Abstract
Purpose
An understanding of the pharmacokinetic (PK) and pharmacodynamic (PD) principles that determine response to antimicrobial therapy can provide the clinician with better-informed dosing regimens. Factors influential on antibiotic disposition and clinical outcome are presented, with a focus on the primary site of infection. Techniques to better understand antibiotic PK and optimize PD are acknowledged.
Methods
PubMed (inception – April 2016) was reviewed for relevant publications assessing antimicrobial exposures within different anatomical locations and clinical outcomes for various infection sites.
Findings
A limited literature base indicates variable penetration of antibiotics to different target sites of infection, with drug solubility and extent of protein binding providing significant PK influences in addition to the major clearing pathway of the agent. PD indices derived from in vitro and animal models determine the optimal magnitude and frequency of dosing regimens for patients. PK/PD modeling and simulation has been shown an efficient means of assessing these PD endpoints against a variety of PK determinants, clarifying the unique effects of infection site and patient characteristics to inform the adequacy of a given antibiotic regimen.
Implications
Appreciation of the PK properties of an antibiotic and its PD measure of efficacy can maximize the utility of these life-saving drugs. Unfortunately, clinical data remains limited for a number of infection site-antibiotic exposure relationships. Modeling and simulation can bridge preclinical and patient data for the prescription of optimal antibiotic dosing regimens, consistent with the tenets of personalized medicine.
Keywords: Antibiotic, Dosing, Exposure, Pharmacokinetics, Pharmacodynamics
Introduction
Antibiotics are a key component of modern medicine, utilized in over half of all US hospitalizations, with over 250 million additional treatment courses provided in the outpatient setting per year.1,2 Along with other classes of anti-infectives, they represent a uniqueness in pharmacotherapy, where one patient’s prescription can have a direct effect on others’, as antimicrobial utilization remains the primary driver of organism resistance.3,4 Despite antibiotic resistance having long been declared a major threat to global public health,3,5,6 the landscape of antimicrobial development has remained arid, with no agents with novel mechanisms of action against resistant Gram-negative organisms currently in late-stage clinical trials.7-9 It is abundantly clear that optimization of antibiotic prescribing is necessary to preserve our current armamentarium. While stewardship practices focusing on the restriction of use and shortening of treatment duration are well-cited,10,11 further research on antibiotic pharmacokinetic (PK) and pharmacodynamic (PD) properties that maximize the probability of successful outcome is needed.
This review serves to provide the clinician with the principal PK/PD considerations for the most common antibiotics encountered in US hospital settings (beta-lactams, vancomycin, fluoroquinolones, and aminoglycosides). The information contained herein can assist in producing dosing regimens that maximize clinical benefit while minimizing the risk of toxicity. While these concepts remain salient to antifungals and antivirals, such agents are beyond the scope of this review. Particular emphasis will be placed on the site of infection when applying these concepts to patient care. This review is by no means exhaustive, and the interested reader is encouraged to access the provided references and available textbooks12,13 for a more in-depth discussion of antimicrobial PK/PD. Instead, the goal is to discuss the key principles related to rational selection of an antibiotic dosing regimen, which remain applicable to agents not discussed here in addition to new agents as they enter clinical practice.
Methods
PubMed (inception – April 2016) was searched for relevant publications using combinations of the search terms “antibiotic”, “penicillin”, “cephalosporin”, “carbapenem”, “vancomycin”, “fluoroquinolone”, “aminoglycoside”, “penetration”, “blood”, “bloodstream”, lung”, “epithelial lining fluid”, “soft tissue”, “interstitial fluid”, “bone”, “central nervous system”, “cerebrospinal fluid”, “pharmacodynamic”, and “outcome”. Reference lists of identified publications were also reviewed for relevant articles.
Antimicrobial Pharmacokinetics
General Considerations
The kinetics of a drug refer to its rate of change as it traverses through a biological system, and is governed by the four essential processes of absorption, distribution, metabolism, and excretion. While antibiotic PK is often considered in terms of the body’s effect on the drug, the agent’s physicochemical properties must also be considered to predict its disposition. Chief among them is the relative solubility of the antimicrobial, which can have a significant impact on its volume of distribution, and thus may prove key in selecting agents expected to attain adequate penetration to the site of infection.14,15 Also influential is the extent of protein binding the antibiotic exhibits, as only free, unbound drug is capable of exerting antimicrobial effects.16-19 As albumin is the primary plasma binding protein for the majority of antibiotics, its concentrations should be considered when implementing and adjusting dosing regimens, with highly protein bound agents being most affected.14,20-22 Finally, the agent’s major route of elimination warrants appreciation, particularly in times of changing clinical condition where development of end-organ dysfunction or critical illness can greatly enhance (renal failure)23,24 or reduce (augmented renal clearance) antibiotic exposures.25-27 Table 1 summarizes these properties for the most commonly utilized parenteral antibiotics in the US hospital setting.
Table 1. Representative PK Properties of Commonly Administered Antibiotics.
| Antibiotic | Solubility | Plasma Protein Binding | Clearance |
|---|---|---|---|
| Beta-lactamsa | Hydrophilic | Low-moderate | Renal |
| Vancomycin | Hydrophilic | Moderate | Renal |
| Fluoroquinolonesb | Lipophilic | Low-moderate | Renal |
| Aminoglycosides | Hydrophilic | Low | Renal |
Exceptions: cefazolin (highly protein bound), ceftriaxone (highly protein bound), ertapenem (highly protein bound), nafcillin/oxacillin (highly protein bound, hepatically cleared)
Exception: moxifloxacin (hepatically cleared)
Site-Specific Considerations
With these PK properties in mind, it becomes clear that the primary infection site is a crucial variable in considering whether sufficient antibiotic exposures are likely to be attained for a given agent and dosing regimen. Indeed, the differing physiology of anatomical sites where bacteria can reside often result in variable degrees of antibiotic penetration and thus concentration at the site where pharmacologic effect occurs.14 The sections that follow examine the relationship between antibiotic PK and exposures in the blood, lung, soft tissue, bone, and central nervous system (CNS); a summative table outlining hypothetical dose alterations based on antimicrobial PK properties and infection site is provided in Table 2.
Table 2. Infection Site, PK Considerations, and Adaptation of Dosing Regimen.
| Infection Site | PK Alteration | Potential Change to Dosing Regimen |
|---|---|---|
| Blood | Expanded Vd, Enhanced CL | Provision of LD, Increase frequency |
| Lung | Impaired permeabilitya | Increase dosea |
| Soft Tissue | Contingent on body composition | Increase dose in obesity |
| Bone | Impaired permeability | Increase dose, duration of therapy |
| CNS | Impaired permeability | Maximal dose |
CL = clearance; LD = loading dose; Vd = volume of distribution
Of hydrophilic agents (beta-lactams, vancomycin, aminoglycosides)
Blood
The bloodstream is perhaps the simplest infection site to consider, as it comprises the central compartment from which systemically administered drug distributes to the tissues. When treating a bacteremic patient, the clinician must account for the likelihood of the proposed antibiotic agent – and more importantly its proposed dosing regimen – to maintain sufficient exposures within the blood to rapidly clear the organism, as delays in appropriate therapy are associated with increased mortality.28-31 Of course, the factors described here must also be reconciled with identification of the primary source of infection, optimizing antimicrobial therapy for that site in parallel with blood to prevent recrudescence and the possibility of antibiotic resistance.
In addition to the underlying pathology of sepsis resulting in significant fluid extravasation and a high probability of augmented renal clearance,32,33 standard therapy bundles that include volume resuscitation and inotrope support are likely to further alter antibiotic PK, with hydrophilic, renally-cleared agents (beta-lactams, vancomycin, aminoglycosides) being most susceptible.34-37 Indeed, recent data has suggested that currently prescribed doses of beta-lactams are prone to underexposure in the critically ill, yielding a lower probability of achieving positive clinical outcomes.38-41 Similar findings of suboptimal exposure for vancomycin26,36 and aminoglycosides42,43 have been observed, correlating with illness severity.44 In contrast, the lipophilic fluoroquinolones are minimally affected by changes in volume status, owing to their considerable permeability across membranes.34,45 While it could be inferred that the presence of augmented renal clearance would result in lower exposures of ciprofloxacin and levofloxacin, the evidence supporting this theory is, to date, lacking.
The presence of endocarditis necessitates the additional consideration of antibiotic penetration within the vegetation, as a high bacterial inoculum and production of biofilm can result in suboptimal concentrations and treatment failures.46,47 Work performed in vitro and in animals has demonstrated the general need for higher doses to attain sufficient exposures,48,49 though clinical evidence remains scarce for the agents under consideration here. Nevertheless, current clinical practice guidelines advocate the use of dosing regimens at the high end of the licensed dosing range (beta-lactams) or measured therapeutic range (vancomycin) to optimize treatment outcomes.46,50
Lung
The lung represents an additional infection site associated with high bacterial densities and variable antimicrobial penetration.14 The epithelial lining fluid (ELF) is considered the target site for the treatment of pneumonia caused by extracellular pathogens, representing an available matrix for the measurement of antibiotic concentrations.51,52 While sparse, literature does exist describing ELF penetration of various antimicrobials in the clinical setting; the data provided below is focused on infected patients wherever possible.
Beta-lactams display a wide variability in ELF-to-plasma penetration ratio, ranging from 0.21 for ceftazidime53 to 1.04 for cefepime.54 Piperacillin represents perhaps the most studied agent, with a reported ELF:plasma ratio of ~0.50 (with corresponding tazobactam values ranging from 0.65 to 1.21).55-57 A single report on ampicillin lung penetration found an ELF:plasma ratio of 0.53 (corresponding sulbactam value, 0.61).58 Preliminary data in healthy volunteers suggests an ELF:plasma ratio of 0.23 for ceftaroline,59 whereas a Phase I trial of ceftolozane produced a value of 0.48 (corresponding tazobactam value, 0.44).60 In the ceftolozane study of healthy volunteers, it is important to note the considerably lower degree of tazobactam penetration versus that observed in critically ill patients,55-57 which could be ascribed to an increase in paracellular permeability that accompanies inflammation;14 indeed, this study reported a demonstrably lower value for piperacillin as well (0.26). Counterintuitively, the opposite is found when considering meropenem, with lower ELF:plasma ratios reported for severely ill patients (~0.25)61,62 versus healthy volunteers (0.65),63 further indicating a critical need for antibiotic penetration studies in the target population. A singular study for ertapenem64 in critically ill patients suggests an ELF:plasma ratio of 0.30, whereas studies of doripenem65 and imipenem66 in healthy individuals report values of ~0.34, and 0.44, respectively. These findings indicate a relatively lower extent of ELF penetration for carbapenems versus penicillins in infected patients, whereas penetration ratios for cephalosporins remain highly variable. This, along with an inability to correlate penetration to extent of protein binding, emphasizes the need for careful consideration of agent and regimen selection when treating patients for pneumonia.67,68 Unfortunately, data is lacking for other commonly used beta-lactams such as cefazolin, ceftriaxone, and oxacillin/nafcillin.
Despite its high degree of utilization, the permeability of vancomycin into ELF has been severely understudied, with only a few reports to guide therapeutic decision.69-71 From this limited literature base, best estimates for ELF:plasma penetration range from ~0.18-0.50, with most authors recommending higher doses to achieve sufficient lung exposures. In stark contrast, lung penetration of ciprofloxacin, levofloxacin, and moxifloxacin has been extensively studied, with the high volume of distribution of fluoroquinolones producing ELF:plasma ratios exceeding 1.72-78 For aminoglycosides, lung disposition appears more complex, with gentamicin and tobramycin ELF:plasma ratios <1 early in the dosing interval, but >1 after 6-8 hours: this apparent PK hysteresis could be explained by the considerable hydrophilicity of these compounds, resulting in slow rates of movement across biological membranes.79-81 It must be cautioned, however, that in none of these studies were exposures examined over an entire dosing interval, thus the possibility of redistribution from ELF to plasma remains a significant and unresolved issue.
