Abstract
Background:
Continuous glucose monitoring (CGM) patient systems have been shown to improve diabetes self-treatment when used consistently. The meaningful integration of this technology into everyday life, however, can vary greatly among CGM users and not all people with diabetes use CGM to its full potential. To address this issue, the study pursued 2 aims: first, to identify patient characteristics that underlie the acceptance of CGM in people with type 1 diabetes and, second, to examine the effects of different levels of experience with CGM use.
Methods:
Guided by a model based on the technology acceptance model (TAM), structural equation modeling (SEM) was employed to model the patient characteristics as predictors of CGM acceptance. In all, 111 participants (60.4% female, mean = 37.6 years, SD = 11.2) participated in a web-based survey; 40 were current CGM users, 18 were former users and 53 had no experience with CGM systems.
Results:
In general, participants evaluated CGM positively; however, the feeling of information overload represented a major barrier to the sustained use of CGM, while perceptions of usefulness and ease of use constituted incentives for using this technology. Moreover, patients without CGM experience imagined more information overload than current users reported. Current users showed more intention to use CGM than former users.
Conclusion:
This study highlights the importance of CGM user experience for the effective use of this technology.
Keywords: continuous glucose monitoring (CGM), type 1 diabetes, technology acceptance model (TAM), human factors, structural equation modeling (SEM)
Continuous glucose monitoring (CGM) has been shown to be a powerful tool in type 1 diabetes self-management facilitating glycemic control, optimizing A1C, and avoiding hypoglycemia, when used consistently.1,2 However, CGM benefits can vary greatly among CGM users and not all patients use the technology to its full potential.3 While there is clear evidence that users exhibiting high adherence and sustained CGM use benefit from it, a substantial number of people with diabetes do not succeed at integrating CGM into their diabetes self-management and, consequently, take less advantage of this technology.4,5 Physical, perceptual, cognitive, or behavioral aspects—also known as human factors6—may play a role in the effectiveness of CGM use.3 Some human factors like expectations, perceived burden, and the ability to trust the technology have demonstrated before to be potential barriers to patients’ engagement with diabetes devices.7
Ritholz and colleagues examined the differences between CGM users who showed a greater improvement in glycemic control (responders) and those who showed less improvement (nonresponders).5 They differed, among other things, in the following facets: First, the attitudes of the patients’ family and social environment may either facilitate or impede effective CGM use, with supportive attitudes being more helpful. Second, nonresponders may have experienced information overload caused by the CGM’s real-time glucose readings. Furthermore, a perceived change in body image and a perceived increased visibility of diabetes while wearing CGM devices were found to be potential disadvantages.5,8
In a similar vein, another study showed that satisfaction with CGM was associated with a more frequent use of it and benefits of the CGM, like the availability of glucose trends/graphs and the ability to self-correct out-of-range glucose levels in real time, were found to influence CGM satisfaction.8 Ease of use and the capacity to trust the information provided by CGM may play, in turn, a role in the perception of usefulness.3 False alarms, for example, give the impression that CGM systems are sometimes unreliable.4,8
As with any other technology innovation, people clearly differ in how easily they accept and adopt CGM. Analogies may be drawn to studies that examined the adoption of information technology that found, for instance, a clear relationship between technology-related self-efficacy, also known as information technology expertise,9 and perceived ease of use of technological systems.10,11 Based on this premise, we assume that technology-related self-efficacy should also play a role in conjunction with CGM use. Although technology-related self-efficacy is associated with age, with older people showing less self-efficacy in this field,12 the effectiveness of CGM was found to be similar for all age groups when the technology was used intensely; however, older patients showed a considerably more frequent use of CGM system than younger patients such as children and adolescents.1
We aimed to investigate these relationships with a focus on adult type 1 diabetics, pursuing 2 major goals: first, to identify possible motives that underlie the acceptance of CGM systems—defined here as the intention to use CGM to support one’s own diabetes treatment—and second, to compare characteristics between patient groups with different levels of CGM experience. For this purpose, we expanded a well-established model used in human factors research, the technology acceptance model (TAM; see Figure 1),13 and derived and developed measures for psychosocial factors as identified in literature. The TAM has been widely used to investigate acceptance and use of technologies.14 In this study, we predicted that the TAM expanded to include CGM-specific human factors (TAM-CGM) is suited to model CGM acceptance in people with type 1 diabetes. Furthermore, to investigate if these factors vary according to the level of experience with CGM, we hypothesized that patients without CGM experience, current users and former users differ in their perceptions of CGM.
