Abstract
Background
Although it is a common practice to estimate dietary intake using three random 24-hour dietary recalls, some studies have suggested up to nine may be necessary to reliably estimate usual intake in youth. Given the resulting increase in resources and participant burden, more research is needed to determine if this method is reliable, particularly in African American youth at increased risk for obesity and other chronic diseases.
Objective
This study estimated the reliability with which 24-hour dietary recalls measure energy, fat, fruit, and vegetable intake in African American youth and examined how reliability changes as a function of the number of recalls.
Design
Cross-sectional data collection across three studies
Participants/setting
Participants were African American youth (n=456, 13.28±1.86 years old, 64% girls, 31.45±7.94 body mass index) who completed random 24-hour dietary recalls (67% completed three) conducted by research assistants using the Automated Self-Administered 24-hour Recall system (n=258) or registered dietitians using the Nutrition Data System for Research (n=198).
Main outcome measures/statistical analyses
Estimates provided by multilevel models were used to calculate the proportion of variance accounted for between individuals and the reliability of means within individuals as a function of the number of recalls.
Results
Reliability estimates for assessing dietary outcomes using 1-3 recalls ranged from 11-62%. To achieve 80% reliability, the following number of recalls would need to be conducted: 8 for energy intake, 13 for fat intake, 21-32 for fruit intake, and 21-25 for vegetable intake.
Conclusions
The common practice of assessing dietary intake with three recalls does so with low reliability in African American youth. Until more objective methods for reliably estimating usual intake are developed, researchers who choose to use 24-hour dietary recalls are encouraged to include estimates of the measure's reliability in a priori power calculations for improved decision-making regarding number observations and/or sample size.
Keywords: 24-hour dietary recall, reliability, African American, youth
Dietary intake has been linked to important health outcomes, including several of the leading causes of death (e.g., cardiovascular disease, cancer, diabetes).1 For researchers aiming to promote the early establishment of healthy eating behaviors in populations at high risk for obesity and other chronic diseases, the dietary patterns of African American youth are of particular interest. Numerous randomized controlled trials have sought to improve dietary outcomes (e.g., % of energy from fat, fruit and vegetable intake) in racially/ethnically diverse children and adolescents and have relied on 24-hour dietary recalls to assess changes in diet.2-4 Demonstrating meaningful changes in youth dietary patterns is challenging, however, with interventions often showing null or only marginally significant effects.5,6 Low reliability of dietary measures contributes to measurement error, and in turn, reduces power to detect effects. The present study expands on past research by examining the reliability of random 24-hour dietary recall measures in African American youth.
The use of self-reported, 24-hour dietary recalls for estimating dietary intake has received a great deal of previous attention.7-15 Among the well-recognized methodological challenges associated with 24-hour recalls is the issue of reliability, defined here as the extent to which repeated 24-hour recalls estimate usual dietary intake without error.9 Low reliability is due to both variations in diet across days as well as inaccuracy in reporting. Reliability is important for dietary assessment because less-reliable estimates have more error and are therefore less likely to show effects of interventions or show the influence of key important predictors. Further, reliability estimates can help determine the number of observations needed to account for daily variation in typical intake patterns.16,17 While collecting three recalls from youth is a common practice in the field,2-4 it has recently been suggested by Ollberding et al.17 that as many as six to nine recalls may be needed to estimate usual intake in youth using 24-hour recalls with reasonably adequate reliability. The gap between what is currently done and this recent recommendation represents a large difference in terms of cost and participant burden, particularly for intervention and longitudinal studies that gather dietary data across repeated intervals. Using data across three different studies with low-income, African American samples, and a similar analytic approach as that taken by Ollberding et al.17, the present study assesses the reliability of 24-hour dietary recalls for estimating four dietary outcomes frequently assessed within randomized controlled trials (i.e., energy, fat, vegetable, and fruit intake).
A number of statistical methods have been proposed to account for unreliability of 24-hour dietary recalls.18,19 While these methods require as few as two recalls collected on nonconsecutive days to model usual intake, they are most applicable for estimating group means at the population level and thus will not resolve the issue of lower power due to unreliability. These methods also require a high degree of technical expertise, and are not widely used, particularly within the context of examining dietary changes in randomized controlled studies, which have largely relied on averaging across recalls.3 It is thus of high interest to examine the reliability of commonly used practices to make appropriate decisions regarding power and sample size calculations as well as appropriate causal inferences from dietary intervention studies conducted with African American youth. The aims of the present study were: (1) to determine the reliability with which 24-hour dietary recalls measure total energy, fat, vegetable, and fruit intake in African American youth ages 10-17 years, and (2) to examine how the reliability of 24-hour dietary recalls changes as a function of the number of recall days across three independent studies.
