Abstract
Arthroscopic osteochondroplasty has become the most common treatment for cam-type femoroacetabular impingement. However, gauging the appropriate depth and location of the femoral osteochondroplasty remains challenging, given the parallax observed from using a 70° arthroscope across multiple viewing perspectives. Consequently, reliable techniques must use a combination of arthroscopic and fluoroscopic checks and balances to assess the femoral head-neck junction to help guide bony resection. We have developed a technique for osteochondroplasty that has made the process more efficient and reliable in our hands. It involves creating a trough at the apex of the osteochondroplasty and then contouring the proximal and distal regions to re-create normal proximal femoral geometry. This article details our technique for femoral osteochondroplasty, which can be performed alone for isolated cam impingement or in concert with other intra- and extra-articular procedures to address associated hip pathology.
Hip arthroscopy has evolved rapidly over the past 10 years.1 Originally, hip arthroscopy was only useful for simple procedures including diagnostic arthroscopy and loose body removal. With improved understanding of young adult hip pathology and development of proper instruments for arthroscopy of the hip, indications for hip arthroscopy have broadened. Femoroacetabular impingement (FAI) is now commonly corrected arthroscopically to achieve pain relief while attempting to preserve long-term hip health and possibly delay osteoarthritis.2
FAI can be caused on the femoral side by asphericity of the femoral head and lack of femoral head and neck offset, which is referred to as “cam-type FAI.”3 The acetabular side can also cause FAI if the femoral head is over-covered, which can be either focal or global. This is referred to as “pincer-type FAI.” Most patients with FAI have a combination of these 2 patterns of impingement.4 Treatment options include open surgical dislocation, a direct anterior open approach, and arthroscopy.5, 6, 7 Many groups have described good outcomes from the arthroscopic treatment of FAI.7, 8
The recent increase in hip arthroscopy for FAI has led to many surgeons practicing hip arthroscopy without the benefit of formalized training in arthroscopic hip techniques. We detail our technique with video guidance for osteochondroplasty of the femoral head-neck junction for cam-type FAI.
Surgical Technique
Patient Positioning and Gaining Access to Hip
The patient is placed in the supine position on the traction table (Smith & Nephew, Andover, MA). The lateral aspect of the operative leg is prepared from anterior to the anterior superior iliac spine distally to the mid thigh and is draped in a sterile fashion. We obtain access to the hip as previously described, starting with the anterior-lateral portal and then using the modified anterior portal.9
Capsulotomy and Addressing Intra-articular Pathology
After access is obtained, an interportal capsulotomy is performed using a radiofrequency ablation device (Super TurboVac 90°; ArthroCare, Austin, TX). Extracapsular fat is removed to facilitate capsular closure at the end of the case. Preparation of the pericapsular tissue and meticulous hemostasis will improve visualization throughout the case. We do not perform a T-capsulotomy routinely; however, this is an option for improved visualization. All intra-articular, acetabular, and labral pathology is first addressed while the hip is in traction.
Peripheral Compartment and Femoral-sided Access
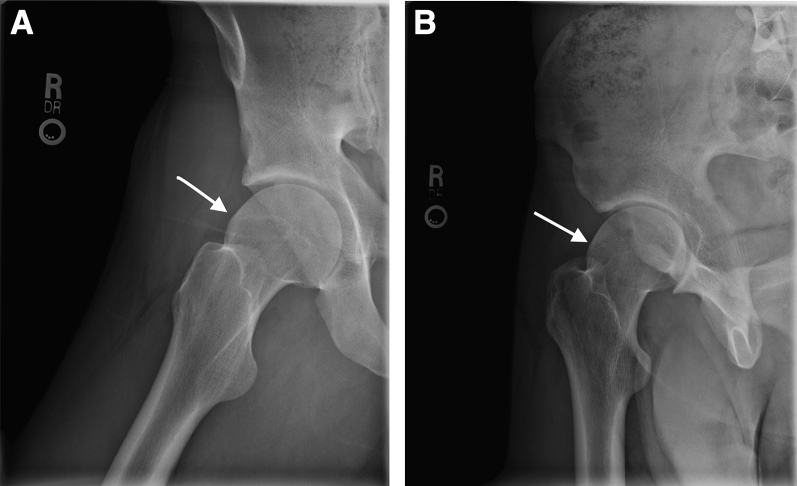
After completion of the intra-articular portion of the procedure, traction is released and attention is turned to the peripheral compartment, where the femoral head-neck deformity is identified. A 70° arthroscope (Smith & Nephew) is positioned in the anterolateral portal in preparation for the osteochondroplasty if it has been moved during the procedure (Video 1). Preoperative false-profile and frog-leg lateral images are used to identify the cam lesion (Fig 1).
