Abstract
Objective
To investigate psychological distress and fertility quality of life (FertiQoL) in infertile Korean women, and to investigate whether a correlation exists between psychological distress and FertiQoL.
Methods
Participants in this study were made up of 141 infertile women and 65 fertile women. We conducted a survey on psychological distress (using the Depression Anxiety Stress Scales [DASS]-42 questionnaire) and administered a FertiQoL questionnaire. The levels of stress hormones (adrenocorticotropic hormone [ACTH] and cortisol) in serum were assessed.
Results
The scores for depression (13.7±8.4), anxiety (10.7±6.4), and stress (18.0±8.3) among the infertile women were significantly higher than the scores for depression (9.4±7.5), anxiety (6.6±6.0), and stress (12.2±8.3, p<0.001) among the fertile women. There was no difference in the scores for depression (13.5±8.2, 13.8±8.6), anxiety (10.0±6.2, 11.5±6.6) and stress (17.7±8.4, 18.4±8.1) between younger (≤34) and older (≥35) participants. The mind-body (r =–0.495) and emotional (r =–0.590) subscales showed a higher negative correlation with stress compared with other scales of psychological distress. At the same time, the social (r =–0.537) and relational (r =–0.385) subscales showed a higher negative correlation with depression. Levels of cortisol and ACTH in infertile women were 9.1 µg/mL and 11.9 pg/mL, respectively, which are within normal ranges.
Conclusion
The levels of psychological distress and quality of life in infertile Korean women seem to require psychological intervention. This study provides a baseline measurement of psychological distress and FertiQoL in infertile women in Korea, which will be available for developing psychological interventions for infertile Korean women.
Keywords: Depression Anxiety Stress Scales-42, Fertility quality of life, Psychological distress
Introduction
Infertile patients are subjected to greater stress and emotional tension than their fertile counterparts [1], and infertility is negatively associated with the relational, sexual, and psychosocial well-being of patients [2]. Moreover, merely a diagnosis of infertility and treatment for infertility can result in not only distress or depression [3,4,5], but also a negative impact on the patient's quality of life [6]. Although the few studies that have examined the issue have been unable to confirm a perception that psychological stress may prevent a woman from attaining and maintaining a pregnancy [7,8], several studies have observed that emotional distress or stressful life events are associated with poor clinical outcomes for assisted reproductive technology (ART) programs [9,10,11,12,13,14,15].
Various potential mechanisms have been postulated to connect psychological stress and infertility. Stress triggers the hypothalamic–pituitary–adrenal axis, which upregulates corticotropin-releasing hormone (CRH), adrenocorticotropic hormone (ACTH), and glucocorticoids. An increase in the levels of these stress hormones can interfere with the timing of ovulation, shorten the luteal phase, and lessen the chance of implantation [16]. In addition, lower concentrations of norepinephrine and cortisol in serum and follicular fluid [17] as well as low urinary concentrations of adrenaline and noradrenaline have been found in women who underwent successful treatment [18]. At the same time, concentrations of cortisol or norepinephrine associated with stress may block or delay follicular development and embryo implantation [19], or decrease the percentage of good quality embryos [14], respectively. These findings have emphasized the importance of psychological intervention and counseling for infertile women.
It is well known that the negative effects of infertility on quality of life and emotional distress were stronger for women than for male partners [20,21,22,23]. Surprisingly, anxiety and depression levels in infertile women were equivalent to those found in women with heart disease or cancer, or to those who had been diagnosed as human immunodeficiency virus (HIV)-positive [24]. To reduce the level of psychological distress in women diagnosed with infertility, some countries have laws recommending that counseling be offered as a part of infertility treatment before the initiation of the treatment [25]. It is well known that expressing thoughts and feelings is generally perceived as a simple and valuable means of psychotherapy for reducing psychological stress. Face-to-face counseling is the most widely used intervention; however, face-to-face counseling was not effective in some patients [26]. The recently introduced method of expressive writing intervention (EWI) may be more easily accessible and provoke less resistance in some patients who feel psychologically burdened by face-to-face psychological interventions. In fact, EWI has been shown to be efficient in reducing infertility-related stress in women seeking ART treatment [27].