Participants and Methods
Participants
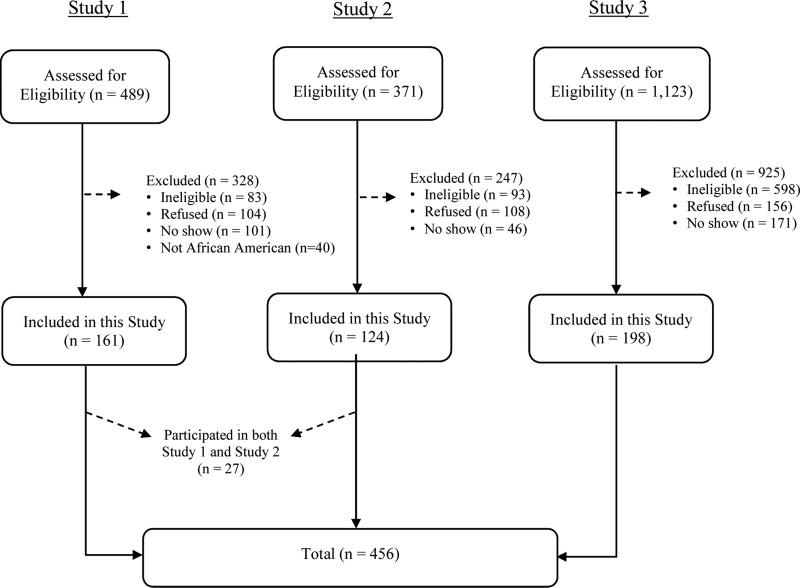
Participants (n = 456) were children and adolescents between the ages 10-17 years old who completed 24-hour dietary recalls as part of their participation in one of three studies: a cross-sectional health assessment study (study 1),20 a family-based health promotion intervention (study 2),21 or a family-based weight loss efficacy trial (study 3).22 All studies were conducted in South Carolina. Participants across the three studies were recruited using numerous strategies, including printed materials (flyers, brochures), through referrals from local pediatrician's offices, or at community events. Youth were eligible to participate in study 1 if they were (1) between the ages of 10-17 years old, (2) classified as overweight or obese, defined as having a body mass index ≥ 85th percentile for age and sex, (3) able to speak English, and (4) without a chronic medical condition, psychiatric condition or developmental delay. Eligible participants from study 1 who did not self-identify as African American (n=40) were removed from the present analyses. Youth were eligible to participate in study 2 if they were (1) African American, (2) between the ages of 11-15 years old, (3) living with at least one parent or primary caregiver willing to participate, (4) without a chronic medical condition, psychiatric condition or developmental delay, and (5) not already taking part in a health or weight loss program. Finally, youth were eligible to participate in study 3 if they were (1) African American, (2) between the ages of 11-16 years old, (3) classified as overweight or obese, (4) living with at least one parent or primary caregiver willing to participate, (5) living in a home with internet access, (6) without a chronic medical condition, psychiatric condition or developmental delay, (7) not already taking part in a weight loss program, and (8) not taking medication that would interfere with weight loss. Recruitment and data collection took place between 2010-2012 for studies 1 and 2 and between 2013-2015 for study 3. See Figure 1 for a participant flow diagram for each of the three studies. Because studies 1 and 2 were conducted at the same time, some youth (n = 27) participated in both studies and data for these participants were shared across studies.
Figure 1.
Participant flow diagram (n = 456 African American youth)
Procedure
Protocols for the three studies were approved by the Institutional Review Board at the University of South Carolina. Before any measures were administered, parents and youth signed informed consent and assent documents, respectively. A team of trained measurement staff collected measures for all participants. Measures included demographics, anthropometric data (height, weight) and three random 24-hour dietary recalls. Participants received a monetary incentive for completing assessments. Cross-sectional data from study 1 and baseline data from studies 2 and 3 were included in the present analyses.
Measures
Anthropometric measures
Height was measured using a stadiometer (ShorrBoard® Infant/Child/Adult Measuring Board, Weigh and Measure, LLC, Olney, MD) and weight was measured with a digital scale (Digital Floor Scale 880, SECA, Hamburg, Germany). Two measures of height and weight were taken, and the average score was used in anthropometric calculations. Body mass index and body mass index percentiles were calculated using the Centers for Disease Control and Prevention 2000 growth reference curves.23
Dietary Intake
Three 24-hour dietary recalls were completed for each participant and used to estimate dietary outcomes, including total energy, fat, fruit, and vegetable intake. Recalls were conducted on randomly assigned days determined by study staff and thus not scheduled with participants in advance. Twenty-four hour recalls calculate intake by taking into account detailed food descriptions including brand names, ingredients, methods of food preparation, and portion sizes. Specific methods used to collect 24-hour recalls across the three studies are described below.
Modified ASA24 protocol
Recalls for studies 1 and 2 were conducted using the Automated Self-Administered 24-hour Recall system (ASA24™) developed by the National Cancer Institute.24 ASA24 is a free online dietary interview system modeled after the USDA's Automated Multiple Pass Method (AMPM) that systematically probes for food descriptions, preparation methods, and portion sizes and subsequently codes food items into nutrient intake.24-27 Preliminary examination of ASA24 suggested acceptable face validity through food group estimates consistent with those found in the National Health and Nutrition Examination Survey.24 Mean reported intakes of various foods on ASA24, including fruits and vegetables, have also been similar to those reported using the AMPM in a sample of 1,200 adults.28 More recent studies comparing ASA24 to the AMPM relative to true (observed) intake indicate close agreement between ASA24 and standardized, interviewer-administered recalls.29
Because the ASA24 youth version (“ASA24-Kids-2012;” released September 2012) was unavailable for studies 1 and 2, administration protocols using the adult self-administered “Beta” and “ASA24-2011” versions were modified for use with youth in these studies. Specifically, trained and certified research assistants (the majority of whom were female and Caucasian) contacted participants via phone on three random days (two weekdays, one weekend day) and entered dietary information from the previous day into the automated system on participants’ behalf in a semi-structured interview style that followed the ASA24 prompts. Prior to conducting recalls, study staff completed extensive training on ASA24, including a detailed overview of the system, live demo, and various practice sessions. Certification was based on achieving a minimum of 80% agreement with two standardized menus. Participants were provided with serving size handouts and prompted by interviewers to reference these during each recall. Interviewers were instructed to contact participants a maximum of three times on their randomly determined days and continue calling difficult-to-reach participants on randomly determined back-up days. Participants were always instructed to recall the previous day's intake.
