Abstract
Objectives
To report the findings of a metasynthesis review of qualitative studies on patient and provider experiences and perspectives on linkage and retention in HIV care.
Design
The review is an extraction, aggregation, interpretation and synthesis of qualitative findings based on the Sandelowski and Barroso method.
Data sources
A search of the literature was conducted in the databases Cumulative Index to Nursing and Allied Health, PubMed and PsycInfo for articles published from 2008–2013. Inclusion criteria were qualitative research articles published in English from across the world and in peer-reviewed journals. Literature reviews, conference abstracts and grey literature were excluded from this metasynthesis.
Review Methods
The review consisted of a) comprehensive search, b) study classification, c) abstraction of findings, d) synthesis. Of the 4640 citations screened, 69 articles were included for this metasynthesis.
Results
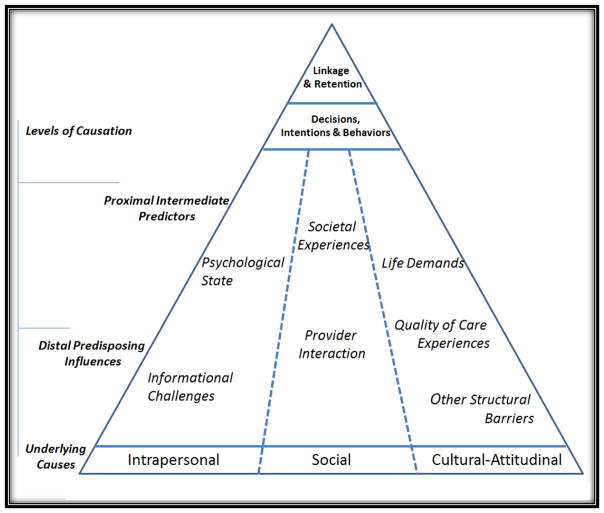
69 unique articles from 44 countries were included. This metasynthesis takes into account the perspectives of at least 2263 HIV-positive participants (740 men, 1008 women, 78 transgender individuals and 437 unspecified sex) and 994 healthcare providers, family members and community members. The most salient barriers and facilitators to HIV linkage and retention in HIV care affirm ecological factors that are mostly beyond individual patients’ control. Triadic streams of influence concurrently affect care engagement that include a person’s psychological state upon diagnosis and their informational challenges (intrapersonal stream); one-on-one interactions with providers and their immediate community (social stream); and life demands, overall quality of care experiences and other structural barriers (cultural-attitudinal stream). Each stream’s influence on HIV care engagement varies at any given point to reflect an individual’s evolving and unique experiences with HIV infection throughout the illness trajectory.
Conclusion
There is sufficient evidence that detail how to best link and retain patients in HIV care. Themes identified indicate going beyond individual-level factors and towards shifting attention and resources to systems that patients navigate. Forceful structural-level actions are needed to correct these long-identified barriers and enhance care engagement facilitators.
The combined advancements in HIV testing technology plus mass screening campaigns have resulted in an increase of people diagnosed with HIV. Developments in treatment options in the last two decades have transformed a diagnosis of HIV infection into a manageable chronic condition. Timely engagement with HIV care has implications for long-lasting successful treatment and antiretroviral adherence for people who test positive for HIV. As seen from a seven-year treatment program in South Africa, linking newly diagnosed people to care is crucial because those retained in care have substantially lower HIV viral loads than those who are not (Stinson, Ford, Cox, & Boulle, 2014). Additionally, a multi-state, epidemiological project in the United States showed that virally-suppressed, HIV-infected adults were likely to engage in less risky sexual behavior than those who are not suppressed (Mattson et al., 2014). Further, findings from retrospective studies established that individuals engaged in care had better survival outcomes than those not as engaged with the healthcare system and that missed visits specifically within the first year of outpatient HIV treatment had deleterious effects on long-term mortality (Giordano et al., 2007; Mugavero et al., 2009). Finally, linkage and retention is also crucial in preventing transmission as viral suppression among people with HIV reduces transmission (Cohen et al., 2011; Yehia et al., 2014) and thus is a pillar of Treatment as Prevention.
A delay in enrolling patients in care and losing them to attrition undermines the benefits of HIV screening campaigns and virologic suppression from mass distribution of antiretrovirals (Gardner, McLees, Steiner, Del Rio, & Burman, 2011). Failure to engage and retain in care can lead to cessation of ARV medication adherence and reversal of the benefits of antiretrovirals (Bangsberg, Kroetz, & Deeks, 2007; Deeks et al., 2009). Globally, with only 65% of eligible patients in 2012 receiving antiretrovirals, UNAIDS established an ambitious goal (‘90-90-90’) that aims to increase to 90% the total number of people with HIV who are diagnosed, are receiving antiretrovirals and are virally suppressed by 2020 (UNAIDS), 2014). In the United States, the National HIV/AIDS Strategy has been updated to also increase from 65% to 90% the proportion of newly-diagnosed patients in clinical care three months after their diagnoses (ONAP, 2015). However, virologic suppression is premised largely on patients’ sustained medical engagement. Given the variety of care services provided between high-resource and resource-challenged settings, there is currently no consensus definition on HIV linkage and retention to care (Okeke, Ostermann, & Thielman, 2014). For purposes of this review, linkage to HIV care is defined as an initial encounter with an HIV care provider within 90 days of diagnosis while retention comprises two or more kept visits at least 90 days apart in a 12-month period (United States Department of Health and Human Services, 2012).
This report is part of a larger metasynthesis study that examined factors affecting the HIV Treatment Cascade. Also known as the HIV/AIDS Care Continuum, the HIV Treatment Cascade is informed by population-level surveillance and clinical-record metrics (Gardner et al., 2011). However, lost in these statistics are the perspectives of those who delay, are partially retained or those who cycle in and out of medical care that may not be consistent with standard continuum of care measures (Castel et al., 2015). Individual perspectives are needed because engagement and retention are the crux of HIV treatment and are the inextricable link between testing seropositive for HIV, linkage to care and effective reduction in viral load (Brennan, Browne, & Horgan, 2014). Qualitative studies from 2008–2013 that had data on linkage and retention factors were analyzed to capture recent findings from patients, providers and key stakeholders about factors that inhibit or facilitate quality of care engagement. Qualitative metasynthesis was selected because this form of inquiry offers an integrated strategy to describe and explain behavior rather than providing a mere summary view of unlinked features (Sandelowski & Barroso, 2007). To facilitate a better contextual understanding of perspectives on engagement and retention in care, this metasynthesis focuses on the literature about patients linking to and staying in care after a diagnosis of HIV infection, the two middle segments of the HIV Treatment Cascade. The first aim of this report was to determine factors that influence linkage and retention in care with which people diagnosed with HIV infection must contend. Also, because metasynthesis studies are an efficient way to condense literature for clinical practice, our second aim was to determine what healthcare providers can do to enhance linkage and retention in care for people with HIV infection.
Methods
Search Strategy
This review follows key metasynthesis guidelines developed by Sandelowski and Barroso (2007) starting with a comprehensive automated searches of the literature found in three electronic databases (Cumulative Index to Nursing and Allied Health Literature [CINAHL], MEDLINE [PubMed] and PsycINFO). The following cross-referenced search terms (i.e., index terms, keywords, proximity terms) were used: ‘Human Immunodeficiency Virus’, ‘Acquired Immune Deficiency Syndrome’, ‘qualitative’, and ‘themes’. The combination of Boolean terms (and, or, not) were also added. Table 1 is an example of the complete CINAHL search strategy protocol. The inclusion criteria for this review include: a) qualitative research studies or the qualitative findings from mixed methods studies, b) published in English and in peer-reviewed journals, and c) published from 2008 to 2013. Reports published prior to 2008 were excluded because we wanted to capture the most current experiences and insights of participants and to avoid the relevancy issues associated with dated findings (Barroso, Sandelowski, & Voils, 2006). Grey literature, reviews, and articles not written in English were also excluded. No geographic restrictions were used during the search because we wanted to reflect the global experiences and views of people with HIV across study settings and regardless of resource availability.
Table 1.
