Abstract
Human epidermal growth factor receptor-2 (HER-2) is a well-established target for anticancer anticancerprecision medicine in humans. A HER-2 homologue with 92% amino acid identity has been described in canine mammary tumors, which whichis termed here as ‘dog epidermal growth factor receptor-2 (DER-2)’, with similar biological implications as those in human breast cancer. Both antigens can principally be immunologically targeted by anti-HER-2 antibodies, such as trastuzumab; however, the in vivo application applicationof humanized antibodies to other species would lead to specific hypersensitivity reactions. Therefore, HER-2 mimotope vaccines that actively induce autologous trastuzumab-like immunoglobulins represent a novel and economic treatment option to overcome species-specific limitations. Thus, the present review proposes the implementation of clinical trials with HER-2 vaccines in canine cancer model modelpatients with spontaneous DER-2 positive mammary gland carcinomas in order to assess their safety and efficacy. This approach would not only pave the way into the veterinary oncology market, but would also similarly generate robust data for human trials and facilitate the testing of novel combinatorial treatments.
Keywords: HER-2, dog, translational, cancer vaccine, oncology, mimotope
1. Introduction: Comparing HER-2 targeted therapies in human and canine cancer
Human epidermal growth factor receptor-2 (HER-2) is overexpressed in 25–30% of human breast cancers due to gene amplification, thus defining ‘HER-2-positive disease’ (1–3). HER-2-overexpression in human breast cancer has been associated with increased metastatic potential (4), poor disease-free and overall survival, and poor responsiveness to chemotherapy in vitro and in vivo (5,6). Besides surgery, radiation and the usual chemotherapy protocols, therapies used most successfully in HER-2-overexpressing cancers are those addressing HER-2 as a target on malignantly transformed cells (7,8). These so called ‘targeted therapies’ are well established in human HER-2-positive breast cancer and several agents have been approved for this indication over the last years (9,10). Examples of such targeted therapies that significantly improved disease outcome are trastuzumab (Herceptin®; Hoffmann-La Roche AG, Basel, Switzerland) and pertuzumab (Perjeta®; Hoffmann-La Roche AG) (11), two monoclonal antibodies used for passive immunotherapy in combination with different chemotherapy protocols (12), but tyrosine kinase inhibitors like lapatinib (Tyverb®; GlaxoSmithKline plc., London, UK) have also been proven to be effective (13).
Hardly any of these targeted therapies have been adapted for the use in canine patients or have yet been studied in veterinary clinical trials. To date, only the tyrosine kinase inhibitors masitinib (Masivet®; AB Science S.A., Paris, France) and toceranib (Palladia®; Pfizer Inc., New York, NY, USA), each targeting c-Kit, have been successfully tested in clinical trials and have been approved for canine mast cell tumor patients (14,15). In the case of toceranib, it was the efficacy of the human counterpart substance sunitinib (Sutent®; Pfizer Inc.) that led to the independent development of a similar drug in dogs (15,16).
A recent study revealed that in addition to a similar ErbB-2 overexpression rate in canine mammary gland tumors compared with the human disease counterpart (17–20), there was also an amino acid identity of 92% and a homology of 95% between canine dog epidermal growth factor receptor-2 (DER-2) and human HER-2 (21). Moreover, it was demonstrated that the targeting of DER-2 with trastuzumab led to the growth inhibition of canine tumor cells (21), indicating a similar biology in canine mammary carcinomas as that of the HER-2 system in human patients (19). The DER-2 status of mammary tumors in dogs is not yet considered in veterinary medicine, although its expression could be important in terms of carcinogenesis and disease severity, as well as in the development of novel targeted drugs (20,22).
2. HER-2 mimotope vaccines - a novel treatment approach
Trastuzumab, as aforementioned, is a humanized monoclonal antibody used for passive immunotherapy in human HER-2-positive breast cancer (12). In its humanized form, it is not applicable in comparative medicine studies, e.g., in canine models, as it represents a xenogeneic and highly immunogenic protein that is capable of inducing hypersensitivity (23–25). This risk can be minimized if the constant region domains are adapted to the given species (24,26). Only two such chimeric canine antibodies have been reported to date. One is based on cetuximab (Erbitux®; Merck KGaA, Darmstadt, Germany), a mouse-human chimeric anti-epidermal growth factor receptor (EGFR) antibody (26), and the second is a rituximab-like (MabThera®; Hoffman-La Roche AG, Basel, Switzerland) antibody targeting the B-cell antigen cluster of differentiation (CD)20 (27). However, these approaches are cost intensive, which may limit their market value in comparative medical studies and veterinary oncology. The cost factor, as well as the induction of autologous antibodies would favor active immunotherapies such as a vaccine over passive immunotherapy, not only for translational or comparative studies, but also for human patients (28,29).
