Abstract
Despite the vast improvement in techniques and technology for arthroscopic rotator cuff surgery, repairs of massive and large tears remain challenging because they are associated with significantly high failure rates. In recent years, patch augmentation has gained popularity as a technique to decrease these high failure rates. Arthroscopic patch augmentation of rotator cuff repair, however, is technically difficult. The purpose of this report is to describe a simple and reproducible technique for all-arthroscopic extracellular matrix graft augmentation. With this technique, which we refer to as the “owl” technique because the prepared extracellular augment resembles an owl, there are relatively few suture ends involved; therefore, augment introduction is straightforward with a reduced risk of suture ends becoming tangled. In addition, the way in which our augmentation is prepared helps to prevent it from becoming bunched up when being secured.
Despite vast advances in technology and arthroscopic rotator cuff techniques, the failure rate may be in excess of 60% for elderly patients who undergo large or massive rotator cuff repair.1 Most of these failures occur at the tendon-bone interface due to intrinsic degenerative changes in the tendon and excessive repair-site tension.2 As a result, researchers have focused on strategies that decrease the tension of the repair and also provide a favorable biological environment to optimize tendon-bone healing. One approach that has gained popularity is the use of extracellular matrix–derived material to augment the repair.3, 4, 5
Arthroscopic augmentation, however, is technically challenging, difficult to reproduce consistently, and time-consuming. Part of this challenge is because of the difficulties in introducing and securing the augment in the desired orientation. In addition, it can be difficult to prevent the patch from folding and bunching when one is securing the augment. Suture management can also be difficult because the space becomes tight with the insertion of the augment and sutures can become tangled. The aim of this report is to describe a consistently reproducible technique that simplifies passage and securing of the graft with decreased risk of the augment bunching up and tangling of sutures (Table 1, Table 2, Table 3, Table 4, Table 5, Table 6).
Table 1.
Key Points
| Extracellular matrix augmentation of large and massive rotator cuff tears may decrease repair failure rates. |
| Arthroscopic augmentation is technically challenging. |
| Our technique addresses some of the challenges involved in the introduction and securing of the augment by reducing the risks of the sutures become tangled and the augmentation bunching up and folding. |
Table 2.
Indications and Contraindications
| Indications |
| Large and massive rotator cuff tears |
| Rotator cuff tears with poor-quality tissue |
| Contraindications |
| Irreparable rotator cuff tears |
| Glenohumeral joint arthritis |
| Active infection or history of shoulder infection |
Table 3.
Surgical Steps of Owl Technique
| 1. Diagnostic glenohumeral joint arthroscopy is performed. |
| 2. The arthroscope is introduced into the bursa. |
| 3. Bursectomy is performed. |
| 4. To preserve the coracoacromial ligament, no acromioplasty is performed. |
| 5. Acromioclavicular excision is performed to address acromioclavicular joint tenderness. |
| 6. Mobilization of the rotator cuff tear is performed. |
| 7. Preparation of the greater tuberosity is performed (Fig 1A). |
| 8. One or 2 medial-row anchors are inserted depending on the anatomy of the tear (Fig 1B). |
| 9. The anchor sutures are passed through the torn rotator cuff tendon (4 passes with 1 anchor or 8 passes with 2 anchors) (Figs 1C and D and 2). |
| 10. Knots are tied to complete the standard medial-row repair (Figs 2 and 3A). |
| 11. The suture ends that are not going to be passed through the augment are cut. |
| 12. The distance between the knots is measured (Fig 3, Fig 4, and 5). |
| 13. The augment is prepared. |
| 14. The suture ends are brought out through the lateral portal and passed through the augment. |
| 15. The augment is rolled over itself and is pushed through the lateral portal cannula as the suture ends are tensioned outside. |
| 16. Once the augment is inside, it is laid open and flat. |
| 17. Medial anchor suture limbs are brought over the augment. |
| 18. Medial anchor suture limbs are passed through 2 lateral-row anchors. |
| 19. The augment is secured by insertion of the lateral-row anchors. |
| 20. If necessary, the augment can be further secured by tying it to the rotator cuff using a free suture. |
Table 4.
Advantages
| Relatively few suture limbs are involved. |
| There is a reduced risk of the suture ends becoming tangled. |
| Introduction of the augment is straightforward. |
| There is a reduced risk of the augment bunching up and folding when the surgeon is securing the augment. |
| If, for any reason, the surgeon cannot insert and secure the augment in the desired situation, then it is very easy to remove the augment and carry on with the double-row repair. |
Table 5.
Risks
| Risks related to standard arthroscopic rotator repair |
| Inflammatory response to augment |
| Infection |
Table 6.
