Abstract
The epithelial response to the opportunistic pathogen Campylobacter concisus is poorly characterised. Here, we assessed the intestinal epithelial responses to two C. concisus strains with different virulence characteristics in Caco-2 cells using RNAseq, and validated a subset of the response using qPCR arrays. C. concisus strains induced distinct response patterns from intestinal epithelial cells, with the toxigenic strain inducing a significantly more amplified response. A range of cellular functions were significantly regulated in a strain-specific manner, including epithelial-to-mesenchymal transition (NOTCH and Hedgehog), cytoskeletal remodeling, tight junctions, inflammatory responses and autophagy. Pattern recognition receptors were regulated, including TLR3 and IFI16, suggesting that nucleic acid sensing was important for epithelial recognition of C. concisus. C. concisus zonula occludens toxin (ZOT) was expressed and purified, and the epithelial response to the toxin was analysed using RNAseq. ZOT upregulated PAR2 expression, as well as processes related to tight junctions and cytoskeletal remodeling. C. concisus ZOT also induced upregulation of TLR3, pro-inflammatory cytokines IL6, IL8 and chemokine CXCL16, as well as the executioner caspase CASP7. Here, we characterise distinct global epithelial responses to C. concisus strains, and the virulence factor ZOT, and provide novel information on mechanisms by which this bacterium may affect the host.
Campylobacter concisus is a member of the human oral microbiota1,2, that has also been detected in the oesophagus3 and lower intestinal tract1 of healthy humans. C. concisus has also been associated with a range of human diseases such as Barrett’s oesophagus4, gastroenteritis5,6,7 and inflammatory bowel diseases8,9.
A number of possible explanations have been suggested for the presence of C. concisus in both healthy and diseased individuals. For example, C. concisus may act as an opportunistic pathogen whose growth and pathogenesis is modulated by host factors such as exposure to inflammation, acid, or bile4,10 or by the host microbiota11. Further, C. concisus strains have now been classified into commensals and at least two different pathotypes [adherent toxigenic C. concisus (AToCC) and adherent invasive C. concisus (AICC)] based on their virulence mechanisms12. One such virulence mechanism pertinent to AToCC strains is the presence of a zonula occludens toxin (ZOT)13, a toxin that was first identified in Vibrio species to target tight junctions of epithelial cells14. A further virulence mechanism present in AICC strains is the ability to survive intracellularly within epithelial cells in a process that involves autophagy15. In addition to these differences, the strains belonging to these pathotypes have been shown using comparative genomics to be highly genetically diverse16.
However, despite an improvement in our understanding of the bacterium’s virulence mechanisms, the epithelial response to C. concisus remains poorly understood. What is clear from our current knowledge of C. concisus-epithelial interaction, is that in addition to the role of autophagy and tight junctions15,17, host cells produce a range of pro-inflammatory cytokines in response to infection10,18. Thus, to gain a better understanding of the interaction between C. concisus and the host at the epithelial interface, this study comprehensively assessed the response of the intestinal epithelial cell-line Caco-2 to AToCC strain BAA-1457 and AICC strain UNSWCD with RNA-seq. The response of Caco-2 cells to purified ZOT from C. concisus BAA-1457 was also determined using the same approach.
Results
Comparative analysis of epithelial response to Campylobacter concisus pathotypes
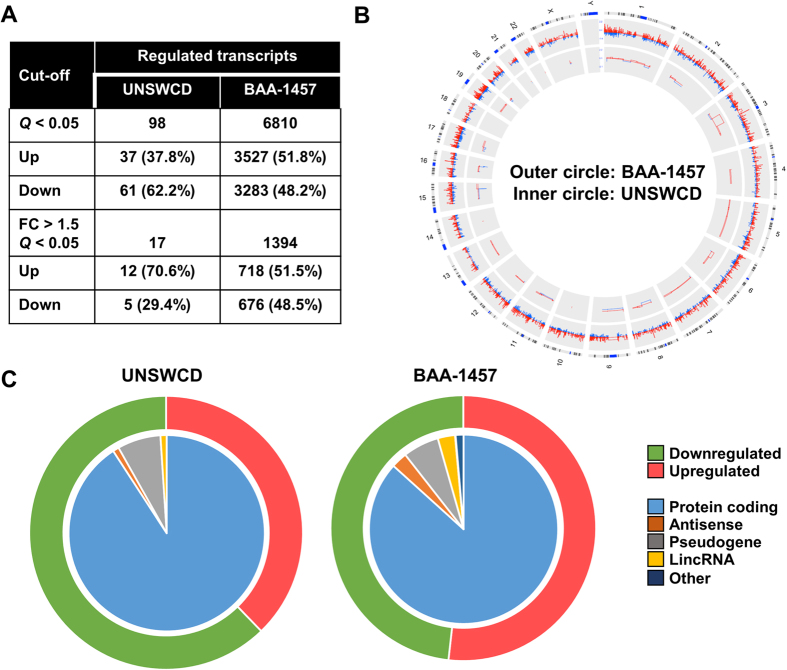
The response of Caco-2 intestinal epithelial cells (IECs) to two C. concisus strains with different virulence mechanisms was examined using RNA-seq. Global gene expression indicated that IECs responded in a distinct manner to each of the AICC (UNSWCD) and AToCC (BAA-1457) strains, with the response to the AToCC strain being markedly larger (Fig. 1A,B). A similar number of transcripts were upregulated and downregulated following infection with BAA-1457, while a higher number of transcripts were downregulated than upregulated following infection with UNSWCD (Fig. 1C). The majority of differentially expressed transcripts were protein coding, however, a range of antisense and long non-coding transcripts were also identified to be differentially expressed (Fig. 1C).
Figure 1. Transcriptional regulation in intestinal epithelial Caco-2 cells infected with Campylobacter concisus.
(A) Number of significantly differentially expressed transcripts following infection with C. concisus BAA-1457 or UNSWCD. (B) Comparison of the responses of Caco-2 cells to C. concisus BAA-1457 (outer circle) and UNSWCD (inner circle). Transcripts were mapped according to location on human chromosomes. Responses were visualised using circular Circos plot, with transcripts increased in expression in red and those decreased in blue. (C) Numbers of upregulated (red) and downregulated (green) transcripts visualised in the outer circles, and types of regulated transcripts visualised independently in the inner circles.
Epithelial response to infection with adherent invasive Campylobacter concisus
Ninety-eight transcripts were found to be differentially expressed (Q < 0.05) following infection of IECs with the AICC strain UNSWCD (Fig. 1A, Supplementary Data 1). When the threshold was increased (Q < 0.1), the number of transcripts only increased to 156 (Supplementary Data 1). This epithelial response was weak when compared to the response of THP-1 derived macrophages19, which differentially expressed 8,343 transcripts at greater than 1.5-fold regulation (Q < 0.05) following infection with C. concisus UNSWCD.