Sample CINAHL Search Protocol
| Search # | # Results | |
|---|---|---|
| 1 | MH “Human Immunodeficiency Virus+” OR MH “HIV Infections+” OR TI HIV OR AB HIV OR TI “Human Immunodeficiency Virus*” OR AB “Human Immunodeficiency Virus*” OR TI “Human Immune Deficiency Virus” OR AB “Human Immune Deficiency Virus” OR MH “Acquired Immunodeficiency Syndrome” OR TI “Acquired Immunodeficiency Syndrome*” OR AB “Acquired Immunodeficiency Syndrome*” OR TI “Acquired Immune Deficiency Syndrome*” OR AB “Acquired Immune Deficiency Syndrome*” OR TI “Acquired Immuno-Deficiency Syndrome*” OR AB “Acquired Immuno-Deficiency Syndrome*” OR TI “AIDS virus*” OR AB “AIDS virus*” OR TI AIDS-related OR AB AIDS- related OR TI AIDS-associated OR AB AIDS-associated OR TX “AIDS serodiagnosis” OR TI Antiretroviral OR AB Antiretroviral OR MH “Anti-HIV Agents+” OR TI Anti-HIV OR AB Anti-HIV | 69,716 |
| #2 | TI qualitative OR AB qualitative OR TI themes OR AB themes | 57,904 |
| #3 | #1 AND #2 | 2,369 |
| #4 | #3 NOT (PT Editorial OR PT Letter OR PT Commentary) | 2,333 |
| #5 | #5 Filters: English, Journal Article, 2008- | 1,119 |
: searches for variant endings;
[AB]: Abstract; [MH]:CINAHL Subject Heading; [PT]: Publication Type; [TI]: Title
We sought the assistance of an information specialist from the Duke University Medical Library to assure search thoroughness. Additionally, principles of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) framework for data retrieval were adapted for this metasynthesis study (i.e., identification, screening, eligibility, and inclusion). Additionally, the 21-item Enhancing Transparency in Reporting The Synthesis of Qualitative Research [ENTREQ] statement (Tong, Flemming, McInnes, Oliver, & Craig, 2012) was also utilized to report the common stages we undertook in the synthesis of these qualitative health reports. Finally, to ensure that a thorough search with maximum specificity was conducted, the validated McMaster Qualitative Filter was used (Letts et al., 2007).
Search Appraisal and Results
This metasyntheses project did not employ any quality appraisal metric due to a lack of agreement in the field about what constitutes a ‘good’ qualitative study (Sandelowski & Barroso, 2007). Sandelowski (2015) further elaborated that “the process of judging inevitably entails the active deployment of taste, or the selection of those considerations deemed applicable to any one object of evaluation in addition to the continual (re)interpretation of those considerations and their applicability to any other comparable object of evaluation (p. 89).” With our tandem focus on 1.) analyzing the results of each study ‘as is’ to remain as close to the data provided by each participant, and 2.) including studies from around the globe, which represented diversity in all aspects of research, the use of an appraisal metric would have forced a very subjective assessment which also had little relevance to our study aims (LeBlanc, Flores, & Barroso, 2016).
Metasynthesis Approach
Extraction of the data began by importing the retrieved studies from the electronic searches into EndNote for citation management. The articles were then read and summarized into Excel spreadsheets using the Matrix method (Garrard, 2013). Column headings about pertinent study details (i.e., design, sample and findings) were used in these evidence tables, along with identifying which components of the Treatment Cascade they addressed (whether testing and notification of results, linkage and retention to HIV care, or antiretroviral initiation and viral suppression). Many articles had several unique findings applicable to multiple components of the HIV Treatment Cascade and therefore cited more than once. Data extraction was performed by DF and NL independently with discrepancies addressed and resolved during team discussions.
Aggregation consisted of first writing summary statements about each finding. These sentences were the reviewers’ summation of the findings that also included direct quotes or key phrases that seemed to describe elements of the phenomenon under study. Next, using Graneheim and Lundman’s content analysis (2004), similar findings were grouped into meaning units. These initial meaning units identified the salient factors that facilitated or inhibited successful linkage to and retention in care across multiple sites. These units were synthesized further to create categories and eventually into consensus themes that addressed our primary metasynthesis aim.
Synthesis was enhanced through reciprocal translation - the inductive constant comparison of our emergent findings in combination with imported concepts (Noblit & Hare, 1988; Sandelowski & Barroso, 2007) from the Triadic Streams of Influence framework (described below). The subsequent recommendations in this study fulfill our secondary aim and are based on findings from the themes grouped according to what works (facilitators) and what does not work (barriers) when linking and retaining patients into HIV care. All three authors contributed evenly in the synthesis and write-up of the manuscript.
Findings
The search of the three databases yielded 4640 initial citations; 1580 duplicate articles were removed. Next, the titles and abstracts of 3060 unique articles were screened. After applying the inclusion and exclusion criteria, we accepted 287 unique articles about the entire HIV Treatment Cascade for metasynthesis. With the potential to exclude relevant literature due to stringent exclusion criteria, we reviewed articles that did not clearly fall into our criteria, discussed it with the review team and decided to err on the side of inclusion (Sandelowski, Voils, Barroso, & Lee, 2008). The findings that focus on linkage and retention barriers and facilitators from 69 articles served as the basis for this current report (Figure 1)
Fig. 1.
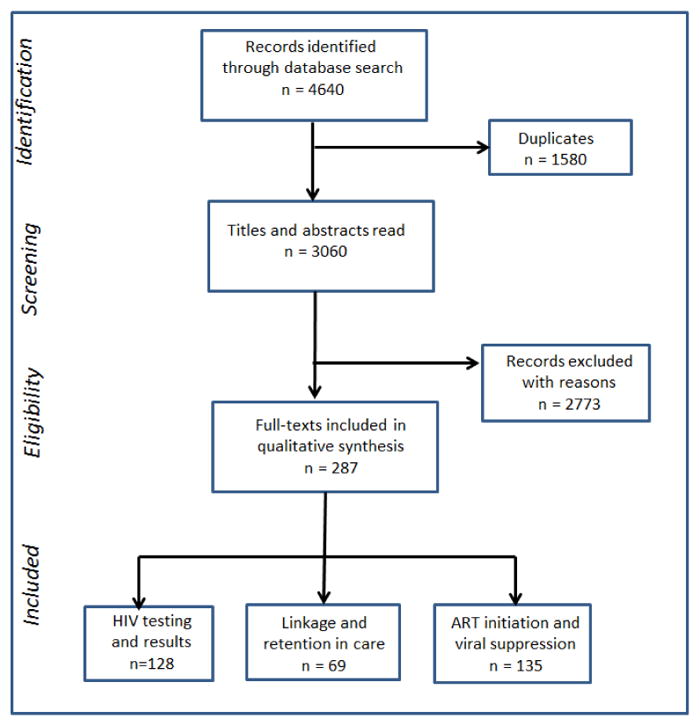
Flow Search
The majority of studies identified contextual factors that facilitate or inhibit linkage to and retention in care for HIV infection. These factors centered on the interaction of patients with family, community members and providers and their interface with the larger healthcare system. The most studied settings were in the United States (22 reports) followed by South Africa (9), Uganda (6), Nigeria (4), Zimbabwe (4) and China (4). There were at least 3257 people included in these studies; 2263 patients or HIV-positive participants from the community (740 men, 1008 women, 78 transgender individuals and 437 people with unspecified gender). 994 other people were included in the studies such as family members, friends, physicians, nurses, treatment advocates, caregivers, clinic staff, program directors, social workers and other key stakeholders. Most of the qualitative data were collected using single method data collection techniques (36 studies used one-on-one interviews followed by 8 focus group discussions) while 26 other studies used multimethod data collection techniques (the most common being a combination of interviews and focus groups used in 19 studies). Fieldwork notes, observations, photovoice, and record reviews were the other sources of data in the included studies.
The findings from this metasynthesis revealed the multifactorial and ecological elements that determine an HIV-infected patient’s relationship with their community and healthcare system. Linkage and retention factors are thus presented here through an adaptation of the Theory of Triadic Influence which underscores three streams of influence that concurrently impact care engagement (Figure 2) (Flay, Snyder, & Petraitis, 2009). First, the intrapersonal stream includes innate predispositions, general competencies and personality traits (such as coping abilities and self-esteem) that converge on one’s efficacy to perform a behavior. Second, the social stream encompasses the individual’s immediate surroundings that are mostly out of their control (such as feedback from family) and may take the form of pressure to comply with expected behavior. Finally, the cultural-attitudinal stream pertains to broader structural elements (such as religion and health policies) that exert palpable influence on patient behavior through ingrained cultural mechanisms.
Fig. 2.
Triadic Streams of Influence Impacting HIV Linkage and Retention to Care
Additionally, this ecological framework posits that these influences interact across the three levels. This triad of influences simultaneously determines how people engage in health-seeking and health-maintaining behaviors. Table 2 is a complete list of the findings from the included articles and how they supported emerging themes as organized through the Triadic Streams of Influence.
Table 2.
Included Articles: Enrollment and Retention in HIV Care
Abbreviations: PS - Psychological State, IC - Informational Challenges, SE- Societal Experiences, PI - Provider Interaction, LD - Life Demands, QCE - Quality of Care Experiences, OSB - Other Structural Barriers
Narrative Summary
Intrapersonal Stream
Psychological State Upon Diagnosis
The psychological state of an individual upon diagnosis with HIV and immediately thereafter was a crucial factor that impacted care engagement. Many people’s denial of the results prevented them from seeking medical care. Shame associated with specific transmission modes kept people from dealing with their diagnoses. For others, the shock from the unexpected results was immobilizing and revealed infidelity problems in their primary relationships. Issues related to self-esteem, such as self-worth as an HIV-infected wife or future effectiveness of a mother to care for her children, became a consuming worry that took primacy over how to take care of her own health.