Dietitian-administered recalls
Recalls for study 3 were conducted by registered dietitians (majority female and Caucasian) from the Diet Assessment Research Unit at the University of South Carolina who were trained in the multiple-pass method using the Nutrition Data System for Research (Version 2008, Released June 2008, Nutrition Coordinating Center, University of Minnesota, Minneapolis, MN). The Nutrition Data System for Research is an interview and food/nutrient database used to collect and code data from 24-hour dietary recalls.30 Participants were provided with two dimensional food models to assist with portion size estimation31 and were prompted by dietitians to reference these during each recall interview. Dietitians contacted participants by phone on three random days (two weekdays, one weekend day) to collect dietary information from the previous days. Dietitians were instructed to contact participants a maximum of three times on their randomly determined days, and participants were always instructed to recall the previous day's intake.
Data Analyses
Data were analyzed separately by data collection method. Specifically, given the same methodology was used to collect dietary recalls in studies 1 and 2 (modified ASA24 protocol), data from these studies were combined and analyzed together. Data from study 3 (dietitian-administered recalls) were analyzed separately. All analyses were conducted in R (Version 3.2.2, Released August 2015, ©The R Foundation for Statistical Computing).
Multilevel modeling was used to model multiple recalls within individuals. Multilevel models, also known as random effects models, are commonly used in bio statistical research for modeling non-independence of observations, in this case caused by having repeated measures data for individuals (e.g., dietary recalls nested within African American youth).32 Multilevel models are particularly well suited for answering the research questions in this study that they partition variance into within- versus between-person components (i.e., how much of the variance in the repeated dietary recall outcomes are due to consistency in participant reports over time versus random variability between individual participants’ recalls).
Before models were run, two outliers were removed from study 3: an estimate of fruit intake equivalent to 21.57 cups on a single recall day and an estimate of vegetable intake equivalent to 13.25 cups on a single recall day. Unconditional models with random effects (i.e., random effects ANOVAs) were first run for each of four dietary outcomes, including (a) total energy intake (kcals), (b) total fat intake (grams), (c) total fruit servings (cups), and (d) total vegetable servings (cups). Using the variance estimates provided by these models, intra-class correlation coefficients were calculated to assess how much of the variance in each of the four dietary outcomes was accounted for between individuals using the following formula: ICC = τ00 / ( σ2 + τ00), where τ00 is the participant level variance and σ2 is the dietary recall level variance from the unconditional model.
By partitioning variance within and between subjects, standard approaches may be used to determine reliability (defined in the present study as “stable levels” of specified dietary outcomes within individuals) by measuring the true score (or parameter variance) relative to the observed score (or total variance) of the sample means. A great advantage of this approach is that it allows one to project how reliability would change if more or fewer observations were collected per participant. As such, reliability of each of the participant means (i.e., the intercepts in the unconditional model) were calculated using the following standard formula : λ= τ00 / ((σ2/n) + τ00)32, where τ00 is the participant level variance, σ2 is the dietary recall level variance from the unconditional model, and n is the number of days of recall (used to extrapolate reliability estimates for anywhere from one recall up through any given number of recalls).32 Estimates of variance components from this model were used to calculate the reliability of means for each dietary outcome as the number of days of recall increased. Up to 35 days of recall per outcome were examined to determine the number of recalls necessary to reach 80% reliability, previously referred to as a “very good” minimum threshold for a measure's consistency.33 This formula and the necessary variance estimates make it possible to calculate the number of days needed for any other level of reliability of interest to researchers. In other words, these results may be used to calculate number of recalls needed for lower or higher targets.
Results
Participant Demographic Characteristics
Participant demographic characteristics are summarized in Table 1. Participants were predominantly female (64%), 13.28 ± 1.86 years old and had a body mass index of 31.45 ± 7.94. Annual household income for 63% of participants was below $40K. Most participants completed three dietary recalls (67%), with an average spread of 4.57 ± 5.60 days between the first and second recall and 9.49 ± 7.84 days between the first and third recall. On average, participants reported consuming 1618.17 ± 516.10 kcals, 64.11 ± 23.89 grams of fat, 0.96 ± 1.01 cups of fruit, and 1.41 ± 0.96 cups of vegetables.
Table 1.