Infection with C. concisus UNSWCD induced an oxidative stress response in IECs, with a range of metallothionein-encoding transcripts found to be upregulated, in addition to nitric oxide synthase 2 (NOS2) and glutathione peroxidase 1 (GPX1) (Supplementary Data 1). Further, transcripts involved in xenobiotic metabolism (CYP1A1 and CYP1B1) and fluid transport (NPPB and VIPR1) were also upregulated.
Transcripts involved in the inflammatory response were also differentially expressed (upregulated) following infection with C. concisus UNSWCD. CCL2 and BIRC3, as well as IKBKE, which is involved in the non-canonical activation of NF-κB, were upregulated (Supplementary Data 1). There also appeared to be an impact on the tight junctions of IECs, with a range of transcripts showing significant changes in expression in both directions (CLDN2, PMP22, CLDN1, and TJP1). One transcript (ATG9B) involved in autophagy was significantly decreased in expression following infection. Given the importance of autophagy in the intracellular survival of C. concisus, we confirmed the repression of this process following infection with another AICC strain, UNSW3 (Table 1). Further, a range of transcripts (SQLE, LDLR, VLDLR, HMGCS1, and INSIG1) involved in cholesterol synthesis, metabolism and transport were significantly decreased in expression following infection with C. concisus UNSWCD.
Table 1. Genes within the autophagy pathway differentially expressed following C. concisus UNSW3 or BAA-1457 infection of intestinal epithelial cells.
| Strain | Gene | Gene Description | Fold Change | Fold Regulation | P-value |
|---|---|---|---|---|---|
| UNSW3 | ATG4A | ATG4 autophagy related 4 homolog A (S. cerevisiae) | 0.64 | −1.57 | 0.040 |
| HDAC1 | Histone deacetylase 1 | 0.66 | −1.51 | 0.035 | |
| HSPA8 | Heat shock 70 kDa protein 8 | 0.45 | −2.21 | 0.020 | |
| MAPK14 | Mitogen-activated protein kinase 14 | 0.60 | −1.67 | 0.0037 | |
| PIK3C3 | Phosphoinositide-3-kinase, class 3 | 0.65 | −1.54 | 0.054 | |
| UVRAG | UV radiation resistance associated gene | 0.73 | −1.36 | 0.077 | |
| BAA-1457 | ATG4A | ATG4 autophagy related 4 homolog A (S. cerevisiae) | 0.47 | −2.12 | 0.0048 |
| EIF4G1 | Eukaryotic translation initiation factor 4 gamma, 1 | 0.37 | −2.70 | 0.021 | |
| MAP1LC3B | Microtubule-associated protein 1 light chain 3 beta | 2.63 | 2.63 | 0.0052 | |
| MTOR | Mechanistic target of rapamycin (serine/threonine kinase) | 0.52 | −1.94 | 0.0021 |
Expression was determined using an autophagy-specific qPCR array.
Fold change values < 1, fold regulation refers to the negative inverse of the fold change. When fold change is ≥1, fold regulation = fold change.
Epithelial response to infection with adherent toxigenic Campylobacter concisus
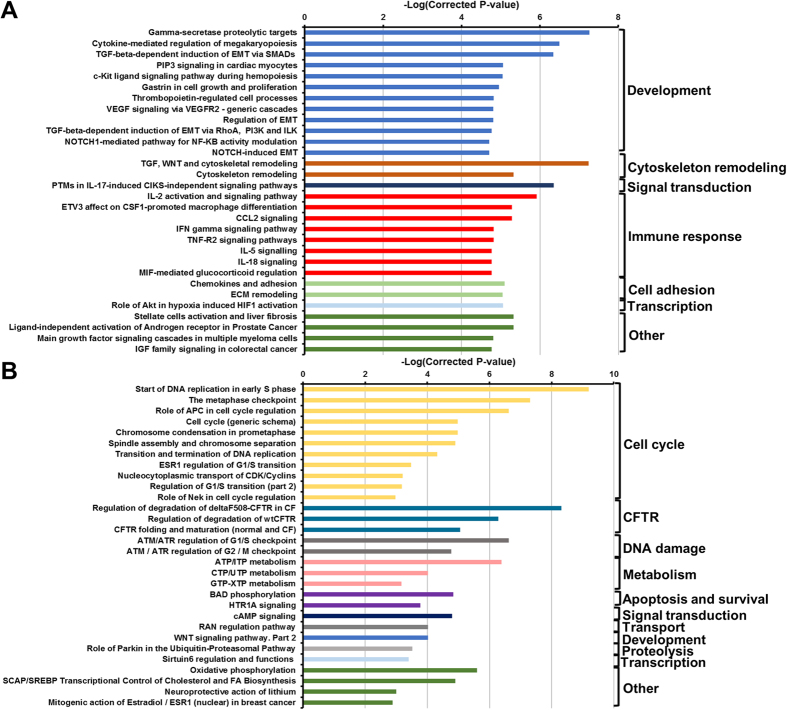
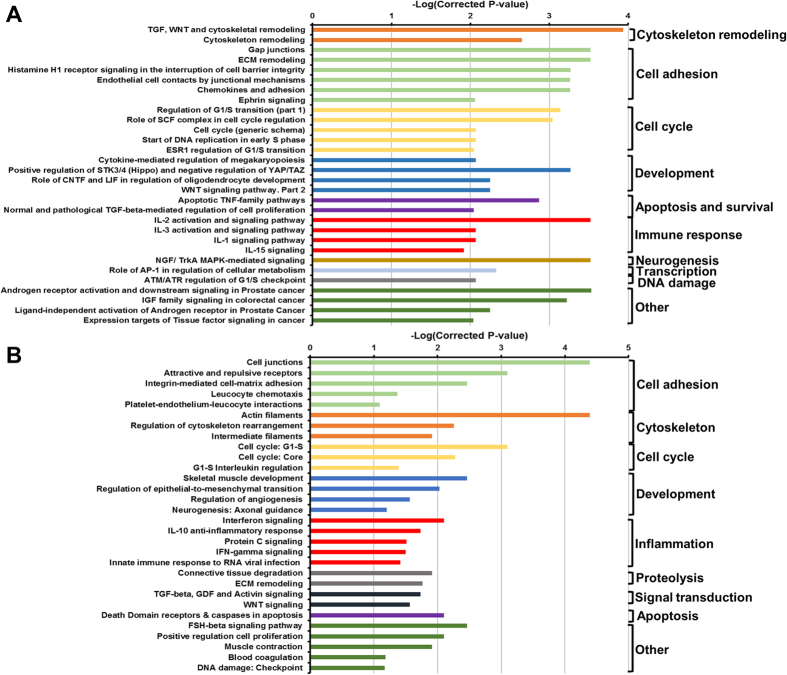
Infection of IECs with the AToCC strain BAA-1457 significantly affected the expression of 6810 transcripts, of which 1394 were differentially expressed at levels greater than 1.5-fold or less than 0.75-fold (Fig. 1A, Supplementary Data 1). A range of pathways and processes were found to be significantly enriched in each of the upregulated and downregulated datasets (Figs 2A,B and 3A,B, Supplementary Data 2). Pathways and processes related to epithelial-to-mesenchymal transition (EMT) were enriched in the upregulated dataset, in particular NOTCH signaling and Hedgehog signaling (Figs 2A and 3A). Processes related to cytoskeletal remodeling and cellular junctions, as well as inflammatory responses (IL-2, IL-5, IL-18, CCL2, TNF, IFN, and TGF-β signaling) were also upregulated following infection with C. concisus BAA-1457 (Figs 2A and 3A). In contrast, cystic fibrosis transmembrane conductance regulator (CFTR)-associated pathways, cell cycle processes (S-phase and others), and DNA damage processes were all downregulated following infection (Figs 2B and 3B).
