Abstract
Objective
To determine the preferred regimen for women with adenomyosis undergoing in vitro fertilization (IVF), we compared the IVF outcomes of fresh embryo transfer (ET) cycles with or without gonadotropin-releasing hormone (GnRH) agonist pretreatment and of frozen-thawed embryo transfer (FET) cycles following GnRH agonist treatment.
Methods
This retrospective study included 241 IVF cycles of women with adenomyosis from January 2006 to January 2012. Fresh ET cycles without (147 cycles, group A) or with (105 cycles, group B) GnRH agonist pretreatment, and FET cycles following GnRH agonist treatment (43 cycles, group C) were compared. Adenomyosis was identified by using transvaginal ultrasound at the initial workup and classified into focal and diffuse types. The IVF outcomes were also subanalyzed according to the adenomyotic region.
Results
GnRH agonist pretreatment increased the stimulation duration (11.5±2.1 days vs. 9.9±2.0 days) and total dose of gonadotropin (3,421±1,141 IU vs. 2,588±1,192 IU), which resulted in a significantly higher number of retrieved oocytes (10.0±8.2 vs. 7.9±6.8, p=0.013) in group B than in group A. Controlled ovarian stimulation for freezing resulted in a significantly higher number of retrieved oocytes (14.3±9.2 vs. 10.0±8.2, p=0.022) with a lower dose of gonadotropin (2,974±1,112 IU vs. 3,421±1,141 IU, p=0.037) in group C than in group B. The clinical pregnancy rate in group C (39.5%) tended to be higher than those in groups B (30.5%) and A (25.2%) but without a significant difference.
Conclusion
FET following GnRH agonist pretreatment tended to increase the pregnancy rate in patients with adenomyosis. Further large-scale prospective studies are required to confirm this result.
Keywords: Adenomyosis, Embryo transfer, Gonadotorpin-releasing hormone, In vitro fertilization
Introduction
Adenomyosis is a benign gynecological disease in which the endometrial stroma invades the uterine myometrium. The common symptom triad of adenomyosis is dysmenorrhea, abnormal uterine bleeding, and an enlarged and tender uterus. However, adenomyosis is a less common but increasingly observed in infertile patients undergoing in vitro fertilization (IVF).
Adenomyosis is associated with several conditions that could interfere with natural conception [1,2,3]. Early miscarriage rates are doubled in oocyte recipients with adenomyosis, resulting in lower live birth rates; this finding suggests that the initial stages of embryo invasion and placentation may be disrupted [4].
Considerable efforts have been made to improve IVF outcomes in women with adenomyosis. Women wishing to preserve their fertility; surgical treatment a difficult option to consider. Achieving a balance between complete removal of adenomyosis and preservation of the normal uterine contour for pregnancy is difficult. Another important issue that should be considered is the high risk of uterine rupture during pregnancy or labor after surgical treatment. Therefore, medical treatment with a gonadotropin-releasing hormone (GnRH) agonist is preferred. Several studies have shown that administration of a GnRH agonist before IVF cycles significantly increases the chances of pregnancy in infertile women with adenomyosis [5,6,7].
Various cycle regimens, including frozen-thawed embryo transfer (FET) combined with a GnRH agonist, are used worldwide for infertile women with adenomyosis undergoing IVF. Cycle regimens can be classified into fresh ET, fresh ET with GnRH agonist pretreatment (or long term down regulation protocol), and FET following GnRH agonist pretreatment. However, insufficient evidence is available to support the preference for any particular regimen over another.
Adenomyosis is an estrogen-responsive disease; thus, the three regimens are expected to have different potentials for a successful pregnancy. We hypothesize that GnRH agonist pretreatment before IVF has a beneficial effect on implantation, and that its effect is more potent in FET, as it is in the euestrogenic state, than in the fresh ET cycles. This retrospective analysis aimed to compare the outcomes of different IVF regimens and determine the preferred regimen in women with adenomyosis undergoing IVF.
Methods
1. Study population
The retrospective study included a total 295 cycles of 241 infertile women with adenomyosis from January 2006 to January 2012. Infertile women included in this study have nonspecific infertile factors based on infertility work up except adenomyosis.