Fig 1.
Preoperative radiographs diagnostic of a cam lesion with lack of femoral head-neck offset. The frog-leg lateral (A) and false-profile (B) radiographs show lack of femoral head-neck offset and asphericity of the femoral head (arrows) in a right hip.
Identification of Cam Lesion
The cam lesion is defined both arthroscopically and radiographically. Dynamic arthroscopic examination identifies the impinging portion of the femoral head-neck junction (Video 1). Arthroscopically, cartilage overlying the deformity commonly has a discoloration or peel-off lesion that distinguishes the lesion from the normal-appearing articular cartilage. Care should be taken to note signs corresponding to areas of impingement including localized hyperemia or fraying of the labrum. Radiographically, arthroscopic instruments are positioned to define the lesion on fluoroscopy and correlate the arthroscopic anatomy with radiographic markers. Fibrocystic or sclerotic changes in the femoral neck can be pathognomonic features of impinging regions (Fig 2). The superior-posterior extent of the cam lesion is easiest to define with the hip in extension and internal rotation, whereas the anterior-inferior extent of the lesion is best defined with the hip in 30° to 45° of flexion and in neutral rotation (Video 1). Anteroposterior and lateral fluoroscopic images are obtained before beginning the osteochondroplasty to allow comparisons during the resection and monitoring of progress. It is important to make sure that the femoral head is completely seated in the acetabulum and not partially subluxated before defining the cam lesion; otherwise, drifting too far medially on the weight-bearing articular cartilage may occur, causing over-resection.
Fig 2.
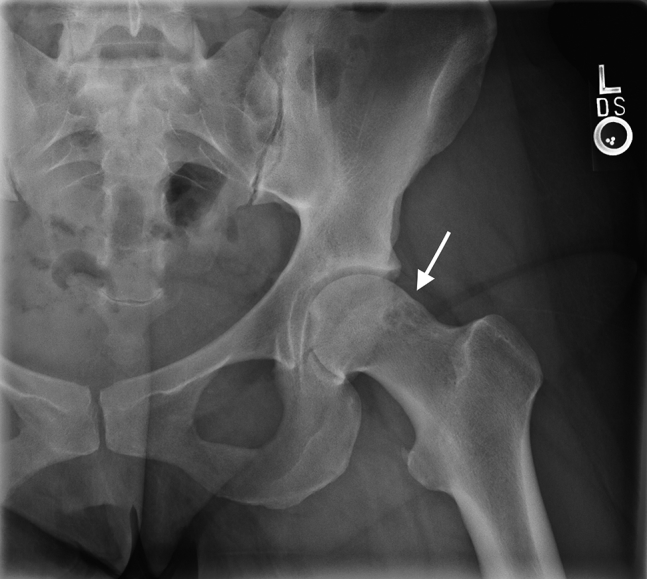
Frog-leg lateral radiograph of a left hip showing fibrocystic changes at the femoral head-neck junction indicative of impingement (arrow).
