2 (0.1) | 174 | 1.1 (0.1) | ||
| I-C difference | −0.1 | 0.0 | 0.0 | 0.1 | ||||||
| p-net | — | 0.404 | 0.499 | 0.182 | ||||||
| Sleep | Total daily sleep (hours) | |||||||||
| Intervention | 210 | 8.4 (0.1) | 194 | 8.2 (0.1) | 188 | 8.3 (0.1) | 179 | 8.4 (0.1) | 0.126 | |
| Control | 209 | 8.3 (0.1) | 194 | 8.3 (0.1) | 184 | 8.3 (0.1) | 174 | 8.1 (0.1) | ||
| I-C difference | 0.1 | −0.1 | 0.0 | 0.3 | ||||||
| p-net | — | 0.245 | 0.438 | 0.155 | ||||||
| Days in the past month not getting enough rest | ||||||||||
| Intervention | 212 | 7.4 (0.5) | 194 | 6.5 (0.6) | 188 | 6.3 (0.6) | 179 | 5.8 (0.5) | 0.061 | |
| Control | 208 | 7.4 (0.6) | 194 | 8.2 (0.6) | 184 | 6.4 (0.6) | 174 | 6.6 (0.6) | ||
| I-C difference | 0.0 | −1.7 | −0.1 | −0.8 | ||||||
| p-net | — | 0.019 | 0.951 | 0.313 | ||||||
| Difficulty staying awake during more than 2 days in the past week | ||||||||||
| Intervention | 212 | 5.0% (1.5) | 194 | 4.3% (1.3) | 188 | 8.4% (1.9) | 179 | 9.5% (2.1) | 0.015 | |
| Control | 209 | 11.2% (2.5) | 194 | 17.4% (3.1) | 184 | 12.6% (2.8) | 174 | 10.8% (2.6) | ||
| I-C difference | −6.2% | −13.1% | −4.2% | −1.3% | ||||||
| p-net | — | 0.190 | 0.408 | 0.139 | ||||||
| Takes 30+ minutes to fall asleep on 3-7 nights/week | ||||||||||
| Intervention | 212 | 29.2% (3.5) | 194 | 25.8% (3.4) | 188 | 26.1% (3.3) | 179 | 27.7% (3.5) | 0.369 | |
| Control | 209 | 25.8% (3.5) | 194 | 23.6% (3.4) | 184 | 30.1% (3.7) | 174 | 23.8% (3.6) | ||
| I-C difference | 3.4% | 2.2% | −4.0% | 3.9% | ||||||
| p-net | — | 0.837 | 0.171 | 0.911 | ||||||
Models adjusted for sex, racial category, cohort, the maximum education of parents of the respondent (as a measure of socio-economic status), and intervention course section, and included school as a random effect. All estimates (including I-C difference estimates) are subject to a small degree of rounding error.
Further analyses examined summary treatment effects, both within and across diet, physical activity/screen time and sleep domains, and represent the composite effect of the intervention on multiple behavioral outcomes, considered simultaneously in a hierarchical mixed model (Table 3). When simultaneously examining the intervention effect on all four dietary factors (fast food, sugary beverages, breakfast, home meal preparation), the overall effect was associated with a p-value of 0.082, with time-specific effects also estimated for 4-month (p=0.038), 12-months (p=0.752) and 24-months (p=0.406). Summary level treatment effects were not statistically significant within physical activity/screen time or sleep domains. However, the overall intervention effect was significant when examining all 12 behavioral outcomes simultaneously (p=0.014). These overall effects appear to be primarily driven by effects at the 4-month time point (p=0.005).
Table 3.
Summary treatment effects on secondary weight-related outcomes by domain: The CHOICES Study.
