Abstract
Background
Between June 2012 and December 2013 Médecins Sans Frontières launched a pilot project with the aim of testing a strategy for improving timely diagnosis of active pulmonary TB among migrants hosted in four centres of identification and expulsion (CIE) in Italy.
Methods
This is a descriptive study. For active TB case finding we used an active symptom screening approach among migrants at admission in four CIE's. Here we describe the feasibility and the yield of this programme.
Results
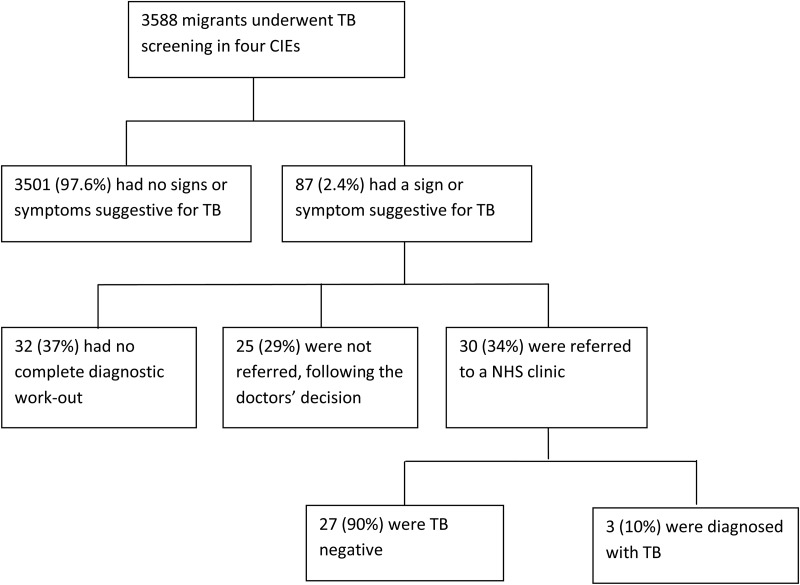
Overall, 3588 migrants were screened, among whom 87 (2.4%) had a positive questionnaire. Out of 30 migrants referred for further investigations, three were diagnosed as having TB, or 0.1% out of 3588 individuals that underwent screening. Twenty-five (29%, 25/87) migrants with positive questionnaires were not referred for further investigation, following the doctors' decision; however, for 32 (37%, 32/87) migrants the diagnostic work-out was not completed. In multivariate analyses, being over 35 years (OR 1.7; 95% CI 1.1–2.6) and being transgender (OR 4.9; 95% CI 2.1–11.7), was associated with a positive questionnaire.
Conclusions
TB screening with symptom screening questionnaires of migrants at admission in closed centres is feasible. However, to improve the yield, follow-up of patients with symptoms or signs suggestive for TB needs to be improved.
Keywords: Immigration detention centres, Italy, Migrants, Questionnaire, Screening, Tuberculosis
Introduction
Migration is a global phenomenon whose magnitude has increased in recent decades as a consequence of the growing political and social instability, wealth disparity, poverty, wars, and natural disasters. Conditions in which the migration process takes place can increase migrants' vulnerability to ill health.1 Persons migrating to low-TB incidence countries may be vulnerable to acquiring or reactivating TB due to more elevated TB prevalence in the home country, and the poor living conditions during migration and upon arrival.2–6 In addition migrants may experience barriers to timely diagnosis and proper treatment.7,8
In many low TB incidence countries, migrants presently represent an important share of incident TB cases, and interventions addressing the needs of migrants and cross-borders issues are needed both in order to guarantee the individual human rights (independent of legal or residential status of the patient) and to progress toward the goal of TB elimination.9,10
In the past decade in Italy TB notification rates have been constantly below 10/100 000 population, a commonly accepted threshold for defining low-incidence countries.10 Since 2009 more than 50% of cases notified each year occurred in foreign born persons.11 However, a standardised approach to address the issue of TB among migrants has not yet been implemented at national level.