Figure 1.
Technology acceptance model (TAM).13
Methods
Sample and Design
People with diabetes were approached in German-speaking diabetes self-help groups on Facebook as well as in other Internet forums about diabetes and invited to complete an online survey. Inclusion criteria were age ≥ 18 years and self-reported type 1 diabetes of at least 1-year disease duration. Patients who currently used or have previously used flash glucose monitoring (FGM) systems were excluded from participation. A total of 111 participants (60.4% female, age mean = 37.6 years, SD = 11.2) completed the survey (Table 1). Of the participants completing the survey, 40 used a CGM system at the time of data collection (group 1), 18 were former CGM users (group 2) and 53 had no CGM experience (group 3). The study protocol was approved by the local ethics committee. All participants gave their informed consent prior to completing the online survey.
Table 1.
Characteristics of Respondents.
| n | % | Mean | SD | Min | Max | |
|---|---|---|---|---|---|---|
| Age (years) | 37.55 | 11.16 | 18 | 63 | ||
| Sex | ||||||
| Female | 67 | 60.36 | ||||
| Male | 43 | 38.74 | ||||
| Not specified | 1 | 0.90 | ||||
| Education level | ||||||
| No education qualifications | 1 | 0.90 | ||||
| High school | 74 | 66.66 | ||||
| Higher education | 36 | 32.43 | ||||
| Living conditions | ||||||
| Alone | 21 | 18.92 | ||||
| With partner and/or children | 74 | 66.66 | ||||
| Shared apartment | 8 | 7.21 | ||||
| With parents | 8 | 7.21 | ||||
| Type of treatment | ||||||
| Intensified insulin therapy | 29 | 26.13 | ||||
| Insulin pump therapy | 81 | 72.97 | ||||
| Other | 1 | 0.90 | ||||
| System acquisition | ||||||
| Reimbursement by health insurance | 20 | 34.48 | ||||
| Purchased/received as gift | 21 | 36.21 | ||||
| As a loan from health care provider | 9 | 15.52 | ||||
| Other | 8 | 13.79 | ||||
Measurement of the Constructs
Since no validated measures were available for some of the variables in the CGM-TAM, novel scales were built based on relevant items of the CGM-Sat,15 on the German translation of the Computer User Self-Efficacy scale16 and on instruments that had previously been developed in TAM studies.13,17-19 The resulting questionnaire comprised 8 scales (see the appendix) besides age: Perceived Reliability was defined as the degree to which the patient confides in the CGM system and the glucose readings provided; Information Overload was defined as feelings of being overwhelmed by the novel kind of information continuously provided by CGM; Technology-Related Self-Efficacy describes confidence in one’s own skills in dealing with technology; Visibility of Body Change refers to the perception that one’s own body (image) changes while wearing a CGM system and that these undesired changes are visible for the patient and for others. The TAM scales were defined following Davis:13 Usefulness describes the degree to which an individual believes that CGM improves their diabetes management; Ease of Use describes the extent to which an individual believes that using a CGM system does not require substantial additional physical or mental effort; Attitude refers to positive or negative feelings toward CGM; finally, Intention is defined as an individual’s subjective probability that they will use a CGM-System. Items were rated on a 6-point Likert-type scale ranging from strongly disagree (1) to strongly agree (6).
