Abstract
Purpose
High intensity interval training (HIIT) has been proposed as a time-efficient format of exercise to reduce the chronic disease burden associated with sedentary behaviour. Changes in oxygen utilisation at the local tissue level during an acute session of HIIT could be the primary stimulus for the health benefits associated with this format of exercise. The recovery periods of HIIT effect the physiological responses that occur during the session. It was hypothesised that in sedentary individuals, local and systemic oxygen utilisation would be higher during HIIT interspersed with active recovery periods, when compared to passive recovery periods.
Methods
Twelve sedentary males (mean ± SD; age 23 ± 3 yr) completed three conditions on a cycle ergometer: 1) HIIT with passive recovery periods between four bouts (HIITPASS) 2) HIIT with active recovery periods between four bouts (HIITACT) 3) HIITACT with four HIIT bouts replaced with passive periods (REC). Deoxygenated haemoglobin (HHb) in the vastus lateralis (VL) and gastrocnemius (GN) muscles and the pre-frontal cortex (FH), oxygen consumption (VO2), power output and heart rate (HR) were measured continuously during the three conditions.
Results
There was a significant increase in HHb at VL during bouts 2 (p = 0.017), 3 (p = 0.035) and 4 (p = 0.035) in HIITACT, compared to HIITPASS. Mean power output was significantly lower in HIITACT, compared to HIITPASS (p < 0.001). There was a significant main effect for site in both HIITPASS (p = 0.029) and HIITACT (p = 0.005). There were no significant differences in VO2 and HR between HIITPASS and HIITACT.
Conclusions
The increase in HHb at VL and the lower mean power output during HIITACT could indicate that a higher level of deoxygenation contributes to decreased mechanical power in sedentary participants. The significant differences in HHb between sites indicates the specificity of oxygen utilisation.
Introduction
Sedentary behaviour, defined as not meeting physical activity recommendations for the achievement of health benefits, is a risk factor for multiple chronic diseases [1, 2] and a global epidemic [1, 3–7]. Physical activity recommendations include accumulating 150–300 minutes of moderate intensity exercise each week [8]. The most frequently cited reason for non-compliance is a lack of time [9]. High intensity interval training (HIIT) of a low volume has been proposed as a time-efficient exercise format to improve exercise adherence, thereby reducing the chronic disease burden associated with sedentary behaviour [10]. The beneficial effect of HIIT interventions on markers of health risk has been well documented [11–13]. HIIT has been shown to be as effective or more effective than longer, moderate intensity exercise interventions at improving specific markers of risk, such as low cardiorespiratory fitness [11, 14, 15].
Benefits of regular HIIT exercise, such as increased cardiorespiratory fitness, have been linked to increases in mitochondrial content and function [16, 17]. Whilst the exact mechanisms underlying these increases are not completely understood, it is possible that the increase in oxygen utilisation at the local tissue level during an acute session of HIIT provides a stimulus for these improvements. The effects of a single HIIT intervention on systemic and locomotor muscle oxygenation have been evaluated previously [18, 19]. However, these investigations were conducted in active individuals, evaluated only one muscle site and used measures of oxygenation in a sports performance context [18, 20].
Site specific oxygen utilisation at the local tissue level can be measured using near infrared spectroscopy (NIRS). NIRS is a non-invasive method for the measurement of the change in concentration of oxyhaemoglobin (O2Hb) (oxygen availability) and deoxyhaemoglobin (HHb) (oxygen utilisation), as measures of tissue level oxygenation. Oxygen utilisation during exercise has been described in active individuals at a single muscle site [21] and in component muscles of the quadriceps [22, 23]. In active individuals, at a single muscle site, oxygen utilisation (as indicated by increased HHb) is increased during HIIT bouts when compared to pre-exercise values [18, 24].However, oxygen utilisation during HIIT in sedentary individuals at the local tissue level has not been determined. Furthermore it is unknown if oxygen utilisation differs between distinct locomotor muscles in a sedentary population during HIIT. Investigation of the oxygen utilisation responses in sedentary individuals will provide additional information on the extent to which oxygen utilisation increases during HIIT in distinct locomotor muscles, a potential stimulus for improved mitochondrial function.
Nine design components (series, inter-series, bout and recovery: number, duration and intensity as well as exercise mode) can be altered in HIIT [25]. The recovery periods of HIIT are an integral part of the exercise session, as these periods have an effect on the physiological responses that occur during the session [26].The two most frequently adopted HIIT recovery formats are passive and active recovery. The effect of recovery formats on local tissue oxygenation and markers of performance have yielded inconsistent findings to date, with active recovery leading to higher [18], lower [26] or an equivalent [24] degree of local muscle deoxygenation when compared with passive recovery. Similarly, inconsistent findings have been shown when mechanical power and heart rate were compared during HIIT that included either active or passive recovery [26–29]. Variations in the HIIT protocols used during these projects may have contributed to the conflicting results. The effect of active versus passive recovery periods on oxygen utilisation during HIIT bouts at specific locomotor muscle and brain tissue sites, in sedentary populations, is unknown.
The primary aim of this project was to compare the local (Δ[HHb]) and systemic (VO2) oxygen utilisation, mean power output and heart rate responses during HIIT conditions which included either passive or active recovery. A secondary aim was to compare the relative Δ[HHb] between local muscle and brain tissue sites during HIIT exercise.
It was hypothesised that in young sedentary individuals, during high intensity exercise bouts that are interspersed with active recovery periods, when compared to passive recovery periods, VO2, Δ[HHb],mean power output and heart rate would be higher and that the increase in Δ[HHb] during HIIT exercise would be higher at the local muscle tissue sites when compared to the brain site.
Methods
Ethics statement
This research project was approved by the human research ethics committee of the University of the Sunshine Coast (S/13/472). All participants received a research project information sheet before providing written informed consent.
Experiment design
The project consisted of three testing sessions, one for each of the three conditions of the project. Exercise was performed using a cycling ergometer.
All testing sessions were separated by three to seven days to prevent a potential carry-over effect between conditions and to minimise the effect of any potential confounding variables between testing sessions. In this article, each 30 s period of high intensity exercise is referred to as a bout. Each complete protocol consisting of four x 30 s bouts of high intensity exercise, separated by 2 min recovery periods, is referred to as a condition.
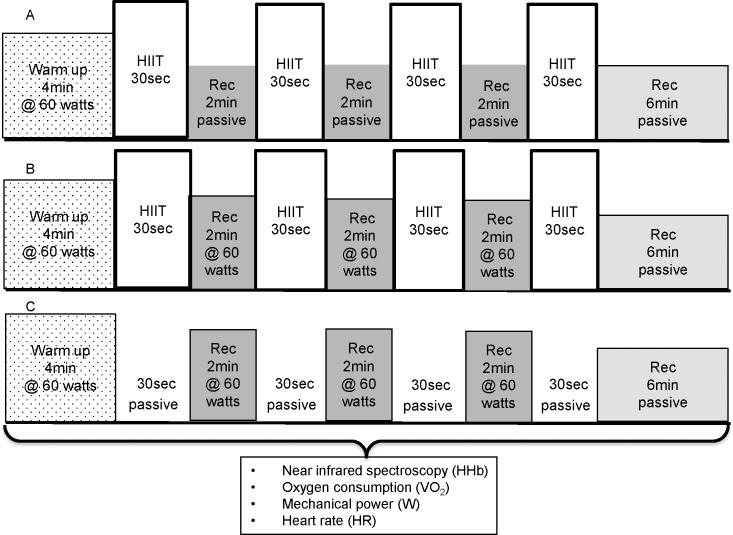
The three conditions were: 1) a protocol of high intensity interval exercise with passive recovery periods between each bout of HIIT (HIITPASS) 2) a protocol of high intensity interval exercise with active recovery periods between each bout of HIIT (HIITACT) 3) a protocol in which only the active recovery periods were completed and the bouts of HIIT were replaced with passive periods (REC), in order to quantify the effect of active recovery. The conditions were randomized and followed a latin-squares cross-over design to control for a possible order effect. The conditions and the timing of measurements are illustrated in Fig 1.
Fig 1. The structure and timing of measurements of the three conditions.
(A) HIITPASS. (B) HIITACT. (C) REC.
Participants
The participant group consisted of twelve males from the University community who met the inclusion criteria of being aged 18–30 yr.; currently completing less than 150 minutes of moderate intensity or 75 minutes of vigorous intensity activity per week; presenting with no cardiovascular and metabolic disease; taking no medications; having no known orthopaedic or other health related issues that would be made worse by participation in, or inhibit completion of the project. Descriptive physical characteristics of these participants are in Table 1.