Soft tissue
Much like ELF for the lung, the interstitial fluid (ISF) concentration of an antibiotic provides the most appropriate measurement of target site exposure for extracellular infections of the soft tissue.82 Utilizing microdialysis techniques, which consist of implanting a perfused semipermeable membrane into the desired tissue and measuring drug concentrations within the dialysate, the most robust quantification of unbound (free) antibiotic in ISF can be achieved.83,84 The physicochemical properties of the antibiotic and its degree of protein binding largely dictate the extent of soft tissue penetration, as the vascular endothelium remains highly permeable to these small molecules.85 Importantly, then, the clinician must remain cognizant of the infected patient’s relative proportions of adipose and muscle, as lower exposures of some hydrophilic agents in the ISF of adipose relative to muscle tissue have been observed.35,86-88 Further, the expected increased volume of distribution of lipophilic agents with increased adipose may result in suboptimal concentrations to treat these infections. While the appreciable influence of obesity is beyond the scope of this review, general measures of body composition (fat free mass, percentage of ideal body weight) may be considered additional factors when determining suitable antibiotic dosing regimens for soft tissue infections.89,90
Bone
The composition of bone is unique, consisting of a matrix of collagen and hydroxyapatite that often provides a protected site for bacteria, evading the effects of the immune system and many antibiotics.14 With osteomyelitis being associated with a high relapse rate and protracted antibiotic courses, emphasis should be placed on optimization of dosing regimens and a better understanding of PK properties that can influence exposure at the target site.91,92 While again the literature is sparse, some overarching patterns can be discerned, albeit the majority of data has been derived from non-infected patients.92,93
As may be expected based on discussions of previous infection sites, beta-lactams display variable penetration into bone, with ratios compared to serum ranging from ~0.1 for oxacillin to ~1 for cefepime.94,95 Most beta-lactams, however, manifest bone:serum ratios between 0.1 and 0.3, consistent with their hydrophilic nature.96-102 Similar variability and point estimates have been found for vancomycin in infected patients, with an average bone:serum ratio of ~0.20.100,103 Higher doses would thus be necessary if mirroring drug exposures in the blood is desired. Fluoroquinolones, maintaining high volumes of distribution secondary to their lipophilicity, achieve higher bone:serum ratios than beta-lactams or vancomycin, ranging from ~0.35 (ciprofloxacin) to ~0.75 for levofloxacin.104-106 Though studies are lacking for aminoglycosides, their high degree of hydrophilicity would be hypothesized to severely limit the penetration of these agents across the bone matrix.
CNS
The combination of tight junctions and active transport systems that form the blood-brain barrier (BBB) create a substantial impendent to the penetration of most antibiotics into the cerebrospinal fluid (CSF).107-109 As such, here perhaps more than any other infection site are the agents’ PK properties determinant of attaining sufficient pharmacologic exposures. Also of critical impact is the presence of inflammation within the meninges, as this significantly alters the permeability of the BBB, profoundly increasing CSF exposures for the majority of antibiotics.107,108,110
Degree of lipophilicity appears the most influential characteristic associated with an antibiotic’s CSF penetration, as this property affords passive diffusion across the otherwise impervious cerebral membranes.111-113 Indeed, fluoroquinolones achieve far higher CSF:plasma ratios than other antimicrobial classes, with values averaging ~0.50,114-116 versus ~0.10 for beta-lactams (range, 0.007 – 0.25),117-123 ~0.15 for vancomycin,124 and ~0.20 for aminoglycosides108 in intact meninges. With inflammation, however, the tight junctions that connect cerebral endothelial cells become more porous, allowing up to an order of magnitude higher CSF penetration for hydrophilic compounds.108,124-128 This knowledge must be reconciled clinically with the frequent use of corticosteroids to decrease meningeal inflammation, which in addition to blunting the immune system’s response to infection can decrease the CSF exposure of first-line agents, thus larger doses are likely necessary to ensure antimicrobial success, consistent with guideline recommendations.128,129 As would be expected, the effect of inflammation on CSF penetration is attenuated with fluoroquinolones, though enhancements have been reported in a limited number of patients.130,131
Collectively, these findings make it clear that target site penetration is an important factor for reconciling PK differences between and within antibiotic classes, and interpreting published literature on antimicrobial effect. It is also apparent that the study of antibiotic exposures at the site of infection is deficient, with much of the evidence base from trials conducted decades ago, hindered by suboptimal experimental designs, limited numbers of observations, and outdated methodologies. Importantly, while published studies often observe infection site concentrations above the minimum inhibitory concentrations (MICs) of common pathogens despite various barriers to entry, as will be presented in the following section, these PK snapshots are ill-suited for drawing definitive conclusions on the adequacy of a given antibiotic regimen.
Antimicrobial Pharmacodynamics
Guiding Principles
The MIC represents the most elemental PD measure for antibiotics; however, this value simply reflects the potency of the given agent, providing no information regarding the time course of antimicrobial effect nor whether the rate of bacterial killing may be altered by changing drug exposure.132 Far more informative is the incorporation of PK information to assess the ability of a given antibiotic and its chosen dosing regimen to kill the infecting pathogen and predict clinical outcome. Three major PD indices – the percent of time that free drug remains above the MIC over a 24-hour period (fT>MIC), the ratio of free drug area under the concentration-time curve to MIC over a 24-hour period (fAUC:MIC), and the ratio of maximum concentration to MIC (Cmax:MIC) – sufficiently link the kinetics of antimicrobial disposition to efficacy.132-134 An additional factor is the agent’s post-antibiotic effect (PAE), which quantifies the persistence of bacterial suppression after short exposure to the drug, thus adding to the overall duration of antimicrobial effect.135 Consideration of these metrics is essential in appropriately selecting and adjusting antibiotic regimens in clinical practice, and should be done in concordance with individual patient status and suspected site of infection. Representative PD and dosing characteristics for the antimicrobial classes discussed previously are provided in Table 3; while the field of antimicrobial PD was borne from in vitro and animal study, for which a rich literature exists,132,134,136,137 the focus here will be on recent clinical applications and appraisals. Thus, alternative PD measures associated with the minimization of antimicrobial resistance such as the mutant prevention concentration (MPC) will not be discussed, as they at current have not been assessed in the clinic, though remain an important focus for future research.138,139 Further, owing to less overall evidence supporting their use, alternative PD indices including measures related to percent of time free drug remains above a low multiple of the MIC (e.g. fT>4 × MIC),140 and minimum free drug concentration to MIC ratio (fCmin:MIC)141 are beyond the scope of this review.
Table 3. PD and Dosing Characteristics of Commonly Administered Antibiotics.
| Antibiotic | PD Index | PAEa | Dosing Paradigm |
|---|---|---|---|
| Beta-lactams | fT>MIC | Minimalb | Higher frequency; prolonged infusions |
| Vancomycin | fAUC:MIC | -- | Flexible |
| Fluoroquinolones | fAUC:MIC, Cmax:MIC | Prolonged | Flexible; high dose |
| Aminoglycosides | Cmax:MIC, fAUC:MIC | Prolonged | High dose, low frequencyc |
PAE = post-antibiotic effect; fT>MIC = percent of time free drug remains above the minimum inhibitory concentration; fAUC:MIC = ratio of free drug area under the concentration-time curve to minimum inhibitory concentration; Cmax:MIC = ratio of maximum concentration to minimum inhibitory concentration
For Gram-negative pathogens only
Exception: carbapenems (Prolonged)
Exception: enterococcal endocarditis (lower dose, higher frequency)
fT>MIC
Beta-lactams serve as the archetypal class of time-dependent antibiotics, whereby substantially increasing drug concentrations have minimal effects on the overall rate and extent of bacterial killing. Instead, maintaining a free drug concentration above the MIC of the organism for a portion of the dosing interval has been shown to best predict microbiologic efficacy.142-145 The magnitude of this PD index varies by beta-lactam subclass, with typical fT>MIC values of ≥60-70% for cephalosporins, ≥50% for penicillins, and ≥40% for carbapenems providing maximal bactericidal effect.132,133
Clinically, these PD targets have been evaluated in a surprisingly limited number of studies, with the majority focusing on antipseudomonals.41,146-152 For these agents, a broad range of fT>MIC values from >45-100% have been reported as necessary for achievement of favorable clinical or microbiological outcomes, a likely consequence of heterogeneous patient populations, infecting organisms, and study designs. However, the most robust evidence remains in line with in vitro and animal estimates, with cefepime fT>MIC values of >53-74% being associated with up to a 10-fold higher likelihood of favorable outcome.149,151,152 Indeed, in a large study assessing the adequacy of contemporary beta-lactam dosing regimens in critically ill patients, the inability to attain a fT>MIC >50% was associated with a 32% decreased likelihood of a positive clinical outcome.41 Extended infusion regimens of certain beta-lactams have become a widespread means of maximizing fT>MIC in specific clinical scenarios.153,154 While likely not warranted in all patients, studies have shown average reductions in mortality of 33-50% when piperacillin/tazobactam and cefepime are dosed over 3-4 hours versus standard intermittent infusions (0.5-1 hour), with the largest benefits seen in critically ill patients and those with multidrug-resistant organisms.155,156 Extending this concept further, continuous infusions of beta-lactams have also been studied,155-157 though employment is likely to be reserved only for extreme cases secondary to logistical issues in maintaining dedicated intravascular access for administration. Despite the recent advances in our ability to derive optimized dosing regimens for beta-lactam agents, studies linking PD target attainment and clinical outcomes are limited, an issue that must be reconciled to ensure patients receive the best antimicrobial therapy based on infecting organism, infection site, and clinical status.
fAUC:MIC
Measures of free drug exposure over a 24-hour period (fAUC) in relation to the organism MIC are correlative with the antimicrobial efficacy for most antibiotic classes, with vancomycin and the fluoroquinolones having accrued the most data.132-134 Importantly, this metric affords a fair amount of flexibility in dosing regimen, as simultaneously adjusting both the magnitude of the dose and the frequency with which it is administered will result in identical fAUC values. Consequently, this PD index incorporates components of both time (vancomycin) and concentration (fluoroquinolones) dependence in determining the rate and extent of bacterial killing.133,134 Despite initial preclinical data showing maximal bacterial killing over a wide range of total drug AUC:MIC values for vancomycin, the threshold of ≥400 is ubiquitously used.158 Early animal and in vitro work indicate total drug AUC:MIC values of ≥30-100 are necessary to achieve maximum kill for fluoroquinolones, based on the infecting organism.132,159 Correcting for protein binding of these respective agents produces equivalent fAUC:MIC values of ≥200 for vancomycin and ≥21-70 for fluoroquinolones.