| Domain | Analysis using available data | Overall Effect | ||||
|---|---|---|---|---|---|---|
| Baseline | 4 month | 12 month | 24 moth | P(df=3) | ||
| Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | |||
| Dietary factors | Intervention-Control difference | -- | 0.13 (0.6) | −0.02 (0.06) | 0.05 (0.06) | 0.082 |
| p-net | — | 0.038 | 0.752 | 0.406 | ||
| Physical activity and screen time | Intervention-Control difference | -- | 0.10 (0.06) | 0.03 (0.07) | −0.02 (0.07) | 0.263 |
| p-net | — | 0.109 | 0.700 | 0.769 | ||
| Sleep | Intervention-Control difference | -- | 0.09 (0.07) | −0.004 (0.07) | 0.02 (0.07) | 0.483 |
| p-net | — | 0.182 | 0.958 | 0.824 | ||
| TOTAL | Intervention-Control difference | -- | 0.11 (0.04) | 0.002 (0.04) | 0.02 (0.04) | 0.014 |
| p-net | — | 0.005 | 0.966 | 0.681 | ||
NOTE: Models adjusted for sex, racial category, cohort, the maximum education of parents of the respondent (as a measure of socioeconomic status), and intervention course section and included school as a random effect. Dietary results included 4 variables modeled simultaneously: frequency of consuming fast food, sugary beverages, eating breakfast and meals at home. Physical activity and screen time included: energy expenditure and time spent in leisure time physical activity, hours of television viewing and leisure-time computer use. Sleep included: total hours, days in the past month not getting enough rest, difficulty staying awake more than two days in the past month and taking 30+ minutes to fall asleep on 3-7 nights/week. Total effects represent the results of all 12 behavioral variables modeled simultaneously across the three domains (diet, physical activity/screen time and sleep).
Discussion
To our knowledge, this study is the first large-scale, randomized, controlled trial of its kind to evaluate a weight gain prevention intervention among young adults attending two-year community colleges. The intervention appeared to be effective in reducing consumption of fast food and but may not have been entirely beneficial for sleep. These effects were seen at 24 months after adjusting for covariates. In addition, at 4 months, which corresponds to immediately after the required one-credit course, marginal effects (p<0.10), in the expected direction were seen for fast food consumption, eating breakfast, and preparing meals at home, and significant effects (p=0.019) were seen at 4 months for the number of days in the past month that participants reported not getting enough rest. Interestingly, further ad hoc analyses examining intervention effects on multiple behavioral outcomes simultaneously indicated statistically significant differences between intervention and control groups. These effects were significant for the 24-month intervention overall and appeared to be largely driven by differences at the 4-month assessment period.
These results run parallel to those from other weight management trials yielding some short-term effects that are not sustained over time.8 CHOICES included an active 24-month intervention, which is much longer than other interventions reported to date with the young adult age group.4 Process evaluation showed that engagement was high during the first intervention phase (i.e., including the CHOICES course and initial months of website utilization).40 However, consistent with other trials using similar intervention platforms,41-43 engagement declined thereafter. After the first 4 months of the intervention, process results indicate that 30-40% of participants continued to engage in the CHOICES website. Overall, previous research has shown that participant engagement is particularly challenging among the young adult age group.44
The results of the summary treatment effects analysis are notable, given they take into account simultaneous behavior change across multiple domains. Importantly, they also reflect the flexible structure of the CHOICES intervention, which allowed participants to select any targeted behavior(s) on which to focus (and which they could change at any time throughout the 24-month intervention). Formative research contributing to the development and refinement of the intervention indicated that providing flexibility and choice to young adult participants was critical.31 As a result, CHOICES was designed with multiple options for participants regarding modes of intervention delivery, mechanisms for communication, behavioral targets for goal setting and various other factors. Study process evaluation results indicated a high degree of participant satisfaction, likely because of this design feature.40
These issues of flexibility and choice, however, present challenges for traditional statistical models and examination of intervention effects. For example, participants were not consistently focusing on the same behaviors at the same time. Since behavioral targets were self-selected, some individuals only focused on a subset of behaviors throughout the 24-month intervention. The study, however, was not powered to examine differences between small groups of participants that selected common behavioral targets at various times during the intervention. Thus, a more comprehensive approach was needed to simultaneously examine intervention effects on numerous weight-related behavioral outcomes of interest. To our knowledge, this is a relatively novel method for examining intervention effects in a trial that targeted multiple behaviors and has not been widely utilized in the literature to date.
Limitations of this research include insufficient statistical power to detect behavioral changes across participant sub-groups, self-reported assessments of behavioral outcomes (which include a notable degree of bias and error) and limited external validity since this study occurred in one metropolitan area. These results may not be generalizable to community colleges across various regions of the U.S. In addition, our sample is limited in racial/ethnic diversity, and thus results cannot be generalized across all racial/ethnic groups. Future research would benefit from studies powered to examine the effect of multiple behavior change strategies on weight gain prevention (rather that being powered only by a weight-related outcome, such as BMI) and by studying similar intervention approaches in more diverse populations. Finding affordable and acceptable objective measures of weight-related behaviors, especially diet, screen time and sleep, remain a significant challenge for population-based intervention research.