All the patients were undertaken transvaginal ultrasound at initial visit, and assessed for the presence of adenomyosis. Adenomyosis was diagnosed according to the following criteria: (1) subjective enlargement of uterine corpus, (2) asymmetrically thickened myometrium between anterior and posterior walls, (3) heterogeneity of myometrium/hypoechoic striations, (4) poor definition of endometrio-myometrial junction.
The study group was divided into three groups according to IVF strategy; fresh ET cycles, fresh ET cycles with GnRH agonist pretreatment and FET cycles following GnRH agonist treatment. Group A was fresh ET without GnRH agonist pretreatment (147 cycles of 116 women), group B was fresh ET with GnRH agonist pretreatment (105 cycles of 87 women), and group C was FET following GnRH agonist treatment (43 cycle of 38 women).
IVF outcomes, such as number of retrieved oocytes, oocyte maturation rate, fertilization rate, clinical pregnancy rate (CPR), miscarriage rate were compared between groups.
2. Controlled ovarian stimulation
Controlled ovarian stimulation (COS) using flexible GnRH antagonist protocol was performed. Ovarian stimulation began on menstrual cycle day 2 with daily injections of 225 or 300 IU of recombinant follicle stimulating hormone (rFSH; Gonal-F, Merck Serono, Mississauga, ON, Canada; Puregon, Organon Espan, Barcelona, Spain). The starting dose of rFSH was determined based on patient's age, weight and ovarian reserve testing. Gonadotropin doses were adjusted according to ovarian response as noted follicular number by transvaginal ultrasound and serum estradiol level. Highly purified human menopausal gonadotrophin (Menopur, Ferring Pharmaceuticals, Geneva, Switzerland) was used if a poor response was anticipated. GnRH antagonist daily dose of 0.25 mg (Cetrorelix acetated, Cetrotide, Merck Serono) was initiated based on a flexible protocol, once a follicle reached ≥12 mm in diameter and was continued until the day of human chorionic gonadotropin (hCG) administration. Two hundred fifty to 500 µg of recombinant hCG (choriogonadotropin-α, Ovidrel, Merck Serono) was administered when at least three follicles measured ≥18 mm. Oocyte retrieval was performed 36 hours later. ET was performed 3 days after oocyte retrieval. The number of embryos transferred depended on embryo quality and patient age. Luteal support consisted of progesterone in oil (50 mg IM, Taiyu Progesterone, Taiyu Chemical & Pharm, Taiwan) daily starting the day after oocyte retrieval until serum pregnancy test.
3. GnRH agonist treatment
GnRH agonist treatment was performed for 2 or 3 month using 3.75 mg of goserelin (Zoladex, Astrazeneca, Macclesfield, UK; Decapeptyl, Ferring, Kiel, Germany) per month.
4. Endomertial preparation in FET
For FET cycles estradiol valerate of 6 mg (Progynova, Schering-plough, Whitehouse Station, NJ, USA) were orally administered 4 weeks after the last GnRH agonist injection and continuded to the initial pregnancy test. Progesterone in oil (50 mg IM, Taiyu Progesteron, Taiyu Chemical & Pharm) was started about 2 weeks after estradiol valerate administration until serum pregnancy test, and progesterone injection was continued until 7 weeks gestation if pregnancy was positive on serum pregnancy test.
Pregnancy was determined by a serial serum β-hCG level of >5 mIU/mL at 12 days after the oocyte retrieval in fresh ET cycles or 12 days after progesterone injection in FET cycrles. Clinical pregnancy was defined as the presence of a G-sac by ultrasonography at approximately 5 weeks of pregnancy.
5. Statistical analysis
All analyses were performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). One-way analysis of variance was used for statistical analysis. Each variable is presented as the mean±standard deviation. A p<0.05 was considered statistically significant. Clinical variables such as age and body mass index were compared using one-way analysis of variance. Fisher's least significant difference post hoc test was used to determine significant differences between groups.