Demographic characteristics of 456 African American youth completing 24-hour dietary recalls across three studies
| Variable | Studies 1 & 2: Modified ASA24 protocol | Study 3: Dietitian-administered recalls | Total |
|---|---|---|---|
| N | 258 | 198 | 456 |
| Sex | |||
| Girls | 62% | 67% | 64% |
| Boys | 38% | 33% | 36% |
| Age (yrs)** | 13.02 (1.91) | 13.61 (1.73) | 13.28 (1.86) |
| Body mass index | 31.02 (8.74) | 32.01 (6.73) | 31.45 (7.94) |
| Household Income** | |||
| < $10 K | 22% | 12% | 18% |
| $10-24 K | 27% | 18% | 23% |
| $25-39K | 26% | 17% | 22% |
| $40+K | 22% | 31% | 26% |
| Missing | 3% | 22% | 11% |
| No. Completed Recalls | |||
| 0 | 6% | <1% | 4% |
| 1 | 7% | 7% | 7% |
| 2 | 24% | 18% | 21% |
| 3 | 61% | 74% | 67% |
| 4 | 2% | 0 | <1% |
| Spread (# days between recalls) | |||
| First and second recall** | 3.66 (3.12) | 5.52 (7.21) | 4.57 (5.60) |
| First and third recall** | 7.34 (6.07) | 11.59 (8.76) | 9.49 (7.84) |
| Participants with 2 consecutive recalls* | 18% | 1% | 11% |
| Total energy intake (kcal) | 1574.08 (530.67) | 1666.20 (497.12) | 1618.17 (516.10) |
| Total fat intake (grams) | 62.35 (24.70) | 66.03 (23.00) | 64.11 (23.89) |
| Total fruit intake (cups) | 0.93 (1.03) | 1.00 (1.00) | 0.96 (1.01) |
| Total vegetable intake (cups)** | 1.00 (0.68) | 1.87 (1.03) | 1.41 (0.96) |
Note. Values are expressed as frequencies (%) or means (standard deviations)
p<.05
p<.01
Youth who completed recalls using the modified ASA24 protocol were younger (t = −3.06, df = 446.3, p < .01), more likely to report a lower household income (χ2 = 16.83, df = 6, p <.01), consumed less vegetables (t = −8.55, df = 245.57, p < .01), had fewer days between the first and second (t = −3.18, df = 245.09, p < .01) and first and third recalls (t = −4.73, df = 260.61. p < .01), and were more likely to complete recalls on consecutive days (χ2 = 33.22, df = 1, p <.01) compared to those who completed dietitian-administered recalls.
Intraclass Correlation Coefficients
For youth who completed recalls using the modified ASA24 protocol, intraclass correlation coefficients for total energy intake (ICC=0.35), fat intake (ICC = 0.24), fruit intake (ICC = 0.11), and vegetable intake (ICC = 0.16) indicated 11-35% of the variance in the repeated dietary recall outcomes was due to consistency in participant reports over time (i.e., the cluster) and the remaining 65-89% of the variance in dietary outcomes was random variability between individual participants’ recalls. That is, on any given day 11-35% of the variance could be attributed to the participant's usual intake and 65-89% of the variance could be attributed to measurement error and day-to-day variation. Similarly, for youth who completed dietitian-administered recalls, intra-class correlation coefficients for total energy intake (ICC = 0.33), fat intake (ICC = 0.23), fruit intake (ICC = 0.16), and vegetable intake (ICC = 0.13) indicated 13-33% of the variance in the repeated dietary recall outcomes was due to the participant and the remaining 67-87% was within individuals across days.
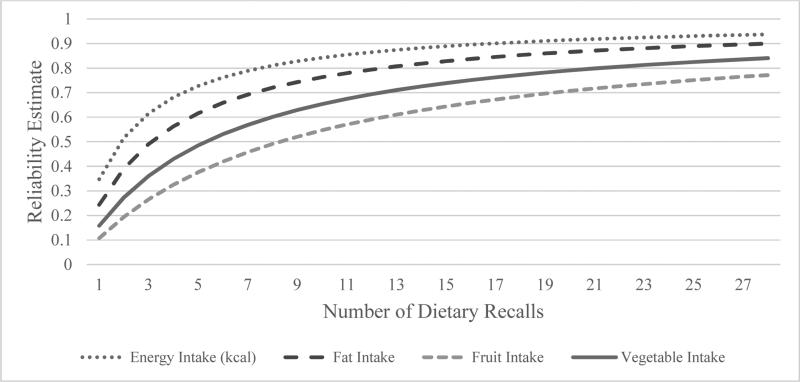
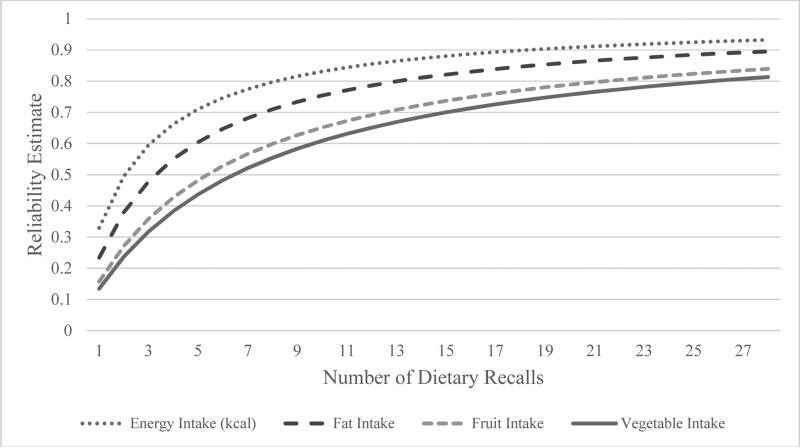
Reliability as a Function of the Number of Recalls
See Figures 2 and 3 for illustrations of how reliability estimates varied across dietary outcomes as a function of the number of observations (i.e., dietary recalls). Across studies, reliability estimates for either total energy, fat, fruit, or vegetable intake ranged from 11-35% for one recall, 19-52% for two recalls, and 27-62% for three recalls (see Table 2). To achieve 80% reliability in assessing dietary outcomes within individuals, it was estimated that the following number of recalls would need to be conducted (see Table 3): 8 recalls for total energy intake, 13 recalls for total fat intake, 21-32 recalls for fruit intake, and 21-25 recalls for vegetable intake.
Figure 2.
Reliability estimates for dietary outcomes based on number of observations (i.e., dietary recalls) in African American youth who completed the modified ASA24 protocol
Figure 3.