Table 1. Participant characteristics.
| Height (cm) | 176.3 ± 8.3 |
| Weight (kg) | 78.19 ± 13.82 |
| Age | 23 ± 3 |
| Vastus lateralis skinfold (mm) | 12.75 ± 5.88 |
| Gastrocnemius skinfold (mm) | 11.00 ± 3.25 |
| FVC (L) | 5.40 ± 0.77 |
| FVC % pred (%) | 104.7 ± 10.2 |
| FEV1 (L) | 4.54 ± 0.72 |
| FEV1% pred (%) | 104 ± 10.9 |
Data are (mean ± SD) (n = 12)
Procedures and equipment
Screening procedures
At the first testing session, participants completed risk screening and medical history questionnaires and a physical activity log. For the physical activity log participants reported the duration, intensity and type of activity which they had completed over the preceding seven days as well as the daily activity undertaken during an average week over the last three months. This physical activity log was used to ensure that participants’ recent activity levels were within the definition of sedentary for the purposes of this project (an individual not achieving the current minimal recommendations for exercise participation to gain health benefits) [30]. Participants were asked to refrain from performing any exercise in the 24 hours preceding each session and to not ingest any caffeine, alcohol or a large meal in the four hours preceding a session. Participants were asked to ensure that they were adequately fed and hydrated on the day of testing and this was confirmed at each testing session. To ensure normal resting pulmonary function, participants completed a pulmonary function test (Spirolab II, Medical International Research, Rome, Italy) following standard procedures [31] (Table 1). Participants were characterised by height, mass and adipose tissue thickness (ATT) (Table 1). ATT measurements, performed by the same researcher in each instance using skinfold callipers (Harpenden, British Indicators Ltd, Burgess Hill UK) and standard procedures, ensured that site-specific changes in oxygenation occurred within the muscle tissue rather than in the skin and adipose tissue.
Exercise conditions
Prior to the first exercise session, participants were familiarised with the Wingate testing protocol, the Velotron cycle ergometer (Racermate, Seattle WA, USA) and the process of holding a constant cadence. The cycle ergometer seat height and handlebar position were adjusted for each participant and replicated for subsequent exercise sessions.
The HIIT protocol utilised during two of the three conditions (HIITPASS and HIITACT) was adapted from protocols used in sporting, recreationally active and untrained populations. [20, 24, 32–36].
Each condition consisted of an initial baseline data collection period of 3 min when the participant remained stationary on the cycle ergometer. Exercise testing began with a 4 min warm up period. The warm up period consisted of each participant cycling against a fixed resistance of 60 Watts (W) at a cadence of 60 revolutions per minute (RPM). The warm up was followed by four 30 s bouts of high intensity exercise in the HIITPASS and HIITACT conditions, with 2 min recovery periods separating each of the high intensity bouts. During the REC condition, the four high intensity exercise bouts were replaced by periods of passive rest. Each participant was asked to increase cadence to a maximum during a five second period immediately preceding each bout of HIIT.
The resistance (0.075kg per kilogram body weight), automatically applied to the flywheel of the ergometer at the start of each bout of HIIT, was utilised during other HIIT Wingate protocols involving untrained adult populations [37]. Power output during the HIIT bouts was determined by participant effort. Participants were instructed to give a maximal effort from the beginning of each bout, using the prompt to ‘go as hard as you can’. Participants were then verbally encouraged using standardised phrases during all bouts of exercise in an attempt to ensure a maximal effort. During the passive recovery periods of the HIITPASS condition, participants were instructed to sit as still as possible with the bicycle cranks in a relaxed horizontal position. During the active recovery periods of the HIITACT and REC conditions, participants were instructed to pedal at a cadence of 60 RPM against a resistance of 60 W (approximately 30–40% VO2max) [38], an intensity of active recovery shown to promote optimal clearance of metabolites [39, 40]). Upon completion of the fourth and final bout, there was a 6 min passive recovery period.
Participants were instructed to remain seated throughout each condition in an attempt to reduce movement artefact in the NIRS data and to allow for consistency in muscular recruitment patterns and hence power data.
Tissue oxygenation
Changes in local tissue oxygenation were measured continuously during rest, exercise and recovery. The terms oxygenated haemoglobin (O2Hb), and deoxygenated haemoglobin (HHb) each include the combined signal of Hb and myoglobin (Mb). The changes in the relative concentration of O2Hb (Δ[O2Hb]) and HHb (Δ[HHb]) as a function of time were measured using a Near Infrared Spectroscopy (NIRS) system (2 x PortaMon and 2 x Portalite devices, Artinis Medical Systems BV, Zetten, Netherlands). This system allows for non-invasive and simultaneous measurement of these variables at multiple sites. The NIRS system uses a modified form of the Beer-Lambert law to calculate changes in O2Hb and HHb using two continuous wavelengths of near infrared light (763 and 855nm). A fixed differential pathlength factor (DPF) of 4 was used for muscle tissue and an age dependant DPF was used for cerebral tissue based on manufacturer recommendations.
The NIRS devices (weighing 84 grams with dimensions of 83 x 52 x 20 mm) were placed on the shaved skin overlying the muscle belly of two locomotor muscles of the left leg, the vastus lateralis (VL) and the gastrocnemius (GN), a muscle involved in respiration: the 7th external intercostal muscle (IC) and the area of the forehead overlying the pre-frontal cerebral cortex (FH) approximately 3 cm left from the forehead midline and immediately above the supra-orbital ridge (between Fp1 and F3, according to the modified international EEG 10–20 system). To ensure measurement consistency, the placement of the NIRS devices was referenced to accepted anatomical landmarks as detailed in previous experiments [18, 24, 41–43]. The location of a devices was marked with a felt tip pen at the first testing session and participants were instructed to maintain these marks between sessions. Each device was secured using standardised procedures to shield against ambient light contamination and to prevent motion artefact due to device slippage. For all testing the same device was used at the same measurement site for each participant. The NIRS system was connected via Bluetooth to a computer for data acquisition and subsequent data analysis.
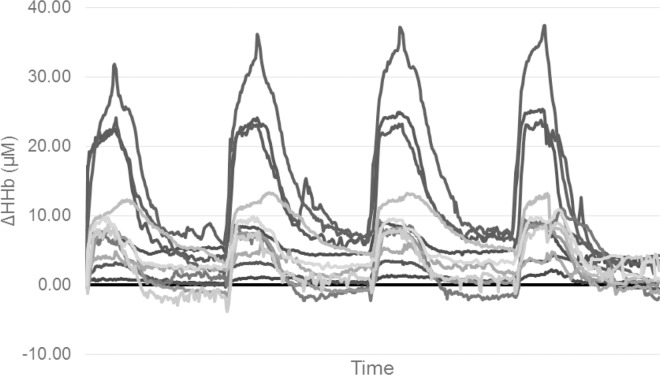
For this project, both Δ[O2Hb] and Δ[HHb] were measured, however only Δ[HHb] values are presented. The Δ[HHb] data are potentially unaffected by changes in perfusion, blood volume or arterial haemoglobin concentration [44–46]. The Δ[O2Hb] data are affected by muscular compression and changes in blood flow and volume [47], especially during the rapid and substantial changes in these variables that accompany HIIT bouts [18]. Using Δ[HHb] is consistent with other research utilising NIRS measurements to investigate HIIT and exercise in general [18, 24] thereby allowing for comparisons to be made between this project and previous research. NIRS data collected at the IC site included gross movement artefact throughout testing, obscuring the NIRS signal. Gross movement artefact was also present in NIRS data collected at the VL and GN sites during the passive recovery periods of the HIITPASS condition. Therefore data collected at the IC site and recovery period data from other sites were not included in further analysis. The inter-individual variability noted in the Δ[HHb] data (range 0.73–32.56 μM) is presented for the VL in HIITACT (Fig 2).
Fig 2. Individual relative change from baseline of deoxygenated haemoglobin (HHb) during the HIITACT condition.
(n = 12).
Systemic oxygen consumption (VO2)
In order to quantify the systemic oxygen utilisation in response to the three conditions, systemic oxygen consumption data was collected continuously during the rest, exercise and recovery periods using a respiratory gas analysis open circuit spirometer system (Parvo Medics, Sandy UT, USA) and a standard gas collection mouthpiece (Hans Rudolph, Kansas, United States of America). Standardised calibration and methods were used [48].
Mechanical power
Mechanical power was measured during the cycling portions of each condition using a SRM ‘Science’ power meter (SRM, Julich, Germany). Prior to each testing session the SRM unit was calibrated according to the manufacturer’s specifications.