Figure 2. Pathways significantly regulated in intestinal epithelial Caco-2 cells infected with Campylobacter concisus BAA-1457.
Top 30 upregulated (A) and downregulated (B) pathways were selected. Pathways were identified using MetaCore and inverse of log(FDR corrected P-value) was plotted. Full list of top 50 upregulated and downregulated pathways can be found in Supplementary Data 2.
Figure 3. Processes significantly regulated in intestinal epithelial Caco-2 cells infected with Campylobacter concisus BAA-1457.
Top 30 upregulated (A) and downregulated (B) processes were selected. Processes were identified using MetaCore and inverse of log(FDR corrected P-value) was plotted. Full list of top 50 upregulated and downregulated processes can be found in Supplementary Data 2.
In order to identify molecules that could be involved in epithelial recognition of C. concisus BAA-1457, the expression of pattern recognition receptors (PRRs) and related transcripts were examined (Table 2). The expression of PRRs involved in sensing nucleic acids (TLR3 and IFI16) and the NOD-like receptor NLRP9 increased following infection. The expression of the cytokines IL-18, IL-34 and chemokine CCL28 also increased following infection (Table 2).
Table 2. Regulation of important transcripts associated with pattern recognition receptor signaling pathways upon infection with Campylobacter concisus BAA-1457.
| Type | ENSEMBL ID | Gene | Fold regulation | P-value | Adjusted P-value |
|---|---|---|---|---|---|
| ALR | ENSG00000163565 | IFI16 | 1.23 | 0.015 | 0.036 |
| CLR | ENSG00000069493 | CLEC2D | 1.27 | 0.0011 | 0.0038 |
| ENSG00000198178 | CLEC4C | 1.45 | 1.08E-13 | 2.09E-12 | |
| ENSG00000152672 | CLEC4F | 1.32 | 0.017 | 0.040 | |
| NLR | ENSG00000022556 | NLRP2 | 1.11 | 0.0022 | 0.0070 |
| ENSG00000167634 | NLRP7 | 1.21 | 5.05E-08 | 4.44E-07 | |
| ENSG00000185792 | NLRP9 | 2.28 | 7.79E-11 | 1.05E-09 | |
| SLR | ENSG00000161011 | SQSTM1 | 1.17 | 8.24E-06 | 4.73E-05 |
| ENSG00000188554 | NBR1 | 1.20 | 1.56E-07 | 1.26E-06 | |
| ENSG00000123240 | OPTN | 1.18 | 9.07E-06 | 5.16E-05 | |
| TLR | ENSG00000164342 | TLR3 | 1.55 | 2.53E-07 | 1.97E-06 |
| ENSG00000196664 | TLR7 | 0.72 | 0.00033 | 0.0013 | |
| Caspases | ENSG00000106144 | CASP2 | 0.89 | 0.0055 | 0.015 |
| ENSG00000164305 | CASP3 | 0.77 | 1.29E-11 | 1.90E-10 | |
| ENSG00000196954 | CASP4 | 1.16 | 0.00026 | 0.0011 | |
| ENSG00000132906 | CASP9 | 1.29 | 7.47E-07 | 5.28E-06 | |
| Chemokines | ENSG00000151882 | CCL28 | 2.03 | 8.02E-44 | 1.17E-41 |
| ENSG00000107562 | CXCL12 | 0.84 | 2.48E-06 | 1.59E-05 | |
| ENSG00000145824 | CXCL14 | 0.69 | 1.02E-17 | 3.00E-16 | |
| ENSG00000161921 | CXCL16 | 1.42 | 1.86E-09 | 2.06E-08 | |
| Cytokines | ENSG00000136244 | IL6 | 1.20 | 0.010 | 0.026 |
| ENSG00000145839 | IL9 | 0.76 | 0.0011 | 0.0038 | |
| ENSG00000150782 | IL18 | 1.40 | 5.10E-09 | 5.22E-08 | |
| ENSG00000157368 | IL34 | 1.41 | 0.017 | 0.041 | |
| IRF | ENSG00000125347 | IRF1 | 1.16 | 0.00013 | 0.00056 |
| ENSG00000168310 | IRF2 | 0.83 | 0.0073 | 0.020 | |
| ENSG00000126456 | IRF3 | 0.90 | 0.0077 | 0.021 | |
| ENSG00000117595 | IRF6 | 1.30 | 6.88E-13 | 1.20E-11 |
Expression was determined using RNA-seq technology. Results obtained from the EdgeR tool were analysed. A complete list of regulated genes involved in these pathways including cytokine receptors and adaptor molecules can be found in Supplementary Data 1.
ALR: AIM2-like receptors; CLR: C-type lectin receptor; NLR: NOD-like receptor; SLR: sequestosome 1/p62-like receptors; TLR: Toll-like receptor; IRF: Interferon regulatory factors.
The differential expression of genes involved in autophagy was also identified in IECs infected with C. concisus BAA-1457 (Supplementary Data 1). Importantly, the expression of MTOR, a master inhibitor of autophagy, was decreased (0.78-fold) following infection with C. concisus BAA-1457. To further validate the modulation of transcripts within the autophagy pathway, we determined the expression of 84 autophagy-related genes and five housekeeping genes following infection with C. concisus BAA-1457 using an autophagy-specific qPCR array. The average triplicate Ct values arising from infected and non-infected cells were normalised against the housekeeping genes B2M and HPRT1. These housekeeping genes were chosen as they produced the lowest difference in geometric mean between the control and test group. In total, four genes were differentially expressed at statistically significant levels: ATG4A, EIG4G1, MAP1LC3B and MTOR (Table 1). The expression of ATG4A, EIG4G1, and MTOR were all decreased in both datasets, while the expression of MAP1LC3B, which was not found to be modulated in the RNAseq data, was found to be significantly increased in the qPCR data (Table 1).
