Abstract
Background:
Cloud-connected diabetes applications enable health care professionals (HCPs) to monitor patient progress and offer the potential for remote consultations. OneTouch Reveal (OTR) is a cloud-based web application that aggregates data from blood glucose (BG) meters or insulin pumps and provides analytics to help patients and HCPs make more informed treatment and lifestyle decisions. This study assessed the experience of patients using OTR and the OneTouch Verio (OTV) BG meter and determined the extent of changes in glycemic control.
Methods:
Subjects with T1DM (23) or T2DM (17) uploaded BG meter results to OTR for 12 weeks. HCPs remotely reviewed progress using OTR and delivered telephone consultations at 4 and 8 weeks based on OTR insights.
Results:
After 12 weeks, mean HbA1c decreased by 0.4% (P < .001) and 25% of subjects had a reduction of ≥1.0%. Reduction in HbA1c was similar in subjects with T1DM and T2DM, although subjects with T1DM started with higher baselines. In subjects with T2DM, mean BG decreased significantly from 175 to 161 mg/dl (P < .001) with the percentage of above-range BG results decreasing from 33% to 24%. 80% of subjects confirmed OTR detected out-of-range glucose patterns and 84% of these subjects were able to correct the underlying pattern to get BG back in-range.
Conclusions:
OTR web application in combination with the OTV meter helped subjects with T1DM and T2DM effectively manage their diabetes and was associated with improved BG control over 12 weeks. Real-time visibility to subject data may help HCPs deliver focused and effective remote consultations.
Keywords: diabetes management software, blood glucose monitor, self-monitoring of blood glucose
Mobile health technologies offer great potential for flexible and cost-effective delivery of diabetes care. Remote monitoring of data by patients and health care professionals (HCP) may be particularly beneficial for diabetes management that requires intensive monitoring and behavioral adjustment.1,2 Baron et al3 reviewed the clinical effectiveness of mobile health interventions in which patients transmit diabetes-related information to their HCP and found improved HbA1c even in studies without direct HCP feedback, suggesting HCP feedback might not always be necessary for success. Nevertheless, knowing their glycemic progress was visible and accessible to their HCPs was considered an incentive for patients’ adherence to their regimen.3 Furthermore, exchanging specific insights and gaining feedback from the HCP was seen as an effective incentive to engage and help patients identify relationships between their lifestyle and blood glucose (BG) patterns. In support of this, it has been reported that regular review of BG data provides the opportunity for patients and HCPs to identify clinically meaningful trends or patterns that may allow appropriate therapeutic decisions to be made.4 In a study by Janssen et al,5 patients using diabetes management software (GLUCOFACTS®) providing both text and graphic presentations from uploaded BG data had significantly lower HbA1c levels of 0.4% over 12 months compared to the control group. Tildesley et al6 assessed the value of an Internet-based system that enabled the HCP to provide feedback remotely between scheduled visits. Improvements in HbA1c were noted in the intervention group after 6 months. Studies evaluating the utility of the WellDoc™ management system across 26 primary care sites involving 163 T2DM subjects showed a mean decline in HbA1c of 1.2% over 12 months in the intervention group compared with usual care,7,8 demonstrating a combination of a mobile and web-based HCP application improved HbA1c.
The OneTouch Reveal® (OTR) web application allows patients and HCPs to track progress and changes in glycemic control to support both self-management and therapy decisions by summarizing BG or insulin data, displaying color-coded trends or low or high BG patterns. OTR also provides online educational tips and enables patients to share their diabetes information with their HCP in real time between scheduled visits or use OTR to review progress during face-to-face consultations. This study focused on gathering experiences of patients using OTR in combination with the OneTouch Verio® (OTV) meter and evaluated changes in glycemic control and diabetes management when patients and HCPs shared progress remotely over time.