Defining Cam Lesion
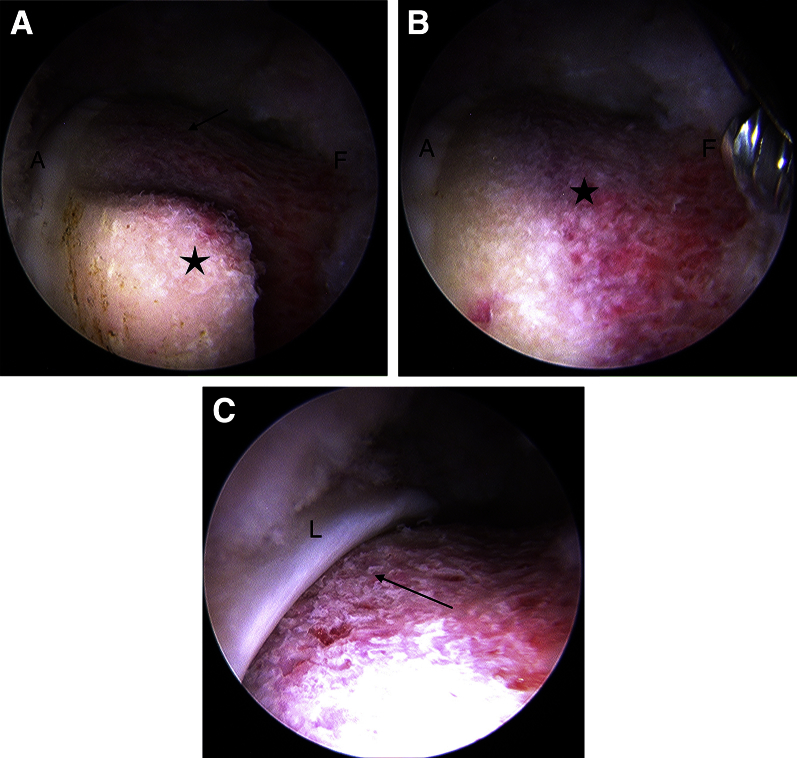
The hip is flexed to 45° to allow for full visualization of the peripheral compartment and to relax the capsular tissue (Video 1). The medial and lateral synovial folds are identified to localize the retinacular vessels. The cam deformity is then localized both superiorly and inferiorly. By use of electrocautery, the soft tissue is removed from the cam lesion. The medial border of the cam can be localized with a combination of fluoroscopy and direct visualization of the discolored and frayed chondral surface overlying the cam lesion (Fig 3).
Fig 3.
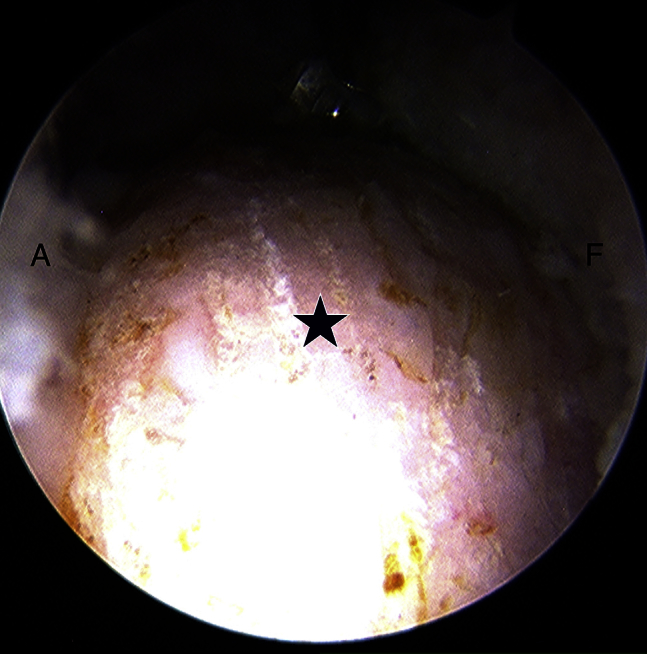
In a right hip, viewed from the anterolateral portal, a cam lesion (star) is defined by radiofrequency ablation before osteoplasty. The articular surface and acetabular side of the capsule (A) are to the left, whereas the femoral neck and femoral side of the capsule (F) are to the right.
Creating Trough to Define Apex of Osteochondroplasty
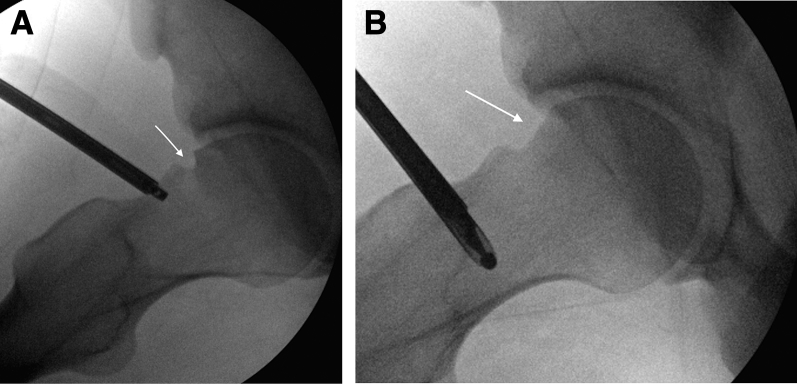
A trough is created through the cam deformity using a 5.5-mm burr (Smith & Nephew). Deepening of the trough (in most cases 3 to 5 mm) can then be performed using the width of the 5.5-mm burr as a guide. The trough parallels the previously defined edge of the femoral head articular cartilage 8 to 10 mm distally and laterally to the articular margin (Fig 4, Video 1). Paralleling the articular surface allows precise localization of this trough as the hip is moved through the flexion-extension arc. For larger cam lesions, the trough can be deepened when fluoroscopy and dynamic examination confirm the need for a larger osteochondroplasty to restore offset. Posteriorly, the trough must be extended through a ledge usually noted around the 1-o'clock position that denotes the posterior border of the cam lesion. Multiple images obtained with C-arm fluoroscopy are used to judge proper creation of the trough (Fig 5A).