The abovementioned studies demonstrate the importance and necessity of psychological counseling for the psychological stabilization of infertility patients. In response, we conducted a preliminary study and a first trial for establishing a psychological testing and counseling system for infertile women in Korea. This study aimed to investigate psychological distress and stress hormone levels in the blood, and to investigate the correlation between psychological distress and fertility quality of life (FertiQoL) in infertile Korean women.
Methods
This is a prospective cohort study and the first validation study of the Korean-language FertiQoL questionnaire. This study was approved by the Institutional Review Boards (IRB) of Mizmedi Hospital (Mizmedi-ART IRB 2012-10-02) and Mamapapa & Baby Clinic (Mamapapa IRB 2015-01). This study was carried out from December 2012 to March 2016.
1. Patients
Out of a total of 206 volunteers, 141 infertile women without children and 65 fertile women with children participated in this study. Even though we explained to all infertile patients who visited our IVF centers about our study and tests, it was difficult to obtain volunteers, perhaps due to unfamiliarity with the psychological tests and their potential inconvenience for many infertile women. Therefore, the tests were performed entirely by voluntary decision of infertile patients without any ask to perform the tests, because we did not want to introduce additional stress that might negatively affect clinical outcomes. The group of infertile women consisted of various infertility patients who were at a stage prior to, during, or after their intra uterine insemination or in vitro fertilization (IVF) treatment. At the same time, the group of fertile women consisted of mothers who use a childcare center (a day care center for children from 0 to 4 years old), because they were similar in age to the infertile women, but had children. The child care center is managed by my friend, due to her help we could collect the fertile volunteers. Both groups of women filled out a survey on psychological distress (the Depression Anxiety Stress Scales [DASS]-42 questionnaire). In addition, the group of infertile women completed the FertiQoL questionnaire, either online or on paper. We analyzed the questionnaires and then provided written results and comments by e-mail or in face-to-face counseling according to the preference of the participants.
2. The DASS-42 questionnaire
Participants' level of psychological distress was measured with the DASS-42 questionnaire. DASS is a set of three self-reported scales designed to measure the negative emotional states of depression, anxiety, and stress, and each of the three DASS scales contains 14 items with similar content [28]. The depression scale assesses dysphoria, hopelessness, devaluation of life, self-deprecation, lack of interest or involvement, anhedonia, and inertia. The anxiety scale assesses autonomic arousal, skeletal muscle effects, situational anxiety, and subjective experience of anxious affect. The stress scale assesses difficulty relaxing, nervous arousal, being easily upset or agitated, irritability/over-reactivity, and impatience. Subjects are asked to use a 4-point severity or frequency scale to rate the extent to which they have experienced each state over the past week. Scores for depression, anxiety, and stress are calculated by summing the scores for the relevant items (DASS-42, Psychology Foundation of Australia, 2014, http://www2.psy.unsw.edu.au/dass/) (Appendix 1).
3. FertiQoL questionnaire
Recently, an international group of institutions (the European Society of Human Reproduction and Embryology, the American Society for Reproductive Medicine, and Merck, Geneva, Switzerland) have collaborated to develop the FertiQoL questionnaire, which is condition-specific and aims to measure quality of life in all people experiencing fertility problems [29]. FertiQoL (36 items) consists of 24 items derived from four subscales (mind-body, emotional, social, and relational), 10 treatment-related items, and two overall life and physical wellness items. FertiQoL is a reliable and valid international tool developed to assess the impact of fertility problems and fertility treatment on personal, social, and relational domains of life. FertiQoL was produced in English and has been translated into 20 languages; however, an official Korean translation was not available until recently. In 2012, we produced and submitted a draft Korean-language version of the FertiQoL and asked for approval and registration with the FertiQoL steering committee at Cardiff University in the U.K. After revision, the Korean version of FertiQoL was registered in 2012 and is available from the Cardiff Fertility Research Group (http://www.fertiqol.org) (Appendix 2).
4. Stress hormones: ACTH and cortisol
ACTH is produced in response to biological stress. Its principal effect is the production and release of cortisol by the cortex of the adrenal gland. Blood samples from study participants were collected at 09:00–12:00 in tubes containing ethylenediaminetetraacetic acid during the injection of gonadotropin for IVF; these samples were immediately centrifuged and stored at -80℃ until assayed.
5. Statistical analysis
The values in the tables are presented as mean±standard deviation. Differences between the two groups were analyzed with a two-tailed Student's t-test. The correlation between FertiQoL and DASS-42 scores was explored using Pearson's r. All statistical analyses were performed using SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA). For the statistical procedure performed, a p-value of <0.05 was considered significant.