Results
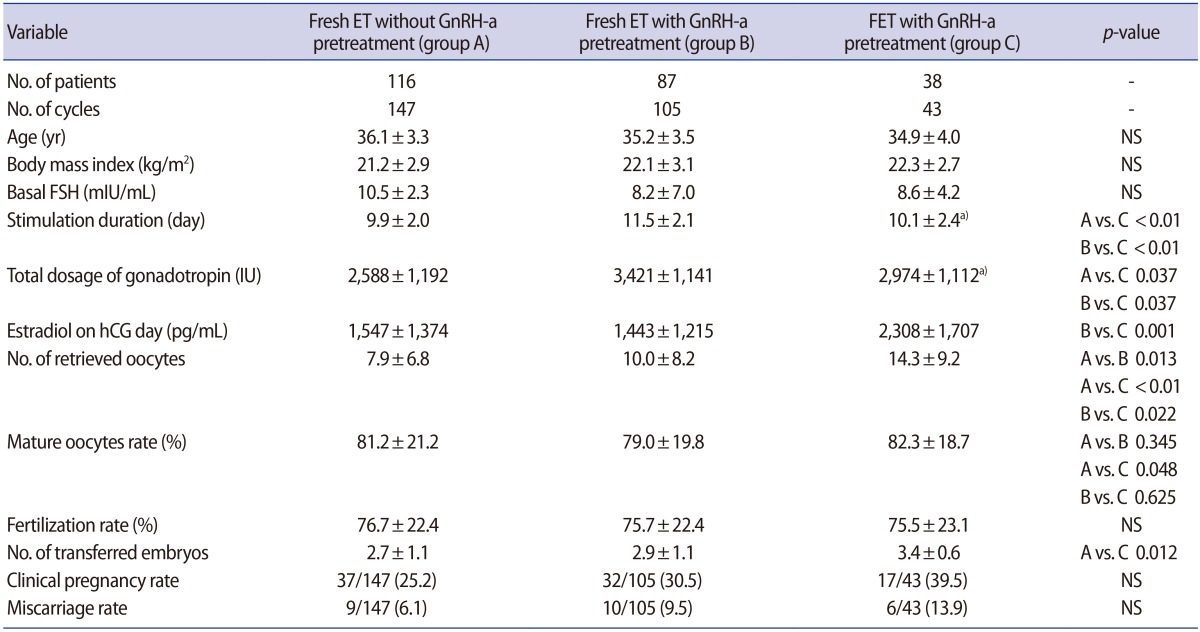
The age, body mass index, and basal FSH levels were not different among the three groups (Table 1). GnRH agonist pretreatment increased the stimulation duration (11.5±2.1 days vs. 9.9±2.0 days) and the total dose of gonadotropin (3,421±1,141 IU vs. 2,588±1,192 IU), which resulted in a significantly higher number of retrieved oocytes (10.0±8.2 vs. 7.9±6.8, p=0.013) in group B than in group A. No difference was observed in the proportion of mature oocytes and the fertilization rate. The CPR also showed no difference between groups A and B.
Table 1. Comparison of IVF outcomes among three different regimen.
NSValues are presented as mean±standard deviation or number (%).
IVF, in vitro fertilization; ET, embryo transfer; GnRH-a, gonadotropin-releasing hormone agonist; FET, frozen-thawed embryo transfer cycle; NS, not significant; FSH, follicle stimulating hormone; hCG, human chorionic gonadotropin.
a)Controlled ovarian stimulation cycle for freezing.
COS for freezing resulted in a significantly higher number of retrieved oocytes (14.3±9.2 vs. 10.0±8.2, p=0.022) with a lower dose of gonadotropin (2,974±1,112 IU vs. 3,421±1,141 IU, p=0.037) in group C than in group B. The CPR in FET following GnRH agonist treatment (group C, 39.5%) was 10% higher than that in fresh ET (group B, 30.5%), but without a significant difference. The CPR in group C was 15% higher than that in group A; however, the difference was not statistically significant.