Conclusions
Few weight gain prevention interventions to date have focused on this age group.4 Large-scale, randomized controlled trials addressing the needs of at-risk or underserved young adults and targeting an array of weight-related behaviors are particularly lacking. CHOICES was centered on a multi-dimensional intervention design including both online and in-person delivery components,27 and it was informed by a multifaceted formative research phase that included a range of key stakeholders and students.31 With obesity risk in young adults a national concern and the paucity of work among two-year colleges students, more work in this area is needed.
Supplementary Material
Highlights.
Few randomized controlled obesity prevention trials have targeted young adults.
The CHOICES intervention had limited impact on individual weight-related behaviors.
Effects were significant when examining 12 behavioral outcomes simultaneously.
Effects observed 4 months post intervention initiation were not evident by 1 year.
Obesity research is needed to address multiple behavioral outcomes in young adults.
Acknowledgements
The clinical trial registration number for CHOICES was NCT01134783. The trial was registered on 4/13/10. Approval from the University of Minnesota Institutional Review Board was obtained on 11/16/10.
The authors would like to acknowledge the dedicated study measurement and data management team: William Baker, Pamela Carr-Manthe, Jennifer Nadeau, and Dawn Nelson, as well as the research study assistant, Megan Treziok. The authors also would like to thank the interventionists and other study co-investigators including: Christine Petrich, Sarah Sevcik, Jerri Kohlhaug, Jolynn Gardner and Darin Erickson. Finally, the team would like to thank the students and the staff at Anoka-Ramsey Community College, Inver Hills Community College, and Saint Paul College for their support and help with this project.
Lytle and Laska were primarily responsible for the study concept and design. Laska, Lytle, Hannan Linde and Nanney were responsible for analysis and/or interpretation of the data. Laska drafted the manuscript and it was also critically reviewed and revised for important intellectual content by Lytle, Linde, Moe, Nanney and Hannan. Moe, Lytle and Laska were responsible for study supervision and acquisition of data.
This research was supported through a grant from NHLBI (1 U01 HL096767-01). Additional salary support was also provided by Grant Number K07CA126837 from the National Cancer Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The sponsor did not play a role in study design; collection, analysis, and interpretation of data; writing the report; and the decision to submit the report for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest statement: The authors have no conflicts of interest to declare.
Financial Disclosure: No financial disclosures were reported by the authors of this paper.
References
- 1.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010;303(3):235–41. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007-2008. JAMA. 2010;303(3):242–9. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 3.Nelson M, Story M, Larson N, Neumark-Sztainer D, Lytle L. Emerging adulthood and college-aged youth: An overlooked age for weight-related behavior change. Obesity. 2008;16(10):2205–11. doi: 10.1038/oby.2008.365. [DOI] [PubMed] [Google Scholar]
- 4.Laska MN, Pelletier JE, Larson NI, Story M. Interventions for weight gain prevention during the transition to young adulthood: a review of the literature. J Adolesc Health. 2012;50(4):324–33. doi: 10.1016/j.jadohealth.2012.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nelson MC, Larson NI, Barr-Anderson D, Neumark-Sztainer D, Story M. Disparities in Dietary Intake, Meal Patterning, and Home Food Environments Among Young Adult nonstudents and 2- and 4-Year College Students. Am J Public Health. 2009;99(7):1216–9. doi: 10.2105/AJPH.2008.147454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Laska MN, Pasch K, Lust K, Story M, Ehlinger E. The differential prevalence of obesity and related behaviors in two- vs. four-year colleges. Obesity (Silver Spring) 2011;19(2):453–6. doi: 10.1038/oby.2010.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Center for Education Statistics [September 22, 2014];Fast Facts: Back to School statistics for 2014. http://nces.ed.gov/fastfacts/display.asp?id=372.