Fig 4.
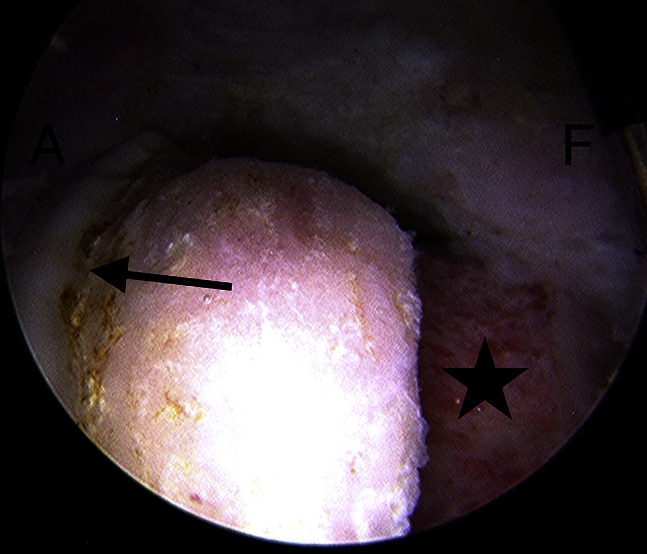
In a right hip, viewed from the anterolateral portal, a trough (star) that is the depth of a 5.5-mm burr is created approximately 8 to 10 mm from the edge of the weight-bearing articular surface (arrow). The acetabular and medial side (A) is to the left, and the femoral and lateral side (F) is to the right.
Fig 5.
Intraoperative fluoroscopic frog-leg lateral images of a right hip. (A) The femoral neck, after trough creation, is used to confirm that the trough (arrow) re-creates appropriate head-neck offset and can be contoured to a spherical femoral head. (B) Contour from the articular surface to the trough after resection of the proximal-medial aspect of the cam lesion (arrow).
Completing Osteochondroplasty Proximally and Distally
When a sufficient trough has been created to define the deepest extent of the osteochondroplasty, the resection is blended proximally and medially to create a smooth graded contour of the femoral neck (Fig 5B). Areas of impingement are commonly sclerotic on the femoral neck. The burr can be used in forward mode to remove the sclerotic cortex and then in reverse mode to smooth the contour of the underlying cancellous bone (Video 1). The key is removing almost nothing directly adjacent to the articular margin and then creating an evenly graded contour distally and laterally to the trough. When the proximal aspect of the resection is halfway complete, dynamic examination can show that the impingement is resolved at the area that has been resected (Fig 6A). Care is taken not to make too sharp a ledge approaching the articular surface because this could compromise the labral suction seal. After complete resection of the deformity, the hip is again brought through a dynamic range of motion and impingement is assessed on arthroscopic visualization and fluoroscopy (Fig 6B). If further areas of impingement are noted on dynamic examination, then these areas can be further resected. Once the medial osteochondroplasty is complete, the rest of the lateral bony prominence can be resected to contour the natural slope of the femoral neck. This is best performed with the hip flexed. Fluoroscopy is then used in a circumferential manner to confirm restoration of femoral head-neck offset.
Fig 6.
A right hip, viewed from the anterolateral portal. (A) Partially resected cam lesion (arrow) on dynamic examination showing continued impingement in the un-resected region (star). The acetabular and articular side (A) is on the left, and the femoral and lateral side (F) is on the right. (B) Fully resected cam lesion (star). The acetabular and articular side (A) is on the left, and the femoral and lateral side (F) is on the right. (C) Resolution of impingement after cam resection (arrow) on dynamic examination the labrum (L) clears without impingement in the area of the resected cam lesion.
