Abstract
Background
The Decision-Making Capacity Assessment (DMCA) Model includes a best-practice process and tools to assess DMCA, and implementation strategies at the organizational and assessor levels to support provision of DMCAs across the care continuum. A Developmental Evaluation of the DMCA Model was conducted.
Methods
A mixed methods approach was used. Survey (N = 126) and focus group (N = 49) data were collected from practitioners utilizing the Model.
Results
Strengths of the Model include its best-practice and implementation approach, applicability to independent practitioners and inter-professional teams, focus on training/mentoring to enhance knowledge/skills, and provision of tools/processes. Post-training, participants agreed that they followed the Model’s guiding principles (90%), used problem-solving (92%), understood discipline-specific roles (87%), were confident in their knowledge of DMCAs (75%) and pertinent legislation (72%), accessed consultative services (88%), and received management support (64%). Model implementation is impeded when role clarity, physician engagement, inter-professional buy-in, accountability, dedicated resources, information sharing systems, and remuneration are lacking. Dedicated resources, job descriptions inclusive of DMCAs, ongoing education/mentoring supports, access to consultative services, and appropriate remuneration would support implementation.
Conclusions
The DMCA Model offers practitioners, inter-professional teams, and organizations a best-practice and implementation approach to DMCAs. Addressing barriers and further contextualizing the Model would be warranted.
Keywords: capacity, competency, decision-making, cognitive decline, older adults, capacity assessment, capacity assessment model, evaluation
INTRODUCTION
Adults with diseases and disabilities contend with barriers that can challenge their autonomy and ability to live independently.(1,2) One barrier can be an inability to make decisions in domains such as health care, place of residence, finances, choice of associates, legal matters, and participation in social, educational or employment activities.(3) As Canadians age, and the incidence both of chronic health conditions rises and dementia-related diseases potentially doubles (by 2038 to one million),(4) more individuals are likely to experience challenges regarding decision-making capacity (DMC).
Reflective of current literature and practice,(5–12) capacity is “the ability to understand and express choices, appreciate the consequences of different options, and follow through (or direct a surrogate) with chosen options” (see Pachet et al.(13) p. 439). A person’s DMC—ranging from capable to incapable—is domain-specific and dependent on the complexity of the decision-making process, one’s ability to engage in that process, and risk(s) associated with the decision;(5–12) it can also vary over time and as a result of disease processes, cognitive impairment, or brain injury.(14–17) Understandings of capacity as a socio-legal construct vary across jurisdictions,(5,12) and its assessment is informed by provincial and national legislation.(5,18,19)
Assessment of DMC is a complex practice area requiring knowledge of bio-psycho-social factors, ethics, and the law,(20) in the absence of which inappropriate or unnecessary decision-making capacity assessments (DMCAs) can occur. Due to a lack of agreement between assessors or within families, unwarranted declarations of incapacity and legal challenges can result. To mitigate this risk, access is needed to standardized DMCAs conducted by competent assessors working independently or on inter-professional (IP) teams who follow best-practices aligned with local legislation.
Models for Assessing Decision-Making Capacity
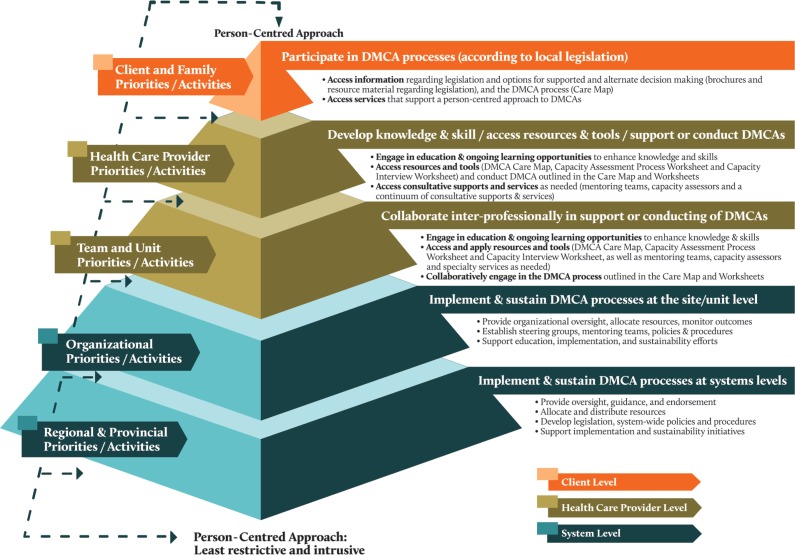
Literature regarding DMCAs has focused on the development of models/frameworks. Skelton et al.(21) developed a capacity assessment and intervention model that uses common assessment methods and a standardized process. Moye and colleagues’ conceptual model and evaluation template(20) offers a cross-jurisdictional approach to conducting and documenting DMCAs. The Regional Capacity Assessment Team (RCAT) Model(13) is an assessment and consultation model. The American Bar Association and American Psychological Association provide a framework and practice examples.(22) Best practices for complex medico-legal-ethical situations are outlined in provincial guidelines and legislation such as those in Ontario,(9) the Yukon,(10) and Alberta.(23,24,25) While the aforementioned resources offer valuable approaches to conducting DMCAs, lacking is a model that outlines best-practice processes and tools, as well as an implementation strategy to enhance the capacity of health-care professionals (HCPs) and systems to integrate and implement the best-practice process. A DMCA Model developed in Alberta has begun to address this gap through its best-practice process and tools, and implementation approach (see Figure 1).
FIGURE 1.
DMCA Model: a best-practice process and implementation approach
Development of the DMCA Model (described in Parmar et al.(26,27)) by an acute care IP team began in 2006. Aiming to improve the quality of DMCAs and reduce unnecessary declarations of incapacity, a well-defined, standardized process and supporting tools were developed and trialed. As development of the Model and the province’s Adult Guardian and Trusteeship Act (AGTA)(25) governing DMCAs coincided, the two are closely aligned, with the Model supporting operationalization of the capacity assessment process in the AGTA. It has since been utilized by independent practitioners, and IP teams in Calgary and Edmonton (serving 65% of Albertans),(28) and continues to be developed and adapted for use across the continuum of care and service sectors.