Heart rate (HR)
To quantify exercise intensity during all exercise conditions, a heart rate monitor (RS400, Polar Electro, Kempele, Finland) was used to measure heart rate data during rest, exercise and recovery periods.
Data calculation and statistical analysis
All NIRS data were collected at a frequency of 10 Hz and smoothed using a 10 point moving average before being averaged to 1 s periods. Due to the HHb data being a measure of change from an arbitrarily assigned baseline zero value, the NIRS data are expressed as units of change (μMol) from the mean value of the 30 s of baseline data preceding the start of exercise (Δ[HHb]). To determine the between test reliability of the HHb data from the NIRS system, absolute reliability (Typical Error: VL = 0.4, GN = 0.8, FH = 0.6) of the baseline data for each site was used. Furthermore, previous research has shown that the NIRS method provides acceptable reliability [49, 50]. VO2 data were averaged over 5 s periods in preparation for further analysis whilst mechanical power and HR data were averaged at 1 s intervals. The NIRS, HR, VO2 and power data were then time aligned and the time periods of data corresponding to the four 30 s bouts of HIIT identified. Mean 30 s values were then calculated for all dependant variables for each bout of HIIT, providing a single value per bout for statistical analysis.
Statistics
Statistical tests were performed using IBM SPSS Statistics (version 22, IBM Corporation, Armonk NY, USA). Data was initially screened for normality of distribution using a Shapiro-Wilk test. A two factor, repeated-measures analysis of variance (ANOVA) was used to analyse the effect of condition and bout on the dependant variables of VO2, HR and mechanical power. A three factor, repeated-measures ANOVA was used to analyse the effect of condition, bout and site on the dependant variable Δ[HHb]. Mauchly’s W test was used to evaluate sphericity for each dependant variable. For those variables that violated the assumption of sphericity, the degrees of freedom were adjusted using the Greenhouse-Geisser correction if the estimate of sphericity (є) < 0.75. If є >0.75 the Huynh-Feldt adjustment was used and significance re-evaluated. If a significant main effect was identified, a Bonferroni’s post hoc test was used to make pair wise comparisons. All variables are presented as mean ± standard deviation (SD). For all statistical analyses, a P value of < 0.05 was accepted as the level of significance.
Results
Tissue oxygenation
For the mean Δ[HHb] from all conditions, sites and bouts combined, there was a main effect for site (p = 0.003, F = 7.493), with significant differences found between FH and VL sites (p = 0.025) and the difference between GN and VL sites approaching significance (p = 0.056). There was also a main effect for condition (p < 0.001, F = 20.899), however no significant differences were found between the two HIIT conditions. There were condition x site (p = 0.016) and site x bout (p = 0.002) interactions.
For the mean Δ[HHb] for each condition, there was a main effect for site for HIITPASS [(p = 0.029, F = 4.346) FH = 1.97 ± 2.69 μM, GN = 4 ± 4.46 μM, VL = 6.97 ± 5.42 μM] and HIITACT [(p = 0.005, F = 10.014) FH = 1.81 ± 2.65 μM, GN = 4.44 ± 3.75 μM, VL = 10.722 ± 8.48 μM] with significant differences found between FH and VL (p = 0.018) and GN and VL (p = 0.035) for HIITACT. There were site x bout interactions for HIITPASS (p = 0.001) and HIITACT (p = 0.042). No significant differences were found for REC [FH = -0.28 ± 1.16 μM, GN = -0.64 ± 2.39 μM, VL = 0.22 ± 3.38 μM].
Forehead (FH)
For the FH there was a main effect in the mean Δ[HHb] for condition, however no significant differences were found between the two HIIT conditions: [(p = 0.002, F = 8.513) HIITPASS 1.97 ± 2.69 μM; HIITACT 1.8 ± 2.65 μM; REC -0.27 ± 1.16 μM]. There was a condition x bout interaction (p = 0.003).
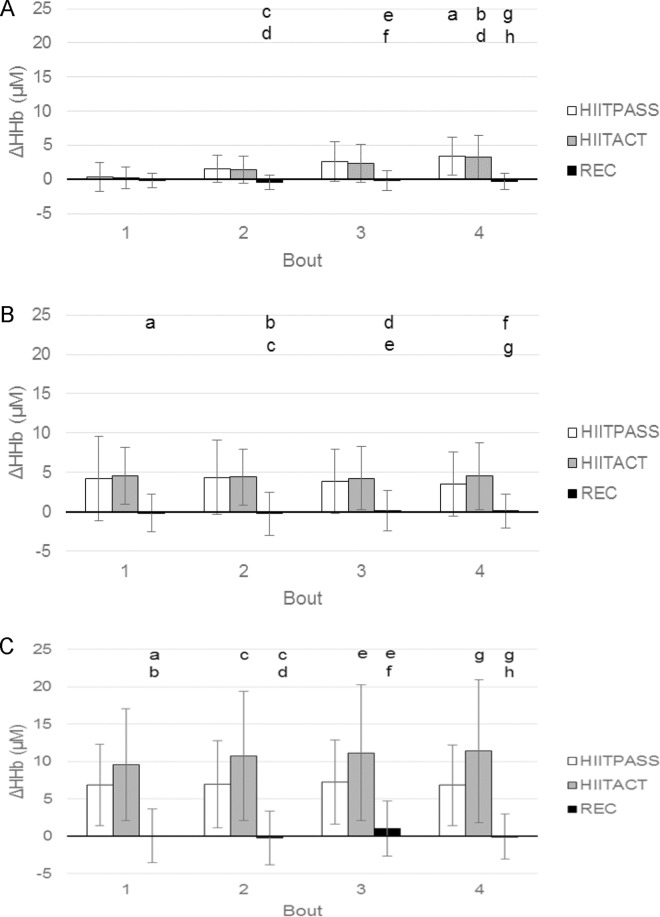
For the mean Δ[HHb] for each bout (Fig 3, panel A), differences were found between conditions for Bout 2 (p = 0.006, F = 6.504), Bout 3 (p = 0.003, F = 7.845) and Bout 4 (p < 0.001, F = 12.758), however no significant differences were found between the two HIIT conditions. For the mean Δ[HHb] within conditions, there were significant increases across bouts, with values increasing over time in the HIITPASS (p = 0.003, F = 9.733) and HIITACT (p = 0.007, F = 8.511) conditions.
Fig 3. Relative change from baseline of deoxygenated haemoglobin (HHb) concentration during the four bouts of the three conditions.
(A) FH. a = significantly different to HIITPASS, bout 1; b = significantly different to HIITACT, bout 1; c = significantly different to HIITPASS, bout 2; d = significantly different to HIITACT, bout 2; e = significantly different to HIITPASS, bout 3; f = significantly different to HIITACT, bout 3; g = significantly different to HIITPASS, bout 4; h = significantly different to HIITACT, bout 4. (B) GN. a = significantly different to HIITACT bout 1; b = significantly different to HIITPASS, bout 2; c = significantly different to HIITACT bout 2; d = significantly different to HIITPASS, bout 3; e = significantly different to HIITACT bout 3; f = significantly different to HIITPASS, bout 4; g = significantly different to HIITACT, bout 4. (C) VL. a = significantly different to HIITPASS, bout 1; b = significantly different to HIITACT, bout 1; c = significantly different to HIITPASS, bout 2; d = significantly different to HIITACT, bout 2; e = significantly different to HIITPASS, bout 3; f = significantly different to HIITACT, bout 3; g = significantly different to HIITPASS, bout 4; h = significantly different to HIITACT, bout 4. Data are mean ± SD. (p >0.05).
Gastrocnemius (GN)
For the GN there was a main effect in the mean Δ[HHb] for condition, however no significant differences were found between the two HIIT conditions: [(p < 0.001, F = 11.911) HIITPASS 4.00 ± 4.46 μM; HIITACT 4.4 ± 3.75 μM; REC -0.06 ± 2.39 μM]. There was no significant condition x bout interaction.
For the mean Δ[HHb] for each bout (Fig 3, panel B), differences were found between conditions for Bout 1 (p = 0.006, F = 9.270), Bout 2 (p < 0.001, F = 11.339), Bout 3 (p = 0.001, F = 9.475) and Bout 4 (p < 0.001, F = 12.765), however no significant differences were found between the two HIIT conditions. For the mean Δ[HHb] within conditions, no significant differences were found across bouts.
Left vastus lateralis (VL)
For the VL, there was a main effect in the mean Δ[HHb] for condition: [(p = 0.003, F = 13.060) HIITPASS 6.97 ± 5.42 μM; HIITACT 10.72 ± 8.48 μM; REC 0.22 ± 3.38 μM]. There was no significant condition x bout interaction.