Sample size calculation was performed with the automatic sample size calculator provided by SurveyMonkey (Palo Alto, CA, USA). The population size was 711, which constituted the total number of infertile women who visited our IVF center for ART treatments for the first time from December 2012 to March 2016. The confidence level and margin of error were determined to be 95% and 5%, respectively. From this survey condition, the optimal sample size was recommended as 249.
Results
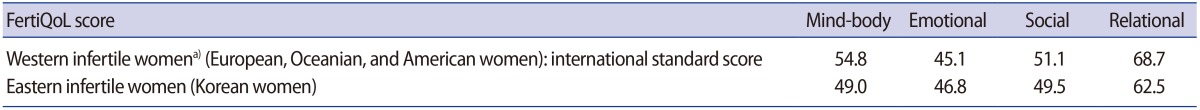
Levels of psychological distress in infertile and fertile women were investigated with DASS-42 (Table 1). There was no difference in age between infertile women (34.3±3.7) and fertile women (35.4±4.6). The scores on the depression (13.7±8.4), anxiety (10.7±6.4), and stress scales (18.0±8.3) in infertile women were significantly higher than the scores (depression, 9.4±7.5; anxiety, 6.6±6.0; stress, 12.2±8.3; p<0.001) in fertile women.
Table 1. Psychological distress levels in Korean infertile and fertile women.
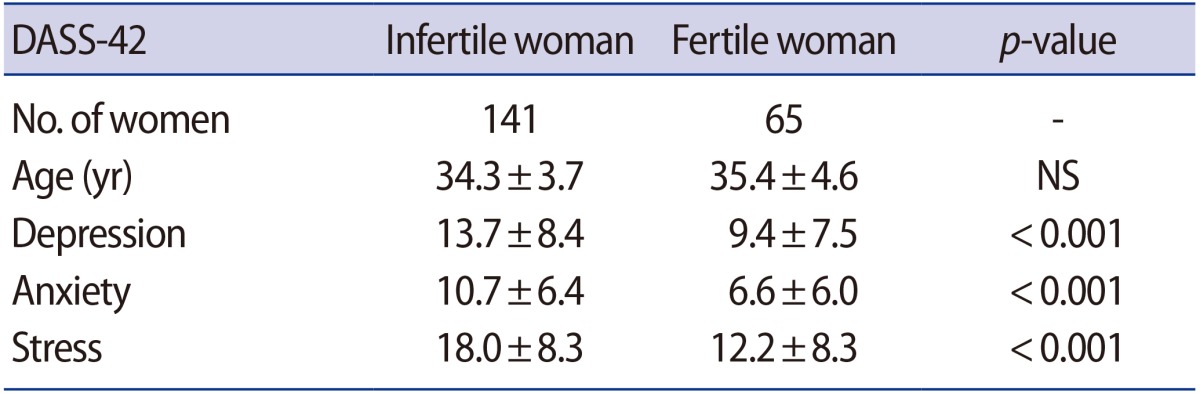
Values are presented as mean±standard deviation.
DASS, Depression Anxiety Stress Scales; NS, not significant.
It is well known that the pregnancy rate gradually decreases with age in women. From the viewpoint of infertile women, increases in age and in the duration of infertility may be a critical factor, increasing the level of psychological distress. To confirm the possibility, we investigated the effects of age and duration of infertility on psychological distress in infertile women (Table 2). The participants with infertility were divided into two groups by age: group 1 (≤34 years old) and group 2 (≥35 years old). Although age (31.4±2.6 years) and duration of infertility (2.8±1.6 years) in group 1 were significantly lower than those (37.4±2.8 and 5.1±4.0 years, p<0.001) in group 2, there was no difference between the two groups in the scores for the depression (13.5±8.2, 13.8±8.6), anxiety (10.0±6.2, 11.5±6.6) and stress scales (17.7±8.4, 18.4±8.1).
Table 2. Effects of patients' age and duration of infertility on psychological distress of infertile women.