Secondary to the dramatic rise of methicillin-resistant Staphylococcus aureus (MRSA) over the past two decades, optimization of vancomycin therapy has received much attention in recent years. Though current practice guidelines recommend the measurement of trough concentrations as a surrogate of total drug AUC:MIC, this may yield overexposure in some patients and thus an increased risk of adverse effects.50,160,161 Evaluation of total drug AUC:MIC thresholds predictive of favorable outcomes have been conducted in various clinical settings, with results ranging from 211 in patients with complicated MRSA bacteremia and endocarditis to 578 in patients with septic shock due to MRSA; assuming 50% protein binding for vancomycin, equivalent fAUC:MIC values are ~106-289.162-167 In studies that assessed mortality, 2 to 4-fold reductions were observed with attainment of these AUC:MIC thresholds,163,164,166 emphasizing the need for careful selection of dosing regimens. Notably, recent data suggests that higher total drug AUC:MIC values within the first 48 hours of therapy may be most associated with clinical outcome, with thresholds upwards of 600 (fAUC:MIC ~300) being necessary.168,169 Unfortunately, achievement of such high vancomycin exposures is likely limited to the most sensitive of isolates, as large dosing requirements produce high likelihoods of toxicity.170,171
In some of the first studies to assess PD indices and clinical outcomes, fluoroquinolone AUC:MIC values of ≥125 for ciprofloxacin and ≥34 for levofloxacin were significantly associated with clinical and microbiologic cure.172,173 Assuming ~30% protein binding for each, this corresponds to fAUC:MIC values of ≥88 and ≥24, respectively, in line with preclinical estimates. Interestingly, later investigations174,175 reported the necessity of higher values to attain similar outcomes, which may be a consequence of infecting pathogen and severity of infection. In these studies, AUC:MIC values of ≥250 for ciprofloxacin and ≥87 for levofloxacin were predictive of favorable outcome, corresponding to fAUC:MIC values of ≥175 and ≥61, respectively. Overall, the evidence shows a 2-28-fold higher probability of favorable outcome when these respective PD index values were reached.174,175
Cmax:MIC
Aminoglycosides serve as the exemplar antimicrobial class for which bacterial kill is maximized by attaining higher maximal concentrations.132 Here, maintaining concentrations above the organism MIC for an extended period of the dosing interval is unnecessary, and in fact discouraged due to an increased risk of adverse effects.176-178 While preclinical studies originally established AUC:MIC as the most predictive PD index for aminoglycosides,136 it must be recognized that employment of once-daily doses will yield a high degree of collinearity between measures of Cmax and 24-hour AUC.178 As such, the focus here will be on Cmax:MIC, which remains the clinically targeted metric, and for which clinical outcomes data exist. Additionally, there have been trials with fluoroquinolones that discern the influence of peak concentrations in their overall killing capacity.
Studies of gentamicin and tobramycin in patients being treated for sepsis and nosocomial pneumonia have established a Cmax:MIC ≥8-10 as the PD target associated with clinical response.179-181 For endocarditis caused by Enterococcus species, current guidelines indicate aminoglycosides are to be given as lower, multiple daily doses instead of the typical once-daily regimen, albeit the evidence to support such dosing is scant.46 Nevertheless, it may be anticipated that a measure of total drug exposure (i.e. AUC:MIC) rather than Cmax:MIC would be a distinct correlate to efficacy for these patients, though such studies have yet to be conducted. While their PD index is often represented by fAUC:MIC, the concentration-dependent nature of bacterial killing by fluoroquinolones also results in Cmax:MIC as a predictive parameter for response.182,183 Values ≥8 for ciprofloxacin and ≥12.2 for levofloxacin were associated with significantly improved clinical and microbiologic outcomes, though as noted in the respective studies and supported by in vitro data, this index is likely most important when faced with an organism capable of rapidly developing resistance, such as Pseudomonas aeruginosa.184,185
PAE
When considering antimicrobial dosing regimens, the selected agent’s PAE, in determining the overall duration of action, can have a significant influence. In general, all antibiotics exhibit some degree of PAE against susceptible Gram-positive organisms, with values ranging from <2 hours for beta-lactams to nearly 5 hours for vancomycin against S. aureus, though point estimates vary considerably.135,186 Agents that alter protein or nucleic acid synthesis, such as aminoglycosides and fluoroquinolones, tend to display a prolonged PAE against any susceptible organism, as it takes considerably longer for bacteria to regenerate these elements than components of the cell wall.132,134 PAE values derived from animal models for these agents are on average between 2 and 6 hours (range, 1.2-12.8 hours for aminoglycosides; 1.9-7.5 hours for fluoroquinolones), thus longer intervals between doses are possible without compromising treatment efficacy.135,187,188 On the contrary, beta-lactams maintain virtually no PAE against Gram-negative pathogens (<1 hour), often requiring multiple daily doses to ensure adequate coverage.135 An exception here is the carbapenem subclass, whose agents have shown prolonged PAEs of ~2-4 hours against Enterobacteriaceae and P. aeruginosa, consistent with their lower fT>MIC requirement versus other beta-lactams.189-191
Modeling and Simulation
The relative paucity of clinical evidence confirming in vitro and animal model PK/PD observations speaks to the difficulty in conducting such trials, necessitating an integrative, efficient, and scientifically valid approach. In silico modeling of PK data and simulation of treatment course provides a powerful means of assessing the adequacy of current antimicrobial dosing regimens, and deriving those that optimize PD indices.192 These techniques are being increasingly employed both as a means of bringing new agents to market and for the evaluation of existing antimicrobials, minimizing industry risk on the one hand while maximizing clinical utility on the other.68,193,194 Through the leveraging of PK/PD data from preclinical models of infection and application of advanced pharmacostatistical modeling, measures of exposure and response can be obtained for various pathogen-antibiotic-infection site combinations. Imputing patient-level data into these models and performing Monte Carlo simulations, which account for interindividual differences in PK parameters and antimicrobial susceptibility, predictions of PD target attainment are possible. This has been shown for numerous agents, with optimal dosing regimens often inferred as those that eclipse the specified PD target (for example, a fT>MIC ≥50% or a fAUC/MIC ≥100) with a 90% or higher probability.195-204 Indeed, much of the aforementioned literature on antimicrobial penetration and efficacy has applied population PK modeling and Monte Carlo simulation to predict exposure-response relationships in patients and infer optimal dosing regimens for the clinical population under study. Extrapolation of the simulation results beyond this should be done with caution, as differing pathogens, infection types, and illness severities are likely to yield differing rates of target attainment for a given drug and dosing regimen; ideally, studies for each combination of antimicrobial agent, infecting pathogen, and clinical scenario should be performed. Additionally, such platforms can be utilized to study the effects of antibiotic resistance205,206 and rare infections,207,208 situations where accruing an adequate number of patients in clinical trials is not feasible. Modeling and simulation can thus enhance the translation of preclinical in vitro and animal studies to clinical practice, informing trial design to optimize the results of future clinical studies in addition to being directly applicable to contemporary patient care.
Summary and Conclusions
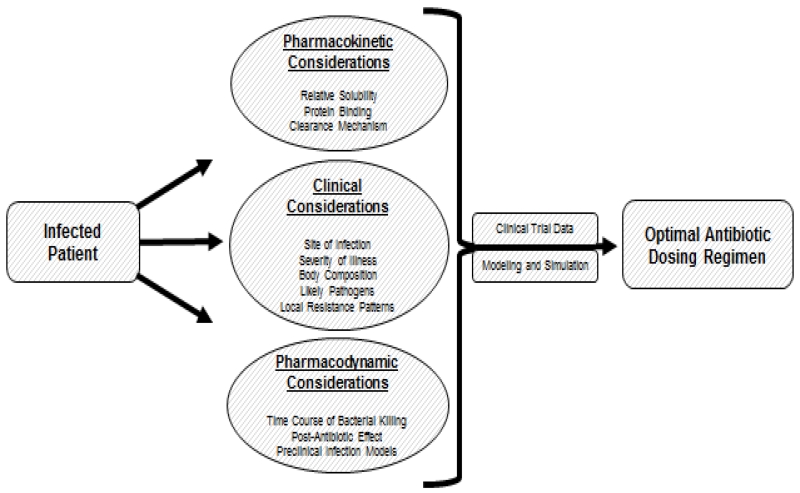
Rising rates of antimicrobial resistance and a limited drug development pipeline underscore the need for preserving the utility of currently available agents. An appreciation of the PK/PD determinants of a given antibiotic can foster more rational and individualized dosing regimens, improving patient outcomes while simultaneously limiting the spread of resistance (Figure 1). Anticipating the extent of distribution to the site of infection is of primary importance for ensuring adequate drug exposures; however, significant knowledge gaps remain. To truly understand the pharmacology of antimicrobials, we must go beyond MICs, employing metrics that account for the rate of bacterial killing, and the effects different dosing regimens have on it. Use of PK/PD modeling and simulation can maximize the amount of clinically useful information derived from limited numbers of patients, guiding optimal therapy and fully aligning with the goals of personalized medicine.
Figure 1.
Approach to the Infected Patient for the Provision of Optimal Antibiotic Therapy.
Acknowledgments
Dr. Gonzalez receives research support through K23HD083465 from the National Institute of Child Health and Human Development (NICHD), and from the nonprofit organization Thrasher Research Fund (www.thrasherresearch.org). Dr. Onufrak performed all literature retrieval and review, and wrote the manuscript. Drs. Forrest and Gonzalez reviewed the manuscript for accuracy and completeness.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement
Dr. Gonzalez receives research support from industry (Cempra, Inc, subaward to HHSO100201300009C) for pediatric drug development. Drs. Onufrak and Forrest have no conflicts to disclose. Further, these sponsors had no role in any facet of this manuscript’s creation or revision.
References
- 1.Fridkin S, Baggs J, Fagan R, et al. Vital Signs: Improving Antibiotic Use Among Hospitalized Patients. MMWR Morb Mortal Wkly Rep. 2014;63(9):194–200. [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention [Accessed March 12, 2016];Outpatient antibiotic prescriptions — United States. 2013 http://www.cdc.gov/getsmart/community/pdfs/annual-reportsummary_2013.pdf.
- 3.Centers for Disease Control and Prevention [Accessed March 12, 2016];Antibiotic resistance threats in the United States. 2013 http://www.cdc.gov/drugresistance/threat-report-2013/pdf/ar-threats-2013-508.pdf.
- 4.Center for Disease Dynamics, Economics & Policy . State of the World’s Antibiotics. CDDEP; Washington, D.C.: [Accessed March 12, 2016]. 2015. 2015. https://cddep.org/sites/default/files/swa_2015_final.pdf. [Google Scholar]
- 5.World Health Organization [Accessed March 12, 2016];Antimicrobial Resistance: Global Report on Surveillance. 2014 http://apps.who.int/iris/bitstream/10665/112642/1/9789241564748_eng.pdf.
- 6.The White House Administration [Accessed March 12, 2016];National Action Plan for Combating Antibiotic-Resistant Bacteria. 2015 https://www.whitehouse.gov/sites/default/files/docs/national_action_plan_for_combating_antibotic-resistant_bacteria.pdf.
- 7.Pew Charitable Trusts [Accessed March 12, 2016];Antibiotics Currently in Clinical Development. http://www.pewtrusts.org/en/multimedia/data-visualizations/2014/antibiotics-currently-in-clinical-development.
- 8.Boucher HW, Talbot GH, Benjamin DK, et al. 10 × ’20 Progress--development of new drugs active against gram-negative bacilli: an update from the Infectious Diseases Society of America. Clin Infect Dis. 2013;56(12):1685–1694. doi: 10.1093/cid/cit152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Drusano GL, Louie A, MacGowan A, Hope W. Suppression of emergence of resistance in pathogenic bacteria: keeping our powder dry-part 1. Antimicrob Agents Chemother. 2016;60(3):1183–93. doi: 10.1128/AAC.02177-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dellit TH, Owens RC, McGowan JE, Jr., et al. Infectious Diseases Society of America and Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis. 2007;44:159–177. doi: 10.1086/510393. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention [Accessed March 12, 2016];Core Elements of Hospital Antibiotic Stewardship Programs. http://www.cdc.gov/getsmart/healthcare/\rimplementation/core-elements.html.