Pearls and Pitfalls
| Pearls |
| Adequate bursectomy, release, and tendon mobilization must be performed. |
| Before insertion of the augment, it is best to mark the augment so that the surgeon will be able to tell which edge of the tendon is medial, lateral, anterior, and posterior, as well as which surface is the top surface, once the augment is in the bursa. |
| A 10-mm-diameter cannula should be used to insert the augment. |
| Pitfalls |
| In the absence of adequate bursectomy, visualization becomes difficult and the augment will not lay open flat. |
| In the absence of marking, if the augment rotates or twists inside the subacromial space, it may be difficult to rotate or untwist the augment to obtain the correct orientation. |
| Using smaller-diameter cannulas may cause difficulties with augment insertion. |
Surgical Technique
The procedure is performed with the patient under general anesthesia combined with an interscalene block and positioned in either the beach-chair or lateral decubitus position. We introduce the arthroscope through the standard posterior viewing portal to perform a diagnostic arthroscopy. The arthroscope is then introduced into the subacromial space through the posterior port. A standard lateral arthroscopic port is created. The tear is identified, and a thorough bursectomy is performed. We do not routinely perform acromioplasty because we want to preserve the coracoacromial ligament; however, if the patient has acromioclavicular joint tenderness, acromioclavicular joint excision is performed before we proceed with repair.
Standard Repair of Cuff Tear
Comprehensive mobilization of the tear is performed with release of the adhesion both superficial and deep to the tendon (Video 1). The mobility of the tendon is then assessed. Matrix augmentation is only considered if we believe that the tear is repairable because we do not use the matrix to bridge the gap between the tendon edge and the greater tuberosity.
The footprint area on the greater tuberosity is prepared with a shaver so that the bone bleeds slightly; however, the tuberosity is not decorticated, and the cortex is not violated (Fig 1A). Depending on the size of the tear, a decision is then made on whether to use 1 or 2 medial-row anchors. For the medial-row anchors, we use double-loaded PEEK (polyether ether ketone) 5.5-mm anchors (Helicoil PEEK; Smith & Nephew, Andover, MA). The first medial-row anchor (or the only medial-row anchor if only such anchor is used) is inserted using the accessory anterior portal (Fig 1B). For simplicity, the suture ends of one of the sutures of this anchor are labeled 1 and 2 and those of the second suture are labeled 3 and 4. A cannula is then passed through the lateral portal (Passport, 10 mm × 4.5 cm; Arthrex, Naples, FL). Suture end 1 is passed through the anterior tendon edge using the Scorpion device (Arthrex). This suture end is brought out through the anterior portal and parked. Suture end 2 is then passed through the tendon in a similar manner 0.5 cm posterior to suture end 1 and is parked in the same manner. Similarly, suture ends 3 and 4 are passed through the tendon posterior to suture end 2 and parked (Figs 1C and D and 2).
Fig 1.
Greater tuberosity preparation (A), medial-row anchor insertion (B), and passage of suture limbs through cuff (C, D). The arthroscope is in the posterior port, viewing the bursa in a left shoulder.
Fig 2.
Rotator cuff repair: medial row. The technique is performed with either 1 medial-row anchor with 4 passes through the torn tendon (A) or 2 medial row anchors with 8 passes through the torn tendon (B).
Depending on the anatomy and dimensions of the tear, the surgeon may elect to use a second medial-row anchor. In such cases this second anchor is inserted through an accessory lateral portal at least 1 cm posterior to the first medial-row anchor. For simplicity, the suture ends of one of the sutures of this anchor are labeled 5 and 6 and those of the second anchor suture are labeled 7 and 8. These suture ends are passed into the cuff and parked in the anterior accessory portal in a similar manner to suture ends 1 to 4 (Fig 2B). After this, suture ends 7 and 8 are brought out through the lateral portal (through the Passport cannula). These are tied to each other using a standard arthroscopic knot-tying technique and then parked. Similarly, suture ends 5 and 6, suture ends 3 and 4, and suture ends 2 and 1 are tied (Figs 2 and 3A).
Fig 3.
Knots of the medial-row anchors (A) and measurement of the distance between the 2 tied knots (B). The arthroscope is in the posterior port, viewing the bursa in a left shoulder.
If 2 medial-row anchors are used, suture ends 3 through 6 are then cut 2 mm distal to the knot (Fig 4). If only 1 medial-row anchor is used, no suture ends are cut. Then, by use of an arthroscopic measuring device or an arthroscopic hook, the distance between the suture 1 and 2 knot and the suture 7 and 8 knot is measured in cases in which 2 medial-row anchors are used whereas the distance between the suture 1 and 2 knot and the suture 3 and 4 knot is measured if only 1 medial-row anchor is used (distance c) (Figs 3B and 5).
Fig 4.

Medial-row repair with 2 anchors. Suture ends 3 and 4 and suture ends 5 and 6 are cut.
Fig 5.
