Abstract
Background: This study examined the effects of dry needling on chronic heel pain due to plantar fasciitis.
Methods: During this single-blinded clinical trial, 20 eligible patients were randomized into two groups: A case group treated with dry needling and a control group. Patients’ plantar pain severity, (using modified visual analog scale [VAS] scoring system), range of motion of ankle joint in dorsiflexion [ROMDF] and plantar extension[ROMPE] and foot function index (using standard questionnaires of SEM5 and MDC7) were assessed at baseline, four weeks after intervention and four weeks after withdrawing treatment. Independent sample t-test, Mann-Whitney U test, paired t-test, Wilcoxon signed rank tests, and chi square test were used for data analysis.
Results: The mean VAS scores in the case group was significantly lower than the control group after four weeks of intervention (p<0.001). Comparison of the ROMDF and ROMPE did not reveal any significant changes after four weeks of intervention in the case and control groups (p=0.7 and p=0.65, respectively). The mean of MDC7 and SEM5 scores in the case group were significantly lower than the control group following four weeks of intervention (p<0.001).
Conclusion: Despite the insignificant effect on ROMDF and ROMPE, trigger point dry needling, by improving the severity of heel pain, can be used as a good alternative option before proceeding to more invasive therapies of plantar fasciitis.
Keywords: Plantar fasciitis, Myofascial trigger points, Chronic heel pain, Dry needling
Introduction
Heel pain due to plantar fasciitis is characterized by pain and tenderness centered under the medial tubercle of the calcaneus on weight-bearing surface, specifically immediately after rest such as getting out of bed in the morning (1). It is one of the most common foot disorders encountered by foot and ankle specialists that affects about 10% of people in their life, and it is responsible for approximately one million physician visits annually (2).
Despite the high prevalence of plantar fasciitis and its detrimental impact on quality of life (2-4), the optimal treatment for this disorder is still unclear (5). Numerous conventional treatments are currently used to treat plantar fasciitis including calf stretching, foot taping, manual therapy (joint mobilization and manipulation; mobilization of soft tissue near sites of nerve entrapment and passive neural mobilization techniques), foot orthosis, oral and injectable anti-inflammatories, and night splints (5,6). Surgery is recommended as a last option and is usually done after failure of at least six months of conservative therapy (7). However, these modalities may be associated with serious side effects (8), and challenges toward an alternative adjunctive treatment are thus demanded. Acupuncture and dry needling are increasingly being used to treat heel pain, as many other musculoskeletal pain conditions (9,10).
Dry needling and acupuncture as alternative and less invasive procedures, stimulate myofascial trigger points [MTPs] (11-13). Dry needling has been shown to alter the biochemical environment surrounding a MTP and reduce spontaneous electrical activity within the MTP region of skeletal muscle (14,15). This method is one of the most popular modalities with minimal side effects used for treating chronic pains. There are a few published studies (16-19) with some methodological limitations, which have examined the effectiveness of trigger point needling in relieving plantar heel pain. In addition, based on the current reporting standards (20), the mentioned studies lack a scientific rigor for outcome measurement and study design, and one of the studies is a case report. We concluded that conducting further research is necessary to establish the efficacy of dry needling for heel pain.
This study was conducted to examine the effects of dry needling in patients with chronic heel pain due to the plantar fasciitis.
Methods
During this single-blinded randomized clinical trial, 20 consecutive patients who referred to the Physical Medicine and Rehabilitation Outpatient Clinic of Shohada Hospital of Tabriz were enrolled from March 2010 to February 2011.
Informed written consent was obtained from all the participants, and the Ethics Committee of Tabriz University of Medical Sciences (TUMS) approved the study protocol, which was in compliance with Helsinki declaration. The trial was registered in the Iranian Clinical Trial Registry with the identification number of 2011 06104641N4.