- 12.Vinks A, Derendorf H, Mouton J, editors. Fundamentals of Antimicrobial Pharmacokinetics and Pharmacodynamics. Springer; New York: 2014. [Google Scholar]
- 13.Nightingale CH, Ambrose PG, Drusano GL, Murakawa T, editors. Antimicrobial Pharmacodynamics in Theory and Clinical Practice. 2nd ed. Taylor & Francis Group, LLC; Boca Raton, FL: 2007. [Google Scholar]
- 14.Bennett JE, Dolin R, Blaser MJ, editors. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. 8th ed. Saunders; Philadelphia: 2015. [Google Scholar]
- 15.Barbour A, Scaglione F, Derendorf H. Class-dependent relevance of tissue distribution in the interpretation of anti-infective pharmacokinetic/pharmacodynamic indices. Int J Antimicrob Agents. 2010;35(5):431–438. doi: 10.1016/j.ijantimicag.2010.01.023. [DOI] [PubMed] [Google Scholar]
- 16.Kunin CM, Craig WA, Kornguth M, Monson R. Influence of binding on the pharmacologic activity of antibiotics. Ann N Y Acad Sci. 1973;226(3):214–234. doi: 10.1111/j.1749-6632.1973.tb20483.x. [DOI] [PubMed] [Google Scholar]
- 17.Craig WA, Welling PG. Protein binding of antimicrobials: clinical pharmacokinetic and therapeutic implications. Clin Pharmacokinet. 1977;2:252–268. doi: 10.2165/00003088-197702040-00002. [DOI] [PubMed] [Google Scholar]
- 18.Craig WA, Ebert SC. Protein binding and its significance in antibacterial therapy. Infect Dis Clin North Am. 1989;3:407–414. [PubMed] [Google Scholar]
- 19.Gonzalez D, Schmidt S, Derendorf H. Importance of relating efficacy measures to unbound drug concentrations for anti-infective agents. Clin Microbiol Rev. 2013;26(2):274–288. doi: 10.1128/CMR.00092-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zeitlinger MA, Sauermann R, Traunmüller F, Georgopoulos A, Müller M, Joukhadar C. Impact of plasma protein binding on antimicrobial activity using time-killing curves. J Antimicrob Chemother. 2004;54(5):876–880. doi: 10.1093/jac/dkh443. [DOI] [PubMed] [Google Scholar]
- 21.Ulldemolins M, Roberts JA, Rello J, Paterson DL, Lipman J. The effects of hypoalbuminaemia on optimizing antibacterial dosing in critically ill patients. Clin Pharmacokinet. 2011;50(2):99–110. doi: 10.2165/11539220-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 22.Roberts JA, Pea F, Lipman J. The clinical relevance of plasma protein binding changes. Clin Pharmacokinet. 2013;52(1):1–8. doi: 10.1007/s40262-012-0018-5. [DOI] [PubMed] [Google Scholar]
- 23.Matzke GR, McGory RW, Halstenson CE, Keane WF. Pharmacokinetics of vancomycin in patients with various degrees of renal function. Antimicrob Agents Chemother. 1984;25:433–437. doi: 10.1128/aac.25.4.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Patel N, Scheetz MH, Drusano GL, Lodise TP. Determination of antibiotic dosage adjustments in patients with renal impairment: elements for success. J Antimicrob Chemother. 2010;65(11):2285–2290. doi: 10.1093/jac/dkq323. [DOI] [PubMed] [Google Scholar]
- 25.Udy AA, Roberts JA, Boots RJ, Paterson DL, Lipman J. Augmented renal clearance: implications for antibacterial dosing in the critically ill. Clin Pharmacokinet. 2010;49(1):1–16. doi: 10.2165/11318140-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 26.Baptista JP, Sousa E, Martins PJ, Pimentel JM. Augmented renal clearance in septic patients and implications for vancomycin optimisation. Int J Antimicrob Agents. 2012;39(5):420–423. doi: 10.1016/j.ijantimicag.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 27.Udy AA, Lipman J, Jarrett P, et al. Are standard doses of piperacillin sufficient for critically ill patients with augmented creatinine clearance? Crit Care. 2015;19:1–9. doi: 10.1186/s13054-015-0750-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gaieski DF, Mikkelsen ME, Band RA, et al. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Crit Care Med. 2010;38(4):1045–1053. doi: 10.1097/CCM.0b013e3181cc4824. [DOI] [PubMed] [Google Scholar]
- 29.Tumbarello M, Viale P, Viscoli C, et al. Predictors of mortality in bloodstream infections caused by Klebsiella pneumoniae carbapenemase-producing K. pneumoniae: Importance of combination therapy. Clin Infect Dis. 2012;55(7):943–950. doi: 10.1093/cid/cis588. [DOI] [PubMed] [Google Scholar]
- 30.Van Hal SJ, Jensen SO, Vaska VL, Espedido BA, Paterson DL, Gosbell IB. Predictors of mortality in Staphylococcus aureus bacteremia. Clin Microbiol Rev. 2012;25(2):362–386. doi: 10.1128/CMR.05022-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign: international guidelines of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41(2):580–637. doi: 10.1097/CCM.0b013e31827e83af. [DOI] [PubMed] [Google Scholar]
- 32.Van Der Poll T. Immunotherapy of sepsis. Lancet Infect Dis. 2001;1(3):165–174. doi: 10.1016/S1473-3099(01)00093-7. [DOI] [PubMed] [Google Scholar]
- 33.Claus BOM, Hoste EA, Colpaert K, Robays H, Decruyenaere J, De Waele JJ. Augmented renal clearance is a common finding with worse clinical outcome in critically ill patients receiving antimicrobial therapy. J Crit Care. 2013;28(5):695–700. doi: 10.1016/j.jcrc.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 34.Roberts JA, Lipman J. Pharmacokinetic issues for antibiotics in the critically ill patient. Crit Care Med. 2009;37(3):840–851. doi: 10.1097/CCM.0b013e3181961bff. quiz 859. [DOI] [PubMed] [Google Scholar]
- 35.Joukhadar C, Frossard M, Mayer BX, et al. Impaired target site penetration of beta-lactams may account for therapeutic failure in patients with septic shock. Crit Care Med. 2001;29(2):385–391. doi: 10.1097/00003246-200102000-00030. [DOI] [PubMed] [Google Scholar]
- 36.Shimamoto Y, Fukuda T, Tanaka K, Komori K, Sadamitsu D. Systemic inflammatory response syndrome criteria and vancomycin dose requirement in patients with sepsis. Intensive Care Med. 2013;39(7):1247–1252. doi: 10.1007/s00134-013-2909-9. [DOI] [PubMed] [Google Scholar]
- 37.Beckhouse M, Whyte I, Byth P, Napier J, Smith A. Altered aminoglycoside pharmacokinetics in the critically ill. Anaesth Intes Care. 1988;16:418–422. doi: 10.1177/0310057X8801600406. [DOI] [PubMed] [Google Scholar]
- 38.Taccone FS, Laterre P-F, Dugernier T, et al. Insufficient β-lactam concentrations in the early phase of severe sepsis and septic shock. Crit Care. 2010;14(4):R126. doi: 10.1186/cc9091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Udy AA, Varghese JM, Altukroni M, et al. Subtherapeutic initial β-lactam concentrations in select critically ill patients: association between augmented renal clearance and low trough drug concentrations. Chest. 2012;142(1):30–39. doi: 10.1378/chest.11-1671. [DOI] [PubMed] [Google Scholar]
- 40.Alves MD, Ribeiro VB, Tessari JP, et al. Effect of cefepime dose on mortality of patients with Gram-negative bacterial bloodstream infections: a prospective cohort study. J Antimicrob Chemother. 2014;69(6):1681–1687. doi: 10.1093/jac/dku001. [DOI] [PubMed] [Google Scholar]
- 41.Roberts JA, Paul SK, Akova M, et al. DALI: Defining antibiotic levels in intensive care unit patients: are current ß-lactam antibiotic doses sufficient for critically ill patients? Clin Infect Dis. 2014;58(8):1072–1083. doi: 10.1093/cid/ciu027. [DOI] [PubMed] [Google Scholar]
- 42.De Montmollin E, Bouadma L, Gault N, et al. Predictors of insufficient amikacin peak concentration in critically ill patients receiving a 25 mg/kg total body weight regimen. Intensive Care Med. 2014;40(7):998–1005. doi: 10.1007/s00134-014-3276-x. [DOI] [PubMed] [Google Scholar]
- 43.Roger C, Nucci B, Molinari N, et al. Standard dosing of amikacin and gentamicin in critically ill patients results in variable and subtherapeutic concentrations. Int J Antimicrob Agents. 2015;46(1):21–27. doi: 10.1016/j.ijantimicag.2015.02.009. [DOI] [PubMed] [Google Scholar]
- 44.Roberts JA, Lipman J. Antibacterial dosing in intensive care: pharmacokinetics, degree of disease and pharmacodynamics of sepsis. Clin Pharmacokinet. 2006;45(8):755–773. doi: 10.2165/00003088-200645080-00001. [DOI] [PubMed] [Google Scholar]
- 45.Gous A, Lipman J, Scribante J, et al. Fluid shifts have no influence on ciprofloxacin pharmacokinetics in intensive care patients with intra-abdominal sepsis. Int J Antimicrob Agents. 2005;26(1):50–55. doi: 10.1016/j.ijantimicag.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 46.Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a Ssientific statement for healthcare professionals from the American Heart Association. Circulation. 2015;132:1–52. doi: 10.1161/CIR.0000000000000296. [DOI] [PubMed] [Google Scholar]
- 47.Forstner C, Dungl C, Tobudic S, Mitteregger D, Lagler H, Burgmann H. Predictors of clinical and microbiological treatment failure in patients with methicillin-resistant Staphylococcus aureus (MRSA) bacteraemia: a retrospective cohort study in a region with low MRSA prevalence. Clin Microbiol Infect. 2013;19(7):E291–E297. doi: 10.1111/1469-0691.12169. [DOI] [PubMed] [Google Scholar]
- 48.Cremieux A-C, Carbon C. Pharmacokinetic and pharmacodynamic requirements for antibiotic therapy of experimental endocarditis. Antimicrob Agents Chemother. 1992;36(10):2069. doi: 10.1128/aac.36.10.2069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tsuji BT, Rybak MJ. Short-course gentamicin in combination with daptomycin or vancomycin against Staphylococcus aureus in an in vitro pharmacodynamic model with simulated endocardial vegetations. Antimicrob Agents Chemother. 2005;49(7):2735–2745. doi: 10.1128/AAC.49.7.2735-2745.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rybak M, Lomaestro B, Rotschafer JC, et al. Therapeutic monitoring of vancomycin in adult patients: a consensus review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists. Am J Heal Pharm. 2009;66(1):82–98. doi: 10.2146/ajhp080434. [DOI] [PubMed] [Google Scholar]
- 51.Baldwin DR, Honeybourne D, Wise R. Pulmonary disposition of antimicrobial agents: in vivo observations and clinical relevance. Antimicrob Agents Chemother. 1992;36(6):1176–1180. doi: 10.1128/aac.36.6.1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rodvold KA, George JM, Yoo L. Penetration of anti-infective agents into pulmonary epithelial lining fluid. Clin Pharmacokinet. 2011;50(10):637–664. doi: 10.2165/11594090-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 53.Boselli E, Breilh D, Rimmelé T, et al. Plasma and lung concentrations of ceftazidime administered in continuous infusion to critically ill patients with severe nosocomial pneumonia. Intensive Care Med. 2004;30(5):989–991. doi: 10.1007/s00134-004-2171-2. [DOI] [PubMed] [Google Scholar]