Methods
This single arm, open label study was conducted at 2 National Health Service (NHS) clinics in Scotland, UK (Highland Diabetes Institute, Inverness, and Royal Infirmary, Edinburgh) with ethics approval. Diabetes specialist nurses recruited subjects already referred to the hospitals for ongoing diabetes care. Subjects provided written informed consent prior to initiation. Subjects were between 18 and 70 years of age, diagnosed with T1DM or T2DM for ≥ 3 months with a current HbA1c of ≤ 11%, currently performing self-monitoring of blood glucose (SMBG) and had a home computer (PC) with Internet access. The OTV meter features a novel color range indicator (CRI) that identifies whether the patient’s current BG result is low (blue), in-range (green), or high (red) based on range limits set in the meter. The default range is 70-180 mg/dl but can be customized by the subject and/or HCP. OTR automatically identifies high and low glucose patterns from SMBG data. A high pattern is identified when 3 high BG results (above the in-range limit) occur in the same 3-hour timeframe over the preceding 5 days. A low pattern is detected when 2 low BG results (below in-range limit) occur in the same 3-hour timeframe over the preceding 5 days.
Visit 1 (Screening)
Visit 1 was performed 1 week before baseline and included informed consent, collection of demographic, medical history information and evaluation of inclusion and exclusion criteria. Subjects received instruction on how to set up the OTR web application online and how to upload BG results or insulin pump data using software cables. Subject SMBG data uploaded to the web application was immediately available for HCPs to view on-line. Subjects also received a short explanation of the OTV meter.
Visit 2 (Baseline)
At Visit 2, the HCP set appropriate identical glucose range targets on both the OTV meter and OTR to ensure consistent color range indication and glucose pattern identification.
Home activities
Subjects were asked to perform ≥ 2 SMBG tests per day, upload their BG data from OTV to OTR every 2 weeks and review their 14-day OTR summary report every 2 weeks to enable insight and education (Figure 1). Subjects were encouraged to add context (e.g., meal tagging, insulin dosage or lifestyle notes) to OTR to enrich the uploaded SMBG data.
Figure 1.
Connectivity between the OneTouch (OT) Verio meter, OT Reveal (patient), and OT Reveal (HCP) web applications
Telephone consultations
After 4 and 8 weeks, HCPs had a telephone consultation with each subject to review OTR data and provide specific therapy (eg, insulin adjustment) or lifestyle recommendations based on their remote review of SMBG trends, patterns and analysis within OTR.
Visit 3
After 12 weeks, subjects returned to the clinic for a final HbA1c determination. Subjects also completed paper acceptance surveys for OTR and the OTV meter.
Statistical Analyses
Continuous demographic variables were described as median and range (minimum to maximum) or mean and standard deviation (SD). Categorical demographic variables were described as percentages within categories. Correlations with HbA1c were assessed using the Pearson correlation coefficient and deemed significant at P < .05. Minitab 16.1.1 was used for all analyses.
Results
Subjects
Baseline characteristics of the 40 subjects are shown in Table 1. The mean age of subjects was 49.3 years with a mean duration of SMBG use of 13.4 years. In all, 85% of subjects reported they currently performed SMBG at least 1-2 times per day, and 50% of the subjects were currently on insulin therapy alone (2 on insulin pump), 22.5% on insulin and anti-hyperglycemic agents (AHA) and 27.5% on AHA alone. The mean HbA1c across all 40 subjects was 8.3%; 8.6% in the 23 subjects with T1DM and 7.9% in the 17 subjects with T2DM. In surveys to understand prior experience with mobile technology/software 70% of subjects responded that their current HCP had never used diabetes software to download their SMBG data; 81% had never used diabetes software; and 68% had no diabetes applications on their smartphone.
Table 1.