A tumor vaccine acts as an active immunotherapy, training the immune system to induce polyclonal antibodies against a tumor-specific antigen. Several tumor vaccines are currently under clinical development in human breast cancer, aiming for the induction of antibodies against different tumor-associated proteins, e.g., mucin-1, telomerase reverse transcriptase or carcinoembryonic antigen (30). Correspondingly, several anti-HER-2 vaccines are also being studied in clinical trials, including NeuVax™, a CD8(+) T-cell-eliciting vaccine (31) and the AdHER2/neu dendritic cell vaccine, which is currently being tested in a phase I study (32).
Mimotopes, i.e. peptides mimicking protein, carbohydrate or lipid epitopes represent another novel and feasible option for cancer vaccines (33,34). In previous studies, we developed a series of mimotope vaccines against important tumor targets, including EGFR (35) and HER-2 (36). HER-2 specific mimotopes were generated via biopanning of phage display libraries with trastuzumab, and the deduced peptides were coupled to immunogenic carriers, such as keyhole limpet hemocyanin, for vaccination (37), or they were expressed as fusion proteins with carriers, such as adeno-associated viruses (AAV) or AAV-like particles (AAVLPs), with predictably high safety (38). The antigenicity, immunogenicity and tumoricidic effects of the HER-2 mimotope vaccines were demonstrated in vitro and in vivo in previous studies (37). The vaccine-induced HER-2 reactive trastuzumab-like antibodies also showed significant tumor inhibitory effects on HER-2-overexpressing human SK-BR-3 cell lines due to growth signal inhibition and growth receptor downregulation by internalization. More recently, an AAV-HER-2 vaccine resulted in significantly slower tumor growth in a BALB/c mouse model engrafted with D2F2E2 tumor cells, which expressed the HER-2 transgene (39). Notably, none of the mice showed any signs of vaccine-related side effects, including local or systemic reactions, or the well-described trastuzumab-associated cardiotoxicity (40).
3. Canine mammary carcinomas resemble human disease
Neoplasms of the mammary gland complex are the most common tumors in dogs, particularly occurring in non-spayed female individuals with a median age of first occurrence of around nine years (41,42). The incidence in female dogs of any breed is estimated at 50%, of which 40 to 50% are diagnosed as malignant (43). All of these malignant tumors have the potential to metastasize, either lymphogenously to the regional lymph nodes and the lung, or haematogenously directly to the lung and other distant organs (44). Metastasizing tumors and a tumor size of >3 cm result in a poor prognosis in terms of survival (44). Other prognostic factors are histological grade, differentiation of the tumor, and the presence of estrogen and/or progesterone receptors (45,46). Corresponding with human breast cancer, steroid-hormone receptor expression is frequent in canine mammary gland tumors and these receptors are important players in tumor development (44,47–49). In addition, other factors, including p53 overexpression and mutations, HER-2 overexpression or the immunological microenvironment of the tumor, are markedly comparable and show similar clinical correlations in dogs as in the human disease (17–21,44,50–53). Based on the discussed pathophysiological similarities between canine and human mammary gland carcinoma, dog cancer patients could serve as potential model patients for the study of disease biology, and particularly for the development of novel immunotherapies.
Usual treatment options at present are primarily surgery, radiation or chemotherapy (42,45). However, these are far from optimal and are often associated with serious side effects (54–56). The therapy of canine mammary carcinomas is therefore limited and the recurrence of the disease is frequent (44,57,58).
In summary, no optimal therapy for this indication exists to date, and treatment options that are commonly used in human clinical oncology, such as passive immunotherapy, have not yet been implemented in standard veterinary care.
Due to the high molecular homology, we anticipate that a vaccine targeted against HER-2, such as the aforementioned AAV HER-2 mimotope vaccine developed for human patients, could induce functional anti-HER-2 antibodies in dogs that are cross-reactive with the canine DER-2 and result in tumoricidic effects. Hence, such an active immunotherapy could be a novel and alternative approach, by inducing a polyclonal immune response with high antibody specificity and by additionally inducing immunological memory (33). In dog model patients, combinatory treatment strategies could be favorably tested. It is likely that a vaccine study in canine cancer patients with spontaneous HER-2-positive mammary gland carcinomas will deliver more robust results for human patients than animal experiments with induced or grafted tumors.
4. Translational relevance
It is clear that dogs with naturally occurring cancer would not only gain individual benefit by participating in a clinical trial, but could also act as animal model patients for human disease (16,46). Currently, the development of novel anticancer drugs is quite an inefficient procedure, where only 10.4% of novel agents that enter clinical phase I trials receive market approval by the Food and Drug Administration (59). The situation is even worse for novel cancer drugs, where this rate drops to only 6.7%, mostly due to the low success rate of anticancer biologicals (59). Another obstacle is that the development of a compound can take up to 15 years (60). The usual procedure of drug-development starts with designing a novel compound on the computer (computer aided drug design) (61) and testing it in vitro. Even though there is a legal requirement to replace animal experiments with alternative, ‘animal-free’ methods where possible (62), each drug has to be tested for toxicity in at least two animal species (61). Such animal models are also used to gain important information on pharmacokinetics and efficacy prior to being used in clinical trials in humans (63). If a drug has passed all preclinical tests, the clinical development starts with phase 0/I studies in healthy volunteers (or patients in oncological phase I trials), followed by further clinical phase II–IV trials in human patients (64,65).