Patients who met the following criteria were included in the study (10,21,22): Those older than 18 years; patients with the ability to understand the instructions or complete the questionnaires; diagnosis of plantar heel pain using the clinical guidelines linked to the International Classification of Function, Disability and Health from the Orthopedic Section of the American Physical Therapy Association (5); experiencing pain for more than one month; having a heel pain on the first step during the last week with the rate of at least 40 mm on visual analogue scale; attending the Physical Medicine and Rehabilitation Outpatient Clinic of Shohada Hospital of Tabriz for initial assessment and being randomly assigned into one of the study groups; accepting to discontinue analgesics, non-steroidal anti-inflammatory medications and oral/topical paracetamol for at least 14 days prior to the initial evaluation and during the study period (four weeks after the final treatment); walking 50 meters without any support; having MTPs on initial physical examination on plantar and calf muscles; and absence of Raynaud's disease.
Exclusion criteria of the study were as follows: Refuse needling and routine physical therapy (e.g., cooling, stretch, massage therapy and/or footwear modifications),; diagnosis of coagulopathy or taking anticoagulants except for acetylsalicylic acid at dosages up to 325 mg/day; pregnancy; dermatological disease in the area of needling; previous history of dry needling or acupuncture; treatment for plantar heel pain within four weeks prior to the study; inability to understand the instructions or complete the questionnaires; presence of peripheral arterial vascular disease; history of connective tissue disease; presence of a chronic medical condition like rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, septic arthritis, neurological abnormalities, sciatica, and/or chronic pain; history of plantar fascia surgery; history of injection therapy in the heel during the previous three months; and known hypersensitivity to metals (10,21,22).
Twenty eligible patients were randomized using closed mail pockets containing A or B letters into two study groups: The case group received dry needling but the control group did not. All the participants were trained for plantar muscles calf massage and stretching at home. Plantar massage was done with a cold can under the foot with the patient rolling his/her foot on the can with pressure; and calf muscle massage was done with the patient crossing his/her foot on the other and pressuring it by thumb and index fingers massaging the muscle. In addition, 50 mg diclofenac sodium per 12 hours and orthostatic plantar pad were administered for all patients.
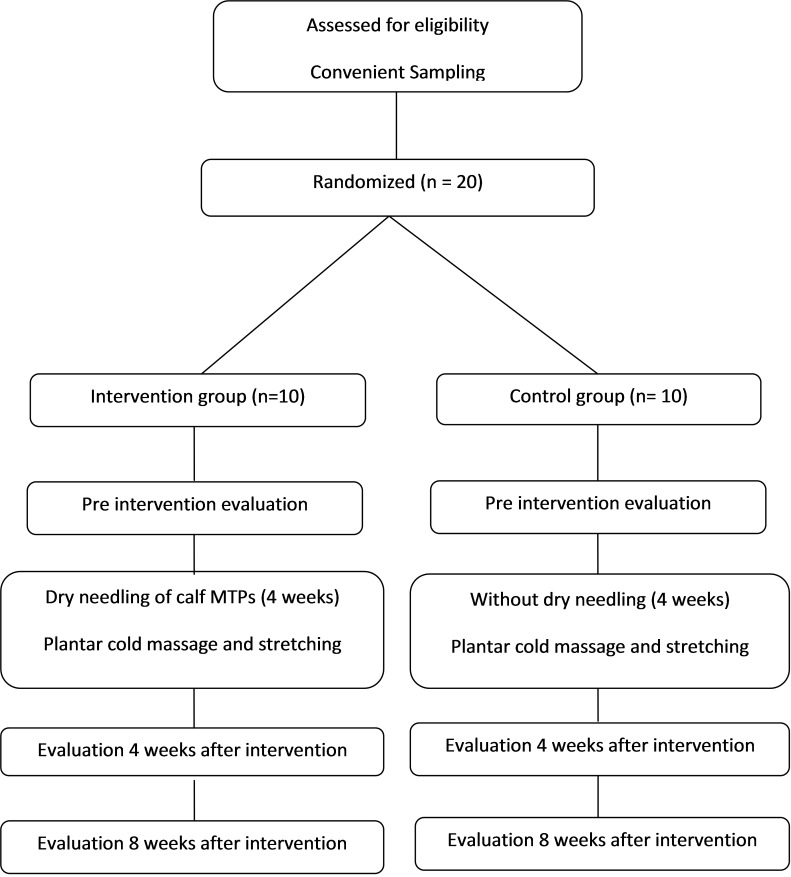