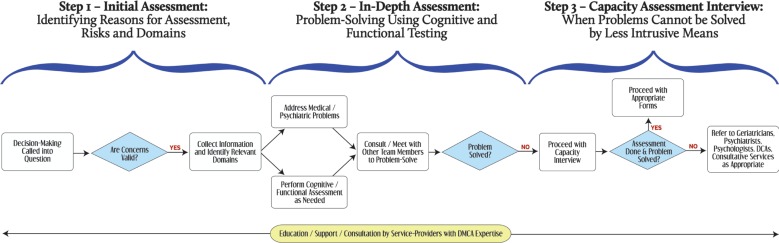
The DMCA Model offers a best-practice process to assess DMCAs at the client level, and implementation strategies at the system and HCP levels to enhance capacity to provide DMCAs (see Figure 1). At the system level, oversight and guidance is provided by senior leaders; where indicated, mentoring teams (MTs: HCPs with expertise in DMCAs available for education/consultation) are identified; the Model is adapted for the particular context; clinical pathways, policies and procedures are developed; resources are allocated; roles and responsibilities are clarified; and implementation and sustainability initiatives are supported. Health-care professionals with DMCA expertise provide education/training and mentorship to HCPs, and offer consultation for more complex cases. HCPs, after receiving DMCA education/training, support or conduct DMCAs, utilizing the best-practice process outlined in the Care Map (see Figure 2) and worksheets/documentation resources.(26)
FIGURE 2.
DMCA Model Care Map
The DMC best-practice assessment process begins with identification and validation of reasons for the DMCA of a client in a specific domain(s). Relevant information is then collected, reversible medical conditions addressed, and social, cognitive, functional and/or psychological assessments are conducted. If the client is medically stable, least intrusive/restrictive options are sought. When less intrusive means cannot be found through problem-solving and a declaration of incapacity is thought to be required, a Capacity Assessment Interview is undertaken. Experts (physicians, geriatricians, psychologists, psychiatrists, designated capacity assessors (DCAs: court-appointed assessors with social work, nursing or occupational therapy backgrounds)) and specialty services are consulted for more complex cases.
Developmental Evaluation of the DMCA Model
This study presents the results of a Developmental Evaluation(29,30,31) of the Model. Conducted in collaboration with primary users, this evaluation includes real-time data gathering to inform development of the Model. As provincial policy and decision-makers are interested in the Model’s appropriateness for widespread use, and experienced clinicians were able to speak to its utility and recommendations for further develop, this form of evaluation was deemed appropriate. The following research questions guided the study: 1) How has the Model been used? 2) What are advantages of and barriers to implementation/use of the Model? 3) How might the Model be further developed? and 4) Can it be widely used by HCPs working independently or on IP teams?
METHODS
Study Design
This evaluation applied a mixed methods approach;(32) focused ethnography(33,34) guided data collection and analysis. HCPs and key stakeholders familiar with the Model were invited to either participate in one of two day-long evaluation workshops held in Edmonton and Calgary that included focus groups (FGs) and a survey, or to complete only the survey. Workshop participants were recruited through invitations distributed by members of advisory and steering committees; surveys were likewise distributed via e-mail and paper copy to HCPs and key stakeholders who were unable to attend the workshops.
Qualitative Data Collection
Qualitative data were collected through FGs and open-ended survey items. HCPs were asked about the Model’s use, strengths and limitations, effectiveness in guiding DMCAs, recommendations for improvement, and the role of MTs and DCAs. Facilitators used a script developed by the research team to lead open-ended discussions. FGs were audio-recorded and transcribed by professional transcriptionists. QSR NVivo 9 qualitative data analysis softwareQSR(35) was used to store, manage and organize data. Transcripts were coded by the research team using Roper and Shapira’s(36) framework for data analysis, including coding for themes and descriptive labels, and sorting to identify patterns and outliers, and generalize constructs.
Quantitative Data Collection
A 22-question survey was distributed via e-mail attachment and a Fluid Survey(37) link to HCPs attending the workshops, as well as those unable to attend. The purpose of the survey was to capture descriptive data and participant perceptions of Model utilization. (See Appendix 1 for survey questions). Workshop participants completed the survey on the day of the workshop; those not able to attend completed and returned the survey within three weeks of receipt, either through the Fluid Survey link or by fax.
Participants
Members of attending teams (ATs: frontline, direct care teams), MTs, and DCAs from sites in Edmonton and Calgary in which the Model had been implemented participated in the evaluation. While the research team was not privy to e-mail distribution lists due to confidentiality, and therefore the total number of individuals to whom the invitation(s) was extended is unknown, the number of participants in attendance at the evaluation workshop and survey respondents exceeded expectations. Workshop attendees participated in FGs (n = 49) and completed a survey (n = 46) (see Table 1 for geographical distribution/profession of participants, and Table 2 for FG topics and number of participants), while other participants completed the survey only (n = 80). Survey participants (N = 126, 90% female) were employed at different facilities/agencies, represented diverse professions/roles, and ranged in age (20–64 years) and years of professional practice (16+ (41%), 6–15 (40%), 0–5 (19%) years).
TABLE 1.