Reliability estimates for dietary outcomes based on number of observations (i.e., dietary recalls) in African American youth who completed dietitian-administered recalls
Table 2.
Reliability estimates of dietary outcomes for African American youth by number of recalls commonly collected
| Dietary Outcome | Studies 1 & 2: Modified ASA24 protocol |
Study 3: Dietitian-administered recalls |
||||
|---|---|---|---|---|---|---|
| Number of Recalls | Number of Recalls | |||||
| 1 | 2 | 3 | 1 | 2 | 3 | |
| Total energy intake (kcal) | 35% | 52% | 62% | 33% | 50% | 60% |
| Total fat intake (grams) | 24% | 39% | 49% | 23% | 38% | 48% |
| Total fruit intake (cups) | 11% | 19% | 27% | 16% | 27% | 36% |
| Total vegetable intake (cups) | 16% | 27% | 36% | 13% | 24% | 32% |
Table 3.
Number of 24-hour dietary recalls required for estimating usual intake with ≥80% reliability in African American youth
| Dietary Outcome | Studies 1 & 2: Modified ASA24 protocol | Study 3: Dietitian-administered recalls |
|---|---|---|
| Total energy intake (kcal) | 8 | 8 |
| Total fat intake (grams) | 13 | 13 |
| Total fruit intake (cups) | 32 | 21 |
| Total vegetable intake (cups) | 21 | 25 |
Discussion
The goals of this study were to estimate the reliability with which 24-hour dietary recalls measure dietary outcomes frequently assessed within randomized controlled trials (i.e., total energy, fat, vegetable, and fruit intake) in African American youth and to examine change in reliability as a function of the number of recall days. Results indicated that reliability estimates for assessing dietary outcomes for African American youth using three recalls, or the number commonly collected in the field, were ≤62%. Reliability for all four dietary outcomes increased as a function of the number of recall days and indicated that between 8-32 recalls would be necessary to achieve an acceptable level of ≥80% reliability for total energy, fat, fruit, or vegetable intake. This estimate exceeds both current practices in the field and recent recommendations and may only be feasible in select situations and/or for select outcomes. Short-term strategies (e.g., pairing self-report with more objective data) may mitigate the impact of measurement error, but in the long term, new technologies are needed for more reliable dietary assessment. Overall, researchers considering the use of 24-hour recalls are encouraged to include estimates of the measure's reliability (such as those provided in this paper) in their a priori power calculations for improved decision-making.
Reliability estimates calculated in this study are similar to those recently reported by Ollberding et al.17, indicating that they seem to be robust despite demographic differences between study samples. Ollberding and colleagues examined the within- to between-individual variance ratios and number of 24-hour recalls required to rank order a large national sample of 3,473 6-17 year old multi-ethnic children and adolescents (over half of which were in the normal weight range and only 21-25% of which were African American) across various macro- and micronutrients, including total energy and fat intake. They found that three to six or six to nine recalls would be necessary to rank order adolescents and children, respectively, on usual intake with an accuracy of r = 0.8 for most nutrients. A correlation of 0.8 was described as providing “a reasonable trade-off between accuracy and participant burden”17 (p. 1757). Notably, however, r = 0.8 is equivalent to a reliability estimate of only 64%. As such, although reliability estimates for three to six recalls in the present study were similar to those reported by Ollberding et al., conclusions regarding the number of days necessary to achieve an acceptable level of reliability differ.
While three to six recalls may be sufficient for some applications such as estimating a usual intake distribution in a population, this low level of reliability would make it increasingly difficult to adequately power randomized controlled trials. Kanyongo et al.34 highlight how statistical power decreases as a function of low reliability across several statistical methods (e.g., independent t-test, one-way ANOVA with three groups). For example, achieving power of .8 to detect a small effect (Cohen's d = .2) with an independent t-test requires a sample size of 309 participants and perfect reliability (r = 1.0). When reliability in this case is reduced to .90, .80, and .70, power is also reduced to .65, .60, and .54, respectively. It is thus not surprising that intervention effects on dietary outcomes such as total energy, fat, vegetable, and fruit intake are difficult to detect. Overall, there are severe limitations to relying on these type of dietary assessment methods and more research is needed in developing new methods for reliably estimating usual intake patterns in racial minority youth. Until objective dietary assessment methods are developed, researchers who choose to assess diet using 24 hour dietary recalls are strongly encouraged to account for levels of reliability when determining optimal sample sizes and/or number of observations necessary to detect effects. Researchers using 24-hour recalls may counteract the low reliability of 24-hour dietary recalls (and thereby increase power in their studies) in one of two ways: (1) increasing the study sample size, and/or (2) increasing the number of observations (i.e., recalls) collected. If low reliability is counteracted by increasing sample size, researchers should understand that this may result in underestimates of effect size due to unreliability. If, however, unreliability is counteracted by increasing number of recalls, effect sizes may be more accurate.
Considerations regarding the number of required recalls are also contingent on the dietary outcome(s) of interest. For example, findings from the present study demonstrated that fewer recalls were required to reliably estimate energy intake than were required for either fat, fruit or vegetable intake. While similar results in required number of intake days across nutrients has been observed by others17,35,36, these studies did not include fruit and vegetable intake, a typical target of youth dietary change interventions.4 Our findings indicated that between 21-32 recalls would be required to measure usual intake of fruits and vegetables in African American youth with at least 80% reliability, which would not be feasible in most settings. This means that the considerable measurement error associated with collecting 2-3 or even 6-8 dietary recalls may limit researchers’ ability to detect changes in specific dietary variables. Compared to total energy and fat intake, for which the number of required recalls was the same across methods used in this study (i.e., modified ASA24 protocol versus dietitian-administered recalls), the number of required recalls for fruit and vegetable intake also demonstrated greater variability across methods. The high number of required recalls and variability across methods highlights difficulties with obtaining reliable estimates of fruits and vegetables in African American youth and has important implications regarding data quality and participant burden.