In addition to the routine treatments, the case group received dry needling of MTPs one session per week (10,18) for four consecutive weeks. Diagnosis of MTPs was based on detecting a tender spot or nodule in a taut band of skeletal muscle. Dry needling was based on calf muscles trigger points, especially four trigger points of gastrocnemius muscle (Fig. 1) and such decisions were made by one physical medicine and rehabilitation specialist with five years of experience in this field (23). In the context of this study, dry needling involved the stimulation of MTPs, using a dry needle with the length of 30-50mm and diameter of 0.6mm. Treatment was conducted within a 30-minute timeframe. The participants were lying flat, and following the insertion, the needle was partially withdrawn and advanced repeatedly to produce an appropriate response. If the participant were sensitive to insertion of the needle, the manipulation would be reduced. If this action was insufficient to reduce the painful stimulus, the manipulation would be ceased and the needle left in situ. The needle was left in the muscle for as long as it was needed to produce an appropriate response and was being tolerated by the participant. Appropriate response was based on twitch response, in which needle movements were repeated until the twitch response of the muscle was disappeared. Once this has occurred, the needle was left in the situ for five minutes. This allowed sufficient time for the stimulus to subside in sensitive participants.
Fig. 1 .
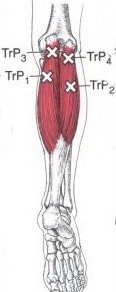
Illustration of Four Myofascial Trigger Points (MTPs) of Gastrocnemius Muscle
The effects of dry needling were evaluated at three time points of baseline, four weeks after intervention and four weeks after withdrawing treatment. Figure 2 demonstrates the study flow diagram.
Fig. 2 .
A Flow Diagram of the Study Protocol
The severity of pain was measured using a modified visual analog scale [VAS] scoring method ranging from none to an extreme amount of pain (24). Operationally, a VAS is usually a horizontal line with 100 mm length, anchored by word descriptors at each end as illustrated in Figure 3. The patients mark a point on the line that they feel represents their perception of their current state, and then the VAS score is determined by measuring, in millimeters, the left hand end of the line to the point that the patient had marked. Patients’ plantar pain severity was assessed using VAS at baseline, four weeks after intervention and four weeks after withdrawing treatment.
Fig. 3 .
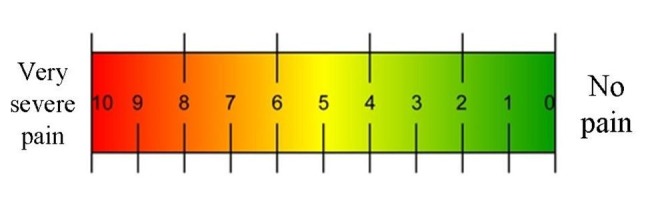
Illustration of Visual Analog Scale, VAS (The VAS is usually a horizontal line with 10 cm length)
Range of motion of ankle joint in dorsiflexion (ROMDF) and plantar extension (ROMPE) was measured at baseline, four weeks after intervention and four weeks after withdrawing treatment.
Foot function index [FFI] was studied using a validated questionnaire developed to measure the impact of foot pathology on function in terms of pain, disability and activity restriction. The questionnaire gave the scores of 7 (MDC7) for minimal detectable changes and 5 for standard error measurement (SEM5). Pain was evaluated in five items, and disability and activity restriction were scored by nine and three items, respectively (25,26). Statistically significant decrement in VAS and other outcome measurements was considered as effectiveness in the two groups.