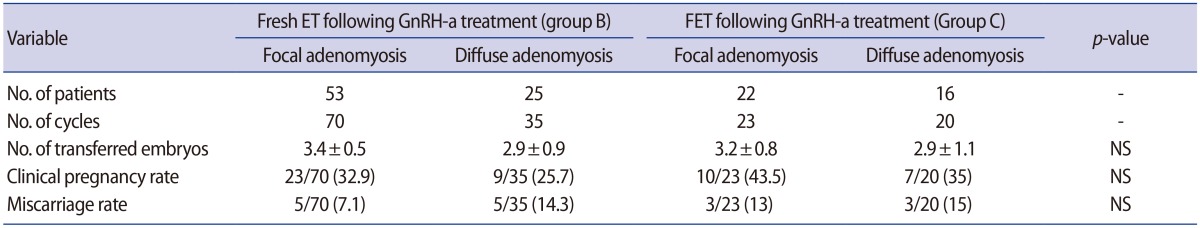
In the subanalyses of groups B and C according to the adenomyotic region, a higher CPR was observed in focal adenomyosis (32.9% and 43.5%) than in diffuse adenomyosis (25.7% and 35%); however, the difference was not significant. Group C showed a higher CPR for both the focal (43.5% vs. 32.9%) and diffuse (35.0% vs. 25.7%) types than did group B, but it was not significantly different (Table 2).
Table 2. Comparison of IVF outcomes according to adenomyotic region.
NSValues are presented as mean±standard deviation or number (%).
IVF, in vitro fertilization; ET, embryo transfer; FET, frozen-thawed embryo transfer; GnRH-a, gonadotropin-releasing hormone agonist; FET, frozen-thawed embryo transfer; NS, not significant.
Discussion
Adenomyosis is histologically defined as the presence of ectopic endometrial islets deep in the myometrium surrounded by a reactive hypertrophic myometrium [8]. Although the effect of adenomyosis on fertility has not been thoroughly investigated, a recent systematic review and meta-analysis concluded that adenomyosis seems to have a negative impact on the outcomes of assisted reproductive techniques, with a pooled relative risk of clinical pregnancy of 0.72 (95% confidence interval [CI], 0.55–0.95) and a pooled risk of miscarriage of 2.12 (95% CI, 1.20–3.75) in women with adenomyosis compared to that in controls [9].
Adenomyosis is associated with several conditions that can interfere with normal implantation; disruption of myometrial architecture and function causes an altered uterine peristaltic activity that can interfere with sperm transport and implantation [1]. Studies have shown an overexpression of aromatase P450; a decrease of integrin β3, osteopontin, and leukemia-inhibiting factor; and an impairment of HOXA-10 gene function during the implantation window. These changes suggest an impaired receptivity and blastocyst-endometrium interaction in women with adenomyosis [2,3,10,11,12].
Given that the GnRH receptor is found in adenomyotic lesions, GnRH agonists are used for medical treatment and exert a direct antiproliferative action within the myometrium. GnRH agonists can markedly reduce the inflammatory reaction and angiogenesis, as well as significantly induce apoptosis in tissues derived from adenomyosis [13]. In addition to its direct antiproliferative effect within the myometrium, a hypoestrogenic effect may be involved in the regression of these reproductive diseases. The expression of the estrogen receptor is more intense in the adenomyotic endometrium than in the eutopic endometrium, and GnRH agonists transiently suppress the hypothalamus–pituitary–ovarian axis and induce a hypoestrogenic effect. This hypoestrogenic effect reduces uterine size and relieves symptoms.
Several case studies have reported successful pregnancies and live births following GnRH agonist treatment in infertile women with adenomyosis [14,15,16]. However, we found no difference between the presence (105 cycles) and absence (147 cycles) of GnRH agonist pretreatment in a large number of fresh ET cycles, indicating that GnRH agonist pretreatment has no benefit in improving IVF outcomes. The hyperestrogenic state resulting from subsequent COS is postulated to diminish the effect of GnRH agonist pretreatment.
We found that FET following GnRH agonist treatment has better potential for a successful pregnancy. Fresh ET with and without GnRH agonist pretreatment both demonstrated no superiority to the FET cycles. After GnRH agonist pretreatment, we postulate that the higher CPR in FET than that in fresh ET is an evidence of improved endometrial receptivity considering the similar average number of transferred embryos.
After GnRH agonist treatment, concerns have been raised on the estrogenic state following COS. The increase in estrogen during COS, resulting in a hyperestrogenic state on hCG administration, can negatively affect the IVF outcome compared with euestrogenic state during hormonal treatment for endometrial preparation in FET cycles. Reduced serum estrogen concentrations in patients undergoing hormonal treatment resulted in a higher CPR, suggesting that euestrogenic concentrations of estradiol may act on the endometrium and provide a better environment for implantation.