Previous research indicates that as the number of recalls increases, the quality of data may decrease.37 This decrease in quality underscores the need for research directed at developing efficient, innovative methods that maximize the accuracy and reliability of usual intake and simultaneously minimize participant fatigue. Some emerging technology-based methods include digital food photography, which compares images of food consumed and discarded to estimate energy and nutrient intake38, and automated wrist motion tracking devices that sense periods of eating.39 While promising, these methods require further testing and validation and are not currently available for widespread use in free-living conditions. In the meantime, pairing 24-hour recalls with more objective measures of diet may reduce measurement error. Increased use of statistical modeling techniques that correct for unreliability in the estimation of usual intake using a smaller number of recalls in combination with food frequency questionnaires may also be beneficial for some select research questions.18,19 An archived webinar series that summarizes some available techniques is available through the National Cancer Institute (http://appliedresearch.cancer.gov/measurementerror/). While these techniques may be more commonly applied to the estimation of population distributions and in some cases of diet-health relationships, extensions of the methods across a wide variety of research questions are lacking.40 In addition, it should be noted that these methods do not fix the problem with low power and they remain technically advanced and difficult to utilize for many diet researchers despite extensive documentation.
Strengths of this study include the large sample of African American youth and use of two different data collection methods for obtaining 24-hour recall data, one of which is freely available. Importantly, and although low cost does not outweigh poor reliability, this study demonstrates that fairly similar levels of reliability may be achieved with a no cost alternative. Given African American youth are at increased risk for obesity and other chronic diseases associated with dietary intake, understanding the reliability of dietary assessment methods in this population is important, particularly for those developing treatment and/or preventive interventions aimed at modifying dietary intake. Reliability estimates in this exclusively African American sample were very similar to those previously reported in a large sample of multi-ethnic children and adolescents.17 Limitations include the availability of only 3 dietary recalls per person, which precluded the examination of whether reliability and data quality is impacted by additional recalls. In addition, some variability in responses could be due to the fact that data from studies 1 and 2 were not collected by dietary experts and/or that the majority of data collection staff across both studies were Caucasian and thus not culturally of the same racial group of participants. Furthermore, some research has shown that 24-hour dietary recall reliability can be improved with modeling that includes food frequency questionnaire data,40 which was not available in the current study. However, many studies exclusively rely on 24-hour dietary recalls. While the current study focused on evaluating reliability of 24-hr dietary recalls, it should be noted that there are additional measurement error concerns including validity, or the accuracy of reported dietary information, and systematic bias.7,10 For example, gender (female) and weight status (overweight/obese) have been associated with the under-reporting of dietary intake in youth.41 Similarly, studies have shown that the accuracy of dietary data may suffer when collecting previous day rather than same-day recalls from youth.42,43 Reliability and validity, though related, represent unique psychometric properties of measures; this paper specifically addresses reliability as it concerns the use of 24-hour dietary recalls in African American youth.
Conclusions
Overall, findings from the present study demonstrate that current standards for assessing usual dietary intake in youth using only three random 24-hour dietary recalls are associated with low reliability. Low reliability, in turn, results in lower power and may help explain the marginal or null results often observed in youth dietary intervention studies. Researchers should include reliability estimates in a priori power calculations to make the most informed decisions regarding the use of 24 hour recalls. Because the number of recalls necessary for increased reliability depends on the dietary outcomes of interest and may exceed what is practically feasible for some outcomes, more research on innovative, objective, and efficient methods for reliably estimating and/or statistically modeling usual intake patterns in youth is urgently needed.
Acknowledgments
Funding/Support Disclosure
This research was supported by three grants (F31 HD066944 to SMS, F31 DK086358 to HGL, R01 HD072153 to DKW) funded by the National Institutes of Health. The study sponsor had no role in study design, data collection, analysis, or interpretation, writing of the paper or decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Disclosure
The authors have no conflicts of interest to disclose.
Contributor Information
Sara M. St. George, Department of Public Health Sciences, University of Miami Miller School of Medicine, 1120 NW 14th Street, Suite 1009, Miami, FL, 33136; 305-243-0726.
M. Lee Van Horn, Department of Individual, Family, and Community Education, College of Education, University of New Mexico, MSC053040, 1 University of New Mexico, Tech 274, Albuquerque, NM 87106; 505-277-4535; mlvh@unm.edu..
Hannah G. Lawman, Chronic Disease Prevention Division, Philadelphia Department of Health, 1101 Market Street, 9th floor, Philadelphia, PA 19107; hannah.lawman@phila.gov..
Dawn K. Wilson, Department of Psychology at the University of South Carolina, 1233 Washington Street, Columbia, SC 292021; 803-978-7500; wilsondk@mailbox.sc.edu..