However, animal patients with similar spontaneous diseases to humans are usually left out during this process of drug development, even though they could serve as ‘real life’ models for human diseases and are a missing link between the laboratory setting of animal experimentation and the ‘real life’ conditions (66). Companion animals, and particularly dogs, not only present with a similar pathophysiology of diseases, but also share their human owners' environmental surrounding and lifestyle, and thus are prone to develop similar diseases to humans, including cancer (67–69).
Drug efficacy and safety should be addressed in naturally occurring cancer, as these questions would be difficult to answer in rodent models or in human clinical trials alone. Research in animal patients could thus serve not only to complete data generation in human medicine, but also to establish novel drugs for usage in veterinary medicine itself (70). As described by Paoloni and Khanna (16), the parallel development of the compound SU11654 in dogs and sunitinib (Sutent®; Pfizer Inc.) in human cancer patients could act as an example of how the two disciplines could co-operate in respect to the translational development of agents in human and veterinary oncology.
An additional advantage of using the dog cancer patient as an animal model for human disease is the relatively shorter lifespan and thus a shorter time of disease development and response to treatment. This remains true even though the timespan to the conclusion of veterinary clinical trials is longer than experiments in rodent models (16,70). This time aspect would be further supported by the fact that clinical trials in pet patients are not constrained by the usual phase I–III trial designs in human medicine, and novel drugs can be offered to animal patients prior to any other conventional treatment being provided (16). Results that would take years to obtain in human clinical trials could be revealed in a relatively short timespan with dog patients, and then translated to humans. However, testing novel treatment strategies, and specifically targeted therapies, in veterinary oncology within clinical trials is not as common as in human oncology. Funding opportunities are rare and the difference to animal experimentation is legally rarely acknowledged (71).
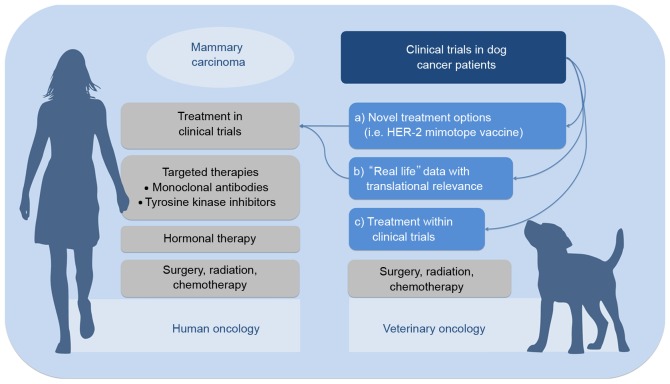
Overall, the clinical development of a drug in human medicine is cost- and time-intensive. With regard to HER-2-positive breast cancer, the high homology of DER-2-positive mammary carcinoma and its responsiveness to specific targeting (21) suggest that canine cancer patients could act as a ‘real-life model’ for human cancer patients. Furthermore, translating well-established therapeutic strategies from human to veterinary oncology would improve the currently available therapeutic options (Fig. 1).
Figure 1.
How clinical trials in canine cancer patients could contribute to the development of novel precision medicine options in mammary carcinomas in human and veterinary oncology. Current treatment options in HER-2-positive mammary carcinoma in veterinary and human oncology are represented in grey. Clinical trials in dog cancer patients can contribute by providing ‘real life’ data that are translatable to human medicine, by introducing novel treatment options in veterinary practice that impact human drug developments, and by granting the opportunity to veterinary patients to participate in clinical trials.
5. Conclusion: Where we stand
The differences in the therapies available to humans compared to those available to animals are very evident, particularly in oncology. Present cancer treatments for pet animals are frequently one step behind human medicine. Thus, surgery, chemotherapy and, if available, radiation therapy represent the most commonly applied treatment options for companion animals. In the meantime, targeted therapies have become indispensable treatment options in human oncology, either as registered therapeutics or as drugs under clinical development. A particularly important change has occurred with regard to implications for the HER-2-positive breast cancer diagnosis in women. HER-2-positivity used to be regarded as an indicator of a bad prognosis (3), however, this evaluation has changed completely in the last 17 years due to the availability of personalized anti-HER-2 therapies that have significantly improved treatment outcomes (1,8,12).
Comparative medicine is systematically revealing more and more similarities in the pathophysiology of a number of diseases, particularly in the comparison between humans and pet animals, such as the example of HER-2-positive mammary tumors in dogs (17–21). This knowledge can be used to gain benefits in each field by simultaneous and thus faster development of novel drugs (72,73).