Study participant: geographic distribution and profession/occupation
| Item | Evaluation Workshop: Focus Group Participants | Evaluation Workshop: Number of Focus Groups | Evaluation Workshop SurveyRespondents | Respondents Survey Only | Total Survey Respondents |
|---|---|---|---|---|---|
| (N=49) % (N) | (Participants per focus group) | (N=46) % (N) | (N=80) % (N) | (N=126) % (N) | |
| Zone | |||||
| Edmonton | 67 (33) | 15 (2–7) | 67 (31) | 49 (39) | 56 (70) |
| Calgary | 33 (16) | 9 (2–5) | 33 (15) | 44 (35) | 40 (50) |
| Unspecified | 0 | 0 | 0 | 4 (3) | 2 (3) |
| Missing | 0 | 0 | 0 | 4 (3) | 2 (3) |
| Professional designation/occupation | |||||
| Nurse | 24.5 (12) | 0 | 26 (12) | 36 (29) | 33 (41) |
| Social Worker | 35 (17) | 0 | 37 (17) | 19 (15) | 25 (32) |
| Occupational Therapist | 24.5 (12) | 0 | 26 (12) | 16 (13) | 20 (25) |
| Psychologist | 6 (3) | 0 | 7 (3) | 0 | 2 (3) |
| Physician | 0 | 0 | 0 | 5 (4) | 3 (4) |
| Physiotherapist | 0 | 0 | 0 | 4 (3) | 2 (3) |
| Program Manager/Unit Supervisor/Administrator | 0 | 0 | 0 | 14 (11) | 9 (11) |
| Care or Transition Coordinator/Director | 0 | 0 | 0 | 6 (5) | 4 (5) |
| Unspecified | 6 (3) | 0 | 0 | 0 | 0 |
| Other (consultant, education coordinator) | 4 (2) | 0 | 4 (2) | 0 | 2 (2) |
TABLE 2.
Focus groups: topics and number of participants
| Focus Group Topics: |
Focus Group #1: Model’s use, strengths, limitations, effectiveness in guiding DMCAs Focus Groups (N=10) Participants (N=45) |
Focus Group #2: Recommendations for improvement of the DMCA Model Focus Groups (N=10) Participants (N=46) |
Focus Group #3: Role of Mentoring Teams and Designated Capacity Assessors Focus Groups (N=4) Participants (N=18) |
|---|---|---|---|
| Calgary | Focus Groups (n=4) | Focus Groups (n=4) | Focus Groups (n=1) |
| Participants (n=16) | Participants (n=15) | Participants (n=5) | |
| Number of Participants: | Number of Participants: | Number of Participants: | |
| Facilitator 1 | 5 | 2 | 0 |
| Facilitator 2 | 3 | 5 | 0 |
| Facilitator 3 | 4 | 4 | 0 |
| Facilitator 4 | 4 | 4 | 5 |
| Edmonton | Focus Groups (n=6) | Focus Groups (n=6) | Focus Groups (n=3) |
| Participants (n=29) | Participants (n=31) | Participants (n=13) | |
| Number of Participants: | Number of Participants: | Number of Participants: | |
| Facilitator 1 | 5 | 6 | 5 |
| Facilitator 2 | 7 | 3 | 6 |
| Facilitator 3 | 5 | 5 | 2 |
| Facilitator 4 | 4 | 5 | 0 |
| Facilitator 5 | 4 | 6 | 0 |
| Facilitator 6 | 4 | 6 | 0 |
Ethics
Ethical review was completed by the University of Alberta’s Health Research Ethics Board (Panel B) and from the Conjoint Health Research Ethics Board, Office of Medical Ethics, and the University of Calgary. Operational approval was obtained from participating site. Participants signed consent forms prior to participation in FGs.
RESULTS
Quantitative Findings
Survey results indicated that 92% of respondents felt that they were reducing risks to clients when following the Model, 90% reported that they followed the Model’s guiding principles, 78% followed the Model in their workplace, 87% indicated that they understood their discipline-specific role, 75% were confident in their knowledge and skills, 72% were confident in their knowledge about applicable legislation, 74% noted that they had opportunities to attend learning sessions, 59% indicated that the DMCA process improved the efficiency and effectiveness of DMCAs, 44% suggested that the Model has reduced angst/conflicts regarding DMCA issues, 64% reported receiving management support, and 88% had access to assistance from a MT (see Table 3).
TABLE 3.
Survey results (quantitative findings)
| Survey Theme and Item | Survey Item # | Responses (N) | Strongly Disagree % (N) | Disagree % (N) | Agree % (N) | Strongly Agree % (N) | Do Not Know % (N) |
|---|---|---|---|---|---|---|---|
| Use of Model | |||||||
| The new DMCA model is followed in my workplace | 1 | 126 | 3 (4) | 10 (13) | 55 (73) | 23 (29) | 6 (7) |
| I follow the guiding principles of DMCA when I am faced with concerns about a patient’s decision making capacity | 2 | 125 | 2 (3) | 3 (4) | 48 (60) | 42 (53) | 6 (7) |
| When a capacity concern is identified in a patient, I and/or my team member (s) will use the “Capacity Assessment Worksheet” to guide our work | 4 | 126 | 3 (4) | 17 (22) | 49 (62) | 22 (28) | 8 (10) |
| I and/or my team members(s) will explore problem solving opportunities in order to reduce the risk to the patient before suggesting a capacity interview | 6 | 124 | 2 (3) | 3 (4) | 44 (55) | 48 (59) | 5 (6) |
| Training Knowledge, Skill | |||||||
| I am confident in my knowledge about legislation as it applies to DMCA | 3 | 124 | 2 (3) | 23 (29) | 55 (68) | 17 (21) | 2 (3) |
| I understand the role of my discipline in DMCA and the part I play in the interdisciplinary approach to assessment | 5 | 126 | 2 (3) | 9 (11) | 45 (57) | 42 (53) | 2 (3) |
| I am confident in my knowledge and skills regarding DMCA and comfortable being involved in these assessments | 7 | 126 | 2 (2) | 17 (22) | 52 (66) | 23 (29) | 6 (8) |
| I have had the opportunity to attend ongoing learning sessions that provide further information and support for the implementation of DMCA | 11 | 124 | 3 (4) | 21 (26) | 51 (63) | 23 (28) | 4 (5) |
| Impact of the Model | |||||||
| The capacity assessment model has reduced the angst/conflicts among staff, patients, and families when dealing with issues related to DMCA | 8 | 125 | 2 (2) | 24 (30) | 38 (48) | 6 (8) | 30 (38) |
| The standardized process for DMCA has improved the efficiency and effectiveness of capacity assessments performed by my team | 10 | 124 | 2 (3) | 14 (17) | 47 (58) | 12 (15) | 25 (31) |
| System Supports | |||||||
| A Capacity Assessment Mentoring Team is available to assist our team with questions and to provide support about DMCA | 9 | 126 | 3 (4) | 7 (9) | 51 (64) | 37 (46) | 4 (5) |
| I and my team receive the necessary management support to implement the model for DMCA | 12 | 123 | 3 (4) | 20 (25) | 54 (66) | 10 (12) | 13 (16) |
Qualitative Findings
Three main themes emerged from qualitative data analysis: facilitators of Model implementation/use, barriers to Model implementation/use, and recommendations for future development of the Model. Qualitative themes are presented below, with a sample of supporting quotes included in Tables 4–7.