For the mean Δ[HHb] for each bout (Fig 3, panel C), differences were found between conditions for Bout 1 (p = 0.002, F = 14.835), Bout 2 (p = 0.003, F = 12.968), Bout 3 (p = 0.006, F = 10.587) and Bout 4 (p = 0.004, F = 12.575) with significant differences found between the two HIIT conditions. For the mean Δ[HHb] within conditions, there were no significant differences found across bouts.
Systemic oxygen consumption
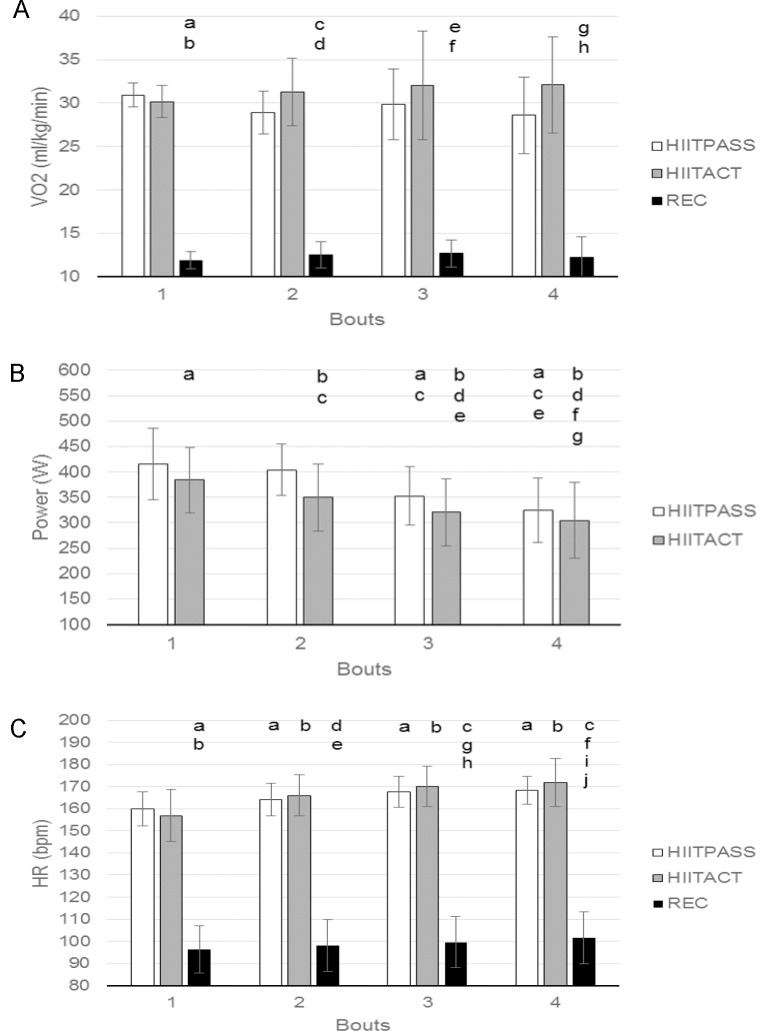
For the mean VO2, there was a main effect for condition [(p < 0.001, F = 161.601), however no significant differences were found between the two HIIT conditions [HIITPASS 29.6 ± 3.26 ml.kg.min-1; HIITACT 31.4 ± 4.53 ml.kg.min-1; REC 12.3 ± 1.61 ml.kg.min-1].There was no significant condition x bout interaction.
For the mean VO2 for each bout (Fig 4, panel A), differences were found between conditions for Bout 1 (p < 0.001, F = 491.444), Bout 2 (p < 0.001, F = 161.961), Bout 3 (p < 0.001, F = 77.016) and Bout 4 (p < 0.001, F = 72.269), however no significant differences were found between the two HIIT conditions. For the mean VO2 within conditions, no significant differences were found across bouts, with values remaining relatively similar over time.
Fig 4. Oxygen consumption, mechanical power and heart rate during the four bouts of the three conditions.
(A) VO2. a = significantly different to HIITPASS, bout 1; b = significantly different to HIITACT, bout 1; c = significantly different to HIITPASS, bout 2; d = significantly different to HIITACT, bout 2; e = significantly different to HIITPASS, bout 3; f = significantly different to HIITACT, bout 3; g = significantly different to HIITPASS, bout 4; h = significantly different to HIITACT, bout 4. (B) Mechanical power. a = significantly different to HIITPASS, bout 1; b = significantly different to HIITACT, bout 1; c = significantly different to HIITPASS, bout 2; d = significantly different to HIITACT, bout 2; e = significantly different to HIITPASS, bout 3; f = significantly different to HIITACT, bout 3; g = significantly different to HIITPASS, bout 4; (C) HR. a = significantly different to HIITPASS, bout 1; b = significantly different to HIITACT bout 1; c = significantly different to REC, bout 1; d = significantly different to HIITPASS bout 2; e = significantly different to HIITACT, bout 2; f = significantly different to REC, bout 2; g = significantly different to HIITPASS, bout 3; h = significantly different to HIITACT, bout 3; i = significantly different to HIITPASS, bout 4; j = significantly different to HIITACT, bout 4. Data are mean ± SD. (p >0.05).
Mean VO2peak within conditions and across bouts had the same statistical differences as mean VO2.The differences in VO2 when comparing the REC condition to the HIITPASS and HIITACT conditions were as expected (Fig 4 panel A).
When total oxygen consumption was compared across the three conditions, differences were found [(p < 0.001, F = 78.562) HITTPASS 12.7 ± 2.06 litres; HIITACT 16.0 ± 3.02 litres; REC 8.4 ± 0.79 litres] with significant differences between all conditions.
Mechanical power
For the mean power output, there was a main effect for condition [(p < 0.001, F = 57.636). HIITPASS 374.3 ± 70 W; HIITACT 339.9 ± 72.7 W]. There was no significant condition x bout interaction.
For the mean power output for each bout (Fig 4, panel B), differences were found between conditions for Bout 1 (p = 0.026, F = 6.612), Bout 2 (p < 0.001, F = 87.513), Bout 3 (p < 0.001, F = 24.144) and Bout 4 (p = 0.045, F = 5.118). For the mean power output within conditions, decreases were found across bouts over time (HIITPASS p < 0.001, F = 25.281; HIITACT p < 0.001, F = 22.923).
Heart rate
For the mean HR there was a main effect for condition [(p < 0.001, F = 395.034), however no significant differences were found between the two HIIT conditions: HIITPASS 165 ± 7.6 bpm. HIITACT 166 ± 11.5 bpm. REC 99 ± 11.3 bpm]. There was a condition x bout interaction (p = 0.022)
For the mean HR for each bout (Fig 4, panel C), differences were found between conditions for Bout 1 (p < 0.001, F = 224.796), Bout 2 (p < 0.001, F = 375.081), Bout 3 (p < 0.001 F = 417.149) and Bout 4 (p < 0.001, F = 289.073) however no significant differences were found between the two HIIT conditions. For the mean HR within conditions, increases were found across bouts over time. HIITPASS (p < 0.001, F = 20.234); HIITACT (p < 0.001, F = 16.574); REC (p < 0.001, F = 14.227).
Average HRpeak within conditions and across bouts provided the same statistical differences as mean HR. The differences in HR when comparing the REC condition to the HIITPASS and HIITACT conditions were as expected (Fig 4, panel C).
Discussion
The primary aim of this project was to compare the local (Δ[HHb]) and systemic (VO2) oxygen utilisation, mean power output and heart rate responses during HIIT conditions which included either passive or active recovery. A secondary aim was to compare the relative Δ[HHb] between local muscle and brain tissue sites during HIIT exercise. In support of our hypotheses, there was a significant increase in HHb at the VL site during the 2nd, 3rd and 4th high intensity exercise bouts interspersed with active recovery periods (HIITACT) when compared to bouts interspersed with passive recovery periods (HIITPASS). Also supporting our hypotheses, when including the exercise performed during the active recovery periods, the total VO2 was significantly higher during the HIITACT condition when compared to both the HIITPASS and REC conditions. In opposition to our hypotheses, mean power output during the exercise bouts was significantly higher in the HIITPASS condition when compared to the HIITACT condition. No significant differences were found in Δ[HHb] at the (FH) and (GN) sites, in mean VO2 and in mean HR during the high intensity exercise bouts when comparing HIITPASS and HIITACT. There were significant differences for all dependant variables when comparing the bouts in REC to HIITPASS and HIITACT. These results were expected and validate the use of the REC protocol as a control condition.