Since cancer incidence rates are also increasing in veterinary medicine (74), the development of targeted therapies is greatly required. However, simply translating human monoclonal antibodies into veterinary medicine is not an option; they have to be specifically adapted for each species in order to prevent immunogenicity and adverse reactions. Only two antibodies have thus far been ‘caninized’ for use in dog cancer patients (26,27). Therefore, the idea of developing an AAVLP HER-2 mimotope vaccine that induces trastuzumab-like immunoglobulins would be a cost-effective and species-independent alternative, and also of great interest to human oncology. The clinical development of such a novel treatment option for animal patients would gain robust clinical ‘real life’ data with a higher predictive value for translation into human medicine as well.
In conclusion, clinical trials in comparative oncology settings may be of increasing importance in the future, but not only for animals. The trials could provide translational evidence for applications in humans, and allow the fast and efficient verification of novel combinatorial treatments. Anticancer vaccines, such as the AAVLP-HER-2 mimotope approach could be particularly effective; they can be applied independent of species as long as the homology of the target antigen is high, such as in the case of HER-2 and DER-2.
Acknowledgements
The present study was supported by the Austrian Science Fund projects P 23398-B11, by W1205-B09 (doctoral program Cell Communication in Health and Disease), and by Biomedical International R+D GmbH (Vienna, Austria). The authors would like to thank Ms. Amelia Wein (Interuniversity Messerli Research Institute, Vienna, Austria) for proofreading the original manuscript.
Glossary
Abbreviations
- AAV
adeno-associated virus
- AAVLP
AAV-like particle
- DER-2
dog epidermal growth factor receptor-2
- EGFR
epidermal growth factor receptor
- HER-2
human epidermal growth factor receptor-2
References
- 1.Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, Fleming T, Eiermann W, Wolter J, Pegram M, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344:783–792. doi: 10.1056/NEJM200103153441101. [DOI] [PubMed] [Google Scholar]
- 2.Slamon DJ, Godolphin W, Jones LA, Holt JA, Wong SG, Keith DE, Levin WJ, Stuart SG, Udove J, Ullrich A, et al. Studies of the HER-2/neu proto-oncogene in human breast and ovarian cancer. Science. 1989;244:707–712. doi: 10.1126/science.2470152. [DOI] [PubMed] [Google Scholar]
- 3.Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, McGuire WL. Human breast cancer: Correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science. 1987;235:177–182. doi: 10.1126/science.3798106. [DOI] [PubMed] [Google Scholar]
- 4.Tan M, Yao J, Yu D. Overexpression of the c-erbB-2 gene enhanced intrinsic metastasis potential in human breast cancer cells without increasing their transformation abilities. Cancer Res. 1997;57:1199–1205. [PubMed] [Google Scholar]
- 5.Yu D, Hung MC. Overexpression of ErbB2 in cancer and ErbB2-targeting strategies. Oncogene. 2000;19:6115–6121. doi: 10.1038/sj.onc.1203972. [DOI] [PubMed] [Google Scholar]
- 6.Knuefermann C, Lu Y, Liu B, Jin W, Liang K, Wu L, Schmidt M, Mills GB, Mendelsohn J, Fan Z. HER2//PI-3K//Akt activation leads to a multidrug resistance in human breast adenocarcinoma cells. Oncogene. 2003;22:3205–3212. doi: 10.1038/sj.onc.1206394. [DOI] [PubMed] [Google Scholar]
- 7.Hudis CA. Trastuzumab-mechanism of action and use in clinical practice. N Engl J Med. 2007;357:39–51. doi: 10.1056/NEJMra043186. [DOI] [PubMed] [Google Scholar]
- 8.Perez EA, Romond EH, Suman VJ, Jeong JH, Davidson NE, Geyer CE, Jr, Martino S, Mamounas EP, Kaufman PA, Wolmark N. Four-year follow-up of trastuzumab plus adjuvant chemotherapy for operable human epidermal growth factor receptor 2-positive breast cancer: Joint analysis of data from NCCTG N9831 and NSABP B-31. J Clin Oncol. 2011;29:3366–3373. doi: 10.1200/JCO.2011.35.0868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singh JC, Jhaveri K, Esteva FJ. HER2-positive advanced breast cancer: Optimizing patient outcomes and opportunities for drug development. Br J Cancer. 2014;111:1888–1898. doi: 10.1038/bjc.2014.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rimawi MF, Schiff R, Osborne CK. Targeting HER2 for the treatment of breast cancer. Annu Rev Med. 2015;66:111–128. doi: 10.1146/annurev-med-042513-015127. [DOI] [PubMed] [Google Scholar]