TABLE 4.
Benefits of the DMCA model (qualitative findings)
| Themes | Quotes |
|---|---|
| a. Person- and family-centred approach | “It is very client-centered; it helps us do a good job being client-centered and focusing on what our patients want.” “With families it helps because now we have a process we can lay out for them.” “We’re looking at the clients’ domains individually as opposed to just throwing a blanket on everything.” |
| b. Aligns with legislation | “The Model ties into legislation beautifully.” |
| c. Supports a culture shift | “I think it’s certainly raised awareness.” “Was really getting us to re-conceptualize our whole area of practice around this clinical issue…it’s a cultural shift.” |
| d. Builds capacity through education | “The strength of this Model is that it requires that you educate.” “It has been really useful to get so many of the staff through this training process, using the right terminology and understanding what domains are.” “The strength of this Model is that you create teaching moments with families.” |
| e. Facilitates collaboration | “It’s interdisciplinary … it’s a shared responsibility; brings the entire multidisciplinary team together to look at capacity assessment;” “It ensures that the team does due diligence in taking a least intrusive approach.” |
| f. Provides a clear, consistent, time-saving best practice process | “It guides us to do more critical and creative thinking around decisions of capacity”; “It provides a consistent structure; … a step-wise process about whether or not these people actually need a capacity assessment”; “The care map is good for people to understand the process, the three steps.” “[Worksheets] provided the multidisciplinary team a spot to write down their thoughts.” “It actually really speeded up the entire capacity assessment process.” “It decreases staff time and anxiety.” |
| g. Supports full scope of practice | “There’s a lot more mentoring and things that you need to learn in order to have that scope of practice.” |
| h. Eliminates unnecessary capacity assessments | “The majority of the time [the person] actually didn’t need a capacity assessment by the time we actually problem solved through it.” |
TABLE 5.
Factors facilitating DMCA implementation (qualitative findings)
| Themes | Quotes |
|---|---|
| a. Model is aligned with person and family-centred priorities | “Seeing the person as a whole benefits the patient.” |
| b. Involvement of staff across the system | “The best thing about this process was having the wide range of people involved, the networks, like, helpful for us to be building connections across the hospital, which is what makes a difference, and having people who are close to the front lines.” |
| c. Leadership buy-in/dedicated resources | “I’m astounded at the support from administration, especially considering that it’s costing money – whether it’s keeping patients in hospital to get the assessment done or the time for Mentoring Team meetings.” |
| d. Dedicated champions | “Particular champions. A physician specialist who has respect among physicians so that there’s buy-in. You need one in nursing; and one on a particular unit.” “The right people can help push this forward.” |
| e. Training and mentoring | “There was a lot of momentum; lots of people were coming to the workshops; we could hardly keep up with the amount of people that wanted to know this information.” “In the community, what has been good and creates accountability is people meeting once a month to discuss capacity issues. It also makes champions on different units.” “If there wasn’t a mentoring team, DCA or CARP [Capacity Assessment Resource Person], I don’t know how these care providers could reasonably develop.” |
| f. Tools and worksheets | “The real essence of this clinical protocol was the conversations around the worksheet; we took a case example and worked through that worksheet. It’s been a tremendous amount of learning for us.” |
| g. Legislation and guiding principles | “Every part of the process echoes the legislation, from the guiding principles and the presumption of capacity right to the very end. You’re accountable to the legislation.” |
TABLE 6.
Barriers to implementation/use of the DMCA model (qualitative findings)
| Themes | Quotes |
|---|---|
| a. Lack of resources and time | “Employees should not be expected to provide services “free of charge” and “off the side of their desks”.” “Proper classification for the work and proper remuneration is lacking.” “As a part-time employee, it’s difficult to complete interviews in a timely manner.” |
| b. Lack of role clarity | “Disciplines are not on the same page about whether an assessment is needed.” “I think most of the workload falls on social work and rehabilitation.” “Some of the medical teams do not understand the process, have low risk tolerance, are uncomfortable with problem solving, and jump straight into the capacity assessment despite our recommendations.” “Workload is additional; it takes away from other roles. So either you don’t perform as good a jobassessing, or another role suffers.” |
| c. Lack of buy-in/accountability | “OT and SW seem to be the only disciplines doing the assessments, thereby increasing OT and SW workload.” “Poor physician buy-in; they don’t seem to understand the process.” “Physicians and psychiatrists are quick to consult, though issues can be solved by the team.” “Nursing reluctance to participate in the process.” “Lack of administration support and understanding.” “There’s no accountability. It became someone else’s problem.” |
| d. Insufficient organizational processes and inter-organizational collaboration | “Time and comfort with the documentation; staff already have so much paperwork; filling out the worksheet increases OT and SW workload; the signature on the form: every team member to sign or just the lead?” “Logistical problems on the unit: location of forms, time dedicated to filling it out, determination of who’s putting the form on the chart.” “We need to formalize and break down silos. How can programs communicate?” |
| e. Knowledge gaps | “It’s an ongoing battle to keep the education up.” “The 4-hour orientations stopped.” “It’s problematic that not ALL key team members have attended the training.” “Not all staff are aware of or comfortable in starting the process.” “The staff are not confident in the process, and when to get a DCA involved.” |
TABLE 7.