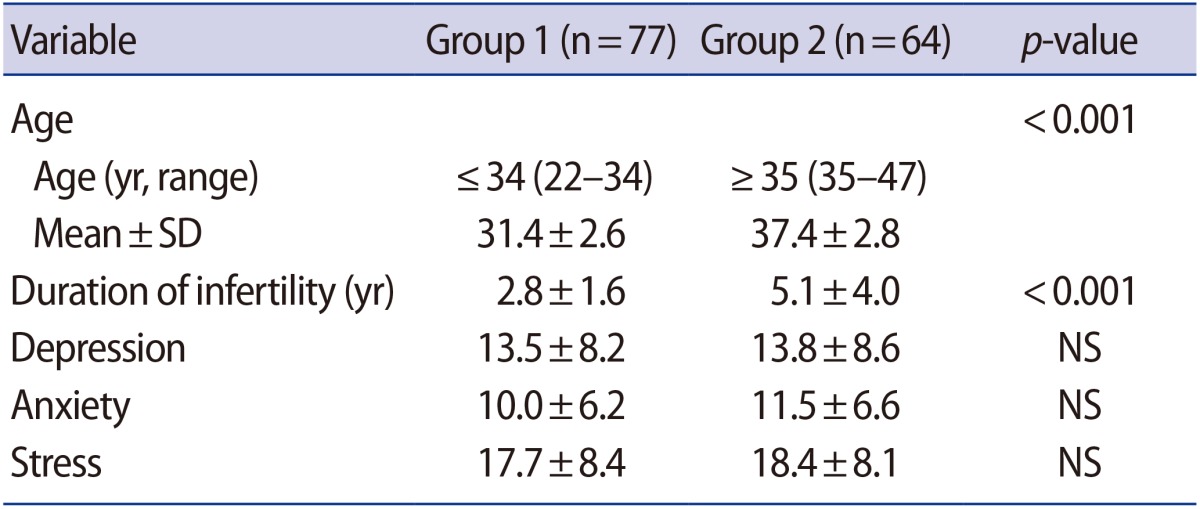
Values are presented as mean±standard deviation unless otherwise indicated.
SD, standard deviation; NS, not significant.
Many studies about FertiQoL have been performed using several translations; however, the present study is the first validation study of the Korean-language FertiQoL. We collected the FertiQoL scores from infertile Korean women, and then compared these with the scores of infertile Western women reported in a previous study (Table 3). Although there was a small difference in the scores on the subscales between Korean and Western infertile women, mind-body (49.0 and 54.8), emotional (46.8 and 45.1), social (49.5 and 51.1), and relational (62.5 and 68.7), respectively, the whole scores were similar to each other.
Table 3. Comparison of FertiQoL scores between Korean and Western infertile women.
FertiQoL, fertility quality of life.
a)Boivin et al. [29]. Ferti-QoL tool; development and general psychometric properties.
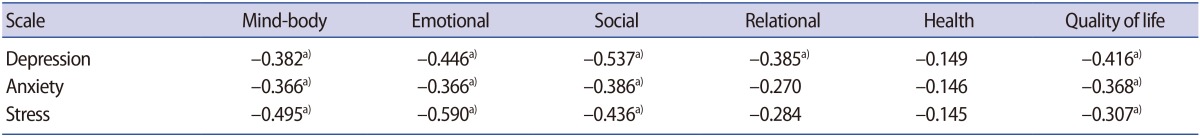
The correlation between level of psychological distress and FertiQoL in Korean infertile women was investigated (Table 4). Mind-body (r=–0.495) and emotional subscales (r=–0.590) showed a higher negative correlation with stress compared with other psychological distress scales. At the same time, social (r=–0.537) and relational subscales (r=–0.385) showed a higher negative correlation with depression compared to other psychological scales. In particular, the relational subscale was significantly correlated with depression alone, but not with the anxiety and stress scales. Psychological distress showed a negative effect on quality of life, but not on the health of infertile women.
Table 4. Correlation between the scores of FertiQoL and DASS-42 in Korean infertile women.
FertiQoL, fertility quality of life; DASS, Depression Anxiety Stress Scales.
a)Correlation is significant at the 0.01 level.