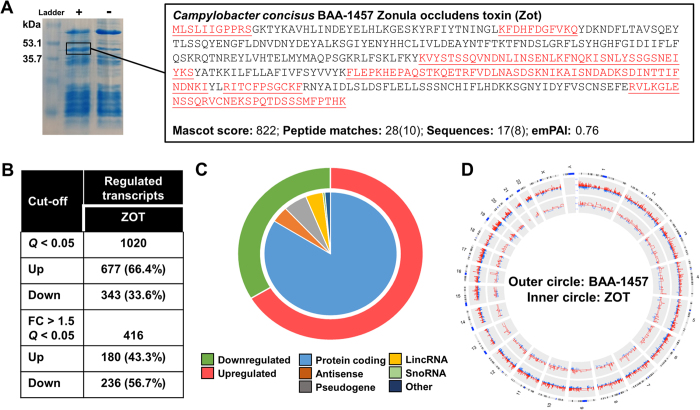
Epithelial response to exposure to Campylobacter concisus zonula occludens toxin
Zonula occludens toxin from C. concisus BAA-1457 was expressed, and its identity subsequently confirmed using mass spectrometry (Fig. 4A). Exposure of IECs to purified ZOT from C. concisus BAA-1457 significantly changed the expression of 1020 transcripts, of which 416 were regulated at levels greater that 1.5-fold or less than 0.75-fold (Fig. 4B, Supplementary Data 1). The majority (66.4%) of significantly differentially expressed transcripts were upregulated (Fig. 4B,C), and 83.9% of the total number of differentially expressed transcripts corresponded to protein coding transcripts (Fig. 4C). However, a substantial proportion of regulated transcripts were antisense or long non-coding RNAs (8.4%, Fig. 4C). Comparison of the IEC response to C. concisus BAA-1457 and purified ZOT suggested that the response to the toxin was more specific (Figs 1A and 4B), while the response to the strain was stronger (Fig. 4D). Of the 1020 transcripts differentially expressed by exposure to ZOT, 555 (54.4%) showed an overlap with the BAA-1457 response (Supplementary Data 1).
Figure 4. Transcriptional regulation in intestinal epithelial Caco-2 cells exposed to zonula occludens toxin.
(A) In vitro expression of ZOT and confirmation of protein identity using mass spectrometry. (B) Number of significantly regulated transcripts following exposure of Caco-2 cells to ZOT. (C) Numbers of upregulated (red) and downregulated (green) transcripts visualised in the outer circle, and types of regulated transcripts visualised independently in the inner circle. (D) Comparison of the responses of Caco-2 cells to C. concisus BAA-1457 (outer circle) and ZOT (inner circle). Transcripts were mapped according to location on human chromosomes. Responses were visualised using circular Circos plot, with transcripts increased in expression in red and those decreased in blue.
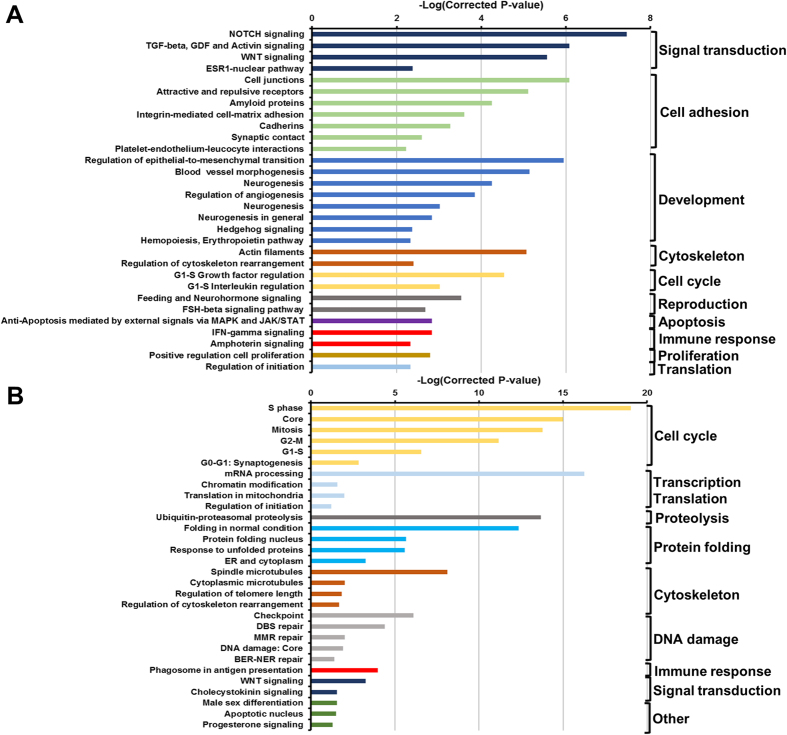
Exposure to ZOT significantly regulated a range of pathways and processes in IECs (Fig. 5A,B, Supplementary Data 2). Similar to the IEC response to C. concisus BAA-1457, processes related to EMT, cytoskeletal remodeling and cellular junctions were upregulated following exposure to ZOT (Fig. 5A,B). Importantly, processes related to cellular junctions and actin filaments were the most enriched within the upregulated dataset (Fig. 5B). Further, a number of inflammatory responses (IL-1, IL-2, IL-3, IL-5, IL-15, and TNF signaling) were also upregulated upon exposure to ZOT (Fig. 5A,B). While several pathways and processes were identified to be significantly downregulated following exposure to ZOT (Supplementary Data 2), the number of transcripts within the pathways identified to be regulated was very low when compared to the total number of transcripts in each of the pathways.
Figure 5. Pathways and processes significantly upregulated in intestinal epithelial Caco-2 cells exposed to zonula occludens toxin.
Top 30 upregulated pathways (A) and processes (B) were selected. Pathways and processes were identified using MetaCore and inverse of log(FDR corrected P-value) was plotted. Full list of top 50 upregulated and downregulated pathways and processes can be found in Supplementary Data 2.