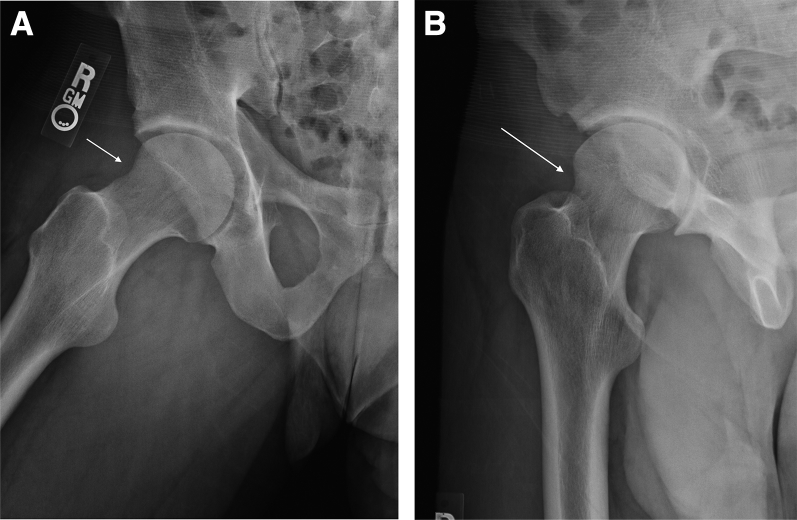
Irrigation and Capsular Closure
On completion of the osteoplasty, the joint is copiously irrigated to remove bony debris and a complete capsular closure is performed in all cases. The SlingShot suture passer (Stryker, Kalamazoo, MI) is used to close the capsule with 5 to 8 No. 2 Ultrabraid sutures (Smith & Nephew). Postoperative frog-leg lateral and false-profile radiographs confirm proper resection of the cam lesion with appropriate head-neck offset (Fig 7).
Fig 7.
Postoperative radiographs confirming re-creation of femoral head-neck offset and resection of cam lesion in a right hip. These can be compared with the preoperative images in Figure 1. The frog-leg lateral (A) and false-profile (B) radiographs show restoration of femoral head-neck offset (arrows) and restoration of sphericity of the femoral head.
Discussion
Multiple authors have published techniques for femoral osteoplasty to correct cam-type FAI. Jackson et al.10 described a technique in which they start distally on the neck and progress proximally to resect the bony deformity with care to not over-resect proximally because this could negate the suction-seal effect of the labrum. Philippon et al.11 described the resection of 5 to 7 mm in depth and 8 to 12 mm in width from the 6- to 12-o'clock position on the femoral head with intermittent dynamic examination to evaluate for impingement, although they start inferiorly and progress superiorly. Similarly, Bedi et al.7 have described their technique for FAI surgery and detailed their use of a T-capsulotomy and osteoplasty with radiographic evaluation and dynamic arthroscopic examination. Byrd and Jones12 presented a proximal-to-distal technique with good functional outcomes at 2 years' follow-up.
Table 1 details the steps to our technique. To create a more structured and efficient osteoplasty technique, we began creating a trough to first resect the amount of bone needed to define the deepest aspect of the osteoplasty. After this was completed, we found the distal and proximal resection to be easier and faster to complete by connecting the trough with a smooth contour to the articular surface proximally and the more distal femoral neck. Advantages and risks or limitations of our technique are detailed in Table 2. This is contrary to the osteoplasty technique described by Jackson et al.10 that progresses from distally to proximally. In the past, we performed our osteoplasty similarly to their technique; however, we have found the described technique to be more effective and time-efficient in our hands.
Table 1.
Steps of Trough Femoral Osteochondroplasty Technique
| 1. Patient positioning and accessing hip |
| 2. Capsulotomy and addressing intra-articular pathology |
| 3. Peripheral compartment and femoral-sided access |
| 4. Identification of cam lesion |
| 5. Defining cam lesion |
| 6. Creating trough to define apex of osteochondroplasty |
| 7. Completing osteochondroplasty proximally and distally |
| 8. Irrigation and capsular closure |
Table 2.