Planning of augmentation. (A) If only 1 anchor is used, the distance between the suture 1 and 2 knot and the suture 3 and 4 knot (distance c) is measured. (B) If 2 medial-row anchors are used, the distance between the suture 1 and 2 knot and the suture 7 and 8 knot (distance c) is measured.
Preparation of Augment Outside Patient
Next, the augment is prepared. By use of an 18-gauge spinal needle, 2 holes are made through the augment (Arthrex Dx Reinforcement Matrix) (Fig 6). The distance between these 2 holes (labeled c) must be the same as the measured distance between the suture 1 and 2 knot and the suture 3 and 4 knot when 1 medial-row anchor is used (or the distance between the suture 1 and 2 knot and the suture 7 and 8 knot when 2 medial-row anchors are used). The length of the patch (the distance between the anterior and posterior edges of the augment, labeled l) is dependent on the size of the tear, but the holes must be at least 5 mm from these edges (distance a). Similarly, the width of the augment (the distance between the medial and lateral edges of the augment, labeled w) is dependent on the tear size, but it must be at least 2 cm and the holes must be at least 1 cm from the top edge (medial border) of the augment (distance b).
Fig 6.
Preparation of augment. Distance a must be at least 5 mm, distance b must be at least 10 mm, and width (w) must be at least 2 cm.
One of the challenges of augmentation is folding of the augment while the surgeon is securing it to the cuff and the greater tuberosity. To decrease the risk of fold formation, some adjustments are made to the rectangular patch (Figs 7 and 8). First, the corners are cut so that one is left with an octagon. Then, an inverted triangular cut is made along the top border of the augment. The prepared augment resembles an owl, hence the name of the technique.
Fig 7.
Forming of owl-shaped augment. First, the corners are cut so that one is left with an octagon. Then, an inverted triangular cut is made along the top border of the augment.
Fig 8.
Suture passage through the augment before the augment is inserted. Suture ends 3 and 4 are passed through the posterior hole on the augment. Suture ends 1 and 2 are passed through the anterior augment hole. These are performed outside the patient. The top surface and the medial end of the augment are marked so that orientation becomes easier once the augment is in the bursa.
Insertion of Augment
The next task is insertion of the augment (Video 1). First, suture ends 3 and 4 are brought out through the lateral port through the Passport cannula (or sutures 7 and 8 when 2 medial-row anchors are used). These 2 suture ends are passed through the posterior hole on the augment (Fig 9). Next, suture ends 1 and 2 are brought out through the lateral port and are passed through the anterior augment hole (Fig 9). All suture passages through the tendon are performed outside the shoulder.
Fig 9.
Passage and securing of augment. Suture ends 3 and 4 (if 1 medial-row anchor is used) or suture ends 7 and 8 (if 2 medial-row anchors are used) are passed through the posterior hole on the augment. Suture ends 1 and 2 are passed through the anterior augment hole.
The augment is rolled over itself to pass it through the Passport cannula. The rolled augment is then pushed through the Passport cannula into the subacromial space by use of an artery clip (Fig 10A). The risk of suture tangling is reduced by tensioning the suture ends outside the patient at the same time. Once the augment is inside the subacromial space, it is laid open flat using a blunt obturator (Fig 10B).
Fig 10.
Passage and securing of augment. (A) The augment is rolled over itself and is pushed through the lateral portal cannula as the suture ends are tensioned outside. (B) Once the augment is inside, it is laid open and flat. (C) Medial anchor suture limbs are brought out over the augment and are then passed through 2 lateral-row anchors. (D) The augment is secure by insertion of the lateral-row anchors. The arthroscope is in the posterior port, looking at the bursa in a left shoulder. The patient is in the lateral position but the arthroscope is orientated so that the superior part of the image presents the superior part of the patient.
Securing of Augment Over Cuff
Once the augment is laid flat, the distal part of the greater tuberosity is prepared for insertion of 2 lateral-row anchors (second-row anchors) (we use 5.5-mm SwiveLock SP [Arthrex]) (Video 1). One of these 2 lateral-row anchors will be inserted anteriorly and the other one posteriorly. A transosseous-equivalent suture bridge technique is then used to insert the lateral-row anchors incorporating the augment into the construct. This involves passing the medial-row anchor's suture ends over the laid-flat augment and then through the 2 lateral-row anchors, which are in turn inserted into the distal part of the greater tuberosity. The anterior lateral-row anchor is inserted first with suture ends 1 and 4 from the medial-row anchor (or suture ends 1 and 8 if 2 medial-row anchors are used) (Figs 9 and 10C and D). This is followed by insertion of the posterior lateral-row anchor with suture ends 2 and 3 if only 1 medial-row anchor is used (or with suture ends 2 and 7 if 2 medial-row anchors are used) (Fig 6). With this technique, the augment is secured as the medial-row anchor suture ends are tensioned during the lateral-row anchor insertion. The tensioned sutures on top of the augment will help to secure it down (Figs 9 and 11). If needed, the augment can be further secured by passing a free suture (FiberWire; Arthrex) through the rotator cuff and then through the augment, after which a knot can be tied. In our series this was rarely necessary.