Baseline Subject Demographics (N = 40).
| Sex (number, %) | |
| Male | 18 (45%) |
| Female | 22 (55%) |
| Age, years (mean, range) | 49.3 (24-70) |
| Diabetes type (number of subjects, %) | |
| T1DM | 23 (58%) |
| T2DM | 17 (42%) |
| HbA1c (mean, SD, range) | |
| All subjects | 8.3% (1.4, 5.7-11.0) |
| T1DM | 8.6% (1.3, 6.7-10.8) |
| T2DM | 7.9% (1.4, 5.7-11.0) |
| Duration of diabetes, years (mean, SD, range) | |
| All subjects | 19.5 (12.9, 3.0-58.0) |
| T1DM | 24.9 (13.9, 4.7-58.0) |
| T2DM | 12.1 ( 6.4, 3.0-30.3) |
| SMBG frequency (number of subjects) | |
| ≥5 times/day | 11 |
| 3-4 times/day | 12 |
| 1-2 times/day | 11 |
| 2-6 times/week | 3 |
| ≤1 time/week | 3 |
| Treatment therapy (number of subjects) | |
| Basal + bolus insulin | 18 |
| Insulin + anti-hyperglycemic agents (AHA) | 9 |
| AHA only | 11 |
| Insulin pump | 2 |
Changes in Glycemic Control
After 12 weeks, mean HbA1c across all 40 subjects decreased by 0.4% from 8.3% to 7.9% (P = .001 paired t test) (Table 2). Statistically significant reductions in HbA1c were observed in the 23 subjects with T1DM (Table 2). Similar changes in HbA1c were seen in the cohort of 17 subjects with T2DM, although not statistically significant (Table 2). In all, 25% and 40% of subjects had HbA1c reductions of ≥1.0% or ≥0.5%, respectively. Overall, HbA1c improvement was observed in 29 subjects with a mean HbA1c improvement of 0.7% (0.5%, SD) (Figure 2). HbA1c increased in 8 subjects and was unchanged in 3 subjects (Figure 2). There was no correlation between changes in HbA1c and duration of diabetes, baseline HbA1c, SMBG or treatment therapy. On average, the percentage of in-range BG results across all 40 subjects increased over the last 2 weeks compared with the first 2 weeks, with mean BG decreasing from 175 to 161 mg/dl (P < .001). In subjects with T2DM, the percentage of high BG results decreased from 33% to 24% (P = .002) and in-range BG results increased from 66% to 75% (P = .001). In subjects with T1DM, high BG results also decreased and in-range BG results also increased, but these changes were not statistically significant.
Table 2.
Baseline HbA1c and Change in Baseline HbA1c After 12 Weeks Home Use of the OneTouch (OT) Verio Meter in Combination With the OT Reveal Web Application.
| All subjects (n = 40) | T1DM (n = 23) | T2DM (n = 17) | |
|---|---|---|---|
| Baseline HbA1c, % | 8.3 ± 0.2 | 8.6 ± 0.2 | 7.9 ± 0.2 |
| Week 12 HbA1c, % | 7.9 ± 0.2 | 8.2 ± 0.2 | 7.5 ± 0.2 |
| Difference, % | −0.40 | −0.41 | −0.38 |
| 95% CI, % | −0.63 to −0.17 | −0.68 to −0.15 | −0.83 to 0.07 |
| P value | .001 | .03 | .09 |
Data are mean ± standard error of the mean (SEM).
Figure 2.
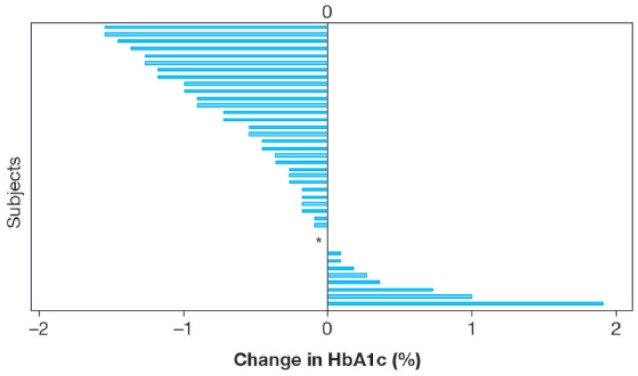
Change in baseline HbA1c after 12 weeks home use of the OneTouch Verio meter in combination with the OneTouch Reveal web application. Each bar represents an individual subject. *3 subjects had no change in HbA1c after 12 weeks.