The differential expression of PRRs and related transcripts following exposure to ZOT were examined (Table 3). Interestingly, the expression of both TLR3 and NLRP2 were increased in IECs exposed to ZOT, as was found for IECs infected with C. concisus BAA-1457 (Tables 2 and 3). Further, IECs increased expression of IL6, IL8, and CXCL16 following exposure to ZOT (Table 3), indicating a level of similarity between the IEC response to BAA-1457 and its toxin. However, in contrast to the response to C. concisus BAA-1457, exposure to ZOT did not affect genes involved in autophagy or DNA-sensing IFI16 (Supplementary Data 1), emphasising that these were responses specific to the C. concisus BAA-1457 cells. Of particular relevance to ZOT function, PAR2 expression was significantly increased upon infection with C. concisus BAA-1457 (1.2-fold), and more so upon exposure to purified ZOT (1.6-fold).
Table 3. Regulation of important transcripts associated with pattern recognition receptor signaling pathways upon exposure to C. concisus Zonula occludens toxin.
| Type | ENSEMBL ID | Gene | Fold regulation | P-value | Adjusted P-value |
|---|---|---|---|---|---|
| NLR | ENSG00000022556 | NLRP2 | 1.22 | 0.00046 | 0.012 |
| ENSG00000179873 | NLRP11 | 0.55 | 0.00059 | 0.014 | |
| TLR | ENSG00000164342 | TLR3 | 1.35 | 0.0028 | 0.046 |
| Caspases | ENSG00000165806 | CASP7 | 1.30 | 2.46E-05 | 0.0011 |
| Chemokines | ENSG00000161921 | CXCL16 | 1.39 | 8.79E-05 | 0.0030 |
| Cytokines | ENSG00000136244 | IL6 | 1.68 | 6.03E-06 | 0.00033 |
| ENSG00000169429 | IL8 | 1.44 | 0.00011 | 0.0037 | |
| IRF | ENSG00000125347 | IRF1 | 1.20 | 0.0022 | 0.039 |
Expression was determined using RNA-seq technology. Results obtained from the EdgeR tool were analysed. A complete list of regulated genes involved in these pathways including cytokine receptors and adaptor molecules can be found in Supplementary Data 1.
NLR: NOD-like receptor; TLR: Toll-like receptor; IRF: Interferon regulatory factors.
Validation of the intestinal epithelial responses to Campylobacter concisus strains
We validated in two cell-lines (Caco-2 and HT-29) the changes in expression of a number of genes (MT1E, NPPB, NOTCH3, CYP26A1, HEY1 and CYP1A1) found to be differentially expressed using RNAseq following infection with C. concisus UNSWCD or BAA-1457 (Supplementary Data 3). Overall, there was good concordance between the RNAseq and qPCR data and between the two cell-lines, specifically in their metallothionein, natriuretic peptide, and cytochrome P450 responses. Further, HEY1, a gene involved in EMT, was consistently upregulated in both cell-lines following infection with strain BAA-1457.
A number of similarities were observed in the response to the potential commensal strain ATCC 51561 (NPPB and CYP1A1); however, a number of genes (e.g. MT1E, NOTCH3, CYP26A1, HEY1) found to be differentially expressed by infection with C. concisus UNSWCD or BAA-1457 were not modulated by this strain.
Discussion
Campylobacter concisus, a commensal within the oral cavity, is an emergent opportunistic pathogen of the gastrointestinal tract, having been associated with Barrett’s oesophagus, gastroenteritis, and inflammatory bowel diseases3,4,5,6,7,8,9. A range of virulence mechanisms and factors have been identified in C. concisus strains13,18, which has led to the division of strains into at least two pathotypes, adherent-invasive (AICC) and adherent-toxigenic (AToCC) strains12. Recently, our group comprehensively characterised the response of macrophages to C. concisus strains using RNAseq, identifying DNA sensing as an important mechanism by which host immune cells recognise C. concisus19. However, despite an increase in our understanding of the virulence mechanisms and immune response to C. concisus, the epithelial response to the bacterium remains poorly understood.
Thus, the responses of IECs to either AICC or AToCC strains were determined using RNAseq. Large-scale differences in the responses of IECs to each of the pathotypes were observed, with the AToCC strain inducing a significantly larger response upon infection of IECs. We have previously found that C. concisus UNSWCD (AICC) can invade IECs and survive intracellularly, while C. concisus BAA-1457 (AToCC) can internalise into IECs but is cleared from the intracellular environment by autophagy15. These findings would suggest that AICC strains appear to avoid detection by IECs, and their ensuing protective response, allowing them to establish a niche intracellularly. However, despite the lack of a strong epithelial response to C. concisus UNSWCD, an AICC strain, a specific protective response was still observed. For example, the upregulation of IKBKE following infection with C. concisus UNSWCD would suggest non-canonical activation of NF-κB20, which supports our previous observation of NF-κB activation in IECs exposed to AICC strains18. Moreover, a strong oxidative stress response in the form of increased expression of metallothioneins and other antioxidant enzymes, as well as the upregulation of xenobiotic metabolism (CYP1A1 and CYP1B1) were found following infection with C. concisus UNSWCD.
In contrast, C. concisus BAA-1457 (AToCC), which produces a zonula occludens toxin, does not avoid detection by IECs, but rather induced a strong epithelial response. This is further emphasised by the decreased expression of MTOR and EIF4GI following infection with C. concisus BAA-1457, both of which are inversely associated with activation of autophagy21. Further, IECs significantly increased expression of two nucleic acid sensing PRRs, TLR3 and IFI16, following infection with C. concisus BAA-1457, which is suggestive of bacterial lysis within the host cell. Notably, increased expression of IFI16 and the formation of the IFI16 inflammasome were observed in immune cells infected with C. concisus BAA-145719, highlighting the importance of host DNA sensing in the recognition of certain C. concisus strains.
In addition to the above PRRs, we also observed a small increase in the IEC expression of NLRP2 following both infection with C. concisus BAA-1457, as well as exposure to the purified ZOT. Interestingly, NLRP2 has been found to mediate the production of β-defensins in gingival epithelial cells infected with Fusobacterium nucleatum22.
Infection with C. concisus BAA-1457 significantly modulated several pathways associated with CFTR, which was not observed in IECs exposed to C. concisus ZOT. Given that Vibrio cholerae targets CFTR through the cholera toxin present on the CTX prophage, which also comprises a zonula occludens toxin23,24, it is conceivable that C. concisus BAA-1457 may have acquired through horizontal gene transfer additional toxins capable of targeting CFTR at the time of acquiring ZOT. Analysis of the C. concisus genome suggests ZOT is present on an incomplete prophage25, thus, proteins within this prophage would serve as possible candidates.