- 8.Partridge SR, Juan J, McGeechan K, Bauman A, Allman-Farinelli M. Poor quality of external validity reporting limits generalizability of overweight and/or obesity lifestyle prevention interventions in young adults: a systematic review. Obes Rev. 2015;16:13–31. doi: 10.1111/obr.12233. [DOI] [PubMed] [Google Scholar]
- 9.Hebden L, Chey T, Allman-Farinelli M. Lifestyle intervention for preventing weight gain in young adults: a systematic review and meta-analysis of RCTs. Obes Rev. 2012;13:692–710. doi: 10.1111/j.1467-789X.2012.00990.x. [DOI] [PubMed] [Google Scholar]
- 10.Hutchesson M, Hulst J, Collins C. Weight management interventions targeting young women: a systematic review. J Acad Nutr Diet. 2013;113(6):795–802. doi: 10.1016/j.jand.2013.01.015. [DOI] [PubMed] [Google Scholar]
- 11.Nielsen LS, Danielsen KV, Sorensen TIA. Short sleep duration as a possible cause of obesity critical analysis of the epidemiological evidence. Obes Res. 2011;12:78–92. doi: 10.1111/j.1467-789X.2010.00724.x. [DOI] [PubMed] [Google Scholar]
- 12.Chen X, Beydoun MA, Wang Y. Is Sleep Duration Associated with Childhood Obesity? A Systematic Review and Meta-Analysis. Obesity. 2008;16(2):265–274. doi: 10.1038/oby.2007.63. [DOI] [PubMed] [Google Scholar]
- 13.Patel SR, Hu FB. Short Sleep Duration and Weight Gain: a systematic review. Obesity. 2008;16(3):643–653. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31(5):619–626. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Knutson KL, Van Cauter E. Associations between sleep loss and increased risk of obesity and diabetes. Ann N Y Acad Sci. 2008;1129:287–304. doi: 10.1196/annals.1417.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marshall NS, Glozier N, Grunstein RR. Is sleep duration related to obesity? A critical review of the epidemiological evidence. Sleep Med Rev. 2008;12(4):289–98. doi: 10.1016/j.smrv.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 17.Hart CN, Jelalian E. Shortened sleep duration is associated with pediatric overweight. Behav Sleep Med. 2008;6(4):251–267. doi: 10.1080/15402000802371379. [DOI] [PubMed] [Google Scholar]
- 18.Van Cauter E, Knutson KL. Sleep and the epidemic of obesity in children and adults. Eur J Endocrinol. 2008;159(Suppl 1):S59–S66. doi: 10.1530/EJE-08-0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Laska MN, Pasch KE, Lust K, Story M, Ehlinger E. Latent class analysis of lifestyle characteristics and health risk behaviors among college youth. Prev Sci. 2009;10(4):376–86. doi: 10.1007/s11121-009-0140-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mathur C, Stigler M, Lust K, Laska M. A Latent Class Analysis of Weight-Related Health Behaviors among 2- and 4-year College Students and Associated Risk of Obesity. Health Educ Behav. 2014;41(6):663–72. doi: 10.1177/1090198114537062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nigg C, Allegrante JP, Ory M. Theory-comparison and multiple-behavior research: common themes advancing health behavior research. Health Educ Res. 2002;17(5):670–679. doi: 10.1093/her/17.5.670. [DOI] [PubMed] [Google Scholar]
- 22.Evers K, Quintiliani L. Advances in multiple health behavior change research. Transl Behav Med. 2013;3(1):59–61. doi: 10.1007/s13142-013-0198-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kattelmann K, Bredbenner CB, White AA, Greene GW, Hoerr SL, Kidd T, et al. The effects of Young Adults Eating and Active for Health (YEAH): a theory-based Web-delivered intervention. J Nutr Educ Behav. 2014;46(6):S27–41. doi: 10.1016/j.jneb.2014.08.007. [DOI] [PubMed] [Google Scholar]
- 24.Werch C, Blan H, Moore M, Ames S, DiClemente C, Weller R. Brief multiple behavior interventions in a college student health care clinic. J Adol Health. 2007;41:577–585. doi: 10.1016/j.jadohealth.2007.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Laranjo L, Arguel A, Neves A, Gallagher A, Kaplan R, Mortimer N, et al. The influence of social networking sites on health behavior change: a systematic review and meta-analysis. J Am Med Inform Assoc. 2015;22(1):243–256. doi: 10.1136/amiajnl-2014-002841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maher C, Lewis L, Ferrar K, Marshall S, De Bourdeauhuij I, Vandelanotte C. Are health behavior change interventions that use online social networks effective? A systematic review. J Med Internet Res. 2014;16(2):e40. doi: 10.2196/jmir.2952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lytle LA, Moe SG, Nanney MS, Laska MN, Linde JA, Petrich CA, et al. Designing a weight gain prevetion trial for young adults: The CHOICES study. Am J Health Educ. 2014;45:67–75. doi: 10.1080/19325037.2013.875962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS Guideline for the Management of Overweight and Obesity in Adults A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll of Cardiol. 2014;63 doi: 10.1016/j.jacc.2013.11.004. (25_PA) [DOI] [PubMed] [Google Scholar]