Advantages and Risks or Limitations of Trough Femoral Osteochondroplasty Technique
| Advantages |
| Defining the cam lesion with a radiofrequency ablation probe can help identify sclerotic-appearing bone in areas of impingement. |
| Once the deepest aspect of the trough is defined to determine head-neck offset, contouring the neck is quick and efficient. |
| The technique follows a systematic order to create head-neck offset and relieve impingement. |
| Risks or limitations |
| Defining the cam lesion with electrocautery can injure the weight-bearing surface if the hip is externally rotated or subluxated during this step. |
| Overzealous creation of the trough can lead to notching of the femoral neck and create a stress riser. |
| Over-resection of the cam lesion proximally can lead to loss of the labral suction seal. |
| Visualization using an interportal capsulotomy requires mobilization of the extremity and may be technically challenging. |
| Lack of fluoroscopic checks and intraoperative dynamic examination can lead to over- or under-resection of the cam lesion. |
Table 3 presents the pearls of this technique. There are multiple potential pitfalls to this technique (Table 4). An overzealous proximal osteoplasty can negate the labral suction seal or can lead to femoral neck fracture or stress fracture.10, 13 To protect against these complications, intraoperative fluoroscopy is needed to visualize the osteoplasty. In addition, frequent examination under arthroscopic visualization is required. Because only an interportal capsulotomy is used, it is important to not inadvertently resect capsular tissue while performing the osteochondroplasty. This can lead to iatrogenic instability of the hip postoperatively if the capsule cannot be repaired. If visualization is a problem, a T-capsulotomy with capsular retraction can be used to help preserve capsular tissue.7 Despite these limitations, we believe this to be an efficient manner to perform an osteochondroplasty for cam-type FAI. The aforementioned potential complications can occur with any osteoplasty technique and are not unique to our technique.
Table 3.
Pearls for Trough Femoral Osteochondroplasty Technique
| Creation of a sufficient interportal capsulotomy should be performed for visualization. |
| A T-capsulotomy should be used for increased visualization as needed. |
| Trough creation should be completed before proximal-distal resection. |
| Sclerotic-appearing bone is commonly encountered on the femoral neck in areas of impingement. |
| The burr should be used in forward mode to remove sclerotic cortical bone and in reverse mode to contour softer cancellous bone. |
| Almost no resection should be performed adjacent to the articular surface with a graded contour to the trough. |
| The surgeon should confirm that resection is creating appropriate clearance on dynamic examination while completing osteochondroplasty. |
| Capsular resection should be avoided. |
| Fluoroscopy should be used in multiple leg positions to confirm complete resection and restoration of head-neck offset. |
Table 4.
Pitfalls to Trough Femoral Osteochondroplasty Technique
| Difficulty in retracting capsular tissue may be encountered while performing resection. |
| Defining the cam lesion with the hip subluxated or excessively externally rotated may lead to excessive medialization of the cam border. |
| Failure to repair the capsule may lead to hip instability. |
| Notching of the femoral neck may occur. |
| Creation of a stress riser in the femoral neck may occur by not smoothing the contour of the distal neck. |
| Excessive proximal resection may compromise the suction seal of the labrum. |
| The cam lesion cannot be visualized in its entirety, all at once without T-capsulotomy. |
Footnotes
The authors report the following potential conflict of interest or source of funding: S.K.A. receives support from Stryker/Pivot Medical (educational consultant).
Supplementary Data
Trough technique for femoral osteochondroplasty for cam-type femoroacetabular impingement. The video starts with definition of the cam lesion by radiography and dynamic examination, proceeds to removal of the soft tissue and cartilage overlying the bone, and then proceeds through our technique to restore spherical anatomy to the femoral head and relieve impingement with the acetabulum and labrum. The technique involves creation of a trough 8 to 10 mm off of the defined articular surface that is the depth of a 5.5-mm burr with the use of fluoroscopic assistance. The contour is then graded to the articular surface proximally with dynamic examination under arthroscopy proving resolution of impingement when it is halfway complete from anteriorly to posteriorly. The proximal cam resection is then completed, and dynamic examination proves resolution of impingement. Fluoroscopy is used to confirm resolution of head-neck offset and creation of a spherical femoral head. The femoral neck is then reshaped to a smooth contour distal to the trough, and bony debris is irrigated followed by capsular closure.