Tissue oxygenation
The significantly higher Δ[HHb], indicating increased oxygen utilisation, at the VL site during the second, third and fourth bouts of the HIITACT condition, when compared to the HIITPASS condition could indicate a response to the reduced reoxygenation of the muscle during the active recovery portions, leading to a higher deoxygenation of the muscle tissue during subsequent bouts. This would explain the significantly decreased mean power outputs that occur during the HIITACT bouts, as increased deoxygenation would impair subsequent performance in this large locomotor muscle, potentially due to impaired phosphocreatine (PCr) resynthesis linked to competition for limited oxygen resources [38] or via centralised neuromuscular downregulation in response to the increased rate of biochemical changes [51]. In intermittent sprints [18, 24] the same pattern of reduced performance measures and higher levels of deoxygenation during active recovery conditions has occurred, if insufficient time is provided for a complete physiological recovery [26, 29]. To the contrary, Calbet et al [52] suggest that there may be a functional reserve in oxygen diffusing capacity during exercise, in which situation the higher level of deoxygenation observed during the HIITACT condition would not be considered limiting. Due to differences in the design of the experiments it is difficult to compare the findings of these projects, however it is possible that the oxygen utilisation at the VL site, which is the primary locomotor muscle for cycling [53], is likely to be underestimated by the assessment of whole leg oxygen utilisation via femoral blood samples by Calbet et al.
Additionally, the significantly higher Δ[HHb] in the VL during the bouts of the HIITACT condition cannot be accounted for by the effect of active recovery as a simple additive process (i.e. HIITPASS + REC = HIITACT), as the differences in the Δ[HHb] between the bouts of the two HIIT conditions are higher than the Δ[HHb] during the bouts of the REC condition (Fig 3C).
In the smaller GN muscle of the same leg, which has a lesser role in power production during cycling [53] and a greater percentage of oxidative muscle fibres [54, 55], there were no significant differences in Δ[HHb] between conditions. During exercise, the muscle with a greater percentage of oxidative fibres (GN) would be able to meet the increasing energy requirements, creating little change in HHb values, compared to pre-exercise values. The reasons provided above could also explain why the magnitude of mean Δ[HHb] in the VL muscle was greater than that in the GN muscle in both the HIITPASS and HIITACT conditions.
When comparing Δ[HHB] within conditions, there was no progressive muscle deoxygenation observed in VL and GN from bouts one to four irrespective of recovery type. If exercise effort was maximal, in line with participant instructions to give a maximal effort during each bout, an upper oxygen utilisation limit was reached during each effort at both muscle sites. This has occurred in previous research involving repeat Wingate testing [24]. When the significant reductions in mechanical power are taken into consideration, this indicates that declining muscle performance is associated with repeated maximal levels of oxygen utilisation, providing evidence that maximal oxygen utilisation may not be a limiting factor during HIIT, in sedentary participants. Assessment of the rate of muscle deoxygenation and reoxygenation could yield important information to further delineate differences between HIIT conditions and provide additional information into potential mechanisms involved in site specific oxygen utilisation. Whilst an important future research direction, this assessment was not possible during the current project due to artefact present in the NIRS data during recovery portions of the PASSHIIT condition and the impracticality of cuff occlusion (a common practice when examining deoxygenation and reoxygenation rates [56]) during supramaximal intermittent exercise whilst measuring HHb in multiple limb segments.
The inter individual variability in the VL Δ[HHb] response during the HIITACT condition (Fig 2) was unrelated to the participants power output (i.e. the participants with the highest power outputs did not show the greatest increases in HHb). Additionally, mean Δ[HHb] remained unchanged over time whilst mean power decreases significantly, hence the variability cannot be explained by a simple demand-driven system. A similar degree of variability in the Δ[HHb] response can be seen in the one project to publish individual results [57] or by noting the standard deviation of the Δ[HHb] signal if the method of data calculation and analysis is similar [58]. Currently there is no standard for NIRS instruments or for the method of calculating, analysing and presenting NIRS data [59]. This makes comparison of Δ[HHb] data between projects difficult, even when projects have been performed in similar populations, performing similar HIIT interventions. This in turn limits the ability of researchers to gain a comprehensive understanding of what constitutes a normal NIRS response (or range) during exercise in sedentary populations.
When comparing the FH Δ[HHb] from bout one to bout four, HHb concentrations did not rise significantly until the last bout of both HIIT conditions. This response could be due to the brain being protected from homeostatic disturbances and therefore adequately perfused during the majority of exercise bouts [51]. Late in maximal exercise cerebral vasoconstriction, diminished cerebral blood flow and an increase in cerebral oxygen uptake occur [60, 61]. These factors would explain the late rise in HHb. A similar response is noted in previous intermittent sprint research [42, 62].
Interpretation of differences in the Δ[HHb] data between sites should be made with caution. A significant main effect for site was found, however the NIRS devices measure relative Δ[HHb] from an arbitrary baseline. Parameters that potentially affect NIRS measures, such as blood flow and muscle tension, are not routinely measured in conjunction with HHb. Therefore a lack of significant differences in the Δ[HHb] between the FH and GN sites does not necessarily indicate that the oxygen utilisation responses to the exercise stimulus are the same at these two sites.
Systemic oxygen consumption
Previous research [63] has indicated that active recovery is associated with increased oxygen consumption during exercise bouts when compared to passive recovery. However, no significant differences were found for the HIITPASS and HIITACT conditions when comparing mean VO2 between conditions and across bouts. Our findings are in agreement with other research [29], although that study incorporated open ended intermittent exercise. Potential mechanisms for no difference between conditions could include compensatory decreased oxygen utilisation at non-exercise associated tissue.
The lack of differences across bouts was unexpected, since the response in each subsequent exercise bout is not an isolated exercise period, but would be expected to be, in part, a function of the previous bouts. Therefore an increase in VO2 and HR as a function of time was predicted due to incomplete physiological recovery in the 2 min available to the sedentary individuals between supramaximal exercise bouts. A potential explanation for no difference across bouts could be, if oxygen utilisation is maximised at the muscle (as indicated by the relatively stable Δ[HHb] over time in both VL and GN) a similar pattern would be expected in systemic oxygen utilisation measured at the mouth, and any differences in work across bouts would be met anaerobically. Other potential contributing factors to the results obtained include the significant decrease in mechanical power output across bouts, effectively requiring less aerobic contribution over time, in effect counteracting the increased VO2 due to the cumulative load of the protocol. Furthermore, whilst we did not measure maximal VO2 in this group of participants, it is conceivable that VO2 values in excess of 30 ml.kg.min-1 were maximal in these sedentary individuals, effectively creating a ceiling effect in each and every bout.
Mechanical power
The mean mechanical power achieved during the exercise bouts was lower than that achieved by active individuals performing repeat Wingate tests [64]. Mean mechanical power declined significantly from the first to the fourth bout in both the HIITPASS and HIITACT conditions. This was expected, due to the cumulative fatigue and incomplete ATP repletion and PCr resynthesis that occur during repeat Wingate exercise that include recovery periods that do not allow for complete recovery [24, 28, 65].
The HIITACT bouts were all performed at a lower mean power output when compared to the HIITPASS bouts. To the best of our knowledge no similar HIIT research has been done in sedentary individuals. However, in active populations when comparing the effect of active and passive recovery on mean power output during intermittent sprints, contradictory results have been published. Some researchers found no significant differences [65–67], whilst others have found that passive recovery protocols yielded greater mean power values [24]. Lopez et al [28] found that an active recovery condition resulted in a significantly greater mean power output in later (5th and 6th) Wingate bouts. This finding could be explained by the fact that the longer the exercise session, the greater the contribution of active recovery to metabolite clearance, the correction of a cellular acidosis and resynthesis of PCr, which enabled a lower magnitude decline in mean power production in the later Wingate bouts.
The contradictory findings above could also be explained by differences in the intensity of active recovery utilised in different projects, highlighting the difficulty in comparing HIIT research due to the variety available when designing exercise protocols.
Current evidence suggests that passive recovery can improve subsequent performance when recovery duration is short (15–120 seconds) and / or exercise intensity is high [26]. Our findings in sedentary individuals support this. Choosing an appropriate recovery format (and duration) is an important consideration when considering prescription of HIIT to time poor sedentary individuals, as recovery periods would be of relatively short duration to ensure that the entire HIIT session is in fact shorter than the current moderate intensity exercise recommendations.
The lower mean power output in the HIITACT condition occurred from the first bout. In a sedentary population with no previous experience of repeat Wingate testing, participants potentially adopted a subconscious feedforward pacing strategy to minimise the ‘additional’ discomfort associated with a condition including an active recovery.