SMBG Uploads
Subjects were asked per protocol to upload SMBG data at least once every 2 weeks. Subjects performed a median of 10 downloads during the 12-week study, almost double the minimum number requested per protocol. There was no significant difference between the median number of uploads performed by subjects with T1DM compared to subjects with T2DM. The frequency of uploads to OTR did not change over 12 weeks.
Glycemic Ranges and Blood Glucose Patterns
In all, 40% of subjects personalized their BG range settings with the remaining 60% accepting the default range (70 to180 mg/dl). Over 12 weeks, 695 high BG patterns (538 in T1DM and 157 in T2DM subjects) and 116 low BG patterns (114 in T1DM and 2 in T2DM subjects) were detected. This translated into approximately 2.1 and 0.8 high BG patterns per subject per week in T1DM and T2DM subjects, respectively. During phone consultations, 80% of subjects confirmed that the OTR web application detected out-of-range glucose patterns, with 84% of these subjects reporting that they were able to correct the underlying glucose pattern to get their BG back in-range.
Therapeutic Adjustments Based on Telephone Consultations
Therapeutic adjustments by the subjects could be advised by their HCP during telephone consultations at 4 and 8 weeks or by the subjects anytime during the study. Based on OTR information, adjustments to insulin dose or timing represented 41% of all adjustments, whether advised by the HCP or taken by subjects themselves. Changes in diet/lifestyle only (11%), diet/lifestyle plus insulin (9%), medication (6%), and SMBG (3%) were also noted. HCPs decided no adjustment was required in 30% of phone consultations, 11% of the time because OTR indicated that the subjects’ SMBG data was generally within range.
Subject Perceptions of OTV and OTR
Surveys designed to explore perceptions of the OTR web application showed that 83% of all subjects felt more secure knowing they had easy access anywhere to all their diabetes information; helped them consider the choices they made; helped them see the big picture; motivated them to stick to their plan; and would recommend the application to other people with diabetes (Table 3). In those subjects expressing a preference, 97% said OTR motivated them to make progress (Table 4).
Table 3.
Subject Responses to Survey Statements Regarding the OneTouch (OT) Reveal Web Application (N = 40).
| Statement | Favorable response, % |
|---|---|
| I feel more secure knowing I have easy access, anywhere, to all my diabetes information | 83 |
| OT Reveal has helped me to consider the choices I make | 83 |
| OT Reveal helps me see the big picture and motivates me to stick to my plan | 83 |
| I would recommend this application to other people with diabetes | 83 |
| OT Reveal unlocked my blood sugar data so I could see trends and patterns | 80 |
| OT Reveal helped me to identify a trouble spot in my blood sugar and I was able to take action to resolve it. | 78 |
| OT Reveal helped me recognize what I was doing right so I can continue to keep my sugars in-range | 78 |
| OT Reveal simplifies my diabetes management | 75 |
| I have been able to correct problems in my blood sugar based on a pattern that OT Reveal helped me detect. | 73 |
Favorable responses are defined as a response of “strongly agree” or “agree” on a 5-point scale (5 = “strongly agree,” 4 = “agree,” 3 = “neither agree nor disagree,” 2 = “disagree,” and 1 = “strongly disagree”).
Table 4.