Recommendations for DMCA model (qualitative findings)
| Themes | Quotes |
|---|---|
| Client Level | |
| a. Support person and family-centred care | “Maintain a problem-solving approach and see the person as a whole.” “Spend time with a family, and reassure them that you are following a process.” “Be proactive so as to decrease time spent on some of the other processes later.” “Ensure professional/respectful service that protects the legal rights of the individual.” |
| Health-care Professional Level | |
| a. Enhance education and mentoring opportunities | “Continued education and promotion of the Model for everyone, beginning with managers, case managers, educators, hospitalists, MD’s, and nursing staff.” “The staff are like little dried sponges; they’re just waiting to get something.” “More sessions for staff; the 4-hour orientation sessions should continue throughout the year; quick talks on the units; a refresher for DCAs.” “Make this mandatory education for health-care professionals; it should be taught in schools of nursing, allied health.” “A provincial learning module for staff. Topics: DMCA, mental health act; forms.” “Mentoring with ongoing discussion/case reviews - straightforward and complex.” |
| b. Integrate DMCAs into job descriptions | “Build DMCA more formally into job descriptions.” |
| c. Clarify scopes of practice | “Eliminate discomfort around legal repercussions by delineating scope of practice.” |
| d. Address issues of remuneration | “Ideally, proper classification for the level of work and remuneration is needed.” |
| e. Ensure access to consultative/specialty services | “We need an expert we can go to and easier access to DCAs; we need more specialists that teams can turn to.” |
| System Level | |
| a. Formalize DMCA resources | “Support the passionate people working to make this work – prevent burnout.” “Recognize and resource DMCA work – additional resources, adequate time to assess and follow up, dedicated staff.” “Access to informal consults.” “List of available resources for less intrusive measures.” “Outcome research.” |
| b. Standardize organizational, province-wide processes | “Standardize practice, interpretation and documentation.” “Document things; don’t allow people to fall through the cracks.” “Identifying which discipline initiates the process worksheet.” “Establish mechanisms to facilitate transfer of information.” |
| c. FacilitateModel adaptation/contextualization | “Adapt the Model to fit the community setting.” |
Benefits of the DMCA Model
Several benefits were identified with use of the Model. Most significantly, it is person-centred, aims to determine least restrictive/intrusive outcomes, and reduces the likelihood of unnecessary declarations of incapacity. The Model supports patients and families; builds capacity among HCPs and senior leaders through education/mentoring; provides a standardized best-practice process; cultivates a problem-solving approach; facilitates IP collaboration; and encourages HCPs to work to full scope of practice. It also facilitates culture change (see Table 4).
Theme #1: Facilitators of Model Implementation
Study participants identified numerous facilitators of Model implementation. These included availability of dedicated resources; buy-in from senior leadership and system level supports (zonal committees, steering committees, MTs); dedicated champions; training/mentoring activities; tools and worksheets; legislative acts and guiding principles (see Table 5).
Participants reported that the Model’s guiding principles and tools have been well-received and implemented into routine practice in facilities that have adequate supports and resourcing, senior leadership buy-in, and IP teams. Information gathering/sharing has been facilitated through use of the Model’s worksheets. HCPs on ATs and MTs have effectively conducted DMCAs, with experts and specialty services being consulted for more complex cases.
Theme #2: Barriers to Model Implementation
Study participants noted that Model implementation has been more difficult in less supportive/resourced environments, or where DMCAs are routinely referred to specialty teams rather than being handled by ATs and MTs. Barriers to Model implementation related to a lack of formal resources and time, clear role descriptions and workload expectations, buy-in and accountability, formal organizational processes, knowledge of HCPs regarding DMCAs, and remuneration (see Table 6).
Participants emphasized that HCPs require time to engage in education/mentoring, and consult on or conduct DMCAs. Many HCPs reported completing DMCAs in addition to their regular duties, which at times compromises the quality of their work and puts them at risk of burnout. Lack of appropriate remuneration, particularly for HCPs paid on a fee-for-service basis, was a significant impediment. Poor IP collaboration, and a lack of both shared responsibility for worksheet completion and standardized processes for documenting, posed further challenges. Restrictions to sharing client data across organizations and services were noted to result in system inefficiencies.
Theme #3: Recommendations for DMCA Model
While participants valued the Model, they also recommended improvements at the client, HCP, and system levels. An increased focus on person-centred care and family inclusion, greater communication across and between organizations, and minimization of duplicated assessments was encouraged. HCP-level recommendations revolved around enhanced and sustained access to education/mentoring, integration of DMCAs into job descriptions, appropriate remuneration, and timely access to consultative/specialty services. Allocation of dedicated DMCA resources, clearer organizational/system processes, a province-wide information and workload measurement system, and better collaboration across systems and organizations were identified at the system level (see Table 7).
DISCUSSION
Overall, the Model was found to offer HCPs, IP teams, and organizations a holistic and adaptable best-practice approach to DMCAs inclusive of tools and processes, and implementation strategies that enable the integration of the best-practice process into routine service provision. The assessment process, tools and education, and mentoring components of the Model enhance the ability of HCPs to more confidently, competently, and collaboratively work in this complex practice area to provide standardized DMCAs that result in least restrictive and intrusive outcomes for clients.
Despite the Model’s utility, however, several barriers warrant further consideration. Given that implementation and sustainability are hampered when HCP role clarity, job descriptions inclusive of DMCAs, physician engagement, inter-professional buy-in, accountability, dedicated time and resources, remuneration, information sharing, ongoing education/mentoring, and access to consultative/specialty services are lacking, strategies to address these challenges need to be found. These barriers would need to be addressed to ensure successful implementation and sustainability.
The survey findings were instructive in identifying areas requiring further attention regarding DMCAs. While a significant number of HCPs reported being confident in their knowledge of legislation, 26% lacked confidence. This highlights the need to ensure that education/training in this area is comprehensive. The Model’s effect on reducing angst, and therefore potential legal action, was limited. Given the potential contentious nature of DMCAs, however (particularly in complex cases), this may be unavoidable. As such, use of the standardized best-practice process outlined in the Model may be instrumental in reducing legal risk and costs. While costs associated with Model implementation and service delivery (e.g., time, resource, training and remuneration), are not insignificant, it may well be worth the investment. This investment becomes especially important when the outcome of a DMCA can have significant ramifications regarding a person’s ability to exercise one’s rights, and in times of fiscal constraint when resources available to manage litigation are all the more limited. Thoughtful consideration of strategies to overcome identified barriers and respond to recommendations may lead to more effective and realistic implementation and sustainability strategies.