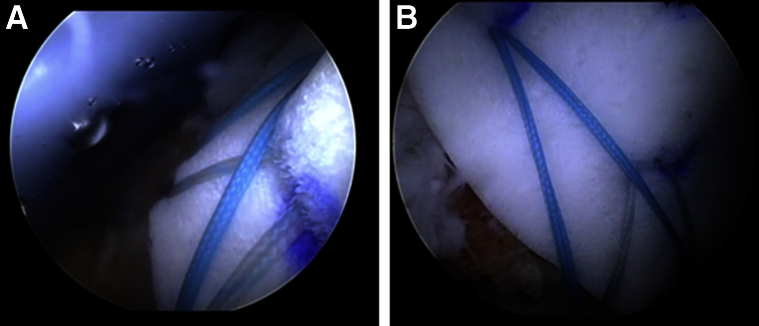
Fig 11.
Secured augment at end of procedure. The arthroscope is in the posterior port (A) or in the lateral port (B), looking at the bursa in a left shoulder.
Discussion
Despite advances in arthroscopic technology, consistently reproducible arthroscopic augmentation is technically challenging. The challenges involved include introduction and securing of augment, prevention of augment from bunching up, and prevention of sutures from becoming tangled.4, 5 Our technique addresses these challenges. The described technique involves relatively few suture limbs; therefore, augment introduction is straightforward with a reduced risk of suture ends becoming tangled. Excising the corners of the augment in addition to cutting out an inverted triangle along the medial edge of the augment (owl-shaped augment) reduces the risk of the augment bunching up and folding when the surgeon is securing the augment. In addition, if for any reason, the surgeon cannot insert and secure the augment in the desired situation, then it is very easy to remove the augment and carry on with the double-row repair by inserting the lateral-row anchors (transosseous-equivalent technique) because the medial-row repair has already been performed before the insertion of the augment.
Risks associated with extracellular matrix augmentation include inflammatory response, stiffness, and infection. With modern extracellular augment, advances in processing techniques have significantly enhanced removal of antigenic material. In our series we did not encounter an excessive inflammatory response or infection in any patient. Nonetheless, we recommend that the augment should not be performed in the presence of any active infection or previous shoulder joint infection. Similarly, the technique should not be used to bridge the gap in the presence of an irreparable tear. It should only be used to augment a tear that is repairable.
Footnotes
The authors report the following potential conflict of interest or source of funding: O.L. receives support from Collplant, Minivasive, Ceramtec, IDO, Estar Medical, and Mitek (educational grant).
Supplementary Data
Arthroscopic owl technique. The arthroscope is in the posterior port, looking at the bursa in a left shoulder. The patient is in the lateral position but the arthroscope is orientated so that the superior part of the image presents the superior part of the patient. Instrumentation is performed through the lateral port. An arthroscopic double-row rotator cuff repair is performed and followed by the positioning of an augment with extracellular matrix graft to reinforce the repair.
References
- 1.Thangarajah T., Pendegrass C.J., Shahbazi S., Lambert S., Alexander S., Blunn G.W. Augmentation of rotator cuff repair with soft tissue scaffolds. Orthop J Sports Med. 2015;3 doi: 10.1177/2325967115587495. 2325967115587495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schaer M., Schober M., Berger S., Boileau P., Zumstein M.A. Biologically based strategies to augment rotator cuff tears. Int J Shoulder Surg. 2012;6:51–60. doi: 10.4103/0973-6042.96995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gilot G.J., Attia A.K., Alvarez A.M. Arthroscopic repair of rotator cuff tears using extracellular matrix graft. Arthrosc Tech. 2014;3:e487–e489. doi: 10.1016/j.eats.2014.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Omae H., Yamamoto S., Mochizuki Y., Ochi M. An augmentation suture technique for arthroscopic rotator cuff repair. Arthrosc Tech. 2014;3:e313–e315. doi: 10.1016/j.eats.2014.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chalmers P.N., Frank R.M., Gupta A.K. All-arthroscopic patch augmentation of a massive rotator cuff tear: Surgical technique. Arthrosc Tech. 2013;2:e447–e451. doi: 10.1016/j.eats.2013.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic owl technique. The arthroscope is in the posterior port, looking at the bursa in a left shoulder. The patient is in the lateral position but the arthroscope is orientated so that the superior part of the image presents the superior part of the patient. Instrumentation is performed through the lateral port. An arthroscopic double-row rotator cuff repair is performed and followed by the positioning of an augment with extracellular matrix graft to reinforce the repair.