Statistical analyses were performed using SPSS 13. The results are shown as mean ± standard deviation, The Kolmogorov-Smirnov test was used to check the normality. Independent sample t-test or Mann-Whitney U test, paired t-test or Wilcoxon signed rank tests, and chi square test were utilized to assess the differences between the stages. A p value of less than 0.05 was considered significant.
Results
Demographic characteristics of the patients in both groups are listed in Table 1. Male to female ratio was 3 to 7 in cases and 4 to 6 in controls (Chi Square, p<0.05). No significant difference was detected between the cases and controls in the mean age, sex distribution and number of trigger points. There was not any drop out or loss to follow up during the study.
Table 1. Demographic Characteristics, VAS Scores, SEM5, MDC7, Ankle joint's ROMDF and ROMPE of the Patients in the Two Groups .
|
Case group Mean±SD |
Control group Mean±SD |
p | ||
| Age (Year) | 50.3±9.0 | 50.9±8.9 | 0.88 | |
| Trigger point (No) | 1 | ------- | ------- | 1 |
| 2 | 2 (20%) | 2 (20%) | ||
| 3 | 5 (50%) | 5 (50%) | ||
| 4 | 3(30%) | 3(30%) | ||
| VAS | A | 8.2±0.7 | 7.6±0.9 | 0.14 |
| B | 2.6±1.5 | 6.6±1.2 | <0.01 | |
| C | 3.0±1.2 | 3.5±1.3 | 0.36 | |
| SEM5, MDC7 | A | 61.0±10.3 | 50.9±14.0 | 0.08* |
| B | 25.9±7.8 | 43.2±13.3 | 0.003* | |
| C | 27.3±6.6 | 26.1±10.7 | 0.81* | |
| Ankle ROMDF (degree) | A | 11.9±3.4 | 6.3±4.8 | 0.008* |
| B | 14.5±4.3 | 9.1±5.3 | 0.02* | |
| C | 17.5±3.5 | 15.8±5.3 | 0.44* | |
| Ankle ROMPE (degree) | A | 21±5.6 | 26.2±4.7 | 0.03* |
| B | 21.5±6.2 | 26.6±4.3 | 0.05* | |
| C | 24±6.1 | 28.3±5.5 | 0.12* |
VAS: Visual analog scale; ROMDF: Range of motion in dorsiflexion; ROMPE: Range of motion in plantar extension; SEM5: Standard error measurement 5; MDC7: Minimal detectable changes 7; A: Baseline; B: Four weeks after intervention; C: Four weeks after withdrawing treatment; * independent or Man Whitney U test was used accordingly
Intragroup Findings in the Case Group after Intervention
Based on paired t-test, the mean VAS scores was significantly decreased after four weeks of intervention (p<0.001) and four weeks of cessation period (p<0.001). The mean ROMDF of ankle joint was significantly increased both after four weeks of intervention (p<0.001) and four weeks of cessation period (p<0.001). Although the change in ROMPE of ankle joint was not significant after four weeks of intervention (p=0.34), the mean ROMPE of ankle joint was significantly increased after four weeks of cessation period (p<0.04).
Based on the Wilcoxon test, the mean of MDC7 and SEM5 scores were significantly decreased after four weeks of intervention (P<0.001). No significant changes were found in the mean of MDC7 and SEM5 scores (p>0.05) after four weeks of cessation period, but they were lower than baseline scores (p<0.001).
Intragroup Findings in the Control Group after Intervention
Based on the paired t-test, the mean VAS scores was significantly decreased after four weeks of intervention (p=0.002) and four weeks of cessation period (p<0.001).
The mean ROMDF of ankle joint was significantly increased both after four weeks of intervention (p=0.01) and four weeks of cessation period (p<0.001). The change in ROMPE of ankle joint was not significant after four weeks of intervention (p=0.18), but the mean ROMPE of ankle joint significantly increased after four weeks of cessation period (p<0.03).