In each subsequent bout, mean power output was significantly lower in the HIITACT condition compared to the HIITPASS condition. The local muscle recovery includes the resynthesis of PCr, which relies on oxygen dependant pathways and is strongly correlated with repeat sprint ability [68]. Competition for available oxygen supplies may occur between the processes of PCr resynthesis, lactate oxidation and the oxygen cost of continued exercise itself during active recovery [26, 28, 38, 69, 70]; causing a decrease in performance and power generation when active recovery protocols are adopted. Additionally, in sedentary populations the improved active recovery clearance of metabolites may not occur in an acute session of HIIT due to the fact that the improved clearance of metabolites is an adaptation that occurs with routine exercise training at higher intensities [71]. Due to the untrained state of participants, passive rest periods may allow participants to recover to a greater extent, enabling a lesser reduction in power output over the entirety of the HIIT session.
Heart rate
In both HIIT conditions mean HR rose significantly when comparing bout one to later bouts, in line with findings from previous research [28].
In opposition to previous research [28, 65, 67] showing an active recovery condition is associated with a greater HR response when compared to a passive recovery condition, no significant differences were found between the HIITPASS and HIITACT conditions for mean HR overall and during each bout. This response is however in agreement with other research [29]. The lack of difference found in our project could be explained by the significantly lower power output generated by the sedentary participants during the HIITACT condition. The lower power output could be responsible for a lesser HR response during the HIITACT bouts even though the active recovery portions of the condition kept HR higher during active recovery. During the HIITPASS condition, a higher power output would cause a greater rise in HR, but from a lower starting point due to a greater HR recovery during the passive recovery portions, in effect providing no difference in mean HR during each bout when comparing across conditions.
Limitations
The participants within this group, whilst relatively homogenous in their sedentary behaviour during the project, were heterogeneous in their past exercise behaviours. This variability could potentially have confounded results. Participants needed to maintain a high level of motivation during the repeated maximal HIIT bouts. Individuals with extensive past exercise experience, even if currently sedentary, could rely on past exercise experience to better cope with the inherent discomfort of HIIT. Those with little or no previous exercise experience would potentially adopt either conscious or subconscious pacing strategies in an attempt to reduce the discomfort associated with repeated all-out efforts, despite instructions to perform maximally.
A number of participants reported feelings of dizziness and nausea during the recovery period of the HIITPASS condition. Although these symptoms were sub-clinical in severity, the negative sensations could have impacted on the participant’s exercise behaviours within the study.
Cycling was chosen for the current project due to practical and safety considerations. However, choosing a mode of exercise with a high degree of specificity may have limited the performance of sedentary individuals who would be more accustomed to weight-bearing forms of ambulation. The effect of mode on performance during HIIT in sedentary individuals requires further investigation.
Conclusions
During the HIITACT condition a higher level of deoxygenation in the VL muscle and a lower mean power output occurred, when compared to the HIITPASS condition. This suggests that the higher level of deoxygenation could have contributed to an impaired performance during the HIITACT condition.
However, when compared across bouts within each condition, the level of deoxygenation did not change significantly at either the VL and GN sites from bout one to bout four, when participants were instructed to give a maximal effort. This indicates that oxygen utilisation reached maximal (but different) values at the two sites in each bout. Mean power output decreased over the course of both conditions. It can therefore be concluded that maximal oxygen utilisation is not a limiting factor in sedentary individuals over the course of a HIIT condition, irrespective of the inclusion of active or passive recovery periods.
The level of deoxygenation at the FH site did not increase significantly from pre-exercise values until the fourth bout in both HIIT conditions. This suggests that cerebral oxygenation was adequate until late in supramaximal exercise, possibly due to the importance of maintaining adequate cerebral perfusion.
To our knowledge this is the first research to show that in sedentary participants, the Δ[HHb] levels attained during HIIT exercise varies in different locomotor muscles of the same leg, indicating the specificity of individual muscle oxygen utilisation.
Acknowledgments
The authors would like to thank the participants of this research project, without whom this project would not have been possible.
Data Availability
The relevant data file is available from the Figshare database (DOI: 10.6084/m9.figshare.3399220).
Funding Statement
The authors received no specific funding for this work. This project was supported by an annual research student allocation. This internal university funding arrangement had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Bijnen FCH, Caspersen CJ, Mosterd WL. Physical Inactivity as a Risk Factor for Coronary Heart-Disease—a Who and International-Society and Federation-of-Cardiology Position Statement. B World Health Organ. 1994;72(1):1–4. [PMC free article] [PubMed] [Google Scholar]
- 2.Blair SN, Kohl HW, Paffenbarger RS, Clark DG, Cooper KH, Gibbons LW. Physical-Fitness and All-Cause Mortality—a Prospective-Study of Healthy-Men and Women. Jama-J Am Med Assoc. 1989;262(17):2395–401. 10.1001/jama.262.17.2395 . [DOI] [PubMed] [Google Scholar]
- 3.Guthold R, Ono T, Strong KL, Chatterji S, Morabia A. Worldwide variability in physical inactivity a 51-country survey. Am J Prev Med. 2008;34(6):486–94. 10.1016/j.amepre.2008.02.013 . [DOI] [PubMed] [Google Scholar]
- 4.Australian Health Survey: First Results, 2011–12. In: Statistics ABo, editor. 2011–2012.
- 5.Tucker JM, Welk GJ, Beyler NK. Physical Activity in US Adults Compliance with the Physical Activity Guidelines for Americans. Am J Prev Med. 2011;40(4):454–61. 10.1016/j.amepre.2010.12.016 . [DOI] [PubMed] [Google Scholar]
- 6.Chastin SFM, Dall PM, Tigbe WW, Grant MP, Ryan CG, Rafferty D, et al. Compliance with physical activity guidelines in a group of UK-based postal workers using an objective monitoring technique. Eur J Appl Physiol. 2009;106(6):893–9. 10.1007/s00421-009-1090-x . [DOI] [PubMed] [Google Scholar]
- 7.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, Mcdowell M. Physical activity in the United States measured by accelerometer. Med Sci Sport Exer. 2008;40(1):181–8. 10.1249/mss.0b013e31815a51b3 . [DOI] [PubMed] [Google Scholar]
- 8.Pescatello LS, American College of Sports Medicine. ACSM's guidelines for exercise testing and prescription 9th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health; 2013. p. p. [DOI] [PubMed] [Google Scholar]
- 9.Strazdins L, Broom DH, Banwell C, McDonald T, Skeat H. Time limits? Reflecting and responding to time barriers for healthy, active living in Australia. Health Promot Int. 2011;26(1):46–54. 10.1093/heapro/daq060 . [DOI] [PubMed] [Google Scholar]
- 10.Gillen JB, Gibala MJ. Is high-intensity interval training a time-efficient exercise strategy to improve health and fitness? Appl Physiol Nutr Me. 2014;39(3):409–12. 10.1139/apnm-2013-0187 . [DOI] [PubMed] [Google Scholar]