- 54.Boselli E, Breilh D, Duflo F, et al. Steady-state and intrapulmonary concentrations of cefepime adminstered in continuous infusion in critically ill patients with severe nosocomial pneumonia. Crit Care Med. 2003;31(8):2102–2106. doi: 10.1097/01.CCM.0000069734.38738.C8. [DOI] [PubMed] [Google Scholar]
- 55.Boselli E, Breilh D, Cannesson M, et al. Steady-state plasma and intrapulmonary concentrations of piperacillin/tazobactam 4 g/0.5 g administered to critically ill patients with severe nosocomial pneumonia. Intensive Care Med. 2004;30(5):976–979. doi: 10.1007/s00134-004-2222-8. [DOI] [PubMed] [Google Scholar]
- 56.Boselli E, Breilh D, Rimmelé T, et al. Alveolar concentrations of piperacillin/tazobactam administered in continuous infusion to patients with ventilator-associated pneumonia. Crit Care Med. 2008;36(5):1500–1506. doi: 10.1097/CCM.0b013e318170ba21. [DOI] [PubMed] [Google Scholar]
- 57.Felton TW, McCalman K, Malagon I, et al. Pulmonary penetration of piperacillin and tazobactam in critically ill patients. Clin Pharmacol Ther. 2014;96:1–11. doi: 10.1038/clpt.2014.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Valcke YJ, Rosseel MT, Pauwels RA, Bogaert MG, Van Der Straeten ME. Penetration of ampicillin and sulbactam in the lower airways during respiratory infections. Antimicrob Agents Chemother. 1990;34(6):958–962. doi: 10.1128/aac.34.6.958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Riccobene T, Pushkin R, Jandourek A. Penetration of Ceftaroline into Epithelial Lining Fluid. Abstract A-469; 55th Interscience Conference on Antimicrobial Agents and Chemotherapy; San Diego, California. 2015; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chandorkar G, Huntington JA, Gotfried MH, Rodvold KA, Umeh O. Intrapulmonary penetration of ceftolozane/tazobactam and piperacillin/tazobactam in healthy adult subjects. J Antimicrob Chemother. 2012;67(10):2463–2469. doi: 10.1093/jac/dks246. [DOI] [PubMed] [Google Scholar]
- 61.Lodise TP, Sorgel F, Melnick D, Mason B, Kinzig M, Drusano GL. Penetration of meropenem into epithelial lining fluid of patients with ventilator-associated pneumonia. Antimicrob Agents Chemother. 2011;55(4):1606–1610. doi: 10.1128/AAC.01330-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Frippiat F, Musuamba FT, Seidel L, et al. Modelled target attainment after meropenem infusion in patients with severe nosocomial pneumonia: The PROMESSE study. J Antimicrob Chemother. 2015;70(1):207–216. doi: 10.1093/jac/dku354. [DOI] [PubMed] [Google Scholar]
- 63.Wenzler E, Gotfried MH, Loutit JS, et al. Plasma, Epithelial Lining Fluid, and Alveolar Macrophage Concentrations of Meropenem-RPX7009 in Healthy Adult Subjects. Antimicrob Agents Chemother. 2015;59(12):7232–7239. doi: 10.1128/AAC.01713-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Boselli E, Breilh D, Saux MC, Gordien JB, Allaouchiche B. Pharmacokinetics and lung concentrations of ertapenem in patients with ventilator-associated pneumonia. Intensive Care Med. 2006;32(12):2059–2062. doi: 10.1007/s00134-006-0401-5. [DOI] [PubMed] [Google Scholar]
- 65.Justo J, Gotfried M, Deyo K, Fischer P, Danziger L, Rodvold K. Doripenem Intrapulmonary Pharmacokinetics in Healthy Adult Subjects; 51st Interscience Conference on Antimicrobial Agents and Chemotherapy; Chicago, Illinois. 2011; Abstract A1-1748. [Google Scholar]
- 66.Van Hasselt JGC, Rizk ML, Lala M, et al. Br J Clin Pharmacol. 2016. Pooled population pharmacokinetic model of imipenem in plasma and the lung epithelial lining fluid. In Press. [Google Scholar]
- 67.Drusano GL. Pharmacokinetics and pharmacodynamics of antimicrobials. Clin Infect Dis. 2007;45(Suppl 1):S89–S95. doi: 10.1086/518137. [DOI] [PubMed] [Google Scholar]
- 68.Ambrose PG, Bhavnani SM, Ellis-Grosse EJ, Drusano GL. Pharmacokinetic-pharmacodynamic considerations in the design of hospital-acquired or ventilator-associated bacterial pneumonia studies: look before you leap! Clin Infect Dis. 2010;51(Suppl 1):103–110. doi: 10.1086/653057. [DOI] [PubMed] [Google Scholar]
- 69.Lamer C, De Beco V, Soler P, et al. Analysis of vancomycin entry into pulmonary lining fluid by bronchoalveolar lavage in critically ill patients. Antimicrob Agents Chemother. 1993;37(2):281–286. doi: 10.1128/aac.37.2.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Georges H, Leroy O, Alfandari S, et al. Pulmonary disposition of vancomycin in critically ill patients. Eur J Clin Microbiol Infect Dis. 1997;16(5):385–388. doi: 10.1007/BF01726369. [DOI] [PubMed] [Google Scholar]
- 71.Lodise TP, Drusano GL, Butterfield JM, Scoville J, Gotfried M, Rodvold KA. Penetration of vancomycin into epithelial lining fluid in healthy volunteers. Antimicrob Agents Chemother. 2011;55(12):5507–5511. doi: 10.1128/AAC.00712-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gotfried MH, Danziger LH, Rodvold KA. Steady-state plasma and intrapulmonary concentrations of levofloxacin and ciprofloxacin in healthy adult subjects. Chest. 2001;119(4):1114–1122. doi: 10.1378/chest.119.4.1114. [DOI] [PubMed] [Google Scholar]
- 73.Mouton JW, Dudley MN, Cars O, Derendorf H, Drusano GL. Standardization of pharmacokinetic/pharmacodynamic (PK/PD) terminology for anti-infective drugs: an update. J Antimicrob Chemother. 2005;55(5):601–607. doi: 10.1093/jac/dki079. [DOI] [PubMed] [Google Scholar]
- 74.Drusano G, Preston S, Gotfried M, Danziger LH, Rodvold KA. Levofloxacin penetration into epithelial lining fluid as determined by population pharmacokinetic modeling and Monte Carlo simulation. Antimicrob Agents Chemother. 2002;46(2):586–589. doi: 10.1128/AAC.46.2.586-589.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rodvold KA, Danziger LH, Gotfried MH. Steady-state plasma and bronchopulmonary concentrations of intravenous levofloxacin and azithromycin in healthy adults. Antimicrob Agents Chemother. 2003;47(8):2450–2457. doi: 10.1128/AAC.47.8.2450-2457.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Capitano B, Mattoes HM, Shore E, et al. Steady-state intrapulmonary concentrations of moxifloxacin, levofloxacin, and azithromycin in older adults. Chest. 2004;125:965–973. doi: 10.1378/chest.125.3.965. [DOI] [PubMed] [Google Scholar]
- 77.Boselli E, Breilh D, Rimmelé T, et al. Pharmacokinetics and intrapulmonary diffusion of levofloxacin in critically ill patients with severe community-acquired pneumonia. Crit Care Med. 2005;33(1):104–109. doi: 10.1097/01.ccm.0000150265.42067.4c. [DOI] [PubMed] [Google Scholar]
- 78.Nicolau DP, Sutherland C, Winget D, Baughman RP. Bronchopulmonary pharmacokinetic and pharmacodynamic profiles of levofloxacin 750mg once daily in adults undergoing treatment for acute exacerbation of chronic bronchitis. Pulm Pharmacol Ther. 2012;25(1):94–98. doi: 10.1016/j.pupt.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 79.Panidis D, Markantonis SL, Boutzouka E, Karatzas S, Baltopoulos G. Penetration of gentamicin into the alveolar lining fluid of critically ill patients with ventilator-associated pneumonia. Chest. 2005;128(2):545–552. doi: 10.1378/chest.128.2.545. [DOI] [PubMed] [Google Scholar]
- 80.Carcas AJ, García-Satué JL, Zapater P, Frías-Iniesta J. Tobramycin penetration into epithelial lining fluid of patients with pneumonia. Clin Pharmacol Ther. 1999;65(3):245–250. doi: 10.1016/S0009-9236(99)70103-7. [DOI] [PubMed] [Google Scholar]
- 81.Boselli E, Breilh D, Djabarouti S, et al. Reliability of mini-bronchoalveolar lavage for the measurement of epithelial lining fluid concentrations of tobramycin in critically ill patients. Intensive Care Med. 2007;33(9):1519–1523. doi: 10.1007/s00134-007-0688-x. [DOI] [PubMed] [Google Scholar]
- 82.Kiang TKL, Häfeli UO, Ensom MHH. A comprehensive review on the pharmacokinetics of antibiotics in interstitial fluid spaces in humans: implications on dosing and clinical pharmacokinetic monitoring. Clin Pharmacokinet. 2014;53(8):695–730. doi: 10.1007/s40262-014-0152-3. [DOI] [PubMed] [Google Scholar]
- 83.Brunner M, Derendorf H, Müller M. Microdialysis for in vivo pharmacokinetic/pharmacodynamic characterization of anti-infective drugs. Curr Opin Pharmacol. 2005;5(5 SPEC.ISS.):495–499. doi: 10.1016/j.coph.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 84.Azeredo FJ, Dalla Costa T, Derendorf H. Role of microdialysis in pharmacokinetics and pharmacodynamics: current status and future directions. Clin Pharmacokinet. 2014;53(3):205–212. doi: 10.1007/s40262-014-0131-8. [DOI] [PubMed] [Google Scholar]
- 85.Barza M. Anatomical barriers for antimicrobial agents. Eur J Clin Microbiol Infect Dis. 1993;12(1):S31–S35. doi: 10.1007/BF02389875. [DOI] [PubMed] [Google Scholar]
- 86.Brunner M, Pernerstorfer T, Mayer BX, Eichler HG, Müller M. Surgery and intensive care procedures affect the target site distribution of piperacillin. Crit Care Med. 2000;28(6):1754–1759. doi: 10.1097/00003246-200006000-00009. [DOI] [PubMed] [Google Scholar]
- 87.Burkhardt O, Brunner M, Schmidt S, Grant M, Tang Y, Derendorf H. Penetration of ertapenem into skeletal muscle and subcutaneous adipose tissue in healthy volunteers measured by in vivo microdialysis. J Antimicrob Chemother. 2006;58(3):632–636. doi: 10.1093/jac/dkl284. [DOI] [PubMed] [Google Scholar]
- 88.Payne CJ, Thomson AH, Stearns AT, et al. Pharmacokinetics and tissue penetration of vancomycin continuous infusion as prophylaxis for vascular surgery. J Antimicrob Chemother. 2011;66(11):2624–2627. doi: 10.1093/jac/dkr326. [DOI] [PubMed] [Google Scholar]
- 89.Hanley MJ, Abernethy DR, Greenblatt DJ. Effect of obesity on the pharmacokinetics of drugs in humans. Clin Pharmacokinet. 2010;49(2):71–87. doi: 10.2165/11318100-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 90.Pai MP. Drug dosing based on weight and body surface area: mathematical assumptions and limitations in obese adults. Pharmacotherapy. 2012;32(9):856–868. doi: 10.1002/j.1875-9114.2012.01108.x. [DOI] [PubMed] [Google Scholar]