Comparison of the Case and Control Groups
Independent t-test revealed that the mean VAS scores in the case group was significantly lower than the control group after four weeks of intervention (p<0.001).
Comparison of the ROMDF and ROMPE of ankle joint did not reveal any significant differences between the case and control groups after four weeks of intervention (p=0.7 and p=0.65, respectively).
Based on the Mann-Whitney U test, the mean of MDC7 and SEM5 scores in the case group was significantly lower than the control group (p<0.001) following four weeks intervention.
Discussion
Treatment options for plantar fasciitis can be divided into conservative and surgical measures. There is a professional consensus that 70–90% of heel pain patients can be managed by non-surgical modalities (27). Although a variety of treatment options are available for pain reduction and improving joint range of motion in patients with plantar fasciitis, there is little convincing evidence to support these various treatments (28,29).
In recent years, dry needling and/or injection of therapeutic medications (local anesthetics, steroids, botulinum toxin A) have been studied for plantar fasciitis treatment. Of these treatment options, steroid injections are more commonly used in treating acute and chronic plantar fasciitis, especially when more conservative managements are unsuccessful. Randomized controlled trials have shown that this method has some short-term benefits (6). A prospective randomized study that evaluated a variety of treatments including autologous blood injection, lidocaine needling, triamcinolone injection, and triamcinolone needling, reported superior results in triamcinolone group (30). Possible risks associated with corticosteroid injection include fat pad atrophy and plantar fascia rupture (22). A quasi-experimental trial using 1% lidocaine injections of MTPs has found a reduction in pain when combined with physical therapy (31). Moreover, few studies have found that Botulinum toxin A injection resulted in significant pain improvement in short and long terms (32).
Physical medicine and rehabilitation specialists increasingly use dry needling, which involves stimulation of MTPs, as an alternative treatment option for musculoskeletal pain. Myofascial trigger point (MTP) is a hyperirritable spot in skeletal muscle tissue, and it is associated with a hypersensitive palpable nodule in a taut band and may result in characteristic tenderness, referred pain, motor dysfunction and even autonomic phenomena. There is no clear guideline to use dry needling for plantar fasciitis (10).
Collectively, this study revealed that despite ineffectiveness in the range of motion of the ankle joint, dry needling improved the severity of pain, evaluated by VAS, MDC7 and SEM5 measurements.
A meta-analysis of randomized controlled trials (33) found that dry needling and acupuncture of MTPs was not significantly superior to placebo in treating musculoskeletal pains. However, this study just included four trials sand it suffers from limited sample size, poor quality and there was a marked statistical heterogeneity in its data pool, which precludes making definitive conclusions.
Only a few studies were conducted on the effectiveness of dry needling in plantar heel pain treatment (34). Also, due to the uncertainty about the relationship between needling of traditional acupuncture points and MTPs (35), only four published quasi-experimental trials (16-19) have investigated the effectiveness of trigger points needling in relieving plantar heel pain.
One study (16) evaluated the effectiveness of a four-week (one treatment per week) period of acupuncture followed by two weeks of acupuncture combined with trigger points needling of the calf and heel regions. This study reported a significant improvement in plantar heel pain, as measured on a VAS. Another study (17) studied the outcome of trigger points dry needling combined with electro-acupuncture, and demonstrated a significant reduction in pain with a six-week (one treatment per week) plan of acupuncture in combination with dry needling of the heel and arch. Cotchett et al. (18) investigated a six-week (one treatment per week) period of dry needling and evaluated VAS and the pain subscale of Foot Health Status Questionnaire. They found a statistically significant improvement in plantar heel pain, but warned about some adverse transitory effects. Akhbari et al. published a case report of plantar fasciitis treated with two-week (one treatment per week) period of dry needling with acupuncture needles and reported 60 to 70% pain reduction. In contrast to our study, most of these studies were limited by some methodological problems, which reduced their quality. One of these studies was a case report with only one patient treated with dry needling. Importantly, most of these studies did not include a control in their trials to compare the intervention and non-intervention effects. Lack of a control group makes it difficult to precisely analyze the absolute effect of needling, and particularly one cannot clarify the influence of the natural course of the disorder from the intervention. In addition, combining acupuncture with dry needling of MTPs made it difficult to isolate the effectiveness of each technique separately. In addition, the absence of clear data on the criteria used to diagnose MTPs, and different methods applied by authors were another important limitation of the previous studies. Because of significant variability of criteria for identifying MTPs (36), it should be outlined by researchers.