Campylobacter concisus BAA-1457 was also found to upregulate a range of pathways and processes associated with EMT, as well as IGF family signaling in colorectal cancer. Further, the strain isolated from a healthy individual (ATCC 51561) did not appear to upregulate EMT. Notably, studies have found that Campylobacter species are among a polymicrobial signature of Gram-negative bacteria (including Fusobacterium) that are enriched in colorectal cancer patient samples26,27, suggesting that the presence of some types of C. concisus strains in the gut may have the potential to promote functions associated with carcinogenesis. Moreover, a similar polymicrobial signature comprising Campylobacter and Fusobacterium species is enriched in patients in the early stages of the oesophageal adenocarcinoma cascade (gastro-oesophageal reflux disease and Barrett’s oesophagus)4. Thus, it would be interesting to determine if some C. concisus strains can regulate EMT in oesophageal epithelial cells.
Processes associated with cytoskeletal remodeling and cellular tight junctions were among the most significantly enriched within the upregulated transcripts in IECs infected with C. concisus BAA-1457, as well as C. concisus ZOT. C. concisus strains have been previously shown to modulate the expression of some tight junction proteins17, and invade IECs through a paracellular mechanism10. Further, it is well established that Vibrio cholerae ZOT targets the tight junctions of IECs and induces disassembly28. More recently, this was found to occur through a mechanism that involves the activation of proteinase activated receptor 2, PAR229. Importantly, infection with C. concisus BAA-1457 and exposure to C. concisus ZOT increased the expression of PAR2 (F2RL1) in IECs (1.21- and 1.58-fold, respectively) in this study. Taken together, these findings would suggest that C. concisus strains possessing ZOT can target intestinal cellular junctions, as has been observed in other bacterial species possessing this toxin.
In addition to this, purified ZOT was also found to increase the expression of the executioner caspase, CASP7. C. concisus strains isolated from the oral cavity and faecal samples have previously been shown to induce apoptosis in intestinal epithelial HT-29 cells10. Given the role of caspase 7 in apoptosis30,31, this would suggest that ZOT may promote apoptosis in IECs. This view is supported by upregulation of pro-apoptotic TNF-family pathways and processes associated with death domain receptors and caspases following exposure of IECs to ZOT. Interestingly, the expression of CXCL16, a chemokine that promotes TNF-induced apoptosis in macrophages32 was found to be increased in IECs both following infection with C. concisus BAA-1457 and upon exposure to ZOT. However, the expression of anti-apoptotic cytokines IL6 and IL8, as well as a number of processes related to cell cycle were also significantly increased in IECs exposed to ZOT, suggesting dual activation of competing pathways. Given this, further work is required to clarify the ability and the possible mechanism by which C. concisus, and its virulence factor ZOT, may induce cell death. Upregulated transcripts such as CXCL16 and those within the identified pro-apoptotic pathways may provide insights into this.
This work is not without limitations. Give the costs associated with human RNAseq, global gene expression profiles were analysed using RNAseq for only two C. concisus strains. Future studies examining the epithelial responses to a range of clinical and commensal isolates across different time-points would help advance our understanding of the host response to C. concisus. While confirmation of gene expression was performed in an additional intestinal epithelial cell-line (HT-29), it would also be beneficial to examine the global response of HT-29 cells, other intestinal epithelial cell-lines (e.g. mucus-producing LS174T cells), and primary intestinal epithelial cells using RNAseq. Further, different RNAseq technologies were employed to examine the epithelial responses to C. concisus BAA-1457 and ZOT. While the consistency in the responses suggests good concordance across technologies, it does not rule out the possibility that this may influence assessment of gene expression, particularly for non-coding RNAs.
In conclusion, we comprehensively examined the response of the intestinal epithelial cell-line Caco-2 to C. concisus, observing major differences between strains possessing distinct virulence mechanisms. A range of important molecules, pathways and processes that were significantly modulated by this bacterium were identified, thus, providing insights into mechanisms by which C. concisus may cause disease. Of particular interest is the ability of C. concisus to affect processes related to epithelial-to-mesenchymal transition (NOTCH and Hedgehog signaling), given that this bacterium has been suggested to play a role in Barrett’s oesophagus4. We also comprehensively studied the response of the intestinal epithelial cell-line Caco-2 to purified C. concisus ZOT, providing evidence that this toxin modulates processes related to cytoskeletal remodeling and cellular tight junctions. This information will serve as a strong basis for future studies addressing the effect of C. concisus on epithelial cells, and the role of this bacterium in gastrointestinal disease.
Methods
Bacterial culture
Camyplobacter concisus strains BAA-1457, UNSWCD, ATCC 51561 and UNSW3 were cultured on Horse Blood Agar (HBA), comprising Blood Agar Base 2 (Oxoid) supplemented with 7% defibrinated horse blood (Oxoid), and incubated for 24–48 h at 37 °C under a microaerobic environment enriched with H2. This atmospheric condition was generated using CampyGen and CO2Gen gas generating kits (Oxoid) and 0.2 M of sodium borohydride (Sigma Aldrich) dissolved in 10 ml water.
Expression of Zonula Occludens Toxin from C. concisus BAA-1457
ZOT was expressed following the procedures outlined for the PURExpress In Vitro Protein Synthesis kit (NEB #E6800; New England Biolabs). Briefly, C. concisus BAA-1457 DNA was extracted using the Puregene Core Kit A (Qiagen) according to the manufacturer’s instructions. A linear DNA template containing a T7 promoter sequence, ribosomal binding site (RBS), and the zot gene sequence was amplified using a two-step PCR protocol. The first PCR generated a template containing the RBS and zot gene using the F1-zot (5′-TAACTTTAAGAAGGAGATATACCAATGCTTAGTTTGATTATCGGTCC) and R1-zot (5′-TATTCACTACTTGTGAGTAGGAAACATAG) primers. This fragment was purified and a second PCR using the primer pair F2-zot (5′-GCGAATTAATACGACTCACTATAGGGCTTAAGTATTAACTTAAGGAGATATACCA) and R2-zot (5′-AAACCCCTCCGTTTAGAGAGGGGTTATATTCACTACTTGTGAGTAGGAA) was performed to generate the final template containing the T7 promoter site before the RBS site and a loop structure following the stop codon. The template was purified and employed to express the ZOT protein using the PURExpress In Vitro Protein Synthesis kit according to the manufacturer’s instructions. ZOT was purified using a reverse His-tag purification protocol as outlined by the manufacturer. The purified protein was run on a SDS-PAGE gel, excised from the gel, trypsin digested, and analysed on an Orbitrap Velos ETD (Thermo Electron) mass spectrometer as previously described19.