Feelings of uncertainty impacted linkage and retention because being in shock and not knowing much about HIV resulted in trepidation and indecisiveness. Fear of the unknown coupled with the inability to formulate expectations resulted in hesitation to enroll in medical care. Contributing to this uncertainty was anticipatory stigma that kept people from incorporating the new reality of HIV into their lives. Even before people shared their status and experienced stigmatization, the uncertain fate of their primary relationships or employment status plus the threat of exclusion, isolation or rejection prevented tentative steps towards disclosure.
Among those who have been diagnosed for a while, a distinct psychological impediment to care retention included the mental fatigue experienced from being engaged in care. For some who were HIV-infected but asymptomatic or did not meet clinical diagnosis for AIDS, the successful management of the disease due to being in care led them to question the necessity of repeated medical tests and procedures. From patient and provider reports, feeling better and not having symptoms of HIV infection subsequently caused them to start missing medical appointments and resulted in care disengagement.
Informational Challenges
An oppositional dynamic centered on individual’s knowledge about HIV/AIDS emerged from the qualitative literature. On one hand, a commonly noted barrier involved people’s doubts about the test’s reliability, particularly among individuals who were unaware of their risk behaviors prior to diagnosis. For many, unfamiliarity with or misinformation about HIV transmission or the meaning of an HIV-positive diagnosis also prevented care-seeking responses. On the other hand, linkage to care was dramatically facilitated through patient education. Extended post-test counselling, both immediately after notification of results or through multiple sessions thereafter, allowed for the accommodation of patients’ psychological reactions and enabled a thorough answering of questions or clarification of misconceptions. In one study of persons diagnosed with HIV but were never engaged in care, one respondent lamented that during diagnosis, providers “could’ve sat down and really talked to me about it,” pg 124 (Garland et al., 2011). Ongoing patient education from peers in support groups or by caseworkers was also a salient feature of this informational factor that contributed to HIV literacy for eventual care competence.
Social Stream
Interaction with Providers
Provider attributes worked in two ways that either ensured or deterred care engagement. The ability of providers to foster a collaborative partnership resulted in unbiased care that established rapport and eventual care relationships with patients. These providers were perceived as members of a network who were supportive and whom patients could view as proxy for absent family or friends. Providers who had a positive impact on patients’ initial care experiences included staff members who tested them for HIV and explained their results, receptionists at the front office, and the doctors and nurses they came into contact with after diagnosis. However, persistent condescending attitudes by some providers hindered the formation of trusting relationships in the clinical setting. Negative experiences included a sense of being disrespected, provider insensitivity of patient emotions, and worries about having confidential health information compromised. Because flaws in the healthcare system exist, such as forced disclosure due to confidentiality breaches, people delayed decision-making on matters that could jeopardize their suddenly uncertain personal and financial prospects.
Societal Experiences
Family and friends’ reactions to an individual’s HIV-positive diagnosis impacted linkage and retention. Supportive networks of families and friends helped individuals with HIV infection cope with their diagnosis and encouraged care engagement. This assistance was extended through a variety of ways that included child care, financial aid, transportation and psychological support. Negative reactions from family and friends, however, made it difficult for individuals to seek or be engaged in their care. Challenges surrounding disclosure of an HIV-infected status were reported most often by women who were at risk for family and spousal rejection, withdrawal of financial support or expulsion from the home. This resulted in non-disclosure, which meant foregoing medical care so they could be at home or only have sporadic contact with the healthcare system for fear of raising suspicions. Also, experiences with actual stigmatizing actions by family and friends resulted in an inability to seek care due to severance of financial support or a diminished capacity to stay in care as the reduction in size of their supportive network meant less assistance at home or in the community. Reports from rural settings and communities with shared misconceptions about HIV also point to a higher degree of stigma for those seen entering HIV clinics or suspected of being HIV-infected due to their repeated contacts with the medical establishment.
Cultural-Attitudinal Stream
Life Demands
Across settings, competing life demands was an often-cited barrier to linkage and retention. Most pressing of these vying concerns are the needs of one’s family followed by expectations in the workplace. Because these commitments did not diminish in significance after a diagnosis of HIV infection, role strain arose when patients had to be away from home or had to manage multiple clinic appointments during work hours. Further, financial difficulties became an impediment when limited resources had to be divided between costs of being in care versus household expenses. For example, “everything concerning this illness is tied to money,” according to one Nigerian man, while the widowed women from a neighboring town described their financial tribulations to challenges related to hospital bills, children’s school fees and buying food (Agbonyitor, 2009).
Quality of Care Experiences
Structural factors related to quality of care received were noted repeatedly across participant populations. Broadly, the experiences of individuals when they interfaced with the healthcare system had effects that impacted their immediate and long-term care engagement behaviors. Structural factors identified that positively linked and kept patients in care began with active referrals and were sustained through case management. Linkage was more successful when patients received their diagnoses and had someone (e.g., testing counselors, peer navigators, healthcare staff) who actively worked to link them into care by assisting them in setting up initial visits to clinics. The provision of guidance and follow-up with individuals through active referrals worked better than passive strategies to linkage such as handing out brochures or leaflets. Case management was also a strong facilitator to linkage and retention because of its holistic approach. Case managers assisted people to prioritize their needs, gradually introduced them to available resources, helped them complete necessary forms for services, identified their personal strengths and taught them skills about disclosing their status to supportive networks. Both active referrals and case management were strategies that assisted people to navigate complex health systems.
While one-on-one interactions with care providers belong in the social stream, the overall efficiency of the health system falls within the cultural-attitudinal dimension. As a macro-level factor, the healthcare staff’s specialized training was deemed influential in keeping patients engaged in their care. Patients noted that the inadequate number of skilled providers and the high turnover rate at HIV clinics made it difficult to form trusting relationships with members of the healthcare team.
The location of clinics was underscored as a salient factor that had oppositional implications for care engagement. According to study participants, clinics that were far from people’s homes or workplace prohibited access to care. Because travel to and from clinics entailed a few hours of disruption from home- or work-related duties, patients either had to arrange for childcare while they kept their medical appointments or were absent from the workplace. Meanwhile, other published studies also highlighted that comprehensive services in centralized sites tended to minimize disruption to daily life and resulted in care compliance. This integration of care services, including electronic health records, resulted in efficiency that reduced the amount of time required for processing paperwork and the receipt of laboratory results. Fragmentation of care, duplication of medical tests, and the uneven quality of care received across varying clinics and hospitals were minimized when services were housed under one roof. This arrangement also reduced perceptions of inadequate clinic management, and patient mistrust and frustration with navigating the healthcare system.
Additional factors cited in studies that belong to quality of care concerns were inconvenient or limited clinic hours, long queues that had implications for confidentiality, medical appointments that were far into the future, and communication barriers. Two primary issues regarding communication took the form of dissonance between the different languages spoken by patients and healthcare providers and the inability of clinic staff to explain complex medical information to lay people.
Other Structural Barriers
Long-held beliefs and shared community views about health were also salient environmental influences that affected care engagement. Going to traditional healers was identified as a routine activity primarily among participants from low-resource settings. Individuals placed a premium on what their spiritual healers offered for their maladies, which sometimes resulted in bypassing services available in the community clinic or city hospital. However, medical providers that incorporated traditional beliefs into HIV care succeeded in earning people’s trust and were sought out in conjunction with the receipt of traditional medicine. Also, partnering with faith-based institutions in linkage and retention campaigns enabled those with disrupted family and peer relationships to have another support system. Finally, community beliefs about preventive health influenced people’s view on when to enter care. In some settings, wellness and illness prevention programs were viewed with suspicion while in other places, residents only equated clinics and hospitals with sickness and death. This resulted in delaying care among those in the asymptomatic phase despite exhibiting occasional symptoms of HIV infection; they were only receptive to medical care when they were unable to continue with daily routines.
Structural challenges experienced by key populations comprise the final set of environmental barriers to linkage and retention. These are closely linked to policies directed at specific populations that make it difficult for them to access health services. Persistent threats of criminalization associated with illegal sex work, drug use or certain sex acts served as barriers to care engagement in both low- and high-resources settings. Across the globe, deportation threats against undocumented immigrants keep individuals from seeking medical attention. Gender bias inherent in many settings also hinders enrollment in care, such as when providers refuse women care without their husband’s consent. Gender stereotypes also affect men as notions of masculinity keep them from prioritizing their health as time spent at clinics may denote weakness or reduce their ability to be the family breadwinner due to absence from work.