- 91.Lazzarini L, Lipsky BA, Mader JT. Antibiotic treatment of osteomyelitis: what have we learned from 30 years of clinical trials? Int J Infect Dis. 2005;9(3):127–138. doi: 10.1016/j.ijid.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 92.Spellberg B, Lipsky BA. Systemic antibiotic therapy for chronic osteomyelitis in adults. Clin Infect Dis. 2012;54(3):393–407. doi: 10.1093/cid/cir842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Landersdorfer CB, Bulitta JB, Kinzig M, Holzgrabe U, Sorgel F. Penetration of antibacterials into bone. Clin Pharmacokinet. 2009;48(2):89–124. doi: 10.2165/00003088-200948020-00002. [DOI] [PubMed] [Google Scholar]
- 94.Fitzgerald RH, Kelly PJ, Snyder RJ, Washington JA. Penetration of methicillin, oxacillin, and cephalothin into bone and synovial tissues. Antimicrob Agents Chemother. 1978;14(5):723–726. doi: 10.1128/aac.14.5.723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Breilh D, Boselli E, Bel J, Chassard D, Saux M, Allaouchiche B. Diffusion of cefepime into cancellous and cortical bone tissue. J Chemother. 2003;15:134–138. doi: 10.1179/joc.2003.15.2.134. [DOI] [PubMed] [Google Scholar]
- 96.Warnke J-P, Wildfeuer A, Eibel G, Pfaff G, Klammer A. Pharmacokinetics of ampicillin/sulbactam in patients undergoing spinal microneurosurgical procedures. Int J Clin Pharmacol Ther. 1998;36:253–257. [PubMed] [Google Scholar]
- 97.Incavo SJ, Ronchetti PJ, Choi JH, Wu H, Kinzig M, Sorgel F. Penetration of piperacillin-tazobactam into cancellous and cortical bone tissues. Antimicrob Agents Chemother. 1994;38(4):905–907. doi: 10.1128/aac.38.4.905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Polk R, Hume A, Kline BJ, Cardea J. Penetration of moxalactam and cefazolin into bone following simultaneous bolus or infusion. Clin Orthop Relat Res. 1983;177:216–221. [PubMed] [Google Scholar]
- 99.Leigh DA, Griggs J, Tighe CM, et al. Pharmacokinetic study of ceftazidime in bone and serum of patients undergoing hip and knee arthroplasty. J Antimicrob Chemother. 1985;16(5):637–642. doi: 10.1093/jac/16.5.637. [DOI] [PubMed] [Google Scholar]
- 100.Garazzino S, Aprato A, Baietto L, et al. Glycopeptide bone penetration in patients with septic pseudoarthritis of the tibia. Clin Pharmacokinet. 2008;47(12):793–805. doi: 10.2165/0003088-200847120-00004. [DOI] [PubMed] [Google Scholar]
- 101.MacGregor RR, Gibson GA, Bland JA. Imipenem pharmacokinetics and body fluid concentrations in patients receiving high-dose treatment for serious infections. Antimicrob Agents Chemother. 1986;29(2):188–192. doi: 10.1128/aac.29.2.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Breilh D, Boselli E, Bel JC, Saux MC, Allaouchiche B, Djabarouti S. Diffusion of ertapenem into bone and synovial tissues. J Antimicrob Chemother. 2007;60(4):893–896. doi: 10.1093/jac/dkm296. [DOI] [PubMed] [Google Scholar]
- 103.Graziani AL, Lawson LA, Gibson GA, Steinberg MA, MacGregor RR. Vancomycin concentrations in infected and noninfected human bone. Antimicrob Agents Chemother. 1988;32(9):1320–1322. doi: 10.1128/aac.32.9.1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Fong IW, Ledbetter WH, Vandenbroucke AC, Simbul M, Rahm V. Ciprofloxacin concentrations in bone and muscle after oral dosing. Antimicrob Agents Chemother. 1986;29(3):405–408. doi: 10.1128/aac.29.3.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Malincarne L, Ghebregzabher M, Moretti MV, et al. Penetration of moxifloxacin into bone in patients undergoing total knee arthroplasty. J Antimicrob Chemother. 2006;57(5):950–954. doi: 10.1093/jac/dkl091. [DOI] [PubMed] [Google Scholar]
- 106.Rimmelé T. Diffusion of levofloxacin into bone and synovial tissues. J Antimicrob Chemother. 2004;53(3):533–535. doi: 10.1093/jac/dkh110. [DOI] [PubMed] [Google Scholar]
- 107.Andes DR, Craig WA. Pharmacokinetics and pharmacodynamics of antibiotics in meningitis. Infect Dis Clin North Am. 1999;13:595–618. doi: 10.1016/s0891-5520(05)70096-9. [DOI] [PubMed] [Google Scholar]
- 108.Nau R, Sörgel F, Eiffert H. Penetration of drugs through the blood-cerebrospinal fluid/blood-brain barrier for treatment of central nervous system infections. Clin Microbiol Rev. 2010;23(4):858–883. doi: 10.1128/CMR.00007-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Spector R. Nature and consequences of mammalian brain and CSF efflux transporters: four decades of progress. J Neurochem. 2010;112(1):13–23. doi: 10.1111/j.1471-4159.2009.06451.x. [DOI] [PubMed] [Google Scholar]
- 110.Di Paolo A, Gori G, Tascini C, Danesi R, Del Tacca M. Clinical pharmacokinetics of antibacterials in cerebrospinal fluid. Clin Pharmacokinet. 2013;52(7):511–542. doi: 10.1007/s40262-013-0062-9. [DOI] [PubMed] [Google Scholar]
- 111.Nau R, Sörgel F, Prange HW. Lipophilicity at pH 7.4 and molecular size govern the entry of the free serum fraction of drugs into the cerebrospinal fluid in humans with uninflamed meninges. J Neurol Sci. 1994;122(1):61–65. doi: 10.1016/0022-510x(94)90052-3. [DOI] [PubMed] [Google Scholar]
- 112.Radouane A, Pehourcq F, Tramu G, Creppy E, Bannwarth B. Influence of lipophilicity on the diffusion of cephalosporins into the cerebrospinal fluid. Fundam Clin Pharmacol. 1996;10:309–313. doi: 10.1111/j.1472-8206.1996.tb00311.x. [DOI] [PubMed] [Google Scholar]
- 113.Djukic M, Munz M, Sörgel F, Holzgrabe U, Eiffert H, Nau R. Overton’s rule helps to estimate the penetration of anti-infectives into patients’ cerebrospinal fluid. Antimicrob Agents Chemother. 2012;56(2):979–988. doi: 10.1128/AAC.00437-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Nau R, Prange HW, Martell J, Sharifi S, Kolenda H, Bircher J. Penetration of ciprofloxacin into the cerebrospinal fluid of patients with uninflamed meninges. J Antimicrob Chemother. 1990;25(6):965–973. doi: 10.1093/jac/25.6.965. [DOI] [PubMed] [Google Scholar]
- 115.Pea F, Pavan F, Nascimben E, et al. Levofloxacin disposition in cerebrospinal fluid in patients with external ventriculostomy. Antimicrob Agents Chemother. 2003;47(10):3104–3108. doi: 10.1128/AAC.47.10.3104-3108.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kanellakopoulou K, Pagoulatou A, Stroumpoulis K, et al. Pharmacokinetics of moxifloxacin in non-inflamed cerebrospinal fluid of humans: implication for a bactericidal effect. J Antimicrob Chemother. 2008;61(6):1328–1331. doi: 10.1093/jac/dkn110. [DOI] [PubMed] [Google Scholar]
- 117.Karlsson M, Hammers S, Nilsson-Ehle I, Malmborg AS, Wretlind B. Concentrations of doxycycline and penicillin G in sera and cerebrospinal fluid of patients treated for neuroborreliosis. Antimicrob Agents Chemother. 1996;40(5):1104–1107. doi: 10.1128/aac.40.5.1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Clumeck N, Thys JP, Vanhoof R, Vanderlinden MP, Butzler JP, Yourassowsky E. Amoxicillin entry into human cerebrospinal fluid. Comparison with ampicillin. Antimicrob Agents Chemother. 1978;14(4):531–532. doi: 10.1128/aac.14.4.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Fong IW, Tomkins KB. Penetration of ceftazidime into the cerebrospinal fluid of patients with and without evidence of meningeal inflammation. Antimicrob Agents Chemother. 1984;26(1):115–116. doi: 10.1128/aac.26.1.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Nau R, Kinzig-Schippers M, Sörgel F, et al. Kinetics of piperacillin and tazobactam in ventricular cerebrospinal fluid of hydrocephalic patients. Antimicrob Agents Chemother. 1997;41(5):987–991. doi: 10.1128/aac.41.5.987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Rhoney DH, Tam VH, Parker D, Jr., McKinnon PS, Coplin WM. Disposition of cefepime in the central nervous system of patients with external ventricular drains. Pharmacotherapy. 2003;23(3):310–314. doi: 10.1592/phco.23.3.310.32108. [DOI] [PubMed] [Google Scholar]
- 122.Nau R, Lassek C, Kinzig-Schippers M, Thiel A, Prange HW, Sörgel F. Disposition and elimination of meropenem in cerebrospinal fluid of hydrocephalic patients with external ventriculostomy. Antimicrob Agents Chemother. 1998;42(8):2012–2016. doi: 10.1128/aac.42.8.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Nalda-Molina R, Dokoumetzidis A, Charkoftaki G, et al. Pharmacokinetics of doripenem in CSF of patients with non-inflamed meninges. J Antimicrob Chemother. 2012;67(7):1722–1729. doi: 10.1093/jac/dks106. [DOI] [PubMed] [Google Scholar]
- 124.Albanèse J, Léone M, Bruguerolle B, et al. Cerebrospinal fluid penetration and pharmacokinetics of vancomycin administered by continuous infusion to mechanically ventilated patients in an intensive care unit. Antimicrob Agents Chemother. 2000;44(5):5–8. doi: 10.1128/aac.44.5.1356-1358.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Dickinson GM, Droller DG, Greenman RL, Hoffman TA. Clinical evaluation of piperacillin with observations on penetrability into cerebrospinal fluid. Antimicrob Agents Chemother. 1981;20(4):481–486. doi: 10.1128/aac.20.4.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Stahl J-P, Bru J-P, Fredj G, Brammer KW, Malleret M-R, Micoud M. Penetration of sulbactam into the cerebrospinal fluid of patients with bacterial meningitis receiving ampicillin therapy. Rev Infect Dis. 1986;8:S612–S616. doi: 10.1093/clinids/8.supplement_5.s612. [DOI] [PubMed] [Google Scholar]
- 127.Dagan R, Velghe L, Rodda JL, Klugman KP. Penetration of meropenem into the cerebrospinal fluid of patients with inflamed meninges. J Antimicrob Chemother. 1994;34(1):175–179. doi: 10.1093/jac/34.1.175. [DOI] [PubMed] [Google Scholar]
- 128.Ricard J, Wolff M, Lacherade J, et al. Levels of vancomycin in cerebrospinal fluid of adult patients receiving adjunctive corticosteroids to treat pneumococcal meningitis : a prospective multicenter observational study. Clin Infect Dis. 2007;44:250–255. doi: 10.1086/510390. [DOI] [PubMed] [Google Scholar]
- 129.Tunkel AR, Hartman BJ, Kaplan SL, et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis. 2004;39(9):1267–1284. doi: 10.1086/425368. [DOI] [PubMed] [Google Scholar]
- 130.Wolff M, Boutron L, Singlas E, Clair B, Decazes J, Regnier B. Penetration of ciprofloxacin into cerebrospinal fluid of patients with bacterial meningitis. Antimicrob Agents Chemother. 1987;31(6):899–902. doi: 10.1128/aac.31.6.899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Alffenaar J, van Altena R, Bökkerink H, et al. Pharmacokinetics of moxifloxacin in cerebrospinal fluid and plasma in patients with tuberculous meningitis. Clin Infect Dis. 2009;49(7):1080–1082. doi: 10.1086/605576. [DOI] [PubMed] [Google Scholar]
- 132.Craig WA. Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin Infect Dis. 1998;26(1):1–10. doi: 10.1086/516284. [DOI] [PubMed] [Google Scholar]