Data Analysis
After investigating the scales’ dimensionality with exploratory factor analysis (EFA) using the principal axis method, promax rotation and Kaiser criterion for each scale, we tested hypothesis 1 with structural equation modeling (SEM) using maximum likelihood (ML) estimation for the total sample. Relative χ2 value (χ2/df) ≤ 2.5, root mean square error of approximation (RMSEA) < .8, comparative fit index (CFI) > .9, incremental fit index (IFI) > .9, and Tucker–Lewis index (TLI) > .9 were used as threshold values to estimate the overall model fit.20-22 In case of a poor model fit, it was necessary to modify the model using modification indices (MI). We also analyzed the possibility of carrying out mediation analyses using bootstrapping (2000 resamples) with bias-corrected confidence intervals (CI) at 95%. For hypothesis 2, Kruskal–Wallis tests were computed with subsequent Mann–Whitney tests for pairwise comparisons if significant. All data were analyzed with IBM SPSS Statistics 23 and IBM Amos 23 (IBM, Armonk, NY, USA).
Results
All scales showed Kaiser–Meyer–Olkin values greater than .5, significant Bartlett test results (P < .001) and measure of sampling adequacy greater than .6, therefore representing suitability for EFA. Communalities ranged from .504 to .897 and item-total correlations were between .623 and .851, which is acceptable. All scales were 1-dimensional and Cronbach’s alpha ranged from .843 to .926. The normality assumption was violated; however, ML estimation is robust for moderated violation of normality.23 Mahalanobis distances showed that the data presented no multivariate outliers. Overall, the mean values showed that the participants rated the advantages of CGM, such as Perceived Reliability (mean = 4.75, SD = 0.831), Ease of Use (mean = 5.35, SD = 0.788), and Usefulness (mean = 5.59, SD = 0.704), as high and the disadvantages, for example, Information Overload (mean = 1.56, SD = 0.815) and Visibility of Body Change (mean = 1.55, SD = 0.856), as small (see Table 2).
Table 2.
Descriptive Statistics of the CGM-TAM Scales.
| N | Mean | SD | Min | Max | |
|---|---|---|---|---|---|
| Perceived Reliability | 111 | 4.75 | 0.831 | 1 | 6 |
| Information Overload | 111 | 1.56 | 0.815 | 1 | 6 |
| Technology-Related Self-Efficacy | 111 | 5.14 | 0.879 | 1 | 6 |
| Visibility of Body Change | 111 | 1.55 | 0.856 | 1 | 5 |
| Ease of Use | 111 | 5.35 | 0.788 | 1 | 6 |
| Usefulness | 111 | 5.59 | 0.704 | 2 | 6 |
| Attitude | 111 | 5.71 | 0.597 | 1 | 6 |
| Intention | 111 | 5.63 | 0.868 | 1 | 6 |
Model Fit
The original CGM-TAM did not reach the required thresholds of the quality criteria, for this reason we modified the model 7 times based on MI. MI offered relationships among items from different scales and among error terms, which suggests multicollinearity of the data. After modifications, the model showed to fit the data acceptably well, χ2/df = 1.553, RMSEA = .071, CFI = .930, IFI = .931, TLI = .918, and to be free of Heywood cases. However, the χ2 value was high and significant with χ2 = 402.2, P < .001. Given that the data violated the normality assumption, we calculated bootstrapped χ2 values; the model fitted better in 1263 of 2000 bootstrap samples and the Bollen–Stine bootstrap resulted in P = .369. This means that the violation of the normality assumption had a strong effect on the P value of χ2.23
Parameter Estimations