In Italy there are five different types of open centres hosting migrants including those for asylum seekers, refugees and migrants that request international protection (Box 1). In such open centres there is no restriction of personal freedom. In addition there are closed centres, named centres of identification and expulsion (CIEs), which host migrants that will be expelled from the Italian territory for different reasons (including those who are not entitled to be under any form of international protection, those who have committed a felony).
Box 1. Types of accommodation centres for undocumented migrants in the Italian reception system29 .
First aid and reception centres (centri di primo soccorso ed assistenza [CPSA]) are temporary structures set up next to sea landing areas, here migrants are supposed to be hosted for the necessary time to be identified and transferred to other centres (max 72 hours).
Reception centres (centri di Accoglienza [CDA]). These facilities are used for the reception of migrants for the time necessary to take the appropriate administrative measures according to their legal status on Italian territory.
Reception centres for asylum seekers (centri di accoglienza per richiedenti asilo [CARA]) are facilities where the asylum applicants are hosted while awaiting identification and access to the procedure of refugee status recognition by the Local Commission (Legislative Decree no. 25 of 28 January 2008).
Extraordinary reception centres (centri di accoglienza straordinaria [CAS]) were created in 2014 due to an overflow of the CARA, especially after the Operation Mare Nostrum. They are facilities which accommodate asylum seekers for the time necessary to define the administrative bureaucracy for their permanence in Italy). They are generally small centres (up to 100 migrants).
Protection system for asylum seekers and refugees (sistema di protezione per richiedenti asilo e rifugiati [SPRAR]) are a network of small accommodations where the migrants with a refugee status or awaiting international protection are hosted. These facilities are conceived to integrate the immigrants in the local social network (institutionalised by law in 2002).
Identification and expulsion centres (centri di identificazione ed espulsione [CIE]) are facilities where the undocumented migrants are detained for the time necessary to carry out the procedures for the execution of the expulsion order. The maximum duration of the administrative detention in a CIE was 18 months. Currently the legislation has been changed and the maximum time of detention is 90 days.
We reasoned that CIEs could be an important target for TB control interventions. In fact, in CIEs overcrowding is frequent and detention can be extended up to 18 months.12 These conditions may facilitate TB transmission.6
Between June 2012 and December 2013 Médecins Sans Frontières (MSF) launched a pilot project with the aim of testing a strategy for improving timely diagnosis of active TB amongst migrants hosted in CIEs. The project was conducted in four CIEs in Italy and used an active symptom screening approach for active TB case finding, which was already evaluated at primary care centres for migrants in Italy.13 Here we describe the feasibility and the yield of this programme.
Methods
The project was conducted in CIEs located in Rome (central Italy), Milan (Northern Italy), and in Trapani and Caltanissetta (Sicily). Geographical and demographical reasons guided the choice of these centres among those operating at the time of the project: Rome CIE hosted both men and women, Milan CIE hosted men and transgenders and Trapani and Caltanissetta CIEs were in the region where the majority of the landings used to take place.
In CIEs primary health care is solely under the responsibility of the Ministry of Interior (MoI), and it is provided by doctors (mainly general practitioners) and nurses hired by the private agency in charge of the management of the centre. Patients have to be referred to the National Health Service (NHS) if diagnostic procedures or specialized care is needed. The medical and non-medical staff of the CIE received basic training on TB provided by an infectious diseases and TB specialists and MSF health promoter.
Every migrant that entered into a participating CIE from June 2012 to December 2013 was eligible for active TB screening at arrival. The tool used was a questionnaire composed of two parts: the first part contained socio-demographical data and was administered by a social worker or psychologist; the second part contained clinical data and was administered by the medical team of the CIE. Socio-demographic variables collected included: gender, age, country of origin, and date of first arrival in Italy. Clinical variables included: history of TB, history of previous TB contact, cough for more than 3 weeks, fever for at least 7 days, night sweats in the last 3 months, weight loss >10% in the last 3 months, one episode of haemoptysis in the last 3 months, and chest pain.13 Persons with a positive TB questionnaire (i.e., those having at least one positive answer to the eight clinical questions) were referred to the nearest NHS outpatient clinic for further evaluation. Outcomes of migrants with a positive questionnaire were classified as: active TB, active TB ruled out, not referred to NHS outpatient TB clinic by medical decision, or lost to follow-up (not evaluated at the TB clinic due to individual refusal, discharge/removal from the immigration centres or missing data regarding referral status). Screened migrants originating from one of the 22 high TB burden countries were categorised accordingly.14 The others were categorised as originating from a non-high TB burden country.