Discussion
The identification of the unique experiences of individuals with HIV regarding linkage and retention in care as presented through the Triadic Streams of Influence Framework reveal that strategies used to mitigate barriers and enhance facilitators must be multifactorial and ecological in their approach. With the recognition that multiple societal processes and mechanisms influence care retention (Blank et al., 2015), the likelihood of sustaining successful single-level interventions to link patients into and keep them engaged in care would be difficult if these strategies ignored relevant contextual factors that may exert the same or even stronger influence. Our findings indicate that each stream may vary in the level of influence it exerts at any given point to reflect an individual’s evolving and unique experiences with HIV infection and their interaction with the healthcare system throughout the illness trajectory. This accounts for the variety of behaviors and experiences one has from diagnosis, initial reaction, denial, enrollment, withdrawal or subsequent reengagement into care. For example, despite an extended period of disbelief or denial upon learning of being HIV-infected (intrapersonal), individuals may find themselves enrolled in care because high social support from family members (social) have linked them to the local health department that has the resources and systems in place to provide compassionate medical care (cultural-attitudinal).
From the data, it also appears that elements in each stream of influence may change positions throughout the care process, which reflects the alternating proximal and distal causes that facilitate or inhibit care engagement. To continue with the scenario above, it is a common situation that even among long-term survivors who have been fully engaged in their care for years, they may still be lost to care when helpful relatives who previously provided transportation assistance move away or when available health services are discontinued or de-funded. Moreover, what may be a facilitator in one section of the HIV Treatment Cascade may not be sufficient to ensure success in another section. For example, in a prospective observational study, Kelly and colleagues (2014) found that while high social support was associated with timely linkage to care for a cohort of newly diagnosed individuals, this same support was not predictive of subsequent retention in care.
Implications
Implications for Clinical Practice
Patient-Focused Recommendations
This metasynthesis has identified that the psychological state of an individual upon diagnosis has significant implications for their care-seeking behavior: the mindset upon diagnosis plus the initial impressions they have of the healthcare system combine to determine one’s lifelong care engagement. With the future enrollment and retention of individuals in care beginning at the testing site the moment they are diagnosed with HIV (Garland et al., 2011), providers must offer ample time and space for post-test counseling to thoroughly answer their questions. This runs counter to the trend of abbreviating or making post-test counseling advisable but not mandatory in medical care settings (Obermeyer & Osborn, 2007). From the findings, when providers take the time to inform patients that their symptoms are consistent with HIV/AIDS, this addresses denial about one’s status and facilitates acceptance of the diagnosis as a better option than to delay seeking care. This is accomplished as well by capitalizing on individuals’ sense of personal responsibility to stay healthy and by highlighting the peace of mind that comes with knowing they are taking command of their health. Elements of this approach are included in strength-based case management, which has been associated with positive health outcomes (Cargill, 2013), and identified as crucial in linkage and retention intervention work according to recent systematic reviews (Liau et al., 2013; Okeke et al., 2014).
For those who are new to care, active referrals and case management assists them to identify resources with which they may not be familiar. These two strategies result in familiarity with health care systems, insurance/payment options, and address their anxiety about specific access issues such as how to receive care in rural settings. Similarly identified in intervention studies as effective in retaining patients in HIV primary care (Higa, Marks, Crepaz, Liau, & Lyles, 2012), peer navigators or treatment advocates can enhance care retention by educating about the medical management of HIV/AIDS and the need for routine medical check-ups and laboratory work, and strategies for dealing with side effects from medications.
All people involved with the care of HIV-infected individuals should initiate stigma management education, especially for newly diagnosed individuals. Our findings indicate that emphasizing stigma management for both internalized and felt stigma is better when one is healthy in care compared to when they are sick and out of care. This is reinforced by presenting engagement in care as a sign of hope, which runs counter to the despondency initially experienced during diagnosis. Recent quantitative studies on care engagement have found that the negative self-image component of HIV stigma significantly hinders early care seeking among those who are newly diagnosed (Hussen, Harper, Bauermeister, & Hightow-Weidman, 2015). We found that when the healthcare team educates patients about disclosure strategies, they help identify support systems and prevent hopelessness and social isolation. This is reinforced with counseling and by establishing peer support groups and programs that foster acceptance of people living with HIV infection and disclosure to family and community.
Gender inequality as experienced by women and stereotypes about masculinity that affect men both make being linked to and retained in HIV care a challenge. Providers can explore with patients the gender and power structures in their lives and ways to manage their health concerns. Among couples, regardless of discordance, encouraging shared decision-making and appealing to the partner’s sense of responsibility to the family is beneficial for engagement in care. For women, HIV care outreach by openly HIV-infected women serving as mentors may lead to a better campaign for other women to engage in care. Further, promoting the image of a healthy mother unencumbered by HIV may counter the stigma associated with dated stereotypes of women with HIV and motherhood. For men, advocating for male-friendly health clinics and hiring male clinic staffers who can normalize HIV care for other men in the community can improve linkage to and retention in care. Perceived threats to one’s masculinity may be clarified by men trained to educate their male peers about the value of HIV care.
Provider-Focused Recommendations
Most of the findings from the perspective of patients worldwide revealed healthcare-related issues and suggestions for improvement in the delivery of care. This underscores the role healthcare providers have in the successful enrollment and sustained engagement of patients. Healthcare staff must be cognizant that the first visit to HIV clinical care has lasting retention implications. Staff-patient rapport is enhanced if patients see staff members as caring and trustworthy. Providers who are competent, who value patients’ input, and who are nonjudgmental encourage active participation in care. Collaborative patient-provider relationships, geared towards establishing individual independence in care management, must be a priority. However, patients also caution that linking people into HIV care must not take priority over but be sensitive of their self-identified concerns (e.g., competing life demands or co-morbidity issues such as alcohol or drug use).
The condescending attitudes that patients have reported, ranging from being patronized to outright verbal abuse by clinic staff, causes patients to drop out of care or rely solely on non-biomedical treatment. Poor patient-provider relationships impair optimal linkage to and retention in care, and may be addressed with education of staff on the significance of establishing trust and rapport, protecting confidentiality and keeping biases in check. The reality for many individuals, especially those from high-risk groups such as IV drug users, commercial sex workers and men who have sex with men, is that providers may perpetuate stigma and bias in the healthcare setting. To this end, emphasizing the provision of judgment-free medical services to counter provider mistrust becomes imperative. Improving provider communication enhances courtesy and increases the perception of trustworthiness. Similarly, undocumented immigrant populations may become engaged in care when policies are clarified with them, especially in countries where receipt of care does not have any deportation repercussions or residency implications. When dealing with patients who have a history of imprisonment, address repeated incarcerations and provide suggestions on how to ensure staying in care within the prison health system. Further, providers who respectfully identify the limitations of traditional healers for the treatment of HIV/AIDS avoid alienating their patients. It is recommended that providers explore with patients their beliefs about spirituality and how care engagement can be enhanced by these beliefs.
System Level Recommendations
Along with the educational interventions focused on empowering patients to be active participants, logistical reinforcement for healthcare staff is essential. Structural support when additional responsibilities are assigned to medical staff allows them to accommodate increases in their workload. Streamlined clinical operations that ensure privacy, eliminate repetitive or duplicate requirements, and reduce wait times create efficient clinic flow. Further, the number of healthcare providers must increase to support the complex needs of people living with HIV infection.
Arranging for multidisciplinary services in one centralized location facilitates care retention. If centralized care is not available, referral systems between community clinics and central hospitals must be enhanced. Arranging for HIV care services via telehealth or at integrated community clinics beyond one centralized hospital also reduce patients’ financial and travel burdens. This includes access to patient information and timely communication between collaborating providers, especially in emergency situations. As described by Carter and colleagues (2015), the use of information technology for sharing information between providers is beneficial. It is recommended that medical documentation be accurate and reflect the nuanced details about patients’ lives such as a transgender person’s gender identity or to whom a mother with HIV has disclosed her status.
Finally, because people seen going into well-known HIV clinics in the community can be stigmatized, alternative care sites are sometimes necessary to enroll and retain individuals in care. This may be achieved through mobile care units or by incorporating HIV care at clinic sites that provide services to other populations. Further, to answer issues of limited and inaccessible sites or clinic hours, extending clinic hours or providing medical services on non-work days may be crucial. According to patients, a good blueprint for retention usually includes appointment reminders, childcare assistance, and engaging patients in between clinic appointments through letters and phone calls. Additionally, limited finance and transportation problems undercut care initiation and retention efforts. To this end, vouchers that offset food and travel costs have been shown to address these well-known constraints.