This study has its own limitations. Although the power calculation of 0.80 was done for this study, the major limitation could be the small sample size. Carrying multicenter and multiethnic study with large sample size would be very helpful in determining eventual results of dry needling. In this study, we just tried to show the independent short-term effect of dry needling. Further, performing routine therapies on all patients did not allow evaluating sole effects of this therapeutic approach on heel dynamics.
In conclusion, this study revealed that trigger point dry needling by improving the severity of heel pain, can be used as a good alternative option before proceeding to more invasive therapies of plantar fasciitis despite its insignificant effect on the range of motion of the ankle joint.
Conflict of interest
The authors have no financial interests to disclose in relation to the content of this article.
Ethical Approval
The study protocol was approved by the Ethics Committee of Tabriz University of Medical Sciences (TUMS), which is in compliance with Helsinki declaration. The trial was registered in the Iranian "Clinical trial Registry" with identification number of "201106104641N4".
Cite this article as: Eftekharsadat B, Babaei-Ghazani A, Zeinolabedinzadeh V. Dry needling in patients with chronic heel pain due to plantar fasciitis: A single-blinded randomized clinical trial. Med J Islam Repub Iran 2016 (23 July). Vol. 30:401.
References
- 1.Barrett SJ, O'Malley R. Plantar fasciitis and other causes of heel pain. Am Fam Physician. 1999;59(8):2200–6. [PubMed] [Google Scholar]
- 2.Crawford F. Plantar heel pain and fasciitis. Clin Evid. 2005;(13):1533–45. [PubMed] [Google Scholar]
- 3.DeMaio M, Paine R, Mangine RE, Drez D, Jr Jr. Plantar fasciitis. Orthopedics. 1993;16(10):1153–63. doi: 10.3928/0147-7447-19931001-13. [DOI] [PubMed] [Google Scholar]
- 4.Irving DB, Cook JL, Young MA, Menz HB. Impact of chronic plantar heel pain on health-related quality of life. J Am Podiatr Med Assoc. 2008;98(4):283–9. doi: 10.7547/0980283. [DOI] [PubMed] [Google Scholar]
- 5.McPoil TG, Martin RL, Cornwall MW, Wukich DK, Irrgang JJ, Godges JJ. Heel pain--plantar fasciitis: clinical practice guildelines linked to the international classification of function, disability, and health from the orthopaedic section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2008;38(4):A1–A18. doi: 10.2519/jospt.2008.0302. [DOI] [PubMed] [Google Scholar]
- 6. Crawford F, Thomson C. Interventions for treating plantar heel pain. Cochrane Database Syst Rev 2003(3):CD000416. [DOI] [PubMed]
- 7.Thomas JL, Christensen JC, Kravitz SR, Mendicino RW, Schuberth JM, Vanore JV. et al. The diagnosis and treatment of heel pain: a clinical practice guideline-revision 2010. J Foot Ankle Surg. 2010;49(3 Suppl):S1–19. doi: 10.1053/j.jfas.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 8.Dequeker J. NSAIDs/corticosteroids--primum non nocere. Adv Exp Med Biol. 1999;455:319–25. [PubMed] [Google Scholar]