The expression of implantation markers, such as integrin β3 subunit and leukemia inhibitory factor, was significantly reduced in the presence of supraphysiologic estrogen concentrations [17,18]. COS may alter the physiologic concentrations of endogenous hormones, resulting in negative effects on the endometrium. Therefore, patients with euestrogenic concentrations may achieve better results than those in a hyperestrogenic state. Given that adenomyosis has not been completely treated after GnRH agonist treatment, an adenomyosis response to high estradiol levels is plausible. A hyperestrogenic state stimulates the adenomyotic region, resulting in anatomic and functional deterioration.
COS after GnRH agonist treatment (group B) required a higher dose of exogenous gonadotropin to overcome GnRH agonist-induced downregulation and prolonged stimulation duration. FET following GnRH agonist treatment (group C) has a benefit in terms of the lower dose of gonadotropin and the shorter duration of injection in COS for freezing cycles, with a higher CPR in subsequent FET cycles.
We categorized adenomyosis into either the diffuse or focal type. In FET cycles following GnRH agonist pretreatment (group C), the CPR was higher in the focal adenomyosis group. As expected, the diffuse type negatively affected the embryo implantation, and the extent of adenomyosis could be considered as a factor negatively affecting implantation. This can be explained by the higher concentration of ectopic endometrial glands in focal adenomyosis, which may be related to the increased hormonal responsiveness [19]. Therefore, focal adenomyosis is theoretically likely to be the most therapeutically responsive subtype following GnRH agonist treatment.
The limitations of this retrospective study are as follows. Patient selection bias may be present because the diagnosis was made by using ultrasound. However, this may not be a significant issue. Although the diagnosis of adenomyosis could be made only retrospectively based on the histological analysis of the uterus after hysterectomy, ultrasound is readily available in infertility clinics and the first imaging study performed at the initial visit. Nevertheless, to the best of our knowledge, our present study is the first to report the pregnancy rates between fresh and FET cycles in women with adenomyosis.
In conclusion, the present study found that FET combined with GnRH agonist pretreatment tended to increase the pregnancy rate in patients with adenomyosis. Further large, well-designed prospective cohort studies are necessary to confirm this finding.
Footnotes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Campo S, Campo V, Benagiano G. Infertility and adenomyosis. Obstet Gynecol Int. 2012;2012:786132. doi: 10.1155/2012/786132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xiao Y, Li T, Xia E, Yang X, Sun X, Zhou Y. Expression of integrin β3 and osteopontin in the eutopic endometrium of adenomyosis during the implantation window. Eur J Obstet Gynecol Reprod Biol. 2013;170:419–422. doi: 10.1016/j.ejogrb.2013.05.007. [DOI] [PubMed] [Google Scholar]
- 3.Fischer CP, Kayisili U, Taylor HS. HOXA10 expression is decreased in endometrium of women with adenomyosis. Fertil Steril. 2011;95:1133–1136. doi: 10.1016/j.fertnstert.2010.09.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Martinez-Conejero JA, Morgan M, Montesinos M, Fortuno S, Meseguer M, Simon C, et al. Adenomyosis does not affect implantation, but is associated with miscarriage in patients undergoing oocyte donation. Fertil Steril. 2011;96:943–950. doi: 10.1016/j.fertnstert.2011.07.1088. [DOI] [PubMed] [Google Scholar]
- 5.Mijatovic V, Florijn E, Halim N, Schats R, Hompes P. Adenomyosis has no adverse effects on IVF/ICSI outcomes in women with endometriosis treated with long-term pituitary down-regulation before IVF/ICSI. Eur J Obstet Gynecol Reprod Biol. 2010;151:62–65. doi: 10.1016/j.ejogrb.2010.02.047. [DOI] [PubMed] [Google Scholar]