Implications for Research
Many of the issues elucidated in this metasynthesis are beyond the control of individual patients. However, most interventions to date aimed at promoting the linkage and utilization of medical care among people with HIV have mostly focused on individual-level factors (Liau et al., 2013). Because multifactorial ecological factors synergistically affect individual-level outcomes, research on the macro-level impediments to system changes similar to the recommendations in this study must be a priority. Research into the experiences of providers and key stakeholders who undertake process improvement projects around HIV surveillance and care delivery can identify persistent macro-level linkage and retention barriers. For example, an individual’s cluster of differentiation4 count and viral load as reported in health surveillance systems can be used as proxy for entry to care and be further combined with records from other data records such as the AIDS Drug Assistance Program to monitor care engagement (Eaton, Saag, & Mugavero, 2014; Zetola et al., 2009). Additionally, investigations into AIDS service organizations’ work on the ground or HIV/AIDS professional organizations’ self-identified difficulties may more clearly identify long-standing care issues that inhibit or facilitate their members’ work.
Strengths and Limitations
A multitude of systematic reviews on HIV linkage and retention literature, with emphasis on intervention work, has been published in recent years (Govindasamy et al., 2014; Higa, Crepaz, & Mullins, 2016; Liau et al., 2013). This article’s main strength is that, to our knowledge, it is the first to systematically examine from qualitative studies the factors that affect linkage and retention issues in HIV care. By its nature, qualitative studies are able to provide rich details about a phenomenon that may be missed in quantitative studies. Further, our larger three-part metasyntheses project is an exhaustive examination of recent literature based on an inclusive global sample. The extraction of qualitative data from a larger dataset that involves the entire HIV Treatment Cascade also allowed us to examine linkage and retention issues in relation to - and not in isolation of - the other components of the care continuum.
However, the strengths of our study should be considered within several limitations. First, articles reviewed here were published from 2008 to 2013 and does not include the more recent linkage and retention literature from the last two years. Due to changes in study staff and resource challenges, the original timeline for extraction, analysis and dissemination was substantially delayed, which speaks about the protracted nature of qualitative metasynthesis work (Sandelowski & Barroso, 2007). Second, the included articles were retrieved from only three electronic databases which may have resulted in our missing of other pertinent literature. Finally, our exclusion of grey literature and articles not written in English has certainly limited the identification of other pertinent barriers and facilitators reported by non-English speaking participants and investigators.
Conclusion
Patients must first be linked to and retained in HIV care before the full benefits of viral suppression are achieved. When patients are not able to utilize HIV medical care, this diminishes the efficacy of antiretrovirals, undercuts prevention programs and wastes limited resources. Because the reasons for enrollment and retention in care are multifactorial, there is impetus to more forcefully address the same issues that have been reported since the early days of the epidemic. The collective voices and stories of the people from these qualitative studies underscore consistent themes and point to going beyond individual-level factors and towards shifting our attention to structures that they must navigate. Strengthening the capacity of healthcare programs to address the barriers and to enhance the facilitators identified in this metasynthesis will help make the goal of fostering an AIDS-free generation a reality.
Supplementary Material
Contribution of the Paper.
What is already known about this topic?
The inability of patients to be linked and retained in HIV care diminishes ART efficacy to prevent AIDS-related sequelae.
Patients successfully engaged in HIV care reduce transmission of the virus.
Linkage and retention to HIV care is affected by multiple individual-level factors that either serve as barriers or facilitators to care engagement.
What this paper adds
This metasynthesis identified seven ecological factors across three streams of influence that affect linking and retaining patients with HIV in their care.
Healthcare providers’ actions during the clinical interface have lasting repercussions in the engagement of patients to their HIV care.
This study described the evolving nature of care engagement through the illness trajectory that explains how patients are linked and attempt to stay engaged with their medical care.
Focus on individual-level factors without regard to long-identified structures beyond the control of patients will continue to hamper successful linkage and retention in care of people with HIV.
Acknowledgments
The authors wish to thank Adrianne Leonardelli of Duke University Medical Library for her assistance.
Funding
NL’s work was supported by the Florida Educational Fund’s McKnight Doctoral Fellowship Program. DF was supported by a grant from the National Institute for Health’s NINR (Grant: 1F31NR015013) and a Surgeon General C. Everrett Koop HIV/AIDS Research Award.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bangsberg D, Kroetz D, Deeks S. Adherence-resistance relationships to combination HIV antiretroviral therapy. Curr HIV/AIDS Rep. 2007;4(2):65–72. doi: 10.1007/s11904-007-0010-0. [DOI] [PubMed] [Google Scholar]
- Barroso J, Sandelowski M, Voils CI. Research results have expiration dates: ensuring timely systematic reviews. J Eval Clin Pract. 2006;12(4):454–462. doi: 10.1111/j.1365-2753.2006.00729.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blank AE, Fletcher J, Verdecias N, Garcia I, Blackstock O, Cunningham C. Factors associated with retention and viral suppression among a cohort of HIV+ women of color. AIDS Patient Care STDS. 2015;29(Suppl 1):S27–35. doi: 10.1089/apc.2014.0272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan A, Browne JP, Horgan M. A systematic review of health service interventions to improve linkage with or retention in HIV care. AIDS Care. 2014;26(7):804–812. doi: 10.1080/09540121.2013.869536. [DOI] [PubMed] [Google Scholar]
- Cargill VA. Linkage, engagement, and retention in HIV care among vulnerable populations: “I”m sick and tired of being sick and tired”. Top Antivir Med. 2013;21(4):133–137. [PMC free article] [PubMed] [Google Scholar]
- Carter M, Wu H, Cohen S, Hightow-Weidman L, Lecher L, Peters PJ. Linkage and referral to HIV and other medical and social services: A focused literature review for sexually transmitted disease prevention and control programs. Sexually Transmitted Diseases. 2015 doi: 10.1097/OLQ.0000000000000290. ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castel AD, Tang W, Peterson J, Mikre M, Parenti D, Elion R, … Greenberg A. Sorting through the lost and found: are patient perceptions of engagement in care consistent with standard continuum of care measures? J Acquir Immune Defic Syndr. 2015;69(Suppl 1):S44–55. doi: 10.1097/qai.0000000000000575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, … Fleming TR. Prevention of HIV-1 Infection with Early Antiretroviral Therapy. New England Journal of Medicine. 2011;365(6):493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deeks SG, Gange SJ, Kitahata MM, Saag MS, Justice AC, Hogg RS, … Moore RD. Trends in multidrug treatment failure and subsequent mortality among antiretroviral therapy-experienced patients with HIV infection in North America. Clinical Infectious Diseases. 2009;49(10):1582–1590. doi: 10.1086/644768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton EF, Saag MS, Mugavero M. Engagement in Human Immunodeficiency Virus Care: Linkage, Retention, and Antiretroviral Therapy Adherence. Infectious Disease Clinics of North America. 2014;28(3):355–369. doi: 10.1016/j.idc.2014.06.004. http://dx.doi.org/10.1016/j.idc.2014.06.004. [DOI] [PubMed] [Google Scholar]
- Flay BR, Snyder F, Petraitis J. The theory of triadic influence. In: DiClemente R, Kegler M, Crosby R, editors. Emerging theories in health promotion practice and research. Vol. 2. New York: Jossey-Bass; 2009. pp. 451–510. [Google Scholar]
- Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800. doi: 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrard J. Health sciences literature review made easy. Jones & Bartlett Publishers; 2013. [Google Scholar]
- Giordano TP, Gifford AL, Clinton White A, Jr, Suarez-Almazor ME, Rabeneck L, Hartman C, … Morgan RO. Retention in Care: A Challenge to Survival with HIV Infection. Clinical Infectious Diseases. 2007;44(11):1493–1499. doi: 10.2307/4485427. [DOI] [PubMed] [Google Scholar]
- Govindasamy D, Meghij J, Negussi EK, Baggaley RC, Ford N, Kranzer K. Interventions to improve or facilitate linkage to or retention in pre-ART (HIV) care and initiation of ART in low-and middle-income settings-a systematic review. Journal of the International AIDS Society. 2014;17(1) doi: 10.7448/IAS.17.1.19032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Education Today. 2004;24(2):105–112. doi: 10.1016/j.nedt.2003.10.001. http://dx.doi.org/10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- Higa DH, Marks G, Crepaz N, Liau A, Lyles CM. Interventions to improve retention in HIV primary care: a systematic review of U.S. studies. Curr HIV/AIDS Rep. 2012;9(4):313–325. doi: 10.1007/s11904-012-0136-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussen SA, Harper GW, Bauermeister JA, Hightow-Weidman LB. Psychosocial influences on engagement in care among HIV-positive young black gay/bisexual and other men who have sex with men. AIDS Patient Care STDS. 2015;29(2):77–85. doi: 10.1089/apc.2014.0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV/AIDS. 90-90-90: An ambitious treatment target to help end the AIDS epidemic. Switzerland: 2014. Retrieved from http://www.unaids.org/sites/default/files/media_asset/90-90-90_en_0.pdf. [Google Scholar]
- Kelly JD, Hartman C, Graham J, Kallen MA, Giordano TP. Social support as a predictor of early diagnosis, linkage, retention, and adherence to HIV care: results from the steps study. Journal of the Association of Nurses in AIDS Care. 2014;25(5):405–413. doi: 10.1016/j.jana.2013.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leblanc N, Flores D, Barroso J. Facilitators and Barriers to HIV Screening A Qualitative Meta-Synthesis. Qualitative Health Research. 2016;26(3):294–306. doi: 10.1177/1049732315616624. [DOI] [PubMed] [Google Scholar]
- Letts L, Wilkins S, Law M, Stewart D, Bosch J, Westmorland M. McMaster Qualitative Filter for Maximum Specificity. 2013 Apr 30; 2007. Retrieved from http://www.srs-mcmaster.ca/ResearchResourcesnbsp/ResearchGroups/CentreforEvidenceBasedRehabilitation/EvidenceBasedPracticeResearchGroup/tabid/630/Default.aspx.