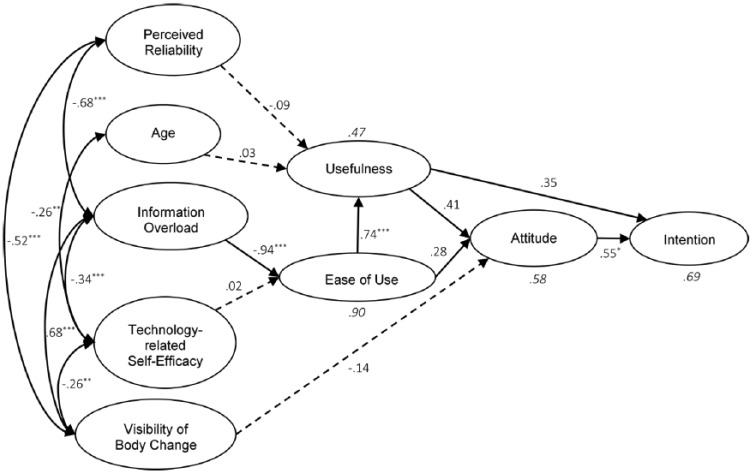
Figure 2 shows the final SEM with standardized parameter estimates of only the constructs. The path coefficients indicate that Information Overload had a strong negative influence on Ease of Use, β = –.943, P < .001; Ease of Use in turn showed a positive relationship with Usefulness, β = .741, P < .001, and with Attitude, β = .282, P < .05. Usefulness had a positive effect on Attitude, β = .411, P < .001, and Intention, β = .353, P < .001. Attitude also showed an influence on Intention, β = .548, P < .001. Perceived Reliability (β = –.088, P = .462), Age (β = .033, P = .679), Technology-Related Self-Efficacy (β = .022, P = .741), and Visibility of Body Change (β = –.189, P = .064) showed no significant effects on the respective endogenous variables.
Figure 2.
Parameter estimates of TAM-CGM with bootstrapped P values. Dotted arrows represent paths that are not significant, while continuous arrows denote significant ML-estimated paths. Paths with P values correspond to bootstrapped values. *P < .05. **P < .01. ***P < .001.
All covariances in the CGM-TAM were added based on MI. Visibility of Body Change showed relationships that seemed to be implausible at first glance; however, the MI that suggested such covariances were very high and thus essential for the model fitness. The highest correlations were found between Information Overload and Visibility of Body Change (.677, P < .001), and between Perceived Reliability and Information Overload (–.675, P < .001). Covariances of Technology-Related Self-Efficacy in relation to Visibility of Body Change (–.256, P < .01) and to Age (.260, P < .01) displayed the lowest relationships. Other covariances were identified between Perceived Reliability and Visibility of Body Change (–.517, P < .01), and between Information Overload and Technology-Related Self-Efficacy (–.340, P < .01). The model could explain 47% of the variance of Usefulness, 90% of Ease of Use, 58% of Attitude, and 69% of Intention.
We performed bootstrap sampling with bias correction for the CI to estimate effects more reliably and to perform mediation analyses. The bootstrapping results could not confirm the ML-based P values, as not all regression weights that originally showed significant coefficients remained significant. The path coefficients that remained significant were from Information Overload to Ease of Use (CI [–1.443, –0.785], P < .001), from Ease of Use to Usefulness (CI [0.297, 1.077], P < .001), and from Attitude to Intention (CI [0.058, 1.528], P < .05). The relationships between Usefulness and Intention (CI [–0.257, 1.463], P = .190), between Ease of Use and Attitude (CI [–0.119, 0.844], P = .158), and Perceived Usefulness and Attitude (CI [–0.105, 0.792], P = .108) were no longer significant. Hence, no relationship constellation showed to be suitable for mediation analyses in this model. Nevertheless, as shown in Table 3, the latent variables Information Overload (β = –.549, P < .05), Ease of Use (β = .582, P < .01), Usefulness (β = .578, P < .05), and Attitude (β = .548, P < .05) still had bootstrapped estimated significant total effects on Intention. Total effect is understood as the summation of the direct and indirect effects of a variable on another.24 All covariances added with MI remained significant except for 1 covariance between 2 error terms.
Table 3.