- 11.Swain SM, Baselga J, Kim SB, Ro J, Semiglazov V, Campone M, Ciruelos E, Ferrero JM, Schneeweiss A, Heeson S, et al. Pertuzumab, trastuzumab, and docetaxel in HER2-positive metastatic breast cancer. N Engl J Med. 2015;372:724–734. doi: 10.1056/NEJMoa1413513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mukohara T. Role of HER2-targeted agents in adjuvant treatment for breast cancer. Chemother Res Pract. 2011;2011:730360. doi: 10.1155/2011/730360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.deAzambuja E, Holmes AP, Piccart-Gebhart M, Holmes E, Di Cosimo S, Swaby RF, Untch M, Jackisch C, Lang I, Smith I, et al. Lapatinib with trastuzumab for HER2-positive early breast cancer (NeoALTTO): Survival outcomes of a randomised, open-label, multicentre, phase 3 trial and their association with pathological complete response. Lancet Oncol. 2014;15:1137–1146. doi: 10.1016/S1470-2045(14)70320-1. [DOI] [PubMed] [Google Scholar]
- 14.Hahn KA, Ogilvie G, Rusk T, Devauchelle P, Leblanc A, Legendre A, Powers B, Leventhal PS, Kinet JP, Palmerini F, et al. Masitinib is safe and effective for the treatment of canine mast cell tumors. J Vet Intern Med. 2008;22:1301–1309. doi: 10.1111/j.1939-1676.2008.0190.x. [DOI] [PubMed] [Google Scholar]
- 15.London CA, Malpas PB, Wood-Follis SL, Boucher JF, Rusk AW, Rosenberg MP, Henry CJ, Mitchener KL, Klein MK, Hintermeister JG, et al. Multi-center, placebo-controlled, double-blind, randomized study of oral toceranib phosphate (SU11654), a receptor tyrosine kinase inhibitor, for the treatment of dogs with recurrent (either local or distant) mast cell tumor following surgical excision. Clin Cancer Res. 2009;15:3856–3865. doi: 10.1158/1078-0432.CCR-08-1860. [DOI] [PubMed] [Google Scholar]
- 16.Paoloni M, Khanna C. Translation of new cancer treatments from pet dogs to humans. Nat Rev Cancer. 2008;8:147–156. doi: 10.1038/nrc2273. [DOI] [PubMed] [Google Scholar]
- 17.Gamba CO, Dias EJ, Ribeiro LG, Campos LC, Estrela-Lima A, Ferreira E, Cassali GD. Histopathological and immunohistochemical assessment of invasive micropapillary mammary carcinoma in dogs: A retrospective study. Vet J. 2013;196:241–246. doi: 10.1016/j.tvjl.2012.08.022. [DOI] [PubMed] [Google Scholar]
- 18.Ressel L, Puleio R, Loria GR, Vannozzi I, Millanta F, Caracappa S, Poli A. HER-2 expression in canine morphologically normal, hyperplastic and neoplastic mammary tissues and its correlation with the clinical outcome. Res Vet Sci. 2013;94:299–305. doi: 10.1016/j.rvsc.2012.09.016. [DOI] [PubMed] [Google Scholar]
- 19.Muhammadnejad A, Keyhani E, Mortazavi P, Behjati F, Haghdoost IS. Overexpression of her-2/neu in malignant mammary tumors; translation of clinicopathological features from dog to human. Asian Pac J Cancer Prev. 2012;13:6415–6421. doi: 10.7314/APJCP.2012.13.12.6415. [DOI] [PubMed] [Google Scholar]
- 20.Kim JH, Im KS, Kim NH, Yhee JY, Nho WG, Sur JH. Expression of HER-2 and nuclear localization of HER-3 protein in canine mammary tumors: Histopathological and immunohistochemical study. Vet J. 2011;189:318–322. doi: 10.1016/j.tvjl.2010.08.012. [DOI] [PubMed] [Google Scholar]
- 21.Singer J, Weichselbaumer M, Stockner T, Mechtcheriakova D, Sobanov Y, Bajna E, Wrba F, Horvat R, Thalhammer JG, Willmann M, Jensen-Jarolim E. Comparative oncology: ErbB-1 and ErbB-2 homologues in canine cancer are susceptible to cetuximab and trastuzumab targeting. Mol Immunol. 2012;50:200–209. doi: 10.1016/j.molimm.2012.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peña L, Gama A, Goldschmidt MH, Abadie J, Benazzi C, Castagnaro M, Díez L, Gärtner F, Hellmén E, Kiupel M, et al. Canine mammary tumors: A review and consensus of standard guidelines on epithelial and myoepithelial phenotype markers, HER2, and hormone receptor assessment using immunohistochemistry. Vet Pathol. 2014;51:127–145. doi: 10.1177/0300985813509388. [DOI] [PubMed] [Google Scholar]