- 9.Zhang SP, Yip TP, Li QS. Acupuncture Treatment for Plantar Fasciitis: A Randomized Controlled Trial with Six Months Follow-up. Evid Based Complement Alternat Med. 2009 doi: 10.1093/ecam/nep186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cotchett MP, Landorf KB, Munteanu SE, Raspovic A. Effectiveness of trigger point dry needling for plantar heel pain: study protocol for a randomised controlled trial. J Foot Ankle Res. 2011;4:5. doi: 10.1186/1757-1146-4-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Itoh K, Katsumi Y, Hirota S, Kitakoji H. Randomised trial of trigger point acupuncture compared with other acupuncture for treatment of chronic neck pain. Complement Ther Med. 2007;15(3):172–9. doi: 10.1016/j.ctim.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 12.Itoh K, Hirota S, Katsumi Y, Ochi H, Kitakoji H. Trigger point acupuncture for treatment of knee osteoarthritis--a preliminary RCT for a pragmatic trial. Acupunct Med. 2008;26(1):17–26. doi: 10.1136/aim.26.1.17. [DOI] [PubMed] [Google Scholar]
- 13.Huguenin L, Brukner PD, McCrory P, Smith P, Wajswelner H, Bennell K. Effect of dry needling of gluteal muscles on straight leg raise: a randomised, placebo controlled, double blind trial. Br J Sports Med. 2005;39(2):84–90. doi: 10.1136/bjsm.2003.009431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shah JP, Danoff JV, Desai MJ, Parikh S, Nakamura LY, Phillips TM. et al. Biochemicals associated with pain and inflammation are elevated in sites near to and remote from active myofascial trigger points. Arch Phys Med Rehabil. 2008;89(1):16–23. doi: 10.1016/j.apmr.2007.10.018. [DOI] [PubMed] [Google Scholar]
- 15.Hong CZ. Lidocaine injection versus dry needling to myofascial trigger point The importance of the local twitch response. Am J Phys Med Rehabil. 1994;73(4):256–63. doi: 10.1097/00002060-199407000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Tillu A, Gupta S. Effect of acupuncture treatment on heel pain due to plantar fasciitis. Acupunct Med. 1998;16(2):66–8. [Google Scholar]
- 17.Perez-Millan R, Foster L. Low frequency electroacupuncture in the management of refractory plantar fasciitis. Med Acupunct. 2001;13(1):1–6. [Google Scholar]
- 18.Cotchett MP, Munteanu SE, Landorf KB. Effectiveness of trigger point dry needling for plantar heel pain: a randomized controlled trial. Phys Ther. 2014;94(8):1083–94. doi: 10.2522/ptj.20130255. [DOI] [PubMed] [Google Scholar]
- 19.Behnam A, Mahyar S, Ezzati K, Rad SM. The use of dry needling and myofascial meridians in a case of plantar fasciitis. J Chiropr Med. 2014;13(1):43–8. doi: 10.1016/j.jcm.2014.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guyatt GH, Sackett DL, Cook DJ. Guyatt GH, Sackett DL, Cook DJUsers' guides to the medical literatureIIHow to use an article about therapy or preventionAAre the results of the study valid? Evidence-Based Medicine Working Group. JAMA. 1993;270(21):2598–601. doi: 10.1001/jama.270.21.2598. [DOI] [PubMed] [Google Scholar]
- 21.Cotchett MP, Landorf KB, Munteanu SE, Raspovic AM. Consensus for dry needling for plantar heel pain (plantar fasciitis): a modified Delphi study. Acupunct Med. 2011;29(3):193–202. doi: 10.1136/aim.2010.003145. [DOI] [PubMed] [Google Scholar]
- 22.Goff JD, Crawford R. Diagnosis and treatment of plantar fasciitis. Am Fam Physician. 2011;84(6):676–82. [PubMed] [Google Scholar]
- 23. Simons DG TJ, Simons LS. ravell & Simons’Myofascial pain and dysfunction: the trigger point manual. 2nd ed. Baltimore: Williams & Wilkins 1999.