Standardized Total Effects in the SEM With Bootstrapped P Values.
| Explanatory variables |
Explained variables | |||
|---|---|---|---|---|
| Ease of Use | Usefulness | Attitude | Intention | |
| Information Overload | −.943** | −.699*** | −.553* | −.549** |
| Technology-Related Self-Efficacy | .022 | .017 | .013 | .013 |
| Perceived Reliability | −.088 | −.036 | −.051 | |
| Age | .033 | .014 | .019 | |
| Ease of Use | .741*** | .586* | .582** | |
| Visibility of Body Change | −.189 | −.104 | ||
| Usefulness | .411 | .578* | ||
| Attitude | .548* | |||
P < .05. **P < .01. ***P < .001.
Effects of CGM Experience
Before performing Kruskal–Wallis tests for the group comparisons, we used nonparametric Levene’s tests to verify the equality of variances in the samples.25 The only variances between the groups which were not equal were of the scales Attitude (P < .01) and Intention (P < .001), thus violating this assumption for Kruskal–Wallis test. The tests showed that there was a significant difference in the sample with respect to Information Overload, H(2) = 8.489, P < .05, with patients without experience rating it higher than current users, U = 716.5, P < .01. A significant difference regarding Intention to use a CGM system could also be observed, H(2) = 11.055, P < .01, whereby current users showed more intention to use CGM than former users, U = 226.5, P < .01. The others scales showed no significant differences between the groups (Perceived Usefulness: H(2) = 0.840, P = .657; Perceived Ease of Use: H(2) = 5.622, P = .060; Perceived Reliability: H(2) = 1.770, P = .413; Attitude: H(2) = 2.465, P = .292). Table 4 shows the pairwise comparisons between the groups for Perceived Information Overload and Intention.
Table 4.
Mean Ranks of the Groups and Pairwise Comparisons for Information Overload and Intention.
| Variable | Pairwise comparisons |
U | P | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Group A | N | Rank means | Group B | N | Rank means | ||||
| Information Overload | CU | 40 | 26.84 | × | FU | 18 | 35.42 | 253.5 | .047 |
| CU | 40 | 38.41 | × | PWE | 53 | 53.48 | 716.5 | .005 | |
| FU | 18 | 38.28 | × | PWE | 53 | 35.23 | 436.0 | .579 | |
| Intention | CU | 40 | 32.84 | × | FU | 18 | 22.08 | 226.5 | .001 |
| CU | 40 | 51.78 | × | PWE | 53 | 43.40 | 869.0 | .028 | |
| FU | 18 | 29.72 | × | PWE | 53 | 38.13 | 364.0 | .068 | |
Significance level is .017 after Bonferroni correction.
Discussion
This online survey investigated the role of human factors in CGM usage as well as describing variation in these factors depending on the level of experience with CGM. The model developed for this analysis, CGM-TAM, was derived from the general TAM and adapted to the specifics of CGM use. It covered the factors Perceived Reliability, Information Overload, Technology-Related Self-Efficacy, Visibility of Body Change, Usefulness, Ease of Use, Attitude and Intention to use CGM, and exhibited a good fit to the data. In general, survey respondents perceived, irrespective of their level of experience, the advantages of CGM as high and the disadvantages as low. However, we found evidence that Information Overload, through its influence on Ease of Use, could represent a major barrier to the effective use of CGM. High Usefulness, Ease of Use and positive Attitude on the other hand constituted incentives for using the technology. Age, Perceived Reliability, Technology-Related Self-Efficacy, and Visibility of Body Change showed no effect. Moreover, patients without CGM experience imagined more Information Overload than current users reported. Not surprisingly, current users showed more Intention to use CGM than former users.