A correlation between the levels of psychological distress and stress hormones in infertile women was investigated (Table 5). Normal ranges of cortisol and ACTH levels assessed in the morning are 6.2 to 19.4 µg/mL and 7.2 to 63.3 pg/mL, respectively. Levels of the hormones in infertile women were 9.1 µg/mL and 10.4 pg/mL, respectively, which are within the normal range. Contrary to our expectation, a negative correlation was observed between the stress hormone levels and the psychological distress levels. ACTH showed a significantly higher correlation with depression (r=–0.622, p=0.008), anxiety (r=–0.718, p=0.001), and stress scales (r=–0.490, p=0.046) compared to the correlation of cortisol with depression (r=–0.386, p=0.126), anxiety (r=–0.357, p=0.159), and stress (r=–0.237, p= 0.360).
Table 5. Correlation between psychological distress and levels of stress hormones in serum of Korean infertile women.
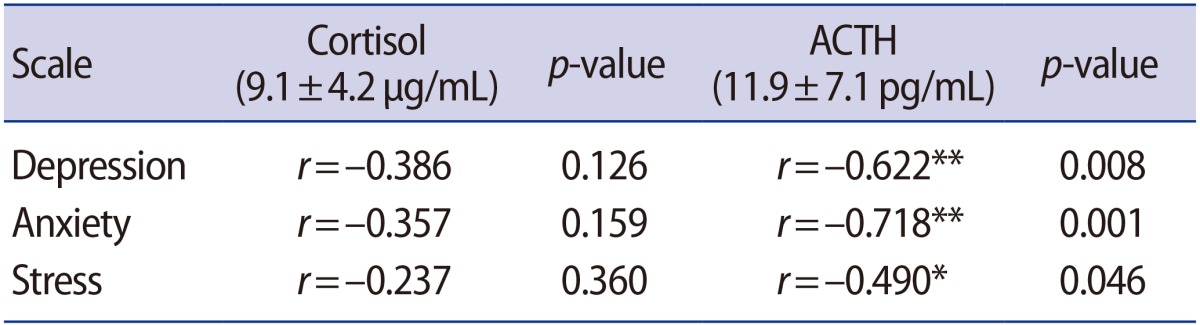
ACTH, adrenocorticotropic hormone. Correlation was significant.
*p<0.05; **p<0.01.
Discussion
We observed that the level of psychological distress in infertile women was significantly higher than the level in fertile women. This result conformed to the result of a previous study [1]. There was a wide difference in the levels of depression and anxiety between infertile and fertile women compared to the differences in stress. This result suggests that it is more difficult to relieve depression and anxiety than stress for infertile women. In general, stress can be relieved by enjoying sports, music, and leisure activities. However, unlike stress, it would be very difficult to reduce the levels of depression and anxiety, unless the causes of depression and anxiety are addressed. Although we do not provide our data about the comparison of psychological distress levels between infertile women and male partners here, we observed that the level in women was nearly twice as high as the level in men. This result is in line with other previous studies [23,30]. Unlike infertile women, the levels of all scales in male partners fell within the normal range, which indicates that women seem to be more affected by infertility compared with their male partners. Moreover, male stress did not contribute to outcomes in infertility treatment, although female stress had a greater effect [12]. We have observed that most counseling and interventions for infertile patients are focused on the female patients rather than the male patients.
It is well known that the pregnancy rate of IVF cycles dramatically decreases after age 38. Therefore, we postulated that older infertile women may be more sensitive to aging compared with younger infertile women. Contrary to our expectation, we did not observe any difference in the levels of psychological distress between younger (≤34) and older (≥35) infertile women. Tiplady et al. [31] also reported a similar result, observing no correlation between age and stress level. These results suggest that a patient's age and duration of infertility is not related to the psychological distress of infertile women. A potential explanation is an enhancement in the ability to cope with infertility in older women, which inhibits an increase in psychological distress levels. This potential explanation is supported by previous reports that overall infertility-related stress declined with age in women [30].
A negative relationship between psychological distress and total mean scores on the FertiQoL questionnaire was found in the present study and other previous study [32]. Mind-body and emotional subscales showed a highly negative correlation with stress, while at the same time, social and relational subscales showed a highly negative correlation with depression. This result is in line with other findings that symptoms of depression were more highly correlated with social, sexual, and relational scales [30]. Notably, the relational subscale was significantly correlated with depression alone, but not with the anxiety and stress scales. This result suggests that satisfaction with the partner is the most important determining factor for the level of depression in infertile women. A similar result was reported showing that anxiety and depression in childless Japanese women were significantly associated with lack of support from the husband and a feeling of stress [33]. Therefore, the role of the male partner is very important for the psychological stability of his wife and, ultimately, for an increase in the pregnancy success rate.