- 23.Pichler WJ. Adverse side-effects to biological agents. Allergy. 2006;61:912–920. doi: 10.1111/j.1398-9995.2006.01058.x. [DOI] [PubMed] [Google Scholar]
- 24.Corominas M, Gastaminza G, Lobera T. Hypersensitivity reactions to biological drugs. J Investig Allergol Clin Immunol. 2014;24:212–225. [PubMed] [Google Scholar]
- 25.Baldo BA. Adverse events to monoclonal antibodies used for cancer therapy: Focus on hypersensitivity responses. Oncoimmunology. 2013;2:e26333. doi: 10.4161/onci.26333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Singer J, Fazekas J, Wang W, Weichselbaumer M, Matz M, Mader A, Steinfellner W, Meitz S, Mechtcheriakova D, Sobanov Y, et al. Generation of a canine anti-EGFR (ErbB-1) antibody for passive immunotherapy in dog cancer patients. Mol Cancer Ther. 2014;13:1777–1790. doi: 10.1158/1535-7163.MCT-13-0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rue SM, Eckelman BP, Efe JA, Bloink K, Deveraux QL, Lowery D, Nasoff M. Identification of a candidate therapeutic antibody for treatment of canine B-cell lymphoma. Vet Immunol Immunopathol. 2015;164:148–159. doi: 10.1016/j.vetimm.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 28.Jensen-Jarolim E, Singer J. Cancer vaccines inducing antibody production: More pros than cons. Expert Rev Vaccines. 2011;10:1281–1289. doi: 10.1586/erv.11.105. [DOI] [PubMed] [Google Scholar]
- 29.Milani A, Sangiolo D, Montemurro F, Aglietta M, Valabrega G. Active immunotherapy in HER2 overexpressing breast cancer: Current status and future perspectives. Ann Oncol. 2013;24:1740–1748. doi: 10.1093/annonc/mdt133. [DOI] [PubMed] [Google Scholar]
- 30.Anderson KS. Tumor vaccines for breast cancer. Cancer Invest. 2009;27:361–368. doi: 10.1080/07357900802574421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sears AK, Perez SA, Clifton GT, Benavides LC, Gates JD, Clive KS, Holmes JP, Shumway NM, Van Echo DC, Carmichael MG, et al. AE37: A novel T-cell-eliciting vaccine for breast cancer. Expert Opin Biol Ther. 2011;11:1543–1550. doi: 10.1517/14712598.2011.616889. [DOI] [PubMed] [Google Scholar]
- 32. NCT01730118, corp-author. https://clinicaltrials.gov/ Ad/HER2/Neu dendritic cell cancer vaccine testing. 2015 Aug 31; Accessed.
- 33.Knittelfelder R, Riemer AB, Jensen-Jarolim E. Mimotope vaccination-from allergy to cancer. Expert Opin Biol Ther. 2009;9:493–506. doi: 10.1517/14712590902870386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ashok BT, David L, Chen YG, Garikapaty VP, Chander B, Kanduc D, Mittelman A, Tiwari RK. Peptide mimotopes of oncoproteins as therapeutic agents in breast cancer. Int J Mol Med. 2003;11:465–471. doi: 10.3892/ijmm.11.4.465. [DOI] [PubMed] [Google Scholar]
- 35.Riemer AB, Kurz H, Klinger M, Scheiner O, Zielinski CC, Jensen-Jarolim E. Vaccination with cetuximab mimotopes and biological properties of induced anti-epidermal growth factor receptor antibodies. J Natl Cancer Inst. 2005;97:1663–1670. doi: 10.1093/jnci/dji373. [DOI] [PubMed] [Google Scholar]
- 36.Riemer AB, Kraml G, Scheiner O, Zielinski CC, Jensen-Jarolim E. Matching of trastuzumab (Herceptin) epitope mimics onto the surface of Her-2/neu-a new method of epitope definition. Mol Immunol. 2005;42:1121–1124. doi: 10.1016/j.molimm.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 37.Riemer AB, Klinger M, Wagner S, Bernhaus A, Mazzucchelli L, Pehamberger H, Scheiner O, Zielinski CC, Jensen-Jarolim E. Generation of Peptide mimics of the epitope recognized by trastuzumab on the oncogenic protein Her-2/neu. J Immunol. 2004;173:394–401. doi: 10.4049/jimmunol.173.1.394. [DOI] [PubMed] [Google Scholar]
- 38.Manzano-Szalai K, Thell K, Willensdorfer A, Weghofer M, Pfanzagl B, Singer J, Ritter M, Stremnitzer C, Flaschberger I, Michaelis U, Jensen-Jarolim E. Adeno-associated virus-like particles as new carriers for B-cell vaccines: Testing immunogenicity and safety in BALB/c mice. Viral Immunol. 2014;27:438–448. doi: 10.1089/vim.2014.0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Singer J, Manzano-Szalai K, Fazekas J, Thell K, Bentley-Lukschal A, Stremnitzer C, Roth-Walter F, Weghofer M, Ritter M, Tossi KP, et al. Proof of concept study with a HER-2 mimotope anti-cancer vaccine deduced from a novel AAV-mimotope library platform. Oncoimmunology. 2016:e1171446. doi: 10.1080/2162402X.2016.1171446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Valicsek E, Kószó R, Dobi Á, Uhercsák G, Varga Z, Vass A, Jebelovszky É, Kahán Z. Cardiac surveillance findings during adjuvant and palliative trastuzumab therapy in patients with breast cancer. Anticancer Res. 2015;35:4967–4973. [PubMed] [Google Scholar]