Usefulness showed a stronger effect than Ease of Use, which is similar to other studies.14,19 However, the relationships of both variables with Intention were according to bootstrapped P values no longer significant. Contrary to previous qualitative research,4 age did not show effects on Usefulness. The lack of effect can be explained by the absence of children and adolescents in the sample, which make up the age groups considered problematic in terms of CGM adherence.1
Limitations
Important limitations of this study are the strong violation of the normality assumption and the rather small sample size, which can be responsible for measurement errors.26 Consequences of nonnormality concern an inflation of the χ2 value and the fact that the P values for the parameter estimates in the ML method tend to be significant, which leads to an increased Type I error rate.27 The bootstrapped P values showed a strong discrepancy in comparison with the ML estimated P values regarding significance, which might indicate the existence of relevant measurement errors.28
Another limitation concerns the fact that to produce valid estimations, the sample must widely represent the intended population, in this case the type 1 diabetics.29 Since the participants here tended to have a higher education level and were internet users, we cannot take this assumption for granted, so that we must expect even more bias in statistical estimations.29 Furthermore, it would have been important to control for other relevant variables: for example, the different CGM models used by the participants of this survey.
Conclusions
The term “human factors” is used in the context of product use, safety and reliability and refers, in the field of diabetes technology, to individual characteristics and abilities that are related to design, operation and use of products for optimizing diabetes self-management.7 The study showed one of these factors that may play an important role in consistent use of CGM, as the perception of Information Overload had a relevant negative effect on all key variables of TAM-CGM. Reduced complexity in the presentation of data may therefore facilitate CGM usability for some patients and thus improve user experience, possibly increasing adherence. The features of CGM should be clearly presented in marketing materials and, more importantly, the initial training for patients using a CGM system should focus on the complexity of the system.
FGM users were not included because of important differences between both systems: First, FGM does not need to be calibrated regularly, contrary to CGM; this could influence the perception of ease of use. Second, FGM is not able to trigger an alarm at risk of hypoglycemia; this can have consequences on the perception of usefulness, specially by users with hypoglycemia unawareness. Third, FGM users get more complex real-time information they need to interpret correctly, and this can lead to a different perception of ease of use and information overload. Hence, the results of this study may not be applicable to FGM users.
TAM-CGM is a model developed to assess CGM acceptance based on patient characteristics in an integrative manner. Based on the results of the present study, future research should focus on refining this model. Information Overload, Ease of Use and Usefulness appear to be promising key factors. Additional factors that could impact perceived information overload should also be considered: User characteristics, such as level of education, gender, or age, should be explored as they could act as powerful moderators. In this manner, it might be possible to identify what kind of patient could take better advantage of a reduced or increased complexity of data presentation: More concretely, it is possible that persons with a higher level of education might appreciate a more complex presentation of information or more available functions in a CGM-system. Following this approach, it would be possible to develop more appropriate CGM-models for specific target groups.
Appendix
Appendix.
Final TAM-CGM Scales and Items.
| Factor loadings (EFA) | |
|---|---|
| Perceived Reliability (Cronbach’s alpha = .88, explained variance = 65.5%) | |
| The device is very susceptible to interferences.a | .897 |
| CGM shows too many measurement errors.a | .825 |
| Overall, I think the system is reliable. | .794 |
| The device triggers false alarms too often.a | .710 |
| Information Overload (Cronbach’s alpha = .87, explained variance = 65.9%) | |
| Sometimes I do not know what to do with all the information provided by the CGM. | .884 |
| CGM provides too many readings. | .850 |
| It would be better if the CGM would provide less information. | .775 |
| CGM delivers too many information for me. | .728 |
| Technology-Related Self-Efficacy (Cronbach’s alpha = .84, explained variance = 64.88%) | |
| Generally, I think it is easy to learn how to use a new technology. | .854 |
| I feel me very confident in my abilities to make use of new technologies. | .782 |