Stress hormones, both cortisol and ACTH levels in infertile women, fell within the normal range. Furthermore, contrary to our expectation, a negative correlation between stress hormone levels and psychological distress levels was observed. This result is opposed to the result of a previous study, which showed a significant positive association between anxiety scores and cortisol levels in the blood [34]. Although further study is needed to identify this discrepancy, it may result from a difference in the endocrine conditions between the female participants. An et al. [34] collected blood from infertile women before the start of IVF treatment. In the present study, in contrast, blood was collected during the gonadotropin-releasing hormone (GnRH) and gonadotropin injections for the IVF cycle. We suggest a hypothesis that a high dose of gonadotropin injection may inhibit the release of stress hormones in infertile women. A reported negative association between stress hormone and GnRH suggests that CRH inhibits hypothalamic GnRH secretion [35].
Infertile Korean women showed a high level of psychological distress and a low level of quality of life, which indicates that infertile women have a marked need for infertility counselling. Psychosocial counseling was effective in reducing anxiety in women undergoing IVF or intracytoplasmic sperm injection for the first time, which resulted in a higher conception rate for the participating women [36]. Matthiesen et al. [27] reported that a reduction in infertility-related stress was observed in the EWI group compared to the control group following intervention in first-time ART patients. EWI is easily accessible and provokes less resistance for some patients who feel a psychological burden with face-to-face counseling. For example, there is general discomfort when talking about sexual behavior during counseling. We conducted a survey with the DASS-42 and FertiQoL questionnaires, administered either online or on paper. We analyzed the questionnaires and then provided the resulting scores of the questionnaires with written advice by e-mail or in face-to-face counseling according to the preference of the participants. Most infertile patients who underwent previous IVF failure wanted face-to-face counseling, but first-time patients seemed hesitant about counseling. Therefore, we suggest that the EWI method may be a feasible intervention as a substitute for face-to-face counseling for first-time ART patients. The development of psychological counseling or intervention to reduce psychological distress and improve coping for infertile women is important not only to reduce emotional suffering, but also to help them reach their ultimate goal of pregnancy.
In conclusion, the levels of psychological distress and quality of life in Korean infertile women seem to require psychological intervention. Results of this study provide a baseline for psychological distress and FertiQoL in infertile women in Korea, and could be used as a basis of information for psychological intervention and further studies, although sample size was not enough. We will clarify the connection between psychological distress and ART outcomes in a future study with the optimal sample size.
Footnotes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Greil AL. Infertility and psychological distress: a critical review of the literature. Soc Sci Med. 1997;45:1679–1704. doi: 10.1016/s0277-9536(97)00102-0. [DOI] [PubMed] [Google Scholar]
- 2.Drosdzol A, Skrzypulec V. Quality of life and sexual functioning of Polish infertile couples. Eur J Contracept Reprod Health Care. 2008;13:271–281. doi: 10.1080/13625180802049187. [DOI] [PubMed] [Google Scholar]
- 3.Chen TH, Chang SP, Tsai CF, Juang KD. Prevalence of depressive and anxiety disorders in an assisted reproductive technique clinic. Hum Reprod. 2004;19:2313–2318. doi: 10.1093/humrep/deh414. [DOI] [PubMed] [Google Scholar]
- 4.Williams KE, Marsh WK, Rasgon NL. Mood disorders and fertility in women: a critical review of the literature and implications for future research. Hum Reprod Update. 2007;13:607–616. doi: 10.1093/humupd/dmm019. [DOI] [PubMed] [Google Scholar]