- Liau A, Crepaz N, Lyles C, Higa D, Mullins M, Deluca J, … Marks G. Interventions to Promote Linkage to and Utilization of HIV Medical Care Among HIV-diagnosed Persons: A Qualitative Systematic Review, 1996–2011. AIDS and Behavior. 2013;17(6):1941–1962. doi: 10.1007/s10461-013-0435-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattson CL, Freedman M, Fagan JL, Frazier EL, Beer L, Huang P, … Skarbinski J. Sexual risk behaviour and viral suppression among HIV-infected adults receiving medical care in the United States. Aids. 2014;28(8):1203–1211. doi: 10.1097/qad.0000000000000273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mugavero MJ, Lin HY, Willig JH, Westfall AO, Ulett KB, Routman JS, … Allison JJ. Missed visits and mortality among patients establishing initial outpatient HIV treatment. Clinical Infectious Diseases. 2009;48(2):248–256. doi: 10.1086/595705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noblit G, Hare R. Meta-ethnography: Synthesizing qualitative methods. Sage University Paper; Newbery Park, CA: 1988. [Google Scholar]
- Obermeyer CM, Osborn M. The Utilization of Testing and Counseling for HIV: A Review of the Social and Behavioral Evidence. American Journal of Public Health. 2007;97(10):1762–1774. doi: 10.2105/AJPH.2006.096263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okeke NL, Ostermann J, Thielman NM. Enhancing linkage and retention in HIV care: a review of interventions for highly resourced and resource-poor settings. Curr HIV/AIDS Rep. 2014;11(4):376–392. doi: 10.1007/s11904-014-0233-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of the National AIDS Policy. National HIV/AIDS Strategy for the United States: Updated to 2020. Washington, DC: 2015. Retrieved from https://aids.gov/federal-resources/national-hiv-aids-strategy/nhas-update.pdf. [Google Scholar]
- Park WB, Choe PG, Kim SH, Jo JH, Bang JH, Kim HB, … Choe KW. One-year adherence to clinic visits after highly active antiretroviral therapy: a predictor of clinical progress in HIV patients. Journal of Internal Medicine. 2007;261(3):268–275. doi: 10.1111/j.1365-2796.2006.01762.x. [DOI] [PubMed] [Google Scholar]
- Sandelowski M. A matter of taste: evaluating the quality of qualitative research. Nursing Inquiry. 2015;22(2):86–94. doi: 10.1111/nin.12080. [DOI] [PubMed] [Google Scholar]
- Sandelowski M, Barroso J. Handbook for synthesizing qualitative research. Springer Publishing Company; 2007. [Google Scholar]
- Sandelowski M, Voils CI, Barroso J, Lee E. “Distorted into clarity”: a methodological case study illustrating the paradox of systematic review. Research in Nursing and Health. 2008;31(5):454–465. doi: 10.1002/nur.20278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stinson K, Ford N, Cox V, Boulle A. Patients lost to care are more likely to be viremic than patients still in care. Clin Infect Dis. 2014;58(9):1344–1345. doi: 10.1093/cid/ciu072. [DOI] [PubMed] [Google Scholar]
- Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC medical research methodology. 2012;12(1):1. doi: 10.1186/1471-2288-12-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Health and Human Services. HIV core indicators. Washington, D.C: 2012. Retrieved from https://www.aids.gov/pdf/hhs-common-hiv-indicators.pdf. [Google Scholar]
- Yehia BR, French B, Fleishman JA, Metlay JP, Berry SA, Korthuis PT, … Gebo KA. Retention in care is more strongly associated with viral suppression in HIV-infected patients with lower versus higher CD4 counts. J Acquir Immune Defic Syndr. 2014;65(3):333–339. doi: 10.1097/qai.0000000000000023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zetola NM, Bernstein K, Ahrens K, Marcus JL, Philip S, Nieri G, … Klausner JD. Using surveillance data to monitor entry into care of newly diagnosed HIV-infected persons: San Francisco, 2006–2007. BMC Public Health. 2009;9:17. doi: 10.1186/1471-2458-9-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Articles Included in Linkage and Retention Metasynthesis
- 1.Abdelrahman I, Lohiniva AL, Kandeel A, et al. Learning about Barriers to Care for People Living with HIV in Egypt: A Qualitative Exploratory Study. Journal of the International Association of Providers of AIDS Care. 2013 doi: 10.1177/2325957413488180. [DOI] [PubMed]
- 2.Addo-Atuah J, Gourley D, Gourley G, et al. Accessibility of antiretroviral therapy in Ghana: convenience of access. SAHARA J: journal of Social Aspects of HIV/AIDS Research Alliance/SAHARA, Human Sciences Research Council. 2012;9(2):74–87. doi: 10.1080/17290376.2012.683581. [DOI] [PubMed] [Google Scholar]
- 3.Agbonyitor M. Home-based care for people living with HIV/AIDS in Plateau State, Nigeria: Findings from a qualitative study. Global Public Health: An International Journal for Research, Policy and Practice. 2009;4(3):303–312. doi: 10.1080/17441690902783165. [DOI] [PubMed] [Google Scholar]
- 4.Ahsan Ullah AK. HIV/AIDS-Related Stigma and Discrimination: A Study of Health Care Providers in Bangladesh. Journal of the International Association of Physicians in AIDS Care (Chicago, Ill : 2002) 2011;10(2):97–104. doi: 10.1177/1545109710381926. [DOI] [PubMed] [Google Scholar]
- 5.Alemu T, Biadgilign S, Deribe K, Escudero HR. Experience of stigma and discrimination and the implications for healthcare seeking behavior among people living with HIV/AIDS in resource-limited setting. SAHARA J: journal of Social Aspects of HIV/AIDS Research Alliance/SAHARA, Human Sciences Research Council. 2013;10(1):1–7. doi: 10.1080/17290376.2013.806645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alfonso V, Toulson A, Bermbach N, Erskine Y, Montaner J. Psychosocial issues influencing treatment adherence in patients on multidrug rescue therapy: perspectives from patients and their health care providers. AIDS Patient Care STDS. 2009;23(2):119–126. doi: 10.1089/apc.2008.0115. [DOI] [PubMed] [Google Scholar]
- 7.Arrivillaga M, Ross M, Useche B, Springer A, Correa D. Applying an expanded social determinant approach to the concept of adherence to treatment: The case of Colombian women living with HIV/AIDS. Womens Health Issues. 2011;21(2):177–183. doi: 10.1016/j.whi.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 8.Arrivillaga M, Springer AE, Lopera M, Correa D, Useche B, Ross MW. HIV/AIDS treatment adherence in economically better off women in Colombia. AIDS Care. 2012;24(7):929–935. doi: 10.1080/09540121.2011.647678. [DOI] [PubMed] [Google Scholar]
- 9.Audu B, Morgan R, Rutter P. Qualitative exploration of the relationship between HIV/AIDS patients’ experiences of clinical services and treatment adherence at Maitama District Hospital, Abuja, Nigeria. AIDS Care. 2013 doi: 10.1080/09540121.2013.819410. [DOI] [PubMed] [Google Scholar]
- 10.Auvinen J, Kylma J, Valimaki M, Bweupe M, Suominen T. Barriers and Resources to PMTCT of HIV: Luba-Kasai Men’s Perspective in Lusaka, Zambia. J Assoc Nurses AIDS Care. 2013 doi: 10.1016/j.jana.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 11.Bhagwanjee A, Petersen I, Akintola O, George G. Bridging the gap between VCT and HIV/AIDS treatment uptake: Perspectives from a mining-sector workplace in South Africa. African Journal of AIDS Research. 2008;7(3):271–279. doi: 10.2989/AJAR.2008.7.3.4.651. [DOI] [PubMed] [Google Scholar]
- 12.Balcha TT, Jeppsson A, Bekele A. Barriers to Antiretroviral Treatment in Ethiopia: A Qualitative Study. JIAPAC: Journal of the International Association of Physicians in AIDS Care. 2011;10(2):119–125. doi: 10.1177/1545109710387674. [DOI] [PubMed] [Google Scholar]
- 13.Benotsch EG, Seal DW, Stevenson LY, et al. Stigma, AIDS, and HIV prevention in Africa: reports from community organizations providing prevention services. J Hum Behav Soc Environ. 2008;18(3):329–349. [Google Scholar]