- 41.Dobson JM, Samuel S, Milstein H, Rogers K, Wood JL. Canine neoplasia in the UK: Estimates of incidence rates from a population of insured dogs. J Small Anim Pract. 2002;43:240–246. doi: 10.1111/j.1748-5827.2002.tb00066.x. [DOI] [PubMed] [Google Scholar]
- 42.Arnold-Gloor S, Hubler M, Reichler I. Diseases of the mammary gland. In: Suter PF, Arnold-Gloor S, Niemand HG, editors. Placement of teh dog clinic. Parey; Stuttgart: 2006. pp. 881–883. (In German) [Google Scholar]
- 43.Baba AI, Câtoi C, Baba AI. Mammary gland tumours-comparative oncology. The publishing house of the Romanian academy; Bucharest: 2007. p. 1. online resource. Accessed August 31, 2015. [PubMed] [Google Scholar]
- 44.Sorenmo K. Canine mammary gland tumors. Vet Clin North Am Small Anim Pract. 2003;33:573–596. doi: 10.1016/S0195-5616(03)00020-2. [DOI] [PubMed] [Google Scholar]
- 45.Novosad CA. Principles of treatment for mammary gland tumors. Clin Tech Small Anim Pract. 2003;18:107–109. doi: 10.1053/svms.2003.36625. [DOI] [PubMed] [Google Scholar]
- 46.Queiroga FL, Raposo T, Carvalho MI, Prada J, Pires I. Canine mammary tumours as a model to study human breast cancer: Most recent findings. In vivo. 2011;25:455–465. [PubMed] [Google Scholar]
- 47.de Las Mulas JM, Millán Y, Dios R. A prospective analysis of immunohistochemically determined estrogen receptor alpha and progesterone receptor expression and host and tumor factors as predictors of disease-free period in mammary tumors of the dog. Vet Pathol. 2005;42:200–212. doi: 10.1354/vp.42-2-200. [DOI] [PubMed] [Google Scholar]
- 48.Queiroga FL, Pérez-Alenza MD, Silvan G, Peña L, Lopes C, Illera JC. Role of steroid hormones and prolactin in canine mammary cancer. J Steroid Biochem Mol Biol. 2005;94:181–187. doi: 10.1016/j.jsbmb.2004.12.014. [DOI] [PubMed] [Google Scholar]
- 49.Torres CG, Pino AM, Sierralta WD. A cyclized peptide derived from alpha fetoprotein inhibits the proliferation of ER-positive canine mammary cancer cells. Oncol Rep. 2009;21:1397–1404. doi: 10.3892/or_00000367. [DOI] [PubMed] [Google Scholar]
- 50.Wakui S, Muto T, Yokoo K, Yokoo R, Takahashi H, Masaoka T, Hano H, Furusato M. Prognostic status of p53 gene mutation in canine mammary carcinoma. Anticancer Res. 2001;21:611–616. [PubMed] [Google Scholar]
- 51.Lee CH, Kweon OK. Mutations of p53 tumor suppressor gene in spontaneous canine mammary tumors. J Vet Sci. 2002;3:321–325. [PubMed] [Google Scholar]
- 52.Carvalho MI, Pires I, Prada J, Queiroga FL. A role for T-lymphocytes in human breast cancer and in canine mammary tumors. Biomed Res Int. 2014;2014:130894. doi: 10.1155/2014/130894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Haga S, Nakayama M, Tatsumi K, Maeda M, Imai S, Umesako S, Yamamoto H, Hilgers J, Sarkar NH. Overexpression of the p53 gene product in canine mammary tumors. Oncol Rep. 2001;8:1215–1219. doi: 10.3892/or.8.6.1215. [DOI] [PubMed] [Google Scholar]
- 54.Tao JJ, Visvanathan K, Wolff AC. Long term side effects of adjuvant chemotherapy in patients with early breast cancer. Breast. 2015;24(Suppl 2):S149–S153. doi: 10.1016/j.breast.2015.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bracha S, Walshaw R, Danton T, Holland S, Ruaux C, Obradovich J. Evaluation of toxicities from combined metronomic and maximal-tolerated dose chemotherapy in dogs with osteosarcoma. J Small Anim Pract. 2014;55:369–374. doi: 10.1111/jsap.12228. [DOI] [PubMed] [Google Scholar]
- 56.Selmic LE, Burton JH, Thamm DH, Withrow SJ, Lana SE. Comparison of carboplatin and doxorubicin-based chemotherapy protocols in 470 dogs after amputation for treatment of appendicular osteosarcoma. J Vet Intern Med. 2014;28:554–563. doi: 10.1111/jvim.12313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Stratmann N, Failing K, Richter A, Wehrend A. Mammary tumor recurrence in bitches after regional mastectomy. Vet Surg. 2008;37:82–86. doi: 10.1111/j.1532-950X.2007.00351.x. [DOI] [PubMed] [Google Scholar]