References
- 1.Glick J.M., Valone F., Safran M.R. Hip arthroscopy: From the beginning to the future—An innovator's perspective. Knee Surg Sports Traumatol Arthrosc. 2014;22:714–721. doi: 10.1007/s00167-014-2859-y. [DOI] [PubMed] [Google Scholar]
- 2.Bedi A., Kelly B.T. Femoroacetabular impingement. J Bone Joint Surg Am. 2013;95:82–92. doi: 10.2106/JBJS.K.01219. [DOI] [PubMed] [Google Scholar]
- 3.Ganz R., Parvizi J., Beck M., Leunig M., Nötzli H., Siebenrock K.A. Femoroacetabular impingement: A cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 4.Beck M., Kalhor M., Leunig M., Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: Femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 5.Cohen S.B., Huang R., Ciccotti M.G., Dodson C.C., Parvizi J. Treatment of femoroacetabular impingement in athletes using a mini-direct anterior approach. Am J Sports Med. 2012;40:1620–1627. doi: 10.1177/0363546512445883. [DOI] [PubMed] [Google Scholar]
- 6.Steppacher S.D., Anwander H., Zurmühle C.A., Tannast M., Siebenrock K.A. Eighty percent of patients with surgical hip dislocation for femoroacetabular impingement have a good clinical result without osteoarthritis progression at 10 years. Clin Orthop Relat Res. 2014;473:1333–1341. doi: 10.1007/s11999-014-4025-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bedi A., Kelly B.T., Khanduja V. Arthroscopic hip preservation surgery: Current concepts and perspective. Bone Joint J. 2012;95-B:10–19. doi: 10.1302/0301-620X.95B1.29608. [DOI] [PubMed] [Google Scholar]
- 8.Gupta A., Redmond J.M., Stake C.E., Dunne K.F., Domb B.G. Does primary hip arthroscopy result in improved clinical outcomes? 2-Year clinical follow-up on a mixed group of 738 consecutive primary hip arthroscopies performed at a high-volume referral center. Am J Sports Med. 2016;44:74–82. doi: 10.1177/0363546514562563. [DOI] [PubMed] [Google Scholar]
- 9.Aoki S.K., Beckmann J.T., Wylie J.D. Hip arthroscopy and the anterolateral portal: Avoiding labral penetration and femoral articular injuries. Arthrosc Tech. 2012;1:e155–e160. doi: 10.1016/j.eats.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jackson T.J., Stake C.E., Trenga A.P., Morgan J., Domb B.G. Arthroscopic technique for treatment of femoroacetabular impingement. Arthrosc Tech. 2013;2:e55–e59. doi: 10.1016/j.eats.2012.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Philippon M.J., Stubbs A.J., Schenker M.L., Maxwell R.B., Ganz R., Leunig M. Arthroscopic management of femoroacetabular impingement: Osteoplasty technique and literature review. Am J Sports Med. 2007;35:1571–1580. doi: 10.1177/0363546507300258. [DOI] [PubMed] [Google Scholar]
- 12.Byrd J.W.T., Jones K.S. Arthroscopic femoroplasty in the management of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2008;467:739–746. doi: 10.1007/s11999-008-0659-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Papavasiliou A.V., Bardakos N.V. Complications of arthroscopic surgery of the hip. Bone Joint Res. 2012;1:131–144. doi: 10.1302/2046-3758.17.2000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trough technique for femoral osteochondroplasty for cam-type femoroacetabular impingement. The video starts with definition of the cam lesion by radiography and dynamic examination, proceeds to removal of the soft tissue and cartilage overlying the bone, and then proceeds through our technique to restore spherical anatomy to the femoral head and relieve impingement with the acetabulum and labrum. The technique involves creation of a trough 8 to 10 mm off of the defined articular surface that is the depth of a 5.5-mm burr with the use of fluoroscopic assistance. The contour is then graded to the articular surface proximally with dynamic examination under arthroscopy proving resolution of impingement when it is halfway complete from anteriorly to posteriorly. The proximal cam resection is then completed, and dynamic examination proves resolution of impingement. Fluoroscopy is used to confirm resolution of head-neck offset and creation of a spherical femoral head. The femoral neck is then reshaped to a smooth contour distal to the trough, and bony debris is irrigated followed by capsular closure.