Subject Responses to Survey Statements Regarding OneTouch (OT) Reveal Web Application Among Those Subjects Expressing a Preference of Strongly Agree, Agree, Disagree, or Strongly Disagree.
| Statement | n | Favorable response, % |
|---|---|---|
| OT Reveal motivates me to continue to make progress | 29 | 97 |
| I now worry less about trying to identify my trouble spots than before | 22 | 96 |
| I’ve been able to better understand how my actions impact my blood sugar averages over time | 32 | 94 |
| I would want my doctor to use this in their clinic | 30 | 93 |
| OT Reveal helped me understand how my day-to-day choices affect my blood sugar levels | 29 | 93 |
| I feel like I’m doing better at managing my diabetes after using OT Reveal | 27 | 89 |
| Since using OT Reveal, I’m now taking better control of my diabetes | 27 | 89 |
| The 14 day summary allowed me to more easily discuss my blood sugar with my doctor (nurse) | 30 | 87 |
| OT Reveal helped me have better conversations with my doctor (nurse) | 24 | 83 |
| Testing my blood sugar is more meaningful when using OT Reveal | 29 | 83 |
| My OT Verio meter is more valuable to me with OT Reveal | 32 | 81 |
| Managing diabetes is now more convenient now that I’m using OT Reveal | 27 | 82 |
| OT Reveal helped me discover new things about my blood sugar control | 31 | 81 |
| My ability to recognize when I’m going out of range has improved since using OT Reveal | 32 | 78 |
| OT Reveal helped me plan a better daily routine | 25 | 76 |
Discussion
Improving glycemic control is challenging both for patients and HCPs, especially when time for office visits is limited.9-11 Tools that facilitate rapid evaluation of SMBG data by patients or HCPs, either remotely or during shorter office visits, may lead to more efficient clinical decisions. We found that the OTR web application used in combination with the OTV meter was associated with a significant reduction in HbA1c after 12 weeks in subjects with T1 and T2DM. The clinically meaningful reduction in HbA1c observed was noteworthy during such a short intervention and may reflect the value of using remote consultations in combination with OTR and OTV. This connected system is intended to enhance the specificity and quality of conversations between patients and HCPs and increase engagement of the patient in lifestyle and other behavioral changes which could improve their diabetes. The results observed are consistent with evidence from systematic reviews and meta-analysis which show that mobile health interventions can effectively reduce HbA1c3,12 and are equally, if not more effective in T2DM patients.13
The subjects in the current study had wide ranging baseline HbA1c values; and 6 subjects (15%) presented with good glycemic control (HbA1c, 5.7-6.9%). We deliberatively did not use a lower limit HbA1c as an exclusion criterion to help determine if usage of OTR and OTV could be associated with improved glycemic control in subjects with “normal” baseline HbA1c. Despite being considered in control at baseline, 4 of these 6 subjects further reduced their HbA1c after 12 weeks.
The T1D exchange14 previously reported a strong association between SMBG testing frequency and the ability to decrease HbA1c. SMBG frequency per subject did not change over time in our study, although it is possible that individual SMBG frequency was higher during the study as compared to self-reported baseline SMBG frequencies.
The primary goal of OTR is in accordance with the observation by Schnell15 that SMBG enables individuals to safely manage their condition, detect hyper- and hypoglycemia, and generate information to support adjustment of medication, diet or activity. Despite this many patients do not readily perform SMBG or utilize data to make adjustments unless they suspected hypo- or hyperglycemia symptoms.16 Using our Internet-based solution, 80% of subjects confirmed that OTR enabled them to visualize low or high BG patterns with 84% of these subjects stating OTR allowed them to self-correct and get results back in-range. Although the ability to enable independent action is an important factor in improving glycemic control, appropriate HCP oversight remains essential. OTR is designed to enable patients and HCPs to easily discover trends and patterns in patient BG and promote appropriate decision-making. OTR assisted the HCP to arrive at therapeutic recommendations remotely and provide feedback to subjects.