Predictors of a positive questionnaire were assessed with univariate and multivariate logistic regression. The constructed multivariate model was simplified by stepwise backwards elimination until the final model included variables with a p-value <0.05. Analyses were conducted with STATA® version 13 (Stata Corp LP, College Station, TX, USA).
The study met the MSF Ethics Review Board (Geneva, Switzerland) approved criteria for studies of routinely collected data and was also approved by the London School of Hygiene & Tropical Medicine MSc Research Ethics Committee. All activities and data collection tools were approved by the Italian national authorities. Oral informed consent was obtained from project participants. No personal identifiers were collected.
Results
In CIEs located in Milan, Rome and Trapani, 99.4% (958/964), 87.3% (1469/1682) and 67.1% (713/1062), respectively, of migrants admitted during the study period were screened for TB. In the Caltanissetta CIE, 448 people were screened; however the total immigrant population that was received by this centre during the study period is unknown.
The majority of the 3588 screened migrants were young adults. Their median age was 30 years (IQR 25–37; range 15–83). The vast majority (2934; 81.8%) were men. The CIE in Milan was the only one which hosted transgender migrants (12.4%; 119/964). The screened migrants came from 93 different countries of origin. They were grouped into five geographical areas: North Africa (43.2%; 1550/3588), Europe (20.1%; 721/3588), Sub Saharan Africa (15.2%; 547/3588), the Americas (9.1%; 327/3588), the Middle East and Asia (7.4%; 264/3588) (Table 1). Almost all transgender migrants originated from Latin American countries (94.9%; 111/117). The most frequently represented countries were Tunisia (19.0%; 681/3588) and Morocco (14.6%; 525/3588), followed by Nigeria (10.2%; 368/3588), Romania (8.1%; 289/3588) and Albania (6.0%; 214/3588). One in five (19.9%; 714/3588) screened migrants originated from high TB burden countries. Median time spent in Italy before detention in a CIE was 5 years (IQR 0.4–11.6).
Table 1.
Characteristics of 3588 migrants screened for TB in four immigration centres in Italy
| Variable | Screened migrants n=3588 n (%) |
|---|---|
| Gender | |
| Female | 427 (11.9) |
| Male | 2934 (81.8) |
| Transgender | 117 (3.3) |
| Missing data | 110 (3.1) |
| Age (years) | |
| <35 | 2293 (63.9) |
| ≥36 | 1140 (31.8) |
| Missing data | 155 (4.3) |
| Geographical regions | |
| North Africa | 1550 (43.2) |
| Europe | 721(20.1) |
| Sub Saharan Africa | 547 (15.3) |
| Americas | 327 (9.1) |
| Middle East and Asia | 264 (7.4) |
| Missing data | 179 (5.0) |
| TB burden in country of origin | |
| High burden | 714 (19.9) |
| Non high burden | 2695 (75.1) |
| Missing data | 179 (5.0) |
| Centres | |
| Trapani | 713 (19.9) |
| Caltanissetta | 448 (12.5) |
| Milan | 958 (26.7) |
| Rome | 1469 (40.9) |
Among 3588 migrants screened, 87 (2.4%) individuals had a positive TB questionnaire (Table 2). In univariate analyses, positivity of the questionnaire was associated with age over 35 years (OR 1.7; 95% CI 1.1–2.6), being transgender (OR 4.8; 95% CI 2.0–11.3); and origin from the Americas (OR 3.4; 95% CI 1.8–6.3). In multivariate