- 11.Kessler HS, Sisson SB, Short KR. The potential for high-intensity interval training to reduce cardiometabolic disease risk. Sports Med. 2012;42(6):489–509. 10.2165/11630910-000000000-00000 . [DOI] [PubMed] [Google Scholar]
- 12.Nybo L, Sundstrup E, Jakobsen MD, Mohr M, Hornstrup T, Simonsen L, et al. High-intensity training versus traditional exercise interventions for promoting health. Med Sci Sport Exer. 2010;42(10):1951–8. 10.1249/MSS.0b013e3181d99203 . [DOI] [PubMed] [Google Scholar]
- 13.Gibala MJ, Little JP, MacDonald MJ, Hawley JA. Physiological adaptations to low-volume, high-intensity interval training in health and disease. J Physiol-London. 2012;590(5):1077–84. 10.1113/jphysiol.2011.224725 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tjønna AE, Lee SJ, Rognmo O, Stolen TO, Bye A, Haram PM, et al. Aerobic interval training versus continuous moderate exercise as a treatment for the metabolic syndrome—A pilot study. Circulation. 2008;118(4):346–54. 10.1161/Circulationaha.108.772822 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weston KS, Wisloff U, Coombes JS. High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: a systematic review and meta-analysis. Brit J Sport Med. 2014;48(16):1227–U52. 10.1136/bjsports-2013-092576 . [DOI] [PubMed] [Google Scholar]
- 16.Russell AP, Foletta VC, Snow RJ, Wadley GD. Skeletal muscle mitochondria: A major player in exercise, health and disease. Bba-Gen Subjects. 2014;1840(4):1276–84. 10.1016/j.bbagen.2013.11.016 . [DOI] [PubMed] [Google Scholar]
- 17.Jacobs RA, Fluck D, Bonne TC, Burgi S, Christensen PM, Toigo M, et al. Improvements in exercise performance with high-intensity interval training coincide with an increase in skeletal muscle mitochondrial content and function. J Appl Physiol. 2013;115(6):785–93. 10.1152/japplphysiol.00445.2013 . [DOI] [PubMed] [Google Scholar]
- 18.Buchheit M, Cormie P, Abbiss CR, Ahmaidi S, Nosaka KK, Laursen PB. Muscle Deoxygenation during Repeated Sprint Running: Effect of Active vs. Passive Recovery. Int J Sports Med. 2009;30(6):418–25. 10.1055/s-0028-1105933 . [DOI] [PubMed] [Google Scholar]
- 19.Buchheit M, Hader K, Mendez-Villanueva A. Tolerance to high-intensity intermittent running exercise: do oxygen uptake kinetics really matter? Front Physiol. 2012;3:406 10.3389/fphys.2012.00406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Buchheit M, Abbiss CR, Peiffer JJ, Laursen PB. Performance and physiological responses during a sprint interval training session: relationships with muscle oxygenation and pulmonary oxygen uptake kinetics. Eur J Appl Physiol. 2012;112(2):767–79. 10.1007/s00421-011-2021-1 . [DOI] [PubMed] [Google Scholar]
- 21.Kime R, Im J, Moser D, Lin YQ, Nioka S, Katsumura T, et al. Reduced heterogeneity of muscle deoxygenation during heavy bicycle exercise. Med Sci Sport Exer. 2005;37(3):412–7. 10.1249/01.Mss.0000155401.81284.76 . [DOI] [PubMed] [Google Scholar]
- 22.Koga S, Poole DC, Ferreira LF, Whipp BJ, Kondo N, Saitoh T, et al. Spatial heterogeneity of quadriceps muscle deoxygenation kinetics during cycle exercise. J Appl Physiol. 2007;103(6):2049–56. 10.1152/japplphysiol.00627.2007 . [DOI] [PubMed] [Google Scholar]
- 23.Chin LM, Kowalchuk JM, Barstow TJ, Kondo N, Amano T, Shiojiri T, et al. The relationship between muscle deoxygenation and activation in different muscles of the quadriceps during cycle ramp exercise. Journal of applied physiology. 2011;111(5):1259–65. 10.1152/japplphysiol.01216.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dupont G, Moalla W, Matran R, Berthoin S. Effect of short recovery intensities on the performance during two wingate tests. Med Sci Sport Exer. 2007;39(7):1170–6. 10.1249/mss.0b013e31804c9976 . [DOI] [PubMed] [Google Scholar]
- 25.Buchheit M, Laursen PB. High-Intensity Interval Training, Solutions to the Programming Puzzle Part I: Cardiopulmonary Emphasis. Sports Med. 2013;43(5):313–38. 10.1007/s40279-013-0029-x . [DOI] [PubMed] [Google Scholar]
- 26.Ohya T, Aramaki Y, Kitagawa K. Effect of Duration of Active or Passive Recovery on Performance and Muscle Oxygenation during Intermittent Sprint Cycling Exercise. Int J Sports Med. 2013;34(7):616–22. 10.1055/s-0032-1331717 . [DOI] [PubMed] [Google Scholar]
- 27.Spierer DK, Goldsmith R, Baran DA, Hryniewicz K, Katz SD. Effects of active vs. passive recovery on work performed during serial supramaximal exercise tests. Int J Sports Med. 2004;25(2):109–14. 10.1055/s-2004-819954 . [DOI] [PubMed] [Google Scholar]
- 28.Lopez EID, Smoliga JM, Zavorsky GS. The Effect of Passive Versus Active Recovery on Power Output Over Six Repeated Wingate Sprints. Res Q Exerc Sport. 2014;85(4):519–26. 10.1080/02701367.2014.961055 . [DOI] [PubMed] [Google Scholar]
- 29.Dupont G, Moalla W, Guinhouya C, Ahmaidi S, Berthoin S. Passive versus active recovery during high-intensity intermittent exercises. Med Sci Sport Exer. 2004;36(2):302–8. 10.1249/01.Mss.0000113477.11431.59 . [DOI] [PubMed] [Google Scholar]
- 30.Barnes J, Behrens TK, Benden ME, Biddle S, Bond D, Brassard P, et al. Letter to the Editor: Standardized use of the terms "sedentary" and "sedentary behaviours". Appl Physiol Nutr Me. 2012;37(3):540–2. 10.1139/H2012-024 . [DOI] [PubMed] [Google Scholar]
- 31.Levy ML, Quanjer PH, Booker R, Cooper BG, Holmes S, Small I, et al. Diagnostic spirometry in primary care: Proposed standards for general practice compliant with American Thoracic Society and European Respiratory Society recommendations: a General Practice Airways Group (GPIAG)1 document, in association with the Association for Respiratory Technology & Physiology (ARTP)2 and Education for Health3 1 www.gpiag.org 2 www.artp.org 3 www.educationforhealth.org.uk. Prim Care Respir J. 2009;18(3):130–47. 10.4104/pcrj.2009.00054 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Burgomaster KA, Howarth KR, Phillips SM, Rakobowchuk M, MacDonald MJ, Mcgee SL, et al. Similar metabolic adaptations during exercise after low volume sprint interval and traditional endurance training in humans. J Physiol-London. 2008;586(1):151–60. 10.1113/jphysiol.2007.142109. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gibala MJ, McGee SL. Metabolic adaptations to short-term high-intensity interval training: a little pain for a lot of gain? Exerc Sport Sci Rev. 2008;36(2):58–63. 10.1097/JES.0b013e318168ec1f . [DOI] [PubMed] [Google Scholar]
- 34.Burgomaster KA, Hughes SC, Heigenhauser GJ, Bradwell SN, Gibala MJ. Six sessions of sprint interval training increases muscle oxidative potential and cycle endurance capacity in humans. J Appl Physiol. 2005;98(6):1985–90. 10.1152/japplphysiol.01095.2004 . [DOI] [PubMed] [Google Scholar]
- 35.Buchheit M, Mendez-Villanueva A, Quod M, Quesnel T, Ahmaidi S. Improving Acceleration and Repeated Sprint Ability in Well-Trained Adolescent Handball Players: Speed Versus Sprint Interval Training. Intj Sport Physiol. 2010;5(2):152–64. . [DOI] [PubMed] [Google Scholar]
- 36.Gibala MJ, Little JP, van Essen M, Wilkin GP, Burgomaster KA, Safdar A, et al. Short-term sprint interval versus traditional endurance training: similar initial adaptations in human skeletal muscle and exercise performance. J Physiol. 2006;575(Pt 3):901–11. 10.1113/jphysiol.2006.112094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McArdle WD, Katch FI, Katch VL. Exercise physiology: nutrition, energy, and human performance 7th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health; 2010. p. p. [Google Scholar]
- 38.Spencer M, Bishop D, Dawson B, Goodman C, Duffield R. Metabolism and performance in repeated cycle sprints: active versus passive recovery. Med Sci Sport Exer. 2006;38(8):1492–9. 10.1249/01.mss.0000228944.62776.a7 . [DOI] [PubMed] [Google Scholar]
- 39.Bonen A, Belcastro AN. Comparison of self-selected recovery methods on lactic acid removal rates. Med Sci Sport Exer. 1976;8(3):176–8. . [DOI] [PubMed] [Google Scholar]
- 40.Belcastro AN, Bonen A. Lactic acid removal rates during controlled and uncontrolled recovery exercise. J Appl Physiol. 1975;39(6):932–6. . [DOI] [PubMed] [Google Scholar]