- 133.Drusano GL. Antimicrobial pharmacodynamics: critical interactions of “bug and drug”. Nat Rev Microbiol. 2004;2(4):289–300. doi: 10.1038/nrmicro862. [DOI] [PubMed] [Google Scholar]
- 134.Ambrose PG, Bhavnani SM, Rubino CM, et al. Pharmacokinetics-pharmacodynamics of antimicrobial therapy: it’s not just for mice anymore. Clin Infect Dis. 2007;44(1):79–86. doi: 10.1086/510079. [DOI] [PubMed] [Google Scholar]
- 135.Craig WA. Post-antibiotic effects in experimental infection models: relationship to in-vitro phenomena and to treatment of infections in man. J Antimicrob Chemother. 1993;31(Suppl D):149–158. doi: 10.1093/jac/31.suppl_d.149. [DOI] [PubMed] [Google Scholar]
- 136.Vogelman B, Gudmundsson S, Leggett J, Turnidge J, Ebert S, Craig WA. Correlation of antimicrobial pharmacokinetic parameters with therapeutic efficacy in an animal model. J Infect Dis. doi: 10.1093/infdis/158.4.831. [DOI] [PubMed] [Google Scholar]
- 137.Velkov T, Bergen PJ, Lora-Tamayo J, Landersdorfer CB, Li J. PK/PD models in antibacterial development. Curr Opin Microbiol. 2013;16(5):573–579. doi: 10.1016/j.mib.2013.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Zhao X, Drlica K. Restricting the selection of antibiotic-resistant mutants: a general strategy derived from fluoroquinolone studies. Clin Infect Dis. 2001;33(Suppl 3(33)):S147–S156. doi: 10.1086/321841. [DOI] [PubMed] [Google Scholar]
- 139.Drlica K, Zhao X. Mutant selection window hypothesis updated. Clin Infect Dis. 2007;44(5):681–688. doi: 10.1086/511642. [DOI] [PubMed] [Google Scholar]
- 140.Tam VH, McKinnon PS, Akins RL, Rybak MJ, Drusano GL. Pharmacodynamics of cefepime in patients with Gram-negative infections. J Antimicrob Chemother. 2002;50(3):425–428. doi: 10.1093/jac/dkf130. [DOI] [PubMed] [Google Scholar]
- 141.Li C, Du X, Kuti JL, Nicolau DP. Clinical pharmacodynamics of meropenem in patients with lower respiratory tract infections. Antimicrob Agents Chemother. 2007;51(5):1725–1730. doi: 10.1128/AAC.00294-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Eagle H, Fleischman R, Musselman AD. Effect of schedule of administration on the therapeutic efficacy of penicillin. Am J Med. 1950;9(3):280–299. doi: 10.1016/0002-9343(50)90425-6. [DOI] [PubMed] [Google Scholar]
- 143.Eagle H, Fleischman R, Levy M. Continuous vs. discontinuous therapy with penicillin. N Engl J Med. 1953;248:481–488. doi: 10.1056/NEJM195303192481201. [DOI] [PubMed] [Google Scholar]
- 144.Craig WA. Interrelationship between pharmacokinetics and pharmacodynamics in determining dosage regimens for broad-spectrum cephalosporins. Diagn Microbiol Infect Dis. 1995;22(1-2):89–96. doi: 10.1016/0732-8893(95)00053-d. [DOI] [PubMed] [Google Scholar]
- 145.Leggett JE, Fantin B, Ebert S, et al. Comparative antibiotic dose-effect relations at several dosing intervals in murine pneumonitis and thigh-infection models. J Infect Dis. 1989;159(2):281–292. doi: 10.1093/infdis/159.2.281. [DOI] [PubMed] [Google Scholar]
- 146.Bhavnani SM, Hammel JP, Van Wart SA, et al. Pharmacokinetic-pharmacodynamic analysis for efficacy of ceftaroline fosamil in patients with acute bacterial skin and skin structure infections. Antimicrob Agents Chemother. 2015;59(1):372–380. doi: 10.1128/AAC.02531-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Ariano RE, Nyhlén A, Donnelly JP, Sitar DS, Harding GKM, Zelenitsky SA. Pharmacokinetics and pharmacodynamics of meropenem in febrile neutropenic patients with bacteremia. Ann Pharmacother. 2005;39(1):32–38. doi: 10.1345/aph.1E271. [DOI] [PubMed] [Google Scholar]
- 148.McKinnon PS, Paladino JA, Schentag JJ. Evaluation of area under the inhibitory curve (AUIC) and time above the minimum inhibitory concentration (T>MIC) as predictors of outcome for cefepime and ceftazidime in serious bacterial infections. Int J Antimicrob Agents. 2008;31(4):345–351. doi: 10.1016/j.ijantimicag.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 149.Crandon JL, Bulik CC, Kuti JL, Nicolau DP. Clinical pharmacodynamics of cefepime in patients infected with Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2010;54(3):1111–1116. doi: 10.1128/AAC.01183-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Muller AE, Punt N, Mouton JW. Optimal exposures of ceftazidime predict the probability of microbiological and clinical outcome in the treatment of nosocomial pneumonia. J Antimicrob Chemother. 2013;68(4):900–906. doi: 10.1093/jac/dks468. [DOI] [PubMed] [Google Scholar]
- 151.MacVane SH, Kuti JL, Nicolau DP. Clinical pharmacodynamics of antipseudomonal cephalosporins in patients with ventilator-associated pneumonia. Antimicrob Agents Chemother. 2014;58(3):1359–1364. doi: 10.1128/AAC.01463-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Rhodes NJ, Kuti JL, Nicolau DP, et al. Defining clinical exposures of cefepime for Gram-negative bloodstream infections that are associated with improved survival. Antimicrob Agents Chemother. 2016;60(3):1401–1410. doi: 10.1128/AAC.01956-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Lodise TP, Lomaestro B, Drusano GL. Piperacillin-tazobactam for Pseudomonas aeruginosa infection: clinical implications of an extended-infusion dosing strategy. Clin Infect Dis. 2007;44(3):357–363. doi: 10.1086/510590. [DOI] [PubMed] [Google Scholar]
- 154.Bauer KA, West JE, O’Brien JM, Goff DA. Extended-infusion cefepime reduces mortality in patients with Pseudomonas aeruginosa infections. Antimicrob Agents Chemother. 2013;57(7):2907–2912. doi: 10.1128/AAC.02365-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Falagas ME, Tansarli GS, Ikawa K, Vardakas KZ. Clinical outcomes with extended or continuous versus short-term intravenous infusion of carbapenems and piperacillin/tazobactam: a systematic review and meta-analysis. Clin Infect Dis. 2013;56(2):272–282. doi: 10.1093/cid/cis857. [DOI] [PubMed] [Google Scholar]
- 156.Yang H, Zhang C, Zhou Q, Wang Y, Chen L. Clinical outcomes with alternative dosing strategies for piperacillin/tazobactam: a systematic review and meta-analysis. PLoS One. 2015;10(1):1–13. doi: 10.1371/journal.pone.0116769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Dulhunty JM, Roberts JA, Davis JS, et al. Continuous infusion of beta-lactam antibiotics in severe sepsis: a multicenter double-blind, randomized controlled trial. Clin Infect Dis. 2013;56(2):236–244. doi: 10.1093/cid/cis856. [DOI] [PubMed] [Google Scholar]
- 158.Craig WA. Basic pharmacodynamics of antibacterials with clinical applications to the use of β-lactams, glycopeptides, and linezolid. Infect Dis Clin North Am. 2003;17(3):479–501. doi: 10.1016/s0891-5520(03)00065-5. [DOI] [PubMed] [Google Scholar]
- 159.Lacy MK, Lu W, Xu X, et al. Pharmacodynamic comparisons of levofloxacin, ciprofloxacin, and ampicillin against Streptococcus pneumoniae in an in vitro model of infection. Antimicrob Agents Chemother. 1999;43(3):672–677. doi: 10.1128/aac.43.3.672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Neely MN, Youn G, Jones B, et al. Are vancomycin trough concentrations adequate for optimal dosing? Antimicrob Agents Chemother. 2014;58(1):309–316. doi: 10.1128/AAC.01653-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Van Hal SJ, Paterson DL, Lodise TP. Systematic review and meta-analysis of vancomycin-induced nephrotoxicity associated with dosing schedules that maintain troughs between 15 and 20 milligrams per liter. Antimicrob Agents Chemother. 2013;57(2):734–744. doi: 10.1128/AAC.01568-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Kullar R, Davis SL, Levine DP, Rybak MJ. Impact of vancomycin exposure on outcomes in patients with methicillin-resistant Staphylococcus aureus bacteremia: support for consensus guidelines suggested targets. Clin Infect Dis. 2011;52(8):975–981. doi: 10.1093/cid/cir124. [DOI] [PubMed] [Google Scholar]
- 163.Brown J, Brown K, Forrest A. Vancomycin AUC 24/MIC ratio in patients with complicated bacteremia and infective endocarditis due to methicillin-resistant Staphylococcus aureus and its association with attributable mortality during hospitalization. Antimicrob Agents Chemother. 2012;56(2):634–638. doi: 10.1128/AAC.05609-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Holmes NE, Turnidge JD, Munckhof WJ, et al. Vancomycin AUC/MIC ratio and 30-day mortality in patients with Staphylococcus aureus bacteremia. Antimicrob Agents Chemother. 2013;57(4):1654–1663. doi: 10.1128/AAC.01485-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Moise-Broder PA, Forrest A, Birmingham MC, Schentag JJ. Pharmacodynamics of vancomycin and other antimicrobials in patients with Staphylococcus aureus lower respiratory tract infections. Clin Pharmacokinet. 2004;43(13):925–942. doi: 10.2165/00003088-200443130-00005. [DOI] [PubMed] [Google Scholar]
- 166.Zelenitsky S, Rubinstein E, Ariano R, et al. Vancomycin pharmacodynamics and survival in patients with methicillin-resistant Staphylococcus aureus-associated septic shock. Int J Antimicrob Agents. 2013;41(3):255–260. doi: 10.1016/j.ijantimicag.2012.10.015. [DOI] [PubMed] [Google Scholar]
- 167.Jung Y, Song KH, Cho JE, et al. Area under the concentration-time curve to minimum inhibitory concentration ratio as a predictor of vancomycin treatment outcome in methicillin-resistant Staphylococcus aureus bacteraemia. Int J Antimicrob Agents. 2014;43(2):179–183. doi: 10.1016/j.ijantimicag.2013.10.017. [DOI] [PubMed] [Google Scholar]
- 168.Lodise TP, Drusano GL, Zasowski E, et al. Vancomycin exposure in patients with methicillin-resistant Staphylococcus aureus bloodstream infections: how much is enough? Clin Infect Dis. 2014;59(5):666–675. doi: 10.1093/cid/ciu398. [DOI] [PubMed] [Google Scholar]
- 169.Casapao AM, Lodise TP, Davis SL, et al. Association between vancomycin day 1 exposure profile and outcomes among patients with methicillin-resistant Staphylococcus aureus infective endocarditis. Antimicrob Agents Chemother. 2015;59(6):2978–2985. doi: 10.1128/AAC.03970-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Lodise TP, Lomaestro B, Graves J, Drusano GL. Larger vancomycin doses (at least four grams per day) are associated with an increased incidence of nephrotoxicity. Antimicrob Agents Chemother. 2008;52(4):1330–1336. doi: 10.1128/AAC.01602-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Patel N, Pai MP, Rodvold KA, Lomaestro B, Drusano GL, Lodise TP. Vancomycin: we can’t get there from here. Clin Infect Dis. 2011;52(8):969–974. doi: 10.1093/cid/cir078. [DOI] [PubMed] [Google Scholar]