References
- 1.Estruch R, Ros E, Salas-Salvadó J, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. New England Journal of Medicine. 2013;368(14):1279–1290. doi: 10.1056/NEJMoa1200303. [DOI] [PubMed] [Google Scholar]
- 2.Ebbeling CB, Feldman HA, Chomitz VR, et al. A randomized trial of sugar-sweetened beverages and adolescent body weight. N Engl J Med. 2012;367(15):1407–1416. doi: 10.1056/NEJMoa1203388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patrick K, Calfas K, Norman G, et al. Randomized controlled trial of a primary care and home-based intervention for physical activity and nutrition behaviors: PACE+ for adolescents. Arch Pediatr Adolesc Med. 2006;160(2):128–136. doi: 10.1001/archpedi.160.2.128. [DOI] [PubMed] [Google Scholar]
- 4.Baranowski T, Baranowski J, Thompson D, et al. Video game play, child diet, and physical activity behavior change: A randomized clinical trial. American Journal of Preventive Medicine. 2011;40(1):33–38. doi: 10.1016/j.amepre.2010.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lytle L, Murray D, Perry C, et al. School-based approaches to affect adolescents' diets: results from the TEENS study. Health Educ Behav. 2004;31(2):270. doi: 10.1177/1090198103260635. [DOI] [PubMed] [Google Scholar]
- 6.Baranowski T, Baranowski J, Cullen K, et al. 5 a Day Achievement Badge for African-American boy scouts: Pilot outcome results. Prev Med. 2002;34(3):353–363. doi: 10.1006/pmed.2001.0989. [DOI] [PubMed] [Google Scholar]
- 7.Archer E, Hand GA, Blair SN. Validity of US nutritional surveillance: National Health and Nutrition Examination Survey caloric energy intake data, 1971–2010. PLoS One. 2013;8(10):e76632. doi: 10.1371/journal.pone.0076632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mitka M. Do flawed data on caloric intake from NHANES present problems for researchers and policy makers? JAMA. 2013;310(20):2137–2138. doi: 10.1001/jama.2013.281865. [DOI] [PubMed] [Google Scholar]
- 9.Hébert JR, Hurley TG, Steck SE, et al. Considering the value of dietary assessment data in informing nutrition-related health policy. Advances in Nutrition: An International Review Journal. 2014;5(4):447–455. doi: 10.3945/an.114.006189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dhurandhar N, Schoeller D, Brown A, et al. Energy balance measurement: When something is not better than nothing. Int J Obes. Advance online publication. 2014 doi: 10.1038/ijo.2015.81. doi: 10.1038/ijo.2014.1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Archer E, Pavela G, Lavie CJ. The inadmissibility of What We Eat In America and NHANES dietary data in nutrition and obesity research and the scientific formulation of national dietary guidelines. Mayo Clinic Proceedings. 2015;90(7):911–926. doi: 10.1016/j.mayocp.2015.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davy BM, Estabrooks PA. The validity of self-reported dietary intake data: Focus on the “What We Eat In America” component of the National Health and Nutrition Examination Survey research initiative. Mayo Clinic Proceedings. 2015;90(7):845–847. doi: 10.1016/j.mayocp.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 13.Hébert JR, Hurley TG, Steck SE, et al. Reply to E Archer and SN Blair. Advances in Nutrition. 2015;6(2):230–233. doi: 10.3945/an.114.007831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Archer E, Blair SN. Response to LS Freedman et al. Advances in Nutrition. 2015;(6):489–490. doi: 10.3945/an.115.009183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Freedman LS, Carroll RJ, Neuhouser ML, et al. Reply to E Archer and SN Blair. Advances in Nutrition. 2015;6:389. doi: 10.3945/an.115.009118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nelson M, Black AE, Morris JA, Cole TJ. Between-and within-subject variation in nutrient intake from infancy to old age: estimating the number of days required to rank dietary intakes with desired precision. The American journal of clinical nutrition. 1989;50(1):155–167. doi: 10.1093/ajcn/50.1.155. [DOI] [PubMed] [Google Scholar]
- 17.Ollberding NJ, Couch SC, Woo JG, Kalkwarf HJ. Within-and between-individual variation in nutrient intake in children and adolescents. Journal of the Academy of Nutrition and Dietetics. 2014;114(11):1749–1758. doi: 10.1016/j.jand.2014.03.016. [DOI] [PubMed] [Google Scholar]
- 18.Dodd KW, Guenther PM, Freedman LS, et al. Statistical methods for estimating usual intake of nutrients and foods: a review of the theory. Journal of the American Dietetic Association. 2006;106(10):1640–1650. doi: 10.1016/j.jada.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 19.Tooze JA, Kipnis V, Buckman DW, et al. A mixed-effects model approach for estimating the distribution of usual intake of nutrients: The NCI method. Statistics in medicine. 2010;29(27):2857–2868. doi: 10.1002/sim.4063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lawman HG, Wilson DK. Associations of social and environmental supports with sedentary behavior, light and moderate-to-vigorous physical activity in obese underserved adolescents. International Journal of Behavioral Nutrition and Physical Activity. 2014;11(1):92. doi: 10.1186/s12966-014-0092-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.St. George SM, Wilson DK, Schneider EM, Alia KA. Project SHINE: Effects of parent– adolescent communication on sedentary behavior in African American adolescents. J Pediatr Psychol. 2013;38:997–1009. doi: 10.1093/jpepsy/jst027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilson DK, Kitzman-Ulrich H, Resnicow K, et al. An overview of the Families Improving Together (FIT) for weight loss randomized controlled trial in African American families. Contemp Clin Trials. 2015;42:145–157. doi: 10.1016/j.cct.2015.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kuczmarski R, Ogden C, Guo S, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital and health statistics. Series 11, Data from the national health survey. 2002(246):1. [PubMed] [Google Scholar]