Study Strengths and Limitations
This study had several strengths and limitations. Reliance on clinical experts who have used the Model offered realistic perspectives regarding its utility and recommendations for further adaptation and development. Given the unique process of Model implementation at various sites, however, their recommendations may not be generalizable. Methodologically, the Developmental Evaluation was well-aligned with the evolving nature of the Model, and the mixed methods design enabled access to numerical patterns and narrative experiences that supported evaluation of the Model. While the research sample was diverse, and extensive networking enabled access to key stakeholders, members of AT were only able to respond to surveys due to clinical demands. Further, the survey design limited the type of information gathered (allowing only for descriptive statistics and frequencies to be reported), and researchers were unable to ascertain the survey response rate. Due to privacy concerns, limited resources, and project timelines, neither review of patient chart data nor collection of data from patients and families was possible. Therefore, direct evaluation of Model impact on patient care was neither realistic nor feasible, nor was it the evaluation’s intent.
Future Research
This study is part of a larger program of research examining the Model and its effectiveness, in particular use by various professional groups; requirements and impacts at client, HCP and system levels; and frameworks for implementation, sustainability and spread. As the Model has predominantly been implemented and evaluated in urban, hospital environments, a more robust evaluation of its application in rural and community contexts is warranted. Future research will also address research limitations. It would be valuable to integrate performance measures, targeted outcomes for clients and systems, and evaluation of HCP core competencies regarding DMCAs. Chart reviews would yield a better understanding of outcomes at the client level. To determine resource requirements needed to support Model implementation and sustainability, establishment of a multi-organizational workload measurement system and costs/benefits analysis would be invaluable. Pre/post-comparison of implementation at sites that have yet to implement the Model would further allow for evaluation of the Model’s effectiveness, impact, and outcomes.
CONCLUSION
With a growing number of individuals experiencing compromised DMC, the need for standardized best-practice processes to assess DMCAs is likely to increase. Those working as independent practitioners or on IP teams within health, human services, education, and criminal justice systems in urban and rural environments might find the Model’s best-practice process and tools appropriate to employ in their jurisdictions. With appropriate contextualization and integration of strategies to address identified barriers, the Model’s best-practice process and implementation strategies may support DMCA service provision across various service sectors.
Several innovations could be introduced to facilitate implementation, sustainability and spread of the DMCA Model across various settings. Educational and implementation materials associated with the Model have been developed and customized for various contexts; adapting these to the on-line environment could make these resources more widely accessible. To ensure equitable access to DMCAs and consultation where expertise is lacking, as well as mentoring of HCPs and development of a community of practice, video-conferencing might be considered. Finally, coordination of services at a provincial systems level and across organizations could allow for greater integration of, and equitable access to, DMCA services. Integration of workload and outcome measurement tools could also be useful for monitoring the cost-benefits associated with Model implementation and use.
Acknowledgments
This Developmental Evaluation was made possible through funding by Alberta Health Services. Thank you to Jennifer Lee, Andrea Schertzer, and Rhianne McKay for their assistance with data analysis and to Lori Sacrey for editing the manuscript.
APPENDICES
Appendix 1: DMCA Research Project Survey (2012)
According to the values of AHS, we strive to provide care that is respectful, accountable, transparent and optimizes the engagement of our patients and others who are involved. Appropriate patient engagement may include assessment of a patient’s decision-making capacity. Please complete the survey questions below to assist AHS to understand the current status of the implementation of the model for assessment of decision-making capacity at your workplace. The survey will take about 10 minutes to complete. Participation in this survey is voluntary. Your responses will be confidential, and the results will only be reported in aggregate form. No individually identifying information will be used. Results will be used to guide future evolution of the DMCA model across AHS.
Please indicate your level of agreement with the following statements:
-
The new DMCA model is followed in my workplace.
❐ Strongly Disagree ❐ Disagree ❐ Agree ❐ Strongly Agree ❐ Do not know
-
I follow the guiding principles of DMCA when I am faced with concerns about a patient’s decision-making capacity.
❐ Strongly Disagree ❐ Disagree ❐ Agree ❐ Strongly Agree ❐ Do not know
-
I am confident in my knowledge about legislation as it applies to DMCA.
❐ Strongly Disagree ❐ Disagree ❐ Agree ❐ Strongly Agree ❐ Do not know
-
When a capacity concern is identified in a patient, I and/or my team member(s) will use the “Capacity Assessment Process Worksheet” to guide our work.
❐ Strongly Disagree ❐ Disagree ❐ Agree ❐ Strongly Agree ❐ Do not know
-
I understand the role of my discipline in DMCA and the part I play in the interdisciplinary approach to the assessment.
❐ Strongly Disagree ❐ Disagree ❐ Agree ❐ Strongly Agree ❐ Do not know
-
I and/or my team member(s) will explore problem-solving opportunities in order to reduce the risk to the patient before suggesting a capacity interview.
❐ Strongly Disagree ❐ Disagree ❐ Agree ❐ Strongly Agree ❐ Do not know
-
I am confident in my knowledge and skills regarding DMCA and comfortable being involved in these assessments.
❐ Strongly Disagree ❐ Disagree ❐ Agree ❐ Strongly Agree ❐ Do not know
-
The capacity assessment model has reduced the angst/conflicts amongst staff, patients and families when dealing with issues related to DMCA.
❐ Strongly Disagree ❐ Disagree ❐ Agree ❐ Strongly Agree ❐ Do not know
-
A Capacity Assessment Mentoring Team is available to assist our team with questions and to provide support about DMCA.
❐ Strongly Disagree ❐ Disagree ❐ Agree ❐ Strongly Agree ❐ Do not know
-
The standardized process for DMCA has improved the efficiency and effectiveness of capacity assessments performed by my team.
❐ Strongly Disagree ❐ Disagree ❐ Agree ❐ Strongly Agree ❐ Do not know
-
I have had the opportunity to attend ongoing learning sessions that provide further information and support for the implementation of DMCA.