The use of simple and consistent color-coded displays to help subjects and HCPs visualize glucose trends and identify specific low or high BG patterns may contribute to achieving more in-range BG results and subsequent decreases in HbA1c.17,18 Patients find BG targets motivational, enabling them to identify problems with control and prompting them to make independent or assisted insulin dose adjustments.19 We previously demonstrated that patients struggle to comprehend whether individual glucose values are low, in-range, or high20 but can significantly improve their ability to classify and interpret values after a short exposure to a meter-based color range indicator. In the current study, use of OTR in T2DM subjects was associated with a significant increase in the percentage of in-range BG values and a decrease in mean BG suggesting that therapy adjustments or behavioral changes translated to tighter glycemic control. In subjects with T1DM similar results were observed, but did not reach significance perhaps due to wider within- and between-subject glycemic fluctuations. A methodological change, such as mandating bimonthly 5-point profiles or structured testing may have enabled clearer trends to emerge.
Most patients continue to rely on their HCP to review SMBG data and determine appropriate actions during their limited number of traditional face-to-face visits. In our study, the ability of each HCP to remotely review data in real time between scheduled visits and offer phone consultations had the advantage of accelerating decision-making, perhaps contributing to the improved HbA1c and SMBG trends. This is consistent with the view of Blevins,21 who postulated that new mobile health technologies can facilitate improved patient-to-HCP communication that could lead to optimized glycemic control through more timely review and effective use of SMBG data. Subjects demonstrated strong engagement by uploading SMBG data to OTR on average about twice as often as required in the protocol, thereby enhancing the value of the phone consultations. In addition, uploading of data was consistent and did not diminish over time suggesting subjects found the experience rewarding. It is not known, however, if this frequency of uploading persisted beyond the study timeframe. In some institutions it is becoming standard practice to offer telemedicine. Tildesley et al22 reported that significant improvements in HbA1c were seen in patients who frequently uploaded data and received endocrinologist feedback by email. We did not observe a difference in HbA1c between frequent or less frequent uploaders to OTR, perhaps as a result of the high overall compliance to uploading in our subjects.
Recent reviews4,23 have highlighted the difficulty faced by patients and HCPs to manually detect and interpret patterns. Furthermore, clinical patterns of low BG may predict increased risk of severe hypoglycemia in the following 24-hour period.24 Algorithms within OTR and OTV automatically identify low and high glucose patterns. Not surprisingly, the majority of low patterns were detected in subjects with T1DM, consistent with their higher testing frequency and possibly wider daily glycemic excursions. We previously studied this algorithm in T1DM subjects on MDI therapy25 and found that the average number of high patterns correlated with higher baseline HbA1c, whereas low patterns correlated with lower baseline HbA1c. However, this association was not found in the present study, primarily because we had a mixed population with more variable SMBG frequency, unlike the study in MDI subjects in which structured testing (≥6 tests/day) was mandated.
It remains unclear which factors predispose patients to accept mobile health technologies or predict whether individual patients might continue to invest time in a given system. Lau et al26 examined the impact of online patient portal usage on glycemic control among patients newly referred to a diabetologist. Factors potentially adversely affecting portal use included level of health literacy, diabetes knowledge, and familiarity with internet technologies. Interestingly, although our subjects reported a lack of previous experience and/or interest in using diabetes software to manage their condition, they nevertheless responded favorably to OTR. Similarly, Glasgow et al27 found improvements in behavioral change associated with an internet-based program in 463 T2DM patients were not associated with education, computer experience or health literacy.
The increasing burden on resources of managing diabetes requires more flexible delivery strategies. In our study, real time access to OTR enabled HCPs to offer remote consultations to provide evidence-based insights and therapy recommendations. Using methodology similar to our study, Zhou et al28 observed improved HbA1c in patients with T2DM conducting 2 weekly uploads of SMBG data to an Internet-based system over 3 months, and concluding that where access to a medical center was more difficult, a significant reduction in face-to-face visits could save time and community resources.