- 24.Subar AF, Kirkpatrick SI, Mittl B, et al. The Automated Self-Administered 24-hour dietary recall (ASA24): A resource for researchers, clinicians, and educators from the National Cancer Institute. Journal of the Academy of Nutrition and Dietetics. 2012;112(8):1134–1137. doi: 10.1016/j.jand.2012.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Subar AF, Crafts J, Zimmerman TP, et al. Assessment of the accuracy of portion size reports using computer-based food photographs aids in the development of an automated self-administered 24-hour recall. J Am Diet Assoc. 2010;110(1):55–64. doi: 10.1016/j.jada.2009.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Subar AF, Thompson FE, Potischman N, et al. Formative research of a quick list for an automated self-administered 24-hour dietary recall. J Am Diet Assoc. 2007;107(6):1002–1007. doi: 10.1016/j.jada.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 27.Zimmerman TP, Hull SG, McNutt S, et al. Challenges in converting an interviewer-administered food probe database to self-administration in the National Cancer Institute automated self-administered 24-hour recall (ASA24). Journal of Food Composition and Analysis. 2009;22:S48–S51. doi: 10.1016/j.jfca.2009.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thompson F, Dixit-Joshi S, Potischman N, et al. Feasibility and performance of NCI's Automated Self-Administered 24-Hour recall (ASA24). Am J Epidemiol. 2013;177(11 Suppl):S1–S181. [Google Scholar]
- 29.Kirkpatrick SI, Subar AF, Douglass D, et al. Performance of the Automated Self-Administered 24-hour Recall relative to a measure of true intakes and to an interviewer-administered 24-h recall. The American Journal of Clinical Nutrition. 2014:ajcn. 083238. doi: 10.3945/ajcn.114.083238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Feskanich D, Sielaff BH, Chong K, Buzzard IM. Computerized collection and analysis of dietary intake information. Comput Methods Programs Biomed. 1989;30(1):47–57. doi: 10.1016/0169-2607(89)90122-3. [DOI] [PubMed] [Google Scholar]
- 31.Posner BM, Smigelski C, Duggal A, Morgan J, Cobb J, Cupples L. Validation of two-dimensional models for estimation of portion size in nutrition research. J Am Diet Assoc. 1992:738–741. [PubMed] [Google Scholar]
- 32.Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods (Second Edition) Sage Publications, Inc.; Thousand Oaks, CA: 2002. [Google Scholar]
- 33.DeVellis RF. Scale Development: Theory and Applications. Second Edition. Sage Publications, Inc; Thousand Oaks, CA: 2003. [Google Scholar]
- 34.Kanyongo GY, Brook GP, Kyei-Blankson L, Gocmen G. Reliability and statistical power: how measurement fallibility affects power and required sample sizes for several parametric and nonparametric statistics. Journal of Modern Applied Statistical Methods. 2007;6(1):9. [Google Scholar]
- 35.Nelson M, Black AE, Morris JA, Cole TJ. Between-and within-subject variation in nutrient intake from infancy to old age: Estimating the number of days required to rank dietary intakes with desired precision. American Journal of Clinical Nutrition. 1989;50(1):155–167. doi: 10.1093/ajcn/50.1.155. [DOI] [PubMed] [Google Scholar]
- 36.Pereira RA, Araujo MC, Lopes TdS, Yokoo EM. How many 24-hour recalls or food records are required to estimate usual energy and nutrient intake? Cadernos de Saúde Pública. 2010;26(11):2101–2111. doi: 10.1590/s0102-311x2010001100011. [DOI] [PubMed] [Google Scholar]
- 37.Arab L, Wesseling-Perry K, Jardack P, Henry J, Winter A. Eight self-administered 24-hour dietary recalls using the Internet are feasible in African Americans and Whites: the energetics study. J Am Diet Assoc. 2010;110(6):857–864. doi: 10.1016/j.jada.2010.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Martin CK, Nicklas T, Gunturk B, Correa JB, Allen H, Champagne C. Measuring food intake with digital photography. Journal of Human Nutrition and Dietetics. 2014;27(s1):72–81. doi: 10.1111/jhn.12014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dong Y, Scisco J, Wilson M, Muth E, Hoover A. Detecting periods of eating during free-living by tracking wrist motion. Biomedical and Health Informatics, IEEE Journal of. 2014;18(4):1253–1260. doi: 10.1109/JBHI.2013.2282471. [DOI] [PubMed] [Google Scholar]
- 40.Kipnis V, Midthune D, Buckman DW, et al. Modeling data with excess zeros and measurement error: Application to evaluating relationships between episodically consumed foods and health outcomes. Biometrics. 2009;65(4):1003–1010. doi: 10.1111/j.1541-0420.2009.01223.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vance VA, Woodruff SJ, McCargar LJ, Husted J, Hanning RM. Self-reported dietary energy intake of normal weight, overweight and obese adolescents. Public Health Nutr. 2009;12(02):222–227. doi: 10.1017/S1368980008003108. [DOI] [PubMed] [Google Scholar]
- 42.Baxter SD, Hitchcock DB, Guinn CH, et al. A validation study concerning the effects of interview content, retention interval, and grade on children's recall accuracy for dietary intake and/or physical activity. Journal of the Academy of Nutrition and Dietetics. 2014;114(12):1902–1914. doi: 10.1016/j.jand.2014.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Baxter SD, Hitchcock DB, Guinn CH, et al. A pilot study of the effects of interview content, retention interval, and grade on accuracy of dietary information from children. Journal of Nutrition Education and Behavior. 2013;45(4):368–373. doi: 10.1016/j.jneb.2013.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]