❐ Strongly Disagree ❐ Disagree ❐ Agree ❐ Strongly Agree ❐ Do not know
-
I and my team receives the necessary management support to implement the model for DMCA.
❐ Strongly Disagree ❐ Disagree ❐ Agree ❐ Strongly Agree ❐ Do not know
-
Describe any barriers or challenges you have encountered to implementing the new Decision Making Capacity Assessment model.
_________________________________________________________________________________________________
-
Do you have any comments or suggestions on how to improve the current approach to the model for assessment of decision-making capacity?
_________________________________________________________________________________________________
-
What is your professional role?
❐ Social Worker ❐ Occupational Therapist ❐ Registered Nurse ❐ Nurse Practitioner
❐ Speech Language Pathologist ❐ Psychologist ❐ Physician ❐ Transition Services Co-ordinator
❐ Program Manager ❐ Unit Supervisor ❐ Clinical Nurse Educator ❐ Other: Please specify
_________________________________________________________________________________________________
-
I am a (check all that apply):
❐ Member of an interdisciplinary/attending team ❐ Member of a Mentoring team ❐ DCA
-
Please select the date of participation in the DMCA interactive education session:
❐ Less than 3 months ❐ 3–6 months ago ❐ 6–12 months ago
❐ 1 year ago ❐ 2 years ago ❐ 3 years ago ❐ 4 years ago
-
How many years have you been in professional practice?
❐ 0–1 ❐ 2–5 ❐ 6–10 ❐ 11–15 ❐ 16 or more
-
Please indicate your age.
❐ 15–19 ❐ 20–24 ❐ 25–29 ❐ 30–34 ❐ 35–39 ❐ 40–44 ❐ 45–49
❐ 50–54 ❐ 55–59 ❐ 60–64 ❐ 65–70 ❐ 70–74 ❐ 75+
-
Please indicate your gender.
❐ Female ❐ Male
-
Please indicate where you currently work.
❐ Peter Lougheed Centre (Calgary)
❐ Rockyview General Hospital (Calgary)
❐ Foothills Medical Centre (Calgary)
❐ Community/Rural (Calgary)
❐ Royal Alexandra Hospital (Edmonton)
❐ Misericordia Community Hospital (Edmonton)
❐ Grey Nuns Community Hospital (Edmonton)
❐ Villa Caritas (Edmonton)
❐ Sturgeon General Hospital (Edmonton)
❐ Glenrose Rehabilitation Hospital (Edmonton)
❐ Westview Health Region (Edmonton)
❐ Good Samaritan Society Choice Program (Edmonton)
❐ Good Samaritan Society Seniors Clinic (Edmonton)
❐ Continuing Care Facility Living (Edmonton)
❐ Continuing Care Supportive Living (Edmonton)
❐ Continuing Care Home Living (Edmonton)
-
Please feel free to offer any additional comments:
__________________________________________________________________________________
________________________________________________________________________________________________________________
Thank you for your time and participation!
Footnotes
CONFLICT OF INTEREST DISCLOSURES
None of the authors have financial, commercial or other conflicts to declare. While the DMCA Model was initially developed by an interdisciplinary working group at Covenant Health where one of the co-authors, Dr. Jasneet Parmar, was Site Lead for Geriatrics (Misericordia Hospital), the development of the Model has since been supported on a broader scale by Alberta Health Services and its partner agencies. Care was taken by the co-authors to ensure that objectivity was maintained during data collection and analysis, and that any associated conflict of interest was mitigated.
REFERENCES
- 1.Berg JW, Appelbaum PS, Lidz CW, et al. Informed consent: Legal theory and clinical practice. 2nd ed. Fair Lawn, NJ: Oxford University Press; 2001. [Google Scholar]
- 2.Coverdale J, McCullough LB, Molinari V, et al. Ethically justified clinical strategies for promoting geriatric assent. Int J Geriatr Psychiat. 2006;21(2):151–57. doi: 10.1002/gps.1443. [DOI] [PubMed] [Google Scholar]
- 3.Government of Alberta, Human Services, Office of the Public Guardian 2012. Available from: http://www.humanservices.alberta.ca/guardianship-trusteeship.html.
- 4.Alzheimer Society of Canada . Rising tide: the impact of dementia on Canadian society. Toronto, ON: Alzheimer’s Society of Canada; 2010. Available from: http://www.alzheimer.ca/~/media/Files/national/Advocacy/ASC_Rising_Tide_Full_Report_e.pdf. [Google Scholar]
- 5.James K, Watts L. Understanding the lived experiences of supported decision-making in Canada — legal capacity, decision-making and guardianship. Toronto, ON: Law Commission of Ontario; 2014. Available from http://www.lco-cdo.org/capacity-guardianship-commissioned-paper-ccel.pdf. [Google Scholar]
- 6.UN General Assembly . Convention on the rights of persons with disabilities (CRPD) New York: UN General Assembly; Resolution/adopted by the General Assembly, 24 January 2007, resolution A/RES/61/106. [Google Scholar]
- 7.Government of British Columbia . Representation Agreement Act [RSBC 1996] Chapter 405 (RAA) Victoria, BC: British Columbia Queen’s Printer; 1996. Available from: http://www.bclaws.ca/Recon/document/ID/freeside/00_96405_01. [Google Scholar]
- 8.Government of Alberta . Guide for capacity assessors — Adult Guardianship And Trusteeship Act. Edmonton, AB: Office of Public Guardian; 2013. Available from: http://humanservices.alberta.ca/documents/opg-guardianship-publication-opg5630.pdf. [Google Scholar]
- 9.Ministry of the Attorney General . Guidelines for conducting assessments of capacity. Toronto, ON: The Capacity Assessment Office; 2005. [Google Scholar]
- 10.Yukon Department of Justice . Guidelines for conducting incapability assessments for the purpose of guardianship applications. Whitehorse, YK: Department of Justice; 2005. [Google Scholar]