Conclusion
The OT Reveal web application in combination with the OT Verio meter enabled subjects with T1DM and T2DM to effectively manage their diabetes and improve glycemic control. Real time access to OTR enabled HCPs to deliver remote consultations and enhanced the conversation during traditional face-to-face consultations. In future, OTR could minimize the need for face-to-face visits for some patients, thereby reducing time and cost associated with delivery of health care.
Acknowledgments
The authors would like to thank Lorna Stewart and Nichola Purvis for leadership of the study setup and conduct, and also Alison Sudworth (DSN, Edinburgh Royal Infirmary) and Claire Henderson (DSN, Highland Diabetes Institute) for the patient interactions.
Footnotes
Abbreviations: AHA, anti-hyperglycemic agent; BG, blood glucose; BGM, blood glucose monitor; HbA1c, hemoglobin A1c; HCP, health care professional; OTR, OneTouch Reveal; OTV, OneTouch Verio; SD, standard deviation; SEM, standard error of the mean; SMBG, self-monitoring of blood glucose.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: MG and HC are employees of LifeScan Scotland, Ltd. BLL and LBK are employees of LifeScan, Inc.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by LifeScan, Inc.
References
- 1. Health Quality Ontario. Home telemonitoring for type 2 diabetes. Ontario Health Technology Assessment Series. 2009;9(24):1-38. [PMC free article] [PubMed] [Google Scholar]
- 2. Agboola S, Hale MT, Masters C, Kvedar J, Jethwani K. “Real-world” practical evaluation strategies: a review of telehealth evaluation. JMIR Res Protoc. 2014;3(4):e75 DOI: 10.2196/resprot.3459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Baron J, McBain H, Newman S. The impact of mobile monitoring technologies on glycosylated hemoglobin in diabetes: a systematic review. J Diabetes Sci Technol. 2012;6(5):1185-1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Choudhary P, Genovese S, Reach G. Blood glucose pattern management in diabetes: creating order from disorder. J Diabetes Sci Technol. 2013;7(6):1575-1584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Janssen M, Portalatin M, Wallace J, Zhong W, Parkes JL. Ascensia® WinGLUCOFACTS® professional software improves diabetes health outcomes. J Diabetes Sci Technol. 2007;1(1):47-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tildesley HD, Adel B, Mazanderani AB, Ross SA. Effect of Internet therapeutic intervention on A1C levels in patients with type 2 diabetes treated with insulin. Diabetes Care. 2010;33:1738-1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Quinn CC, Sysko-Clough S, Minor JM, Lender D, Okafor MC, Gruber-Baldini A. WellDoc™ mobile diabetes management RCT: change in clinical and behavioral outcomes and patient and physician satisfaction. Diabetes Technol Ther. 2008;10(3):160-168. [DOI] [PubMed] [Google Scholar]
- 8. Quinn CC, Shardell MD, Terrin LM, Barr EA, Ballew SH, Gruber-Baldini A. Cluster-randomized trial of a mobile phone personalized behavioral intervention for blood glucose control. Diabetes Care. 2011;34:1934-1942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Barnes CS, Ziemer DC, Miller CD, et al. Little time for diabetes management in the primary care setting. Diabetes Educ. 2004;30:126-135. [DOI] [PubMed] [Google Scholar]
- 10. Valentine V. Insulin initiation during a 20-minute office visit: part 1: setting the scene. Diabetes Spectrum. 2010;23:188-193. [Google Scholar]
- 11. Willens D, Cripps R, Wilson AW, Wolff K, Rothman R. Interdisciplinary team care for diabetic patients by primary care physicians, advanced practice nurses, and clinical pharmacists. Clin Diabetes. 2011;29:60-68. [Google Scholar]
- 12. Saffari M, Ghanizadeh G, Koenig HG. Health education via mobile text messaging for glycemic control in adults with type 2 diabetes: a systematic review and meta-analysis. Primary Care Diabetes. 2014;8(4):275-285. [DOI] [PubMed] [Google Scholar]