- 172.Forrest A, Nix DE, Ballow CH, Goss TF, Birmingham MC, Schentag JJ. Pharmacodynamics of intravenous ciprofloxacin in seriously ill patients. Antimicrob Agents Chemother. 1993;37(5):1073–1081. doi: 10.1128/aac.37.5.1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Ambrose PG, Grasela DM, Grasela TH, Passarell J, Mayer HB, Pierce PF. Pharmacodynamics of fluoroquinolones against Streptococcus pneumoniae in patients with community-acquired respiratory tract infections. Antimicrob Agents Chemother. 2001;45(10):2793–2797. doi: 10.1128/AAC.45.10.2793-2797.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Drusano GL, Preston SL, Fowler C, Corrado M, Weisinger B, Kahn J. Relationship between fluoroquinolone area under the curve: minimum inhibitory concentration ratio and the probability of eradication of the infecting pathogen, in patients with nosocomial pneumonia. J Infect Dis. 2004;189(9):1590–1597. doi: 10.1086/383320. [DOI] [PubMed] [Google Scholar]
- 175.Zelenitsky SA, Ariano RE. Support for higher ciprofloxacin AUC24/MIC targets in treating Enterobacteriaceae bloodstream infection. J Antimicrob Chemother. 2010;65(8):1725–1732. doi: 10.1093/jac/dkq211. [DOI] [PubMed] [Google Scholar]
- 176.Nicolau DP, Freeman CD, Belliveau PP, Nightingale CH, Ross JW, Quintiliani R. Experience with a once-daily aminoglycoside program administered to 2,184 adult patients. Antimicrob Agents Chemother. 1995;39(3):650–655. doi: 10.1128/AAC.39.3.650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Rybak MJ, Abate BJ, Kang SL, et al. Prospective evaluation of the effect of an aminoglycoside dosing regimen on rates of observed nephrotoxicity and ototoxicity. Antimicrob Agents Chemother. 1999;43(7):1549–1555. doi: 10.1128/aac.43.7.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Eliopoulos GM, Drusano GL, Ambrose PG, et al. Back to the future: using aminoglycosides again and how to dose them optimally. Clin Infect Dis. 2007;45(6):753–760. doi: 10.1086/520991. [DOI] [PubMed] [Google Scholar]
- 179.Moore RD, Lietman PS, Smith CR. Clinical response to aminoglycoside therapy: importance of the ratio of peak concentration to minimal inhibitory concentration. J Infect Dis. 1987;155(1):93–99. doi: 10.1093/infdis/155.1.93. [DOI] [PubMed] [Google Scholar]
- 180.Kashuba ADM, Nafziger AN, Drusano GL, Bertino JS. Optimizing aminoglycoside therapy for nosocomial pneumonia caused by gram-negative bacteria. Antimicrob Agents Chemother. 1999;43(3):623–629. doi: 10.1128/aac.43.3.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Pajot O, Burdet C, Couffignal C, et al. Impact of imipenem and amikacin pharmacokinetic/pharmacodynamic parameters on microbiological outcome of Gram-negative bacilli ventilator-associated pneumonia. J Antimicrob Chemother. 2014;70(5):1487–1494. doi: 10.1093/jac/dku569. [DOI] [PubMed] [Google Scholar]
- 182.Preston SL, Drusano GL, Berman a L, et al. Pharmacodynamics of levofloxacin: a new paradigm for early clinical trials. JAMA. 1998;279(2):125–129. doi: 10.1001/jama.279.2.125. [DOI] [PubMed] [Google Scholar]
- 183.Zelenitsky SA, Harding GKM, Sun S, Ubhi K, Ariano RE. Treatment and outcome of Pseudomonas aeruginosa bacteraemia: an antibiotic pharmacodynamic analysis. J Antimicrob Chemother. 2003;52(4):668–674. doi: 10.1093/jac/dkg403. [DOI] [PubMed] [Google Scholar]
- 184.Drusano GL, Johnson DE, Rosen M, Standiford HC. Pharmacodynamics of a fluoroquinolone antimicrobial agent in a neutropenic rat model of Pseudomonas sepsis. Antimicrob Agents Chemother. 1993;37(3):483–490. doi: 10.1128/aac.37.3.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Rees VE, Bulitta JB, Nation RL, Tsuji BT, Sörgel F, Landersdorfer CB. Shape does matter: short high-concentration exposure minimizes resistance emergence for fluoroquinolones in Pseudomonas aeruginosa. J Antimicrob Chemother. 2015;70(3):818–826. doi: 10.1093/jac/dku437. [DOI] [PubMed] [Google Scholar]
- 186.Eagle H, Musselman AD. The slow recovery of bacteria from the toxic effects of penicillin. J Bacteriol. 1949;58:475–490. doi: 10.1128/jb.58.4.475-490.1949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Vogelman B, Gudmundsson S, Turnidge J, Leggett J, Craig WA. In vivo postantibiotic effect in a thigh infection in neutropenic mice. J Infect Dis. 1988;157(2):287–298. doi: 10.1093/infdis/157.2.287. [DOI] [PubMed] [Google Scholar]
- 188.Craig WA. The postantibiotic effect. Clin Microbiol Newsl. 1991;13(16):121–124. [Google Scholar]
- 189.Bustamante CI, Drusano GL, Tatem BA, Standiford HC. Postantibiotic effect of imipenem on Pseudomonas aeruginosa. Antimicrob Agents Chemother. 1984;26(5):678–682. doi: 10.1128/aac.26.5.678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Nadler HL, Pitkin DH, Sheikh W. The postantibiotic effect of meropenem and imipenem on selected bacteria. J Antimicrob Chemother. 1989;24(Suppl A):225–231. doi: 10.1093/jac/24.suppl_a.225. [DOI] [PubMed] [Google Scholar]
- 191.Hanberger H, Svensson E, Nilsson M. Control-related effective regrowth time and post-antibiotic effect of meropenem on Gram-negative bacteria studied by bioluminescence and viable counts. J Antimicrob Chemother. 1995:585–592. doi: 10.1093/jac/35.5.585. [DOI] [PubMed] [Google Scholar]
- 192.Nielsen EI, Friberg LE. Pharmacokinetic-pharmacodynamic modeling of antibacterial drugs. Pharmacol Rev. 2013;65(3):1053–1090. doi: 10.1124/pr.111.005769. [DOI] [PubMed] [Google Scholar]
- 193.Bulitta JB, Landersdorfer CB, Forrest A, et al. Relevance of pharmacokinetic and pharmacodynamic modeling to clinical care of critically ill patients. Curr Pharm Biotechnol. 2011;12:2044–2061. doi: 10.2174/138920111798808428. [DOI] [PubMed] [Google Scholar]
- 194.Nielsen EI, Cars O, Friberg LE. Pharmacokinetic/pharmacodynamic (PK/PD) indices of antibiotics predicted by a semimechanistic PKPD model: a step toward model-based dose optimization. Antimicrob Agents Chemother. 2011;55(10):4619–4630. doi: 10.1128/AAC.00182-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Ambrose PG, Grasela DM. The use of Monte Carlo simulation to examine pharmacodynamic variance of drugs: fluoroquinolone pharmacodynamics against Streptococcus pneumoniae. Diagn Microbiol Infect Dis. 2000;38(3):151–157. doi: 10.1016/s0732-8893(00)00185-1. [DOI] [PubMed] [Google Scholar]
- 196.Kuti JL, Dandekar PK, Nightingale CH, Nicolau DP. Use of Monte Carlo simulation to design an optimized pharmacodynamic dosing strategy for meropenem. J Clin Pharmacol. 2003;43(10):1116–1123. doi: 10.1177/0091270003257225. [DOI] [PubMed] [Google Scholar]
- 197.Tam V, McKinnon P. Pharmacokinetics and pharmacodynamics of cefepime in patients with various degrees of renal function. Antimicrob Agents Chemother. 2003;47(6):1853–1861. doi: 10.1128/AAC.47.6.1853-1861.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Lodise TP, Lomaestro B, Rodvold KA, Danziger LH, Drusano GL. Pharmacodynamic profiling of piperacillin in the presence of tazobactam in patients through the use of population pharmacokinetic models and Monte Carlo simulation. Antimicrob Agents Chemother. 2004;48(12):4718–4724. doi: 10.1128/AAC.48.12.4718-4724.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Zelenitsky S, Ariano R, Harding G, Forrest A. Evaluating ciprofloxacin dosing for Pseudomonas aeruginosa infection by using clinical outcome-based Monte Carlo simulations. Antimicrob Agents Chemother. 2005;49(10):4009–4014. doi: 10.1128/AAC.49.10.4009-4014.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Del Mar Fernandez De Gatta Garcia M, Revilla N, Calvo MV, Domínguez-Gil A, Sánchez Navarro A. Pharmacokinetic/pharmacodynamic analysis of vancomycin in ICU patients. Intensive Care Med. 2007;33(2):279–285. doi: 10.1007/s00134-006-0470-5. [DOI] [PubMed] [Google Scholar]
- 201.Rea RS, Capitano B, Bies R, Bigos KL, Smith R, Lee H. Suboptimal aminoglycoside dosing in critically ill patients. Ther Drug Monit. 2008;30(6):674–681. doi: 10.1097/FTD.0b013e31818b6b2f. [DOI] [PubMed] [Google Scholar]
- 202.Samtani MN, Flamm R, Kaniga K, Nandy P. Pharmacokinetic-pharmacodynamic-model-guided doripenem dosing in critically ill patients. Antimicrob Agents Chemother. 2010;54(6):2360–2364. doi: 10.1128/AAC.01843-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Van Wart SA, Ambrose PG, Rubino CM, et al. Pharmacokinetic-pharmacodynamic target attainment analyses to evaluate in vitro susceptibility test interpretive criteria for ceftaroline against Staphylococcus aureus and Streptococcus pneumoniae. Antimicrob Agents Chemother. 2014;58(2):885–891. doi: 10.1128/AAC.01680-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Xiao AJ, Miller BW, Huntington JA, Nicolau DP. Ceftolozane/tazobactam pharmacokinetic/pharmacodynamic derived dose justification for phase 3 studies in patients with nosocomial pneumonia. J Clin Pharmacol. 2016;56(1):56–66. doi: 10.1002/jcph.566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Jumbe N, Louie A, Leary R, et al. Application of a mathematical model to prevent in vivo amplification of antibiotic-resistant bacterial populations during therapy. J Clin Invest. 2003;112(2):275–285. doi: 10.1172/JCI16814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Drusano GL, Bonomo RA, Bahniuk N, et al. Resistance emergence mechanism and mechanism of resistance suppression by tobramycin for cefepime for Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2012;56(1):231–242. doi: 10.1128/AAC.05252-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Ambrose PG, Bhavnani SM, Jones RN. Pharmacokinetics-pharmacodynamics of cefepime and piperacillin-tazobactam against Escherichia coli and Klebsiella pneumoniae strains producing extended-spectrum β-lactamases: report from the ARREST program. Antimicrob Agents Chemother. 2003;47(5):1643–1646. doi: 10.1128/AAC.47.5.1643-1646.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Vourli S, Tsala M, Kotsakis S, et al. Comparison of short versus prolonged infusion of standard dose of meropenem against carbapenemase-producing Klebsiella pneumoniae isolates in different patient groups: a pharmacokinetic-pharmacodynamic approach. J Pharm Sci. 2016;105(4):1513–1518. doi: 10.1016/j.xphs.2016.02.008. [DOI] [PubMed] [Google Scholar]