- 5.Volgsten H, Skoog Svanberg A, Ekselius L, Lundkvist O, Sundstrom Poromaa I. Prevalence of psychiatric disorders in infertile women and men undergoing in vitro fertilization treatment. Hum Reprod. 2008;23:2056–2063. doi: 10.1093/humrep/den154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Verhaak CM, Smeenk JM, Evers AW, Kremer JA, Kraaimaat FW, Braat DD. Women's emotional adjustment to IVF: a systematic review of 25 years of research. Hum Reprod Update. 2007;13:27–36. doi: 10.1093/humupd/dml040. [DOI] [PubMed] [Google Scholar]
- 7.Klonoff-Cohen H. Female and male lifestyle habits and IVF: what is known and unknown. Hum Reprod Update. 2005;11:179–203. doi: 10.1093/humupd/dmh059. [DOI] [PubMed] [Google Scholar]
- 8.de Klerk C, Hunfeld JA, Heijnen EM, Eijkemans MJ, Fauser BC, Passchier J, et al. Low negative affect prior to treatment is associated with a decreased chance of live birth from a first IVF cycle. Hum Reprod. 2008;23:112–116. doi: 10.1093/humrep/dem357. [DOI] [PubMed] [Google Scholar]
- 9.Facchinetti F, Matteo ML, Artini GP, Volpe A, Genazzani AR. An increased vulnerability to stress is associated with a poor outcome of in vitro fertilization-embryo transfer treatment. Fertil Steril. 1997;67:309–314. doi: 10.1016/S0015-0282(97)81916-4. [DOI] [PubMed] [Google Scholar]
- 10.Demyttenaere K, Bonte L, Gheldof M, Vervaeke M, Meuleman C, Vanderschuerem D, et al. Coping style and depression level influence outcome in in vitro fertilization. Fertil Steril. 1998;69:1026–1033. doi: 10.1016/s0015-0282(98)00089-2. [DOI] [PubMed] [Google Scholar]
- 11.Gallinelli A, Roncaglia R, Matteo ML, Ciaccio I, Volpe A, Facchinetti F. Immunological changes and stress are associated with different implantation ratesin patients undergoing in vitro fertilization-embryo transfer. Fertil Steril. 2001;76:85–91. doi: 10.1016/s0015-0282(01)01826-x. [DOI] [PubMed] [Google Scholar]
- 12.Boivin J, Schmidt L. Infertility-related stress in men and women predicts treatment outcome 1 year later. Fertil Steril. 2005;83:1745–1752. doi: 10.1016/j.fertnstert.2004.12.039. [DOI] [PubMed] [Google Scholar]
- 13.Ebbesen SM, Zachariae R, Mehlsen MY, Thomsen D, Hojgaard A, Ottosen L, et al. Stressful life events are associated with a poor in-vitro fertilization (IVF) outcome: a prospective study. Hum Reprod. 2009;24:2173–2182. doi: 10.1093/humrep/dep185. [DOI] [PubMed] [Google Scholar]
- 14.Li XH, Ma YG, Geng LH, Qin L, Hu H, Li SW. Baseline psychological stress and ovarian norepinephrine levels negatively affect the outcome of in vitro fertilisation. Gynecol Endocrinol. 2011;27:139–143. doi: 10.3109/09513590.2010.501871. [DOI] [PubMed] [Google Scholar]
- 15.Klonoff-Cohen H, Natarajan L. The concerns during assisted reproductive technologies (CART) scale and pregnancy outcomes. Fertil Steril. 2004;81:982–988. doi: 10.1016/j.fertnstert.2003.08.050. [DOI] [PubMed] [Google Scholar]
- 16.Nakamura K, Sheps S, Arck PC. Stress and reproductive failure: past notions, present insights and future directions. J Assist Reprod Genet. 2008;25:47–62. doi: 10.1007/s10815-008-9206-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.An Y, Wang Z, Ji H, Zhang Y, Wu K. Pituitary-adrenal and sympathetic nervous system responses to psychiatric disorders in women undergoing in vitro fertilization treatment. Fertil Steril. 2011;96:404–408. doi: 10.1016/j.fertnstert.2011.05.092. [DOI] [PubMed] [Google Scholar]
- 18.Smeenk JM, Verhaak CM, Vingerhoets AJ, Sweep CG, Merkus JM, Willemsen SJ, et al. Stress and outcome success in IVF: the role of self-reports and endocrine variables. Hum Reprod. 2005;20:991–996. doi: 10.1093/humrep/deh739. [DOI] [PubMed] [Google Scholar]
- 19.Michael AE. Life after liquorice: the link between cortisol and conception. Reprod Biomed Online. 2003;7:683–690. doi: 10.1016/s1472-6483(10)62091-3. [DOI] [PubMed] [Google Scholar]
- 20.Wright J, Duchesne C, Sabourin S, Bissonnette F, Benoit J, Girard Y. Psychosocial distress and infertility: men and women respond differently. Fertil Steril. 1991;55:100–108. [PubMed] [Google Scholar]