| When I use a technological device, I do feel that I am in control. | .779 |
| Usefulness (Cronbach’s alpha = .85, explained variance = 56.2%) | |
| CGM makes it easier to keep blood glucose levels under control. | .889 |
| CGM improves diabetes self-management. | .787 |
| Ease of Use (Cronbach’s alpha = .86, explained variance = 67.6%) | |
| I think the system is ease to use. | .848 |
| I think it is difficult to adjust the system’s settings properly.a | .808 |
| Using the CGM is awkward.a | .811 |
| Attitude (Cronbach’s alpha = .85, explained variance = 68.6%) | |
| All in all, I can say: CGM to help with my diabetes disease is . . . | |
| Helpful. | .863 |
| Adversely.a | .863 |
| Visibility of Body Change (Cronbach’s alpha = .88, explained variance = 68.0%) | |
| CGM changes my body in a negative way. | .731 |
| CGM embarrasses me because I perceive myself as being different from the others. | .875 |
| I do not like to wear CGM because it arouses attention of other people. | .774 |
| The CGM embarrasses me, because I have to justify myself constantly. | .906 |
| Intentionb (Cronbach’s alpha = .92, explained variance = 86.1%) | |
| Assuming I continue having a CGM, I intend to use it. (current users). | .928 |
| Assuming I obtain a CGM again, I intend to use it. (former users). | |
| Assuming I obtain a CGM, I intend to use it. (patients without experience). | |
| Given that I continue having access to a CGM system, I predict that I will use it. (current users) | .928 |
| Given that I have access to a CGM system again, I predict that I would use it. (former users) | |
| Given that I have access to a CGM system, I predict that I would use it. (patients without experience) | |
Translated from German. aThe score of these items were inverted in the data analysis. bThese items have been presented separately depending on experience with CGM and grouped accordingly for data analysis.
Footnotes
Abbreviations: CFI, comparative fit index; CGM, continuous glucose monitoring; CU, current users; EFA, exploratory factor analysis; FGM, flash glucose monitoring; FU, former users; IFI, incremental fit index; MI, modification indices; ML, maximum likelihood; PWE, patients without experience; RMSEA, root mean square error of approximation; SEM, structural equation modeling; TAM, technology acceptance model; TLI, Tucker–Lewis index.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group,Beck RW, Buckingham B, et al. Factors predictive of use and of benefit from continuous glucose monitoring in type 1 diabetes. Diabetes Care. 2009;32(11):1947-1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. O’Connell MA, Donath S, O’Neal DN, et al. Glycaemic impact of patient-led use of sensor-guided pump therapy in type 1 diabetes: a randomised controlled trial. Diabetologia. 2009;52(7):1250-1257. [DOI] [PubMed] [Google Scholar]
- 3. Kubiak T, Mann C, Heinemann L. [Continuous glucose monitoring by the experience of the individual patient]. Diabetologie und Stoffwechsel. 2015;10(1):29-35 [German]. [Google Scholar]
- 4. Schmidt S, Duun-Henriksen AK, Nørgaard K. Psychosocial factors and adherence to continuous glucose monitoring in type 1 diabetes. J Diabetes Sci Technol. 2012;6(4):986-987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ritholz MD, Atakov-Castillo A, Beste M, et al. Psychosocial factors associated with use of continuous glucose monitoring. Diabet Med. 2010;27(9):1060-1065. [DOI] [PubMed] [Google Scholar]
- 6. Schaeffer NE. The role of human factors in the design and development of an insulin pump. J Diabetes Sci Technol. 2012;6(2):260-264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Barnard KD, Hood KK, Weissberg-Benchell J, Aldred C, Oliver N, Laffel L. Psychosocial assessment of artificial pancreas (AP): commentary and review of existing measures and their applicability in AP research. Diabetes Technol Ther. 2015;17(4):295-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tansey M, Laffel L, Cheng J, et al. Satisfaction with continuous glucose monitoring in adults and youths with type 1 diabetes. Diabet Med. 2011;28(9):1118-1122. [DOI] [PubMed] [Google Scholar]
- 9. Ernstmann N, Ommen O, Neumann M, Hammer A, Voltz R, Pfaff H. Primary care physician’s attitude towards the German e-health card project—determinants and implications. J Med Syst. 2009;33(3):181-188. [DOI] [PubMed] [Google Scholar]
- 10. Al-Haderi SMS. The effect of self-efficacy in the acceptance of information technology in the public sector. Int J Bus Soc Sci. 2013;4(9):188-198. [Google Scholar]
- 11. Igbaria M, Iivari J. The effects of self-efficacy on computer usage. Omega. 1995;23(6):587-605. [Google Scholar]
- 12. Reed K, Doty DH, May DR. The impact of aging on self-efficacy and computer skill acquisition. J Managerial Issues. 2005;17(2):212-228. [Google Scholar]
- 13. Davis FD. A technology acceptance model for empirically testing new end-user information systems: theory and results. Massachusetts Institute of Technology; 1985. Available at: http://dspace.mit.edu/handle/1721.1/15192. Accessed December 8, 2015.