- 14.Beer L, Fagan JL, Valverde E, Bertolli J. Health-related beliefs and decisions about accessing HIV medical care among HIV-infected persons who are not receiving care. AIDS Patient Care STDS. 2009;23(9):785–792. doi: 10.1089/apc.2009.0032. [DOI] [PubMed] [Google Scholar]
- 15.Blake BJ, Jones Taylor GA, Reid P, Kosowski M. Experiences of women in obtaining human immunodeficiency virus testing and healthcare services. J Am Acad Nurse Pract. 2008;20(1):40–46. doi: 10.1111/j.1745-7599.2007.00283.x. [DOI] [PubMed] [Google Scholar]
- 16.Boehme AK, Moneyham L, McLeod J, et al. HIV-infected women’s relationships with their health care providers in the rural deep south: an exploratory study. Health Care Women Int. 2012;33(4):403–419. doi: 10.1080/07399332.2011.610533. [DOI] [PubMed] [Google Scholar]
- 17.Bogart LM, Chetty S, Giddy J, et al. Barriers to care among people living with HIV in South Africa: Contrasts between patient and healthcare provider perspectives. AIDS Care. 2013;25(7):843–853. doi: 10.1080/09540121.2012.729808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Campbell C, Scott K, Madanhire C, Nyamukapa C, Gregson S. A ‘good hospital’: nurse and patient perceptions of good clinical care for hiv-positive people on antiretroviral treatment in rural zimbabwe—a mixed-methods qualitative study. Int J Nurs Stud. 2011;48(2):175–183. doi: 10.1016/j.ijnurstu.2010.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chakrapani V, Newman PA, Shunmugam M, Dubrow R. Barriers to free antiretroviral treatment access among kothi-identified men who have sex with men and aravanis (transgender women) in Chennai, India. AIDS Care. 2011;23(12):1687–1694. doi: 10.1080/09540121.2011.582076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chakrapani V, Newman PA, Shunmugam M, Kurian AK, Dubrow R. Barriers to free antiretroviral treatment access for female sex workers in Chennai, India. AIDS Patient Care STDS. 2009;23(11):973–980. doi: 10.1089/apc.2009.0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chinkonde JR, Sundby J, Martinson F. The prevention of mother-to-child HIV transmission programme in Lilongwe, Malawi: why do so many women drop out. Reproductive health matters. 2009;17(33):143–151. doi: 10.1016/S0968-8080(09)33440-0. [DOI] [PubMed] [Google Scholar]
- 22.Chomat AMB, Wilson IB, Wanke CA, Selvakumar A, John KR, Isaac R. Knowledge, beliefs, and health care practices relating to treatment of HIV in Vellore, India. AIDS Patient Care STDS. 2009;23(6):477–484. doi: 10.1089/apc.2008.0222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Church K, Wringe A, Fakudze P, Kikuvi J, Simelane D, Mayhew SH. The relationship between service integration and client satisfaction: a mixed methods case study within HIV services in a high prevalence setting in Africa. AIDS Patient Care STDS. 2012;26(11):662–673. doi: 10.1089/apc.2012.0191. [DOI] [PubMed] [Google Scholar]
- 24.Chow MYK, Li M, Quine S. Client satisfaction and unmet needs assessment: Evaluation of an HIV ambulatory health care facility in Sydney, Australia. Asia Pac J Public Health. 2012;24(2):406–414. doi: 10.1177/1010539510384843. [DOI] [PubMed] [Google Scholar]
- 25.Dahab M, Kielmann K, Charalambous S, et al. Contrasting reasons for discontinuation of antiretroviral therapy in workplace and public-sector HIV programs in South Africa. AIDS Patient Care STDS. 2011;25(1):53–59. doi: 10.1089/apc.2010.0140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dang BN, Giordano TP, Kim JH. Sociocultural and structural barriers to care among undocumented Latino immigrants with HIV infection. Journal of immigrant and minority health/Center for Minority Public Health. 2012;14(1):124–131. doi: 10.1007/s10903-011-9542-x. [DOI] [PubMed] [Google Scholar]
- 27.Dutcher MV, Phicil SN, Goldenkranz SB, et al. “Positive Examples”: a bottom-up approach to identifying best practices in HIV care and treatment based on the experiences of peer educators. AIDS Patient Care STDS. 2011;25(7):403–411. doi: 10.1089/apc.2010.0388. [DOI] [PubMed] [Google Scholar]
- 28.Enriquez M, Farnan R, Neville S. What experienced HIV-infected lay peer educators working in Midwestern U.S. HIV medical care settings think about their role and contributions to patient care. AIDS Patient Care STDS. 2013;27(8):474–480. doi: 10.1089/apc.2013.0021. [DOI] [PubMed] [Google Scholar]
- 29.Fredriksen-Goldsen KI, Shiu CS, Starks H, et al. You must take the medications for you and for me”: family caregivers promoting HIV medication adherence in China. AIDS Patient Care STDS. 2011;25(12):735–741. doi: 10.1089/apc.2010.0261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Garland PM, Valverde EE, Fagan J, et al. HIV counseling, testing and referral experiences of persons diagnosed with HIV who have never entered HIV medical care. AIDS Educ Prev. 2011;23(3, Suppl):117–127. doi: 10.1521/aeap.2011.23.3_supp.117. [DOI] [PubMed] [Google Scholar]
- 31.Ho C, Twinn S, Cheng KKF. Quality of life constructs of Chinese people living with HIV/AIDS. Psychol Health Med. 2010;15(2):210–219. doi: 10.1080/13548501003623948. [DOI] [PubMed] [Google Scholar]
- 32.Hodgson I, Nakiyemba A, Seeley J, Bitira D, Gitau-Mburu D. Only connect—The role of PLHIV group networks in increasing the effectiveness of Ugandan HIV services. AIDS Care. 2012;24(11):1368–1374. doi: 10.1080/09540121.2012.656568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ibrahim K, Haroen H, Pinxten L. Home-based Care: A Need Assessment of People Living With HIV Infection in Bandung, Indonesia. JANAC: Journal of the Association of Nurses in AIDS Care. 2011;22(3):229–237. doi: 10.1016/j.jana.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 34.Johansen PS, Kohli H. Long-term HIV/AIDS survivors: Coping strategies and challenges. Journal of HIV/AIDS & Social Services. 2012;11(1):6–22. [Google Scholar]
- 35.Joseph HA, Fasula AM, Morgan RL, et al. ‘The Anticipation Alone could Kill You’: Past and Potential Clients’ Perspectives on HIV Testing in Non-Health Care Settings. AIDS Educ Prev. 2011;23(6):577–594. doi: 10.1521/aeap.2011.23.6.577. [DOI] [PubMed] [Google Scholar]
- 36.Kasenga F, Hurtig AK, Emmelin M. HIV-positive women’s experiences of a PMTCT programme in rural Malawi. Midwifery. 2010;26(1):27–37. doi: 10.1016/j.midw.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 37.Kempf M, McLeod J, Boehme AK, et al. A Qualitative Study of the Barriers and Facilitators to Retention-in-Care Among HIV-Positive Women in the Rural Southeastern United States: Implications for Targeted Interventions. AIDS Patient Care STDS. 2010;24(8):515–520. doi: 10.1089/apc.2010.0065. [DOI] [PubMed] [Google Scholar]
- 38.Lubega M, Nsabagasani X, Tumwesigye NM, et al. Policy and practice, lost in transition: Reasons for high drop-out from pre-antiretroviral care in a resource-poor setting of eastern Uganda. Health Policy. 2010;95(2–3):153–158. doi: 10.1016/j.healthpol.2009.11.021. [DOI] [PubMed] [Google Scholar]
- 39.McCoy SI, Miller WC, MacDonald PD, et al. Barriers and facilitators to HIV testing and linkage to primary care: narratives of people with advanced HIV in the Southeast. AIDS Care. 2009;21(10):1313–1320. doi: 10.1080/09540120902803174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moneyham L, McLeod J, Boehme A, et al. Perceived barriers to HIV care among HIV-infected women in the Deep South. J Assoc Nurses AIDS Care. 2010;21(6):467–477. doi: 10.1016/j.jana.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 41.Muhamadi L, Nsabagasani X, Tumwesigye MN, et al. Inadequate pre-antiretroviral care, stock-out of antiretroviral drugs and stigma: policy challenges/bottlenecks to the new WHO recommendations for earlier initiation of antiretroviral therapy (CD<350 cells/microL) in eastern Uganda. Health Policy. 2010;97(2–3):187–194. doi: 10.1016/j.healthpol.2010.06.003. [DOI] [PubMed] [Google Scholar]