- 24.Boonstra AM, Schiphorst Preuper HR, Reneman MF, Posthumus JB, Stewart RE. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. International journal of rehabilitation research Internationale Zeitschrift fur Rehabilitationsforschung Revue internationale de recherches de readaptation. 2008;31(2):165–9. doi: 10.1097/MRR.0b013e3282fc0f93. [DOI] [PubMed] [Google Scholar]
- 25.Saag KG, Saltzman CL, Brown CK, Budiman-Mak E. The Foot Function Index for measuring rheumatoid arthritis pain: evaluating side-to-side reliability. Foot Ankle Int. 1996;17(8):506–10. doi: 10.1177/107110079601700814. [DOI] [PubMed] [Google Scholar]
- 26.SooHoo NF, Samimi DB, Vyas RM, Botzler T. Evaluation of the validity of the Foot Function Index in measuring outcomes in patients with foot and ankle disorders. Foot Ankle Int. 2006;27(1):38–42. doi: 10.1177/107110070602700107. [DOI] [PubMed] [Google Scholar]
- 27.Othman AM, Ragab EM. Endoscopic plantar fasciotomy versus extracorporeal shock wave therapy for treatment of chronic plantar fasciitis. Arch Orthop Trauma Surg. 2010;130(11):1343–7. doi: 10.1007/s00402-009-1034-2. Epub 2009/12/25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cole C, Seto C, Gazewood J. Plantar Fasciitis: Evidence-Based Review of Diagnosis and Therapy. American Family Physician. 2005;72(11):2237–42. [PubMed] [Google Scholar]
- 29.McNally EG, Shetty S. Plantar fascia: imaging diagnosis and guided treatment. Semin Musculoskelet Radiol. 2010;14(3):334–43. doi: 10.1055/s-0030-1254522. [DOI] [PubMed] [Google Scholar]
- 30.Kalaci A, Cakici H, Hapa O, Yanat AN, Dogramaci Y, Sevinc TT. Treatment of plantar fasciitis using four different local injection modalities: a randomized prospective clinical trial. J Am Podiatr Med Assoc. 2009;99(2):108–13. doi: 10.7547/0980108. [DOI] [PubMed] [Google Scholar]
- 31.Imamura M, Fischer AA, Imamura ST, Kaziyama HS, Carvalho AEJr, Salomao O. Treatment of myofascial pain components in plantar fasciitis speeds up recovery: documentation by algometry. J Musculoskelet Pain. 1998;6(1):91–110. [Google Scholar]
- 32.Tatli YZ, Kapasi S. The real risks of steroid injection for plantar fasciitis, with a review of conservative therapies. Curr Rev Musculoskelet Med. 2009;2(1):3–9. doi: 10.1007/s12178-008-9036-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tough EA, White AR, Cummings TM, Richards SH, Campbell JL. Acupuncture and dry needling in the management of myofascial trigger point pain: a systematic review and meta-analysis of randomised controlled trials. Eur J Pain. 2009;13(1):3–10. doi: 10.1016/j.ejpain.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 34.Cotchett MP, Landorf KB, Munteanu SE. Effectiveness of dry needling and injections of myofascial trigger points associated with plantar heel pain: a systematic review. J Foot Ankle Res. 2010;3:18. doi: 10.1186/1757-1146-3-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dorsher PT. On the probability of trigger point-acupuncture point correspondences: an evidence-based rebuttal of Stephen Birch's commentary. J Altern Complement Med. 2008;14(10):1183–4. doi: 10.1089/acm.2008.0329. [DOI] [PubMed] [Google Scholar]
- 36.Tough EA, White AR, Richards S, Campbell J. Variability of criteria used to diagnose myofascial trigger point pain syndrome--evidence from a review of the literature. Clin J Pain. 2007;23(3):278–86. doi: 10.1097/AJP.0b013e31802fda7c. [DOI] [PubMed] [Google Scholar]