- 29.Dietz WH, Baur LA, Hall K, Puhl RM, Taveras EM, Uauy R, et al. Management of obesity: improvement of health-care training and systems for prevention and care. Lancet. 2015;385(9986):2521–33. doi: 10.1016/S0140-6736(14)61748-7. [DOI] [PubMed] [Google Scholar]
- 30.Lytle LA, Svetkey LP, Patrick K, Belle SH, Fernandez ID, Jakicic JM, et al. The EARLY Trials: A Consortium of Studies Targeting Weight Control in Young Adults. Transl Behav Med. 2014;4(3):304–13. doi: 10.1007/s13142-014-0252-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Linde JA, Sevcik SM, Petrich CA, Gardner JK, Laska MN, Lozano P, et al. Translating a health behavior change intervention for delivery to two-year college students: the importance of formative research. Transl Behav Med. 2013 doi: 10.1007/s13142-013-0243-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nelson MC, Larson NI, Barr-Anderson D, Neumark-Sztainer D, Story M. Disparities in dietary intake, meal patterning, and home food environments among young adult nonstudents and 2- and 4-year college students. Am J Public Health. 2009;99(7):1216–9. doi: 10.2105/AJPH.2008.147454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nanney MS, Lytle L, Farbakhsh K, Moe SG, Linde JA, Gardner JK, et al. Weight and weight-related behaviors among 2-year college students. J Am Coll Health. 2015;63(4):221–9. doi: 10.1080/07448481.2015.1015022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nelson MC, Lytle LA. Development and evaluation of a brief screener to estimate fast-food and beverage consumption among adolescents. J Am Diet Assoc. 2009;109(4):730–4. doi: 10.1016/j.jada.2008.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.National Cancer Institute [July 28, 2010];Diet History Questionnaire II. Available at: http:riskfactor.cancer.gov/dhq2/forms.
- 36.Paffenbarger RS, Jr, Hyde RT, Wing AL, Hsieh CC. Physical activity, all-cause mortality, and longevity of college alumni. N Engl J Med. 1986;314:605–613. doi: 10.1056/NEJM198603063141003. [DOI] [PubMed] [Google Scholar]
- 37.Gluck ME, Geliebter A, Satov T. Night eating syndrome is associated with depression, low self-esteem, reduced daytime hunger, and less weight loss in obese outpatients. Obes Res. 2001;9(4):264–7. doi: 10.1038/oby.2001.31. [DOI] [PubMed] [Google Scholar]
- 38.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index (PSQUI): A new instrument for psychiatric research and practice. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 39.Littell RC, Milliken GA, Stroup WW, Wolfinger RD, Schabenberger O. SAS for Mixed Models. 2nd ed. SAS Institute Inc; Cary, NC: 2006. [Google Scholar]
- 40.Laska M, Sevick SM, Moe SG, Petrich CA, Nanney MS, Linde JA, et al. A 2-year young adult obesity prevention trial in the US: Process evaluation results. Health Promot Int. 2015 doi: 10.1093/heapro/dav066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Short CE, Vandelanotte C, Dixon MW, Rosenkranz R, Caperchione C, Hooker C, et al. Examining participant engagement in an information technology-based physical activity and nutrition intervention for men: The Manup randomized controlled trial. JMIR Res Protoc. 2014;3(1):e2. doi: 10.2196/resprot.2776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Glasgow RE, Nelson CC, Kearney KA, Reid R, Ritzwoller DP, Strecher VJ, et al. Reach, Engagement, and Retention in an Internet-Based Weight Loss Program in a Multi-Site Randomized Controlled Trial. J Med Internet Res. 2007;9(2):e11. doi: 10.2196/jmir.9.2.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Johnson F, Wardle J. The association between weight loss and engagement with a web-based food and exercise diary in a commerical weight loss programme: a retrospective analysis. Int J Behav Nutr Phys Act. 2011;8(83) doi: 10.1186/1479-5868-8-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gokee-Larose J, Gorin AA, Raynor HA, Laska MN, Jeffery RW, Levy RL, et al. Are standard behavioral weight loss programs effective for young adults? Int J Obes (Lond) 2009;33(12):1374–80. doi: 10.1038/ijo.2009.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.