- 6.Costello MF, Lindsay K, McNally G. The effect of adenomyosis on in vitro fertilisation and intra-cytoplasmic sperm injection treatment outcome. Eur J Obstet Gynecol Reprod Biol. 2011;158:229–234. doi: 10.1016/j.ejogrb.2011.04.030. [DOI] [PubMed] [Google Scholar]
- 7.Niu Z, Chen Q, Sun Y, Feng Y. Long-term pituitary downregulation before frozen embryo transfer could improve pregnancy outcomes in women with adenomyosis. Gynecol Endocrinol. 2013;29:1026–1030. doi: 10.3109/09513590.2013.824960. [DOI] [PubMed] [Google Scholar]
- 8.Bergeron C, Amant F, Ferenczy A. Pathology and physiopathology of adenomyosis. Best Pract Res Clin Obstet Gynaecol. 2006;20:511–521. doi: 10.1016/j.bpobgyn.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 9.Vercellini P, Consonni D, Dridi D, Bracco B, Frattaruolo MP, Somigliana E. Uterine adenomyosis and in vitro fertilization outcome: a systematic review and meta-analysis. Hum Reprod. 2014;29:964–977. doi: 10.1093/humrep/deu041. [DOI] [PubMed] [Google Scholar]
- 10.Kitawaki J, Noguchi T, Amatsu T, Maeda K, Tsukamoto K, Yamamoto T, et al. Expression of aromatase cytochrome P450 protein and messenger ribonucleic acid in human endometriotic and adenomyotic tissues but not in normal endometrium. Biol Reprod. 1997;57:514–519. doi: 10.1095/biolreprod57.3.514. [DOI] [PubMed] [Google Scholar]
- 11.Brosens J, Verhoeven H, Campo R, Gianaroli L, Gordts S, Hazekamp J, et al. High endometrial aromatase P450 mRNA expression is associated with poor IVF outcome. Hum Reprod. 2004;19:352–356. doi: 10.1093/humrep/deh075. [DOI] [PubMed] [Google Scholar]
- 12.Xiao Y, Sun X, Yang X, Zhang J, Xue Q, Cai B, et al. Leukemia inhibitory factor is dysregulated in the endometrium and uterine flushing fluid of patients with adenomyosis during implantation window. Fertil Steril. 2010;94:85–89. doi: 10.1016/j.fertnstert.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 13.Khan KN, Kitajima M, Hiraki K, Fujishita A, Sekine I, Ishimaru T, et al. Changes in tissue inflammation, angiogenesis and apoptosis in endometriosis, adenomyosis and uterine myoma after GnRH agonist therapy. Hum Reprod. 2010;25:642–653. doi: 10.1093/humrep/dep437. [DOI] [PubMed] [Google Scholar]
- 14.Huang FJ, Kung FT, Chang SY, Hsu TY. Effects of short-course buserelin therapy on adenomyosis: a report of two cases. J Reprod Med. 1999;44:741–744. [PubMed] [Google Scholar]
- 15.Lin J, Sun C, Zheng H. Gonadotropin-releasing hormone agonists and laparoscopy in the treatment of adenomyosis with infertility. Chin Med J (Engl) 2000;113:442–445. [PubMed] [Google Scholar]
- 16.Silva PD, Perkins HE, Schauberger CW. Live birth after treatment of severe adenomyosis with a gonadotropin-releasing hormone agonist. Fertil Steril. 1994;61:171–172. doi: 10.1016/s0015-0282(16)56471-1. [DOI] [PubMed] [Google Scholar]
- 17.Ma WG, Song H, Das SK, Paria BC, Dey SK. Estrogen is a critical determinant that specifies the duration of the window of uterine receptivity for implantation. Proc Natl Acad Sci U S A. 2003;100:2963–2968. doi: 10.1073/pnas.0530162100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen QJ, Sun XX, Li L, Gao XH, Gemzell-Danielsson K, Cheng LN. Effects of ovarian stimulation on endometrial integrin beta3 and leukemia inhibitory factor expression in the peri-implantation phase. Fertil Steril. 2008;89(5 Suppl):1357–1363. doi: 10.1016/j.fertnstert.2007.03.073. [DOI] [PubMed] [Google Scholar]
- 19.Togashi K, Ozasa H, Konishi I, Itoh H, Nishimura K, Fujisawa I, et al. Enlarged uterus: differentiation between adenomyosis and leiomyoma with MR imaging. Radiology. 1989;171:531–534. doi: 10.1148/radiology.171.2.2704819. [DOI] [PubMed] [Google Scholar]