- 14. King WR, He J. A meta-analysis of the technology acceptance model. Info Manage. 2006;43(6):740-755. [Google Scholar]
- 15. Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group. Validation of measures of satisfaction with and impact of continuous and conventional glucose monitoring. Diabetes Technol Ther. 2010;12(9):679-684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Spannagel C, Bescherer C. [Computer-related self-efficacy in courses with computer use]. Notes in Educational Informatics—Section A: Concepts and Techniques. 2009. 5(1):23-43 [German]. [Google Scholar]
- 17. van Bon AC, Kohinor MJE, Hoekstra JBL, von Basum G, deVries JH. Patients’ perception and future acceptance of an artificial pancreas. J Diabetes Sci Technol. 2010;4(3):596-602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Venkatesh V, Davis FD. A model of the antecedents of perceived ease of use: development and test. Decision Sci. 1996;27(3):451-481. [Google Scholar]
- 19. Venkatesh V. Determinants of perceived ease of use: integrating control, intrinsic motivation, and emotion into the technology acceptance model. Info Sys Res. 2000;11(4):342-365. [Google Scholar]
- 20. Bagozzi RP, Yi Y. On the evaluation of structural equation models. JAMS. 1988;16(1):74-94. [Google Scholar]
- 21. Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Structural Equation Modeling: A Multidisciplinary Journal. 2002;9(2):233-255. [Google Scholar]
- 22. Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107(2):238-246. [DOI] [PubMed] [Google Scholar]
- 23. Anderson JC, Gerbing DW. Structural equation modeling in practice: A review and recommended two-step approach. Psychol Bull. 1988;103(3):411-423. [Google Scholar]
- 24. Schreiber JB, Nora A, Stage FK, Barlow EA, King J. Reporting structural equation modeling and confirmatory factor analysis results: a review. J Educ Res. 2006;99(6):323-338. [Google Scholar]
- 25. Nordstokke DW, Zumbo BD, Cairns SL, Saklofske DH. The operating characteristics of the nonparametric Levene test for equal variances with assessment and evaluation data. Practical Assess Res Eval. 2011;16(5):1-8. [Google Scholar]
- 26. Kline RB. Principles and Practice of Structural Equation Modeling. 3rd ed. New York, NY: Guilford; 2011. [Google Scholar]
- 27. Finney SJ, DiStefano C. Non-normal and categorical data in structural equation modeling. In: Hancock GR, Mueller RO, eds. Structural Equation Modeling: A Second Course. Greenwich, CT: Information Age; 2006:269-314. [Google Scholar]
- 28. Cheung GW, Lau RS. Testing mediation and suppression effects of latent variables bootstrapping with structural equation models. Organizational Res Methods. 2008;11(2):296-325. [Google Scholar]
- 29. Haukoos JS, Lewis RJ. Advanced statistics: bootstrapping confidence intervals for statistics with “difficult” distributions. Acad Emerg Med. 2005;12(4):360-365. [DOI] [PubMed] [Google Scholar]