- 42.Mutchler MG, Wagner G, Cowgill BO, McKay T, Risley B, Bogart LM. Improving HIV/AIDS care through treatment advocacy: Going beyond client education to empowerment by facilitating client-provider relationships. AIDS Care. 2011;23(1):79–90. doi: 10.1080/09540121.2010.496847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nakigozi G, Atuyambe L, Kamya M, et al. A Qualitative Study of Barriers to Enrollment into Free HIV Care: Perspectives of Never-in-Care HIV-Positive Patients and Providers in Rakai, Uganda. BioMed research international. 2013;2013:470245. doi: 10.1155/2013/470245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ndirangu EW, Evans C. Experiences of African immigrant women living with HIV in the U.K.: implications for health professionals. Journal of Immigrant & Minority Health. 2009;11(2):108–114. doi: 10.1007/s10903-008-9116-8. [DOI] [PubMed] [Google Scholar]
- 45.Njunga J, Blystad A. ‘The divorce program’: gendered experiences of HIV positive mothers enrolled in PMTCT programs - the case of rural Malawi. International breastfeeding journal. 2010;5:14. doi: 10.1186/1746-4358-5-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.O’Brien S, Broom A. Gender, culture and changing attitudes: Experiences of HIV in Zimbabwe. Culture, health & sexuality. 2013;15(5):583–597. doi: 10.1080/13691058.2013.776111. [DOI] [PubMed] [Google Scholar]
- 47.Odlum M, Gordon P, Camhi E, Schnall R, Teixeira P, Bakken S. Perceptions of predisposing, enabling, and reinforcing factors influencing the use of a continuity of care document in special needs PLWH. J Health Care Poor Underserved. 2012;23(4):1457–1476. doi: 10.1353/hpu.2012.0172. [DOI] [PubMed] [Google Scholar]
- 48.Orner P, Cooper D, Myer L, Zweigenthal V, Bekker L, Moodley J. Clients’ perspectives on HIV/AIDS care and treatment and reproductive health services in South Africa. AIDS Care. 2008;20(10):1217–1223. doi: 10.1080/09540120701867008. [DOI] [PubMed] [Google Scholar]
- 49.Peltzer K, Phaswana-Mafuya N, Ladzani R. Implementation of the national programme for prevention of mother-to-child transmission of HIV: A rapid assessment in Cacadu district, South Africa. African Journal of AIDS Research. 2010;9(1):95–106. doi: 10.2989/16085906.2010.484594. [DOI] [PubMed] [Google Scholar]
- 50.Phakathi Z, Van Rooyen H, Fritz K, Richter L. The influence of antiretroviral treatment on willingness to test: a qualitative study in rural KwaZulu-Natal, South Africa. African Journal of AIDS Research (AJAR) 2011;10(2):173–180. doi: 10.2989/16085906.2011.593381. [DOI] [PubMed] [Google Scholar]
- 51.Quinlivan EB, Messer LC, Adimora AA, et al. Experiences with HIV Testing, Entry, and Engagement in Care by HIV-Infected Women of Color, and the Need for Autonomy, Competency, and Relatedness. AIDS Patient Care STDS. 2013;27(7):408–415. doi: 10.1089/apc.2012.0434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rajabiun S, Coleman S, Drainoni M-L. Keeping at-risk persons living with HIV/AIDS in care: A qualitative study of staff perspectives. Journal of HIV/AIDS & Social Services. 2011;10(2):120–138. [Google Scholar]
- 53.Rivero-Mendez M, Dawson-Rose CS, Solis-Baez SS. A Qualitative Study of Providers’ Perception of Adherence of Women Living with HIV/AIDS in Puerto Rico. Qualitative report (Online) 2010;15(2):232–251. [PMC free article] [PubMed] [Google Scholar]
- 54.Schrader SM, Deering EN, Zahl DA, Wallace M. Visually storying living with HIV: Bridging stressors and supports in accessing care. Health Educ Res. 2011;26(4):638–652. doi: 10.1093/her/cyr023. [DOI] [PubMed] [Google Scholar]
- 55.Shedlin MG, Decena CU, Beltran O. Geopolitical and cultural factors affecting ARV adherence on the US-Mexico border. Journal of immigrant and minority health/Center for Minority Public Health. 2013;15(5):969–974. doi: 10.1007/s10903-012-9681-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shin S, Munoz M, Zeladita J, et al. How does directly observed therapy work? The mechanisms and impact of a comprehensive directly observed therapy intervention of highly active antiretroviral therapy in Peru. Health & social care in the community. 2011;19(3):261–271. doi: 10.1111/j.1365-2524.2010.00968.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Shuster JM, Sterk CE, Frew PM, del Rio C. The cultural and community-level acceptance of antiretroviral therapy (ART) among traditional healers in Eastern Cape, South Africa. J Community Health. 2009;34(1):16–22. doi: 10.1007/s10900-008-9121-9. [DOI] [PubMed] [Google Scholar]
- 58.Shroufi A, Mafara E, Saint-Sauveur JF, Taziwa F, Vinoles MC. Mother to Mother (M2M) peer support for women in Prevention of Mother to Child Transmission (PMTCT) programmes: a qualitative study. PLoS One. 2013;8(6):e64717. doi: 10.1371/journal.pone.0064717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sison N, Yolken A, Poceta J, et al. Healthcare provider attitudes, practices, and recommendations for enhancing routine HIV testing and linkage to care in the Mississippi Delta region. AIDS Patient Care STDS. 2013;27(9):511–517. doi: 10.1089/apc.2013.0169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Stevens PE, Keigher SM. Systemic barriers to health care access for U.S. women with HIV: the role of cost and insurance. Int J Health Serv. 2009;39(2):225–243. doi: 10.2190/HS.39.2.a. [DOI] [PubMed] [Google Scholar]
- 61.Theilgaard ZP, Katzenstein TL, Chiduo MG, et al. Addressing the fear and consequences of stigmatization - a necessary step towards making HAART accessible to women in Tanzania: a qualitative study. AIDS Res Ther. 2011;8:28. doi: 10.1186/1742-6405-8-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tripathi V, King EJ, Finnerty E, Koshovska-Kostenko N, Skipalska H. Routine HIV counseling and testing during antenatal care in Ukraine: A qualitative study of the experiences and perspectives of pregnant women and antenatal care providers. AIDS Care. 2013;25(6):680–685. doi: 10.1080/09540121.2012.749332. [DOI] [PubMed] [Google Scholar]
- 63.Xavier J, Bradford J, Hendricks M, et al. Transgender Health Care Access in Virginia: A Qualitative Study. International Journal of Transgenderism. 2012;14(1):3–17. [Google Scholar]
- 64.Yeap AD, Hamilton R, Charalambous S, et al. Factors influencing uptake of HIV care and treatment among children in South Africa - a qualitative study of caregivers and clinic staff. AIDS Care. 2010;22(9):1101–1107. doi: 10.1080/09540121003602218. [DOI] [PubMed] [Google Scholar]
- 65.Wang X, Zhang X, Xu Y, Zhang Y. Health service access for rural people living with HIV/AIDS in China: A critical evaluation. Journal of Sociology and Social Welfare. 2011;38(4):77–100. [Google Scholar]
- 66.Ware NC, Wyatt MA, Geng EH, et al. Toward an Understanding of Disengagement from HIV Treatment and Care in Sub-Saharan Africa: A Qualitative Study. PLoS Med. 2013;10(1):e1001369–e1001369. doi: 10.1371/journal.pmed.1001369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wei C, Yan H, Yang C, et al. Accessing HIV testing and treatment among men who have sex with men in China: A qualitative study. AIDS Care. 2013 doi: 10.1080/09540121.2013.824538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Williams B, Amico KR, Konkle-Parker D. Qualitative assessment of barriers and facilitators to HIV treatment. JANAC: Journal of the Association of Nurses in AIDS Care. 2011;22(4):307–312. doi: 10.1016/j.jana.2010.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Winestone LE, Bukusi EA, Cohen CR, Kwaro D, Schmidt NC, Turan JM. Acceptability and feasibility of integration of HIV care services into antenatal clinics in rural Kenya: A qualitative provider interview study. Global public health. 2012;7(2):149–163. doi: 10.1080/17441692.2011.621964. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.