- 13. Liang X, Wang Q, Yang X, et al. Effect of mobile phone intervention for diabetes on glycaemic control: a meta-analysis. Diabetic Med. 2011;28:455-463. [DOI] [PubMed] [Google Scholar]
- 14. Miller KM, Beck RW, Bergenstal RM, et al. Evidence of a strong association between frequency of self-monitoring of blood glucose and hemoglobin A1c Levels in T1D exchange clinic registry participants. Diabetes Care. 2013;36:2009-2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Schnell O. Addressing schemes of self-monitoring of blood glucose in type 2 diabetes: a European perspective and expert recommendation. Diabetes Technol Ther. 2011;13(9):959-965. [DOI] [PubMed] [Google Scholar]
- 16. Hansen MV, Pedersen-Bjergaard U, Heller SR, et al. Frequency and motives of blood glucose self-monitoring in type 1 diabetes. Diabetes Res Clin Pract. 2009;85:183-188. [DOI] [PubMed] [Google Scholar]
- 17. Wei N, Zheng H, Nathan DM. Empirically establishing blood glucose targets to achieve HbA1c goals. Diabetes Care. 2014;37(4):1048-1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Spollet RS. Self-monitoring of blood glucose: an underutilized tool. Clin Diabetes. 2010;28(3):127-129. [Google Scholar]
- 19. Rankin D, Cooke DD, Heller S, Elliott J, Amiel S, Lawton J. Experiences of using blood glucose targets when following an intensive insulin regimen: a qualitative longitudinal investigation involving patients with Type 1 diabetes. Diabetes Med. 2012;29:1079-1084. [DOI] [PubMed] [Google Scholar]
- 20. Grady M, Warren G, Levy BL, Katz LB. Interactive exposure with a blood glucose monitor with a novel glucose color range indicator is associated with improved glucose range interpretation and awareness in patients with type 2 diabetes. J Diabetes Sci Technol. 2015;9(4):841-848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Blevins T. Value and utility of self-monitoring of blood glucose in non-insulin treated patients with type 2 diabetes mellitus. Postgrad Med. 2013;125(3):191-204. [DOI] [PubMed] [Google Scholar]
- 22. Tildesley HD, Conway ME, Ross SA, et al. Review of the effect of Internet therapeutic intervention in patients with type 1 and type 2 diabetes. Diabetes Care. 2014;37:31-32. [DOI] [PubMed] [Google Scholar]
- 23. Hirsch IB, Amiel SA, Blumer IR, et al. Using multiple measures of glycemia to support individualized diabetes management: recommendations for clinicians, patients, and payers. Diabetes Technol Ther. 2012;14(11):973-983. [DOI] [PubMed] [Google Scholar]
- 24. Lee-Davey J, Alexander S, Raja P. Clinical patterns of low blood glucose identified by a pattern algorithm may predict increased risk of severe hypoglycemia in the following 24-hour period. Paper presented at: ATTD Conference; February 16-19, 2011; London, UK. [Google Scholar]
- 25. Grady M, Campbell D, MacLeod K, Srinivasan A. Evaluation of a blood glucose monitoring system with automatic high- and low-pattern recognition software in insulin-using patients: pattern detection and patient-reported insights. J Diabetes Sci Technol. 2013;7(4):970-978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lau M, Campbell H, Tang T, Darby J, Thompson D, Elliot T. Impact of patient use of an online patient portal on diabetes outcomes. Can J Diabetes 2014;38:17-21. [DOI] [PubMed] [Google Scholar]
- 27. Glasgow RE, Kurz D, King D, et al. Twelve-month outcomes of an Internet-based diabetes self-management support program. Patient Education Counseling. 2012;87:81-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Zhou P, Xu L, Liu X, Huang J, Xu W, Chen W. Web-based telemedicine for management of type 2 diabetes through glucose uploads: a randomized controlled trial. Int J Clin Exp Pathol. 2014;12(7):8848-8854. [PMC free article] [PubMed] [Google Scholar]