- 58.Betz D, Schoenrock D, Mischke R, Baumgärtner W, Nolte I. Postoperative treatment outcome in canine mammary tumors. Multivariate analysis of the prognostic value of pre- and postoperatively available information. Tierarztl Prax Ausg K Kleintiere Heimtiere. 2012;40:235–242. (In English, German) [PubMed] [Google Scholar]
- 59.Hay M, Thomas DW, Craighead JL, Economides C, Rosenthal J. Clinical development success rates for investigational drugs. Nat Biotechnol. 2014;32:40–51. doi: 10.1038/nbt.2786. [DOI] [PubMed] [Google Scholar]
- 60.Marchetti S, Schellens JH. The impact of FDA and EMEA guidelines on drug development in relation to Phase 0 trials. Br J Cancer. 2007;97:577–581. doi: 10.1038/sj.bjc.6603925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Stapff M. Drug trials: An introduction to clinical trials for doctors, students, medical assistants and interested laymen. 5th. Zuckschwerdt; Munich: 2008. [Google Scholar]
- 62.Directive 2010/63/EU, corp-author. eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2010:276:0033:0079:en:PDF. Directive 2010/63/EU of the European Parliament and of the Council of 22 September 2010 on the protection of animals used for scientific purposes. 2010 Accessed May 17, 2016.
- 63.eur-lex.europa.eu/legalcontent/EN/TXT/?uri=celex%3A32010L0063. ICH-GCP: ICH Topic E6 (R1) Guideline for Good Clinical Practice. 2002 European Medicines Agency. Accessed August 31, 2015.
- 64.clinicaltrials.gov. U.S. National Library of Medicine: Clinical Trial Phases. 2015 National Institutes of Health. Accessed August 31, 2015.
- 65.Ciociola AA, Cohen LB, Kulkarni P. FDA-Related Matters Committee of the American College of Gastroenterology: How drugs are developed and approved by the FDA: Current process and future directions. Am J Gastroenterol. 2014;109:620–623. doi: 10.1038/ajg.2013.407. [DOI] [PubMed] [Google Scholar]
- 66.Khanna C, London C, Vail D, Mazcko C, Hirschfeld S. Guiding the optimal translation of new cancer treatments from canine to human cancer patients. Clin Cancer Res. 2009;15:5671–5677. doi: 10.1158/1078-0432.CCR-09-0719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Monath TP, Kahn LH, Kaplan B. Introduction: One health perspective. ILAR J. 2010;51:193–198. doi: 10.1093/ilar.51.3.193. [DOI] [PubMed] [Google Scholar]
- 68.Séveré S, Marchand P, Guiffard I, Morio F, Venisseau A, Veyrand B, Le Bizec B, Antignac JP, Abadie J. Pollutants in pet dogs: A model for environmental links to breast cancer. Springerplus. 2015;4:27. doi: 10.1186/s40064-015-0790-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kelsey JL, Moore AS, Glickman LT. Epidemiologic studies of risk factors for cancer in pet dogs. Epidemiol Rev. 1998;20:204–217. doi: 10.1093/oxfordjournals.epirev.a017981. [DOI] [PubMed] [Google Scholar]
- 70.Hansen K, Khanna C. Spontaneous and genetically engineered animal models; use in preclinical cancer drug development. Eur J Cancer. 2004;40:858–880. doi: 10.1016/j.ejca.2003.11.031. [DOI] [PubMed] [Google Scholar]
- 71.Fürdös I, Fazekas J, Singer J, Jensen-Jarolim E. Translating clinical trials from human to veterinary oncology and back. J Transl Med. 2015;13:265. doi: 10.1186/s12967-015-0631-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jensen-Jarolim E, editor. Comparative Medicine. Anatomy and Physiology. Springer; Wien: 2014. Definition of comparative medicine: History and new identity; pp. 1–18. [Google Scholar]
- 73.Singer J, Jensen-Jarolim E. IgE-based immunotherapy of cancer-a comparative oncology approach. J Carcinog Mutagen. 2014;5:1000176. doi: 10.4172/2157-2518.1000176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Merlo DF, Rossi L, Pellegrino C, Ceppi M, Cardellino U, Capurro C, Ratto A, Sambucco PL, Sestito V, Tanara G, Bocchini V. Cancer incidence in pet dogs: Findings of the Animal Tumor Registry of Genoa, Italy. J Vet Intern Med. 2008;22:976–984. doi: 10.1111/j.1939-1676.2008.0133.x. [DOI] [PubMed] [Google Scholar]