- 11.Grisso T, Appelbaum PS. Assessing competence to consent to treatment: a guide for physicians and other health professionals. New York: Oxford University Press; 1998. [Google Scholar]
- 12.Weisstub DN. Enquiry on mental capacity — final report. Toronto, ON: Queen’s Printer for Ontario; 1990. [Google Scholar]
- 13.Pachet A, Newberry A, Erskine L. Assessing capacity in the complex patient: RCAT’s unique evaluation and consultation model. Can Psychol. 2007;48(3):174–86. doi: 10.1037/cp2007016. [DOI] [Google Scholar]
- 14.Brindle N, Holmes J. Capacity and coercion: Dilemmas in the discharge of older people with dementia from general hospital settings. Age and Ageing. 2005;34(1):16–20. doi: 10.1093/ageing/afh228. [DOI] [PubMed] [Google Scholar]
- 15.Etchells E. Aid to capacity evaluation (ACE) Toronto, ON: University of Toronto, Joint Centre for Bioethics; 2008. [Google Scholar]
- 16.Mukherjee D, McDonough C. Clinician perspectives on decision-making capacity after acquired brain injury. Topics in Stroke Rehabil. 2006;13(3):75–83. doi: 10.1310/2M1U-71FQ-QV33-56PX. [DOI] [PubMed] [Google Scholar]
- 17.Sturman ED. The capacity to consent to treatment and research: a review of standardized assessment tools. Clin Psychol Rev. 2005;25(7):954–74. doi: 10.1016/j.cpr.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization . Dementia — a public health priority. Geneva, Switzerland: WHO; 2015. Report No: WHO/MSD/MER/15.2. Available from: http://www.who.int/mental_health/neurology/dementia/dementia_thematicbrief_executivesummary.pdf. [Google Scholar]
- 19.World Health Organization . Ensuring a human rights-based approach for people living with dementia. Geneva, Switzerland: WHO; 2015. Report No.: WHO/MSD/MER/15.4. Available from: http://www.who.int/mental_health/neurology/dementia/dementia_thematicbrief_human_rights.pdf. [Google Scholar]
- 20.Moye J, Butz SW, Marson DC, et al. A conceptual model and assessment template for capacity evaluation in adult guardianship. The Gerontologist. 2007;47(5):591–603. doi: 10.1093/geront/47.5.591. [DOI] [PubMed] [Google Scholar]
- 21.Skelton F, Kunik ME, Regev T, et al. Determining if an older adult can make and execute decisions to live safely at home: a capacity assessment and intervention model. Arch Gerontol Geriatr. 2010;50(3):300–05. doi: 10.1016/j.archger.2009.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.American Bar Association and the American Psychological Association Assessment of older adults with diminished capacity: a handbook for psychologists. 2008. Available from: http://www.apa.org/pi/aging/programs/assessment/capacity-psychologist-handbook.pdf.
- 23.Government of Alberta . Personal directives act – revised statues of Alberta 2000, Chapter P-6. Edmonton: Alberta Queen’s Printer; 2013. Available from: http://www.qp.alberta.ca/documents/Acts/p06.pdf. [Google Scholar]
- 24.Government of Alberta . Powers Of Attorney Act — revised statutes of Alberta 2000, Chapter P-20. Edmonton, AB: Alberta Queen’s Printer; 2014. Available from: http://www.qp.alberta.ca/documents/Acts/p20.pdf. [Google Scholar]
- 25.Government of Alberta . Adult Guardianship And Trusteeship Act. Edmonton, AB: Government of Alberta; 2013. Available from: http://www.qp.alberta.ca/documents/Acts/A04P2.pdf. [Google Scholar]
- 26.Parmar J, Brémault-Phillips S, Charles L. The development and implementation of a decision-making capacity assessment model. Can Geriatr J. 2015;18(1):15–28. doi: 10.5770/cgj.18.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brémault-Phillips S, Parmar J. Assessment of decision-making capacity in adults with diseases and disabilities: is the decision- making capacity assessment model appropriate for Alberta? 2012. A project funded by Alberta Health Services. Available from: http://hdl.handle.net/10402/era.38855.
- 28.Statistics Canada . Focus on geography series, 2011 census. Ottawa, ON: Statistics Canada; 2011. Statistics Canada Catalogue no. 98-310-XWE2011004. Available from: http://www12.statcan.gc.ca/census-recensement/2011/as-sa/fogs-spg/Facts-pr-eng.cfm?Lang=eng&GC=48. [Google Scholar]
- 29.Patton MQ. A utilization-focused approach to contribution analysis. Evaluation. 2012;18(3):364–77. doi: 10.1177/1356389012449523. [DOI] [Google Scholar]
- 30.Patton MQ. The roots of utilization-focused evaluation. In: Alkin MC, editor. Evaluation roots: a wider perspective of theorists? Views and influences. Thousand Oaks, CA: SAGE Publications Inc; 2013. pp. 293–97. [Google Scholar]
- 31.Patton MQ. Developmental Evaluation — applying complexity concepts to enhance innovation and use. New York: Guilford Press; 2010. [Google Scholar]
- 32.Creswell J, Plano Clark V. Designing and conducting mixed methods research. 2nd ed. Thousand Oaks, CA: Sage Publications Inc; 2010. [Google Scholar]
- 33.Cruz EV, Higginbottom G. The use of focused ethnography in nursing research. Nurse Res. 2013;20(4):36–43. doi: 10.7748/nr2013.03.20.4.36.e305. [DOI] [PubMed] [Google Scholar]
- 34.Higginbottom G, Pillay Jennifer J, Boadu NY. Guidance on performing focused ethnographies with an emphasis on healthcare research. The Qualitative Report. 2013;18(17):1–16. Available from: http://www.nova.edu/ssss/QR/QR18/higginbottom17.pdf. [Google Scholar]
- 35.QSR International . Nvivo 9 [software] Victoria, Australia: QSR International Pty Ltd.; [n.d.]. Available from: http://www.qsrinternational.com. [Google Scholar]
- 36.Roper JM, Shapira J. Ethnography in nursing research. Thousand Oaks, CA: SAGE Publications Inc; 2000. [DOI] [Google Scholar]
- 37.Fluid Survey [survey website] Available from: http://fluidsurveys.com/