Mammalian cell culture and infection
Caco-2 cells (American Type Culture Collection: HTB-37) were passaged in Minimal Essential Media (MEM) (Life Technologies), supplemented with 10% v/v Fetal Bovine Serum (FBS) (Bovogen), 1 mM sodium pyruvate, 0.1 mM non-essential amino acids, 2.25 mg l−1 sodium bicarbonate and 100 μg ml−1 penicillin and streptomycin (Life Technologies), and incubated at 37 °C, with 5% CO2. Cell culture medium was replaced every 3–4 days, and cells were passaged approximately every week. HT-29 cells were passaged in McCoy’s 5A Medium Modified (Life Technologies), supplemented with 10% v/v FBS and 100 μg ml−1 penicillin and streptomycin, and incubated at 37 °C, with 5% CO2. Cell culture medium was replaced every 2 days, and cells were passaged after approximately 5–7 days.
For bacterial infection, Caco-2 or HT-29 cells in antibiotic-free cell culture media were seeded in a 24-well plate (Thermo Fisher Scientific) at a concentration of 1 × 106 cells ml−1 and incubated for 48 h at 37 °C with 5% CO2. Cells were then infected in triplicate with either C. concisus BAA-1457, UNSWCD or UNSW3 at a Multiplicity of Infection (MOI) of 200, or purified ZOT at a concentration of 30 nM. After a 6 h infection period, infected monolayers were washed once with 1 ml DPBS and then RNA extraction was performed using the Isolate II RNA Extraction Mini Kit (Bioline) according to the manufacturer’s instructions. The concentration and quality of extracted RNA was assessed using a NanoDrop ND-1000 (Thermo Fisher Scientific) and stored at −80 °C.
Library preparation, RNA sequencing and data analysis
For C. concisus UNSWCD and BAA-1457, Illumina TruSeq RNA Sample Prep Kit (version 3) was used according to the manufacturer’s instructions for RNA-Seq sample preparation, with 2 μg of total RNA being used per sample (three biological replicates per condition). The libraries were PCR enriched (15 cycles and insert size range: 80 to 330 bp). Six libraries were multiplexed in each lane, using randomisation to control for bias. Libraries were then sequenced on the HiSeq 2000, at the Ramaciotti Centre for Genomics at the University of New South Wales, using TruSeq v3 SBS reagents to generate 100 bp paired-end reads (UNSWCD: Control: 40842678 ± 1799916; Infected: 36991969 ± 1083140; BAA-1457: Control: 38041062 ± 835723; Infected: 35510220 ± 1124242).
For ZOT, the RNA samples were prepared with Illumina TruSeq Stranded Total RNA Kit (Ribozero) using 1 μg of total RNA as input (three biological replicates per condition). The samples were ribosomal RNA depleted as per the manufacturer’s instructions. The libraries were amplified using 12 cycles of PCR. Six libraries were run on a NextSeq500 75 bp PE High Output run (Control: 88799846 ± 8046210; ZOT: 94967481 ± 3083486 paired-end reads).
Sequencing reads were quality checked, filtered, trimmed, and mapped against the human genome as previously described19. BioConductor package EdgeR v2.4.633 was used in the R programming environment to identify genes that were significantly differentially expressed between the conditions, following standard normalisation procedures. Data were analysed for regulated pathways and processes using Metacore (Thomson Reuters), and genome-wide transcriptional regulation was visualised using Circos34. All RNAseq raw data has been deposited in NCBI Gene Expression Omnibus (GSE84338).
Autophagy PCR arrays and qPCR validation
cDNA was synthesised from extracted RNA using the RT2 First Strand cDNA synthesis kit (Qiagen) according to the manufacturer’s instructions. The concentration and quality of cDNA was assessed using a NanoDrop ND-1000. The cDNA mastermix was prepared using RT2 SYBR Green ROX FAST Mastermix (Qiagen) according to the manufacturer’s instructions and loaded onto a Human Autophagy RT2 ProfilerTM PCR Array (Catalogue No. PAHS-084ZR). Twenty microlitres of cDNA mastermix was loaded into each well of the array, and the array was then sealed using Rotor-Disc Heat-Sealing Film (Qiagen) and a Rotor Disc Heat Sealer (Qiagen). The qPCR was performed using a Rotor Gene Q PCR cycler (Qiagen) under the following cycling conditions: 95 °C for 10 min, 40 cycles of 95 °C for 10 s and 60 °C for 30 s (with acquisition of data occurring during this step), followed by melting curve analysis to verify PCR specificity. The CT threshold was determined manually according to the manufacturer’s recommendations. Data were analysed using online analysis software provided by the manufacturer (Qiagen) using the 2−ΔΔCT method following normalisation against housekeeping gene(s) (Actin beta, ACTB; Beta-2-microglobulin, B2M; Glyceraldehyde-3-phosphate dehydrogenase, GADPH; Hypoxanthine phosphoribosyltransferase 1, HPRT1; Ribosomal protein large P0, RPLP0). Quality controls were included within the PCR array to test for reproducibility, reverse transcriptase efficiency and human genomic DNA contamination. Three biological replicates were analysed per condition. Methods for additional qPCR validation of RNAseq data are available in Supplementary Data 3.
Additional Information
How to cite this article: Deshpande, N. P. et al. Campylobacter concisus pathotypes induce distinct global responses in intestinal epithelial cells. Sci. Rep. 6, 34288; doi: 10.1038/srep34288 (2016).
Supplementary Material
Acknowledgments
This work was supported by a Cancer Institute NSW Career Development Fellowship (15/CDF/1-11 to N.O.K.). M.R.W. and N.P.D. acknowledge funding from the Australian Federal Government NCRIS Scheme, the New South Wales State Government RAAP Scheme and the University of New South Wales. H.M.M. receives funding from the Ministry of Higher Education, Malaysia (UM.C/625/HIR/MOHE/CHAN/13/1).
Footnotes
Author Contributions N.O.K., N.P.D., M.R.W. and H.M.M. conceived the idea; H.M.M., M.R.W., S.M.R. and N.O.K. contributed reagents and funds; N.P.D. and N.O.K. performed the RNA-seq experiments and analysed the data; N.O.K. and N.S. expressed and purified ZOT; E.B. and N.C.-R. performed the Autophagy PCR array experiments and analysed the data; N.O.K. drafted the manuscript; N.O.K., N.P.D., M.R.W., H.M.M., N.C.-R., S.M.R., E.B. and N.S. read, corrected, and approved the manuscript.