- 41.Prieur F, Mucci P. Effect of high-intensity interval training on the profile of muscle deoxygenation heterogeneity during incremental exercise. Eur J Appl Physiol. 2013;113(1):249–57. 10.1007/s00421-012-2430-9 . [DOI] [PubMed] [Google Scholar]
- 42.Smith KJ, Billaut F. Influence of cerebral and muscle oxygenation on repeated-sprint ability. Eur J Appl Physiol. 2010;109(5):989–99. 10.1007/s00421-010-1444-4 . [DOI] [PubMed] [Google Scholar]
- 43.Buchheit M, Ufland P, Haydar B, Laursen PB, Ahmaidi S. Reproducibility and sensitivity of muscle reoxygenation and oxygen uptake recovery kinetics following running exercise in the field. Clin Physiol Funct Imaging. 2011;31(5):337–46. 10.1111/j.1475-097X.2011.01020.x . [DOI] [PubMed] [Google Scholar]
- 44.Jones AM, Davies RC, Ferreira LF, Barstow TJ, Koga S, Poole DC. Reply to Quaresima and Ferrari. J Appl Physiol. 2009;107(1):372–3. 10.1152/japplphysiol.00314.2009 [DOI] [Google Scholar]
- 45.Wang L, Yoshikawa T, Hara T, Nakao H, Suzuki T, Fujimoto S. Which common NIRS variable reflects muscle estimated lactate threshold most closely? Appl Physiol Nutr Me. 2006;31(5):612–20. Epub 2006/11/18. 10.1139/h06-069 . [DOI] [PubMed] [Google Scholar]
- 46.Adami A, Koga S, Kondo N, Cannon DT, Kowalchuk JM, Amano T, et al. Changes in whole tissue heme concentration dissociates muscle deoxygenation from muscle oxygen extraction during passive head-up tilt. J Appl Physiol. 2015;118(9):1091–9. 10.1152/japplphysiol.00918.2014 . [DOI] [PubMed] [Google Scholar]
- 47.Grassi B, Pogliaghi S, Rampichini S, Quaresima V, Ferrari M, Marconi C, et al. Muscle oxygenation and pulmonary gas exchange kinetics during cycling exercise on-transitions in humans. J Appl Physiol. 2003;95(1):149–58. 10.1152/japplphysiol.00695.2002 . [DOI] [PubMed] [Google Scholar]
- 48.Macfarlane DJ, Wu HL. Inter-unit variability in two ParvoMedics TrueOne 2400 automated metabolic gas analysis systems. Eur J Appl Physiol. 2013;113(3):753–62. 10.1007/s00421-012-2483-9 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Austin KG, Daigle KA, Patterson P, Cowman J, Chelland S, Haymes EM. Reliability of near-infrared spectroscopy for determining muscle oxygen saturation during exercise. Res Q Exerc Sport. 2005;76(4):440–9. . [DOI] [PubMed] [Google Scholar]
- 50.Muthalib M, Millet GY, Quaresima V, Nosaka K. Reliability of near-infrared spectroscopy for measuring biceps brachii oxygenation during sustained and repeated isometric contractions. J Biomed Opt. 2010;15(1). Artn 017008 10.1117/1.3309746 . [DOI] [PubMed] [Google Scholar]
- 51.Amann M, Calbet JAL. Convective oxygen transport and fatigue. J Appl Physiol. 2008;104(3):861–70. 10.1152/japplphysiol.01008.2007 . [DOI] [PubMed] [Google Scholar]
- 52.Calbet JAL, Losa-Reyna J, Torres-Peralta R, Rasmussen P, Ponce-Gonzalez JG, Sheel AW, et al. Limitations to oxygen transport and utilization during sprint exercise in humans: evidence for a functional reserve in muscle O-2 diffusing capacity. J Physiol-London. 2015;593(20):4649–64. 10.1113/Jp270408 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bijker KE, de Groot G, Hollander AP. Differences in leg muscle activity during running and cycling in humans. Eur J Appl Physiol. 2002;87(6):556–61. 10.1007/s00421-002-0663-8 . [DOI] [PubMed] [Google Scholar]
- 54.Hagström-Toft E, Qvisth V, Nennesmo I, Ryden M, Bolinder H, Enoksson S, et al. Marked heterogeneity of human skeletal muscle lipolysis at rest. Diabetes. 2002;51(12):3376–83. 10.2337/diabetes.51.12.3376 . [DOI] [PubMed] [Google Scholar]
- 55.Houmard JA, Weidner ML, Gavigan KE, Tyndall GL, Hickey MS, Alshami A. Fiber type and citrate synthase activity in the human gastrocnemius and vastus lateralis with aging. J Appl Physiol. 1998;85(4):1337–41. . [DOI] [PubMed] [Google Scholar]
- 56.Buchheit M, Ufland P. Effect of endurance training on performance and muscle reoxygenation rate during repeated-sprint running. European journal of applied physiology. 2011;111(2):293–301. 10.1007/s00421-010-1654-9 . [DOI] [PubMed] [Google Scholar]
- 57.Jones B, Hamilton DK, Cooper CE. Muscle oxygen changes following Sprint Interval Cycling training in elite field hockey players. Plos One. 2015;10(3):e0120338 10.1371/journal.pone.0120338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Spencer MD, Murias JM, Lamb HP, Kowalchuk JM, Paterson DH. Are the parameters of VO2, heart rate and muscle deoxygenation kinetics affected by serial moderate-intensity exercise transitions in a single day? Eur J Appl Physiol. 2011;111(4):591–600. 10.1007/s00421-010-1653-x . [DOI] [PubMed] [Google Scholar]
- 59.Ferrari M, Muthalib M, Quaresima V. The use of near-infrared spectroscopy in understanding skeletal muscle physiology: recent developments. Philos T R Soc A. 2011;369(1955):4577–90. 10.1098/rsta.2011.0230. WOS:000296558900014. [DOI] [PubMed] [Google Scholar]
- 60.Rooks CR, Thom NJ, McCully KK, Dishman RK. Effects of incremental exercise on cerebral oxygenation measured by near-infrared spectroscopy: a systematic review. Prog Neurobiol. 2010;92(2):134–50. 10.1016/j.pneurobio.2010.06.002 . [DOI] [PubMed] [Google Scholar]
- 61.Subudhi AW, Lorenz MC, Fulco CS, Roach RC. Cerebrovascular responses to incremental exercise during hypobaric hypoxia: effect of oxygenation on maximal performance. Am J Physiol-Heart C. 2008;294(1):H164–H71. 10.1152/ajpheart.01104.2007 . [DOI] [PubMed] [Google Scholar]
- 62.Shibuya K, Tanaka J, Kuboyama N, Ogaki T. Cerebral oxygenation during intermittent supramaximal exercise. Respir Physiol Neurobiol. 2004;140(2):165–72. 10.1016/j.resp.2003.11.004 . [DOI] [PubMed] [Google Scholar]
- 63.Bogdanis GC, Nevill ME, Lakomy HKA, Graham CM, Louis G. Effects of active recovery on power output during repeated maximal sprint cycling. Eur J Appl Physiol O. 1996;74(5):461–9. 10.1007/Bf02337727 . [DOI] [PubMed] [Google Scholar]
- 64.Jaafar H, Rouis M, Coudrat L, Attiogbe E, Vandewalle H, Driss T. Effects of Load on Wingate Test Performances and Reliability. J Strength Cond Res. 2014;28(12):3462–8. 10.1519/JSC.0000000000000575 [DOI] [PubMed] [Google Scholar]
- 65.Wahl P, Mathes S, Kohler K, Achtzehn S, Bloch W, Mester J. Effects of active vs. passive recovery during Wingate-based training on the acute hormonal, metabolic and psychological response. Growth Horm Igf Res. 2013;23(6):201–8. 10.1016/j.ghir.2013.07.004 . [DOI] [PubMed] [Google Scholar]
- 66.Connolly DA, Brennan KM, Lauzon CD. Effects of active versus passive recovery on power output during repeated bouts of short term, high intensity exercise. J Sport Sci Med. 2003;2(2):47–51. [PMC free article] [PubMed] [Google Scholar]
- 67.Bishop D, Ruch N, Paun V. Effects of active versus passive recovery on thermoregulatory strain and performance in intermittent-sprint exercise. Med Sci Sport Exer. 2007;39(5):872–9. 10.1249/mss.0b013e318031b026 . [DOI] [PubMed] [Google Scholar]
- 68.Bogdanis GC, Nevill ME, Boobis LH, Lakomy HK, Nevill AM. Recovery of power output and muscle metabolites following 30 s of maximal sprint cycling in man. J Physiol. 1995;482 (Pt 2):467–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Spencer M, Dawson B, Goodman C, Dascombe B, Bishop D. Performance and metabolism in repeated sprint exercise: effect of recovery intensity. Eur J Appl Physiol. 2008;103(5):545–52. 10.1007/s00421-008-0749-z . [DOI] [PubMed] [Google Scholar]
- 70.Haseler LJ, Hogan MC, Richardson RS. Skeletal muscle phosphocreatine recovery in exercise-trained humans is dependent on O-2 availability. J Appl Physiol. 1999;86(6):2013–8. . [DOI] [PubMed] [Google Scholar]
- 71.Laursen PB, Jenkins DG. The scientific basis for high-intensity interval training: optimising training programmes and maximising performance in highly trained endurance athletes. Sports Med. 2002;32(1):53–73. . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The relevant data file is available from the Figshare database (DOI: 10.6084/m9.figshare.3399220).