- 21.Newton CR, Houle M. Gender differences in psychological response to infertility treatment. In: Greenfeld DA, editor. Infertility and reproductive medicine clinics of North America. Philadelphia: WB Saunders; 1993. pp. 545–558. [Google Scholar]
- 22.Wischmann T, Scherg H, Strowitzki T, Verres R. Psychosocial characteristics of women and men attending infertility counselling. Hum Reprod. 2009;24:378–385. doi: 10.1093/humrep/den401. [DOI] [PubMed] [Google Scholar]
- 23.Wichman CL, Ehlers SL, Wichman SE, Weaver AL, Coddington C. Comparison of multiple psychological distress measures between men and women preparing for in vitro fertilization. Fertil Steril. 2011;95:717–721. doi: 10.1016/j.fertnstert.2010.09.043. [DOI] [PubMed] [Google Scholar]
- 24.Cwikel J, Gidron Y, Sheiner E. Psychological interactions with infertility among women. Eur J Obstet Gynecol Reprod Biol. 2004;117:126–131. doi: 10.1016/j.ejogrb.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 25.Burns LH. Psychiatric aspects of infertility and infertility treatments. Psychiatr Clin North Am. 2007;30:689–716. doi: 10.1016/j.psc.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 26.Hammerli K, Znoj H, Barth J. The efficacy of psychological interventions for infertile patients: a meta-analysis examining mental health and pregnancy rate. Hum Reprod Update. 2009;15:279–295. doi: 10.1093/humupd/dmp002. [DOI] [PubMed] [Google Scholar]
- 27.Matthiesen S, Klonoff-Cohen H, Zachariae R, Jensen-Johansen MB, Nielsen BK, Frederiksen Y, et al. The effect of an expressive writing intervention (EWI) on stress in infertile couples undergoing assisted reproductive technology (ART) treatment: a randomized controlled pilot study. Br J Health Psychol. 2012;17:362–378. doi: 10.1111/j.2044-8287.2011.02042.x. [DOI] [PubMed] [Google Scholar]
- 28.Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychol Assess. 1998;10:176–181. [Google Scholar]
- 29.Boivin J, Takefman J, Braverman A. The fertility quality of life (FertiQoL) tool: development and general psychometric properties. Fertil Steril. 2011;96:409–415.e3. doi: 10.1016/j.fertnstert.2011.02.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Newton CR, Sherrard W, Glavac I. The Fertility Problem Inventory: measuring perceived infertility-related stress. Fertil Steril. 1999;72:54–62. doi: 10.1016/s0015-0282(99)00164-8. [DOI] [PubMed] [Google Scholar]
- 31.Tiplady S, Jones G, Campbell M, Johnson S, Ledger W. Home ovulation tests and stress in women trying to conceive: a randomized controlled trial. Hum Reprod. 2013;28:138–151. doi: 10.1093/humrep/des372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aarts JW, van Empel IW, Boivin J, Nelen WL, Kremer JA, Verhaak CM. Relationship between quality of life and distress in infertility: a validation study of the Dutch FertiQoL. Hum Reprod. 2011;26:1112–1118. doi: 10.1093/humrep/der051. [DOI] [PubMed] [Google Scholar]
- 33.Matsubayashi H, Hosaka T, Izumi S, Suzuki T, Kondo A, Makino T. Increased depression and anxiety in infertile Japanese women resulting from lack of husband's support and feelings of stress. Gen Hosp Psychiatry. 2004;26:398–404. doi: 10.1016/j.genhosppsych.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 34.An Y, Sun Z, Li L, Zhang Y, Ji H. Relationship between psychological stress and reproductive outcome in women undergoing in vitro fertilization treatment: psychological and neurohormonal assessment. J Assist Reprod Genet. 2013;30:35–41. doi: 10.1007/s10815-012-9904-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kalantaridou SN, Makrigiannakis A, Zoumakis E, Chrousos GP. Stress and the female reproductive system. J Reprod Immunol. 2004;62:61–68. doi: 10.1016/j.jri.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 36.Chan CH, Ng EH, Chan CL, Ho, Chan TH. Effectiveness of psychosocial group intervention for reducing anxiety in women undergoing in vitro fertilization: a randomized controlled study. Fertil Steril. 2006;85:339–346. doi: 10.1016/j.fertnstert.2005.07.1310. [DOI] [PubMed] [Google Scholar]