References
- Kaakoush N. O. & Mitchell H. M. Campylobacter concisus - A new player in intestinal disease. Front. Cell. Infect. Microbiol. 2, 4 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L. et al. Isolation and detection of Campylobacter concisus from saliva of healthy individuals and patients with inflammatory bowel disease. J. Clin. Microbiol. 48, 2965–2967 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackett K. L. et al. Oesophageal bacterial biofilm changes in gastro-oesophageal reflux disease, Barrett’s and oesophageal carcinoma: association or causality? Aliment. Pharmacol. Therap. 37, 1084–1092 (2013). [DOI] [PubMed] [Google Scholar]
- Kaakoush N. O., Castano-Rodriguez N., Man S. M. & Mitchell H. M. Is Campylobacter to esophageal adenocarcinoma as Helicobacter is to gastric adenocarcinoma? Trends Microbiol. 23, 455–462 (2015). [DOI] [PubMed] [Google Scholar]
- Kaakoush N. O., Castano-Rodriguez N., Mitchell H. M. & Man S. M. Global Epidemiology of Campylobacter Infection. Clin. Microbiol. Rev. 28, 687–720 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen H. L., Ejlertsen T., Engberg J. & Nielsen H. High incidence of Campylobacter concisus in gastroenteritis in North Jutland, Denmark: a population-based study. Clin. Microbiol. Infect. 19, 445–450 (2013). [DOI] [PubMed] [Google Scholar]
- Nielsen H. L., Engberg J., Ejlertsen T., Bucker R. & Nielsen H. Short-term and medium-term clinical outcomes of Campylobacter concisus infection. Clin. Microbiol. Infect. 18, E459–465 (2012). [DOI] [PubMed] [Google Scholar]
- Castano-Rodriguez N., Kaakoush N. O., Lee W. S. & Mitchell H. M. Dual role of Helicobacter and Campylobacter species in IBD: a systematic review and meta-analysis. Gut, 10.1136/gutjnl-2015-310545 (2015). [DOI] [PubMed] [Google Scholar]
- Kirk K. F., Nielsen H. L., Thorlacius-Ussing O. & Nielsen H. Optimized cultivation of Campylobacter concisus from gut mucosal biopsies in inflammatory bowel disease. Gut Pathog. 8, 27 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Man S. M. et al. Host attachment, invasion, and stimulation of proinflammatory cytokines by Campylobacter concisus and other non-Campylobacter jejuni Campylobacter species. J. Infect. Dis. 202, 1855–1865 (2010). [DOI] [PubMed] [Google Scholar]
- Kaakoush N. O. et al. Campylobacter concisus and exotoxin 9 levels in paediatric patients with Crohn’s disease and their association with the intestinal microbiota. J. Med. Microbiol. 63, 99–105 (2014). [DOI] [PubMed] [Google Scholar]
- Kaakoush N. O., Mitchell H. M. & Man S. M. Role of emerging Campylobacter species in inflammatory bowel diseases. Inflamm. Bowel Dis. 20, 2189–2197 (2014). [DOI] [PubMed] [Google Scholar]
- Kaakoush N. O. et al. The secretome of Campylobacter concisus. FEBS J. 277, 1606–1617 (2010). [DOI] [PubMed] [Google Scholar]
- Fasano A. et al. Zonula occludens toxin modulates tight junctions through protein kinase C-dependent actin reorganization, in vitro. J. Clin. Invest. 96, 710–720 (1995). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgos-Portugal J. A., Mitchell H. M., Castano-Rodriguez N. & Kaakoush N. O. The role of autophagy in the intracellular survival of Campylobacter concisus. FEBS Open Bio 4, 301–309 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deshpande N. P., Kaakoush N. O., Wilkins M. R. & Mitchell H. M. Comparative genomics of Campylobacter concisus isolates reveals genetic diversity and provides insights into disease association. BMC Genomics 14, 585 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen H. L. et al. Oral and fecal Campylobacter concisus strains perturb barrier function by apoptosis induction in HT-29/B6 intestinal epithelial cells. PLoS One 6, e23858 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaakoush N. O. et al. The pathogenic potential of Campylobacter concisus strains associated with chronic intestinal diseases. PLoS One 6, e29045 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaakoush N. O. et al. Transcriptomic and proteomic analyses reveal key innate immune signatures in the host response to the gastrointestinal pathogen Campylobacter concisus. Infect. Immun. 83, 832–845 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koop A. et al. Novel splice variants of human IKKepsilon negatively regulate IKKepsilon-induced IRF3 and NF-kB activation. Eur. J. Immunol. 41, 224–234 (2011). [DOI] [PubMed] [Google Scholar]
- Ramirez-Valle F., Braunstein S., Zavadil J., Formenti S. C. & Schneider R. J. eIF4GI links nutrient sensing by mTOR to cell proliferation and inhibition of autophagy. J. Cell Biol. 181, 293–307 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji S. et al. Toll-like receptor 2 and NALP2 mediate induction of human beta-defensins by Fusobacterium nucleatum in gingival epithelial cells. Infect. Immun. 77, 1044–1052 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd E. F., Moyer K. E., Shi L. & Waldor M. K. Infectious CTXPhi and the vibrio pathogenicity island prophage in Vibrio mimicus: evidence for recent horizontal transfer between V. mimicus and V. cholerae. Infect. Immun. 68, 1507–1513 (2000). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabriel S. E., Brigman K. N., Koller B. H., Boucher R. C. & Stutts M. J. Cystic fibrosis heterozygote resistance to cholera toxin in the cystic fibrosis mouse model. Science 266, 107–109 (1994). [DOI] [PubMed] [Google Scholar]
- Zhang L. et al. Campylobacter concisus and inflammatory bowel disease. World J. Gastroenterol. 20, 1259–1267 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren R. L. et al. Co-occurrence of anaerobic bacteria in colorectal carcinomas. Microbiome 1, 16 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu N. et al. Dysbiosis signature of fecal microbiota in colorectal cancer patients. Microbial Ecol. 66, 462–470 (2013). [DOI] [PubMed] [Google Scholar]
- Fasano A. et al. Vibrio cholerae produces a second enterotoxin, which affects intestinal tight junctions. P. N. A. S. 88, 5242–5246 (1991). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldblum S. E. et al. The active Zot domain (aa 288-293) increases ZO-1 and myosin 1C serine/threonine phosphorylation, alters interaction between ZO-1 and its binding partners, and induces tight junction disassembly through proteinase activated receptor 2 activation. FASEB J. 25, 144–158 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirata H. et al. Caspases are activated in a branched protease cascade and control distinct downstream processes in Fas-induced apoptosis. J. Exp. Med. 187, 587–600 (1998). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh J. G. et al. Executioner caspase-3 and caspase-7 are functionally distinct proteases. P. N. A. S. 105, 12815–12819 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kee J. Y. et al. CXCL16 suppresses liver metastasis of colorectal cancer by promoting TNF-alpha-induced apoptosis by tumor-associated macrophages. BMC Cancer 14, 949 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson M. D., McCarthy D. J. & Smyth G. K. edgeR: a Bioconductor package for differential expression analysis of digital gene expression data. Bioinformatics 26, 139–140 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krzywinski M. et al. Circos: an information aesthetic for comparative genomics. Genome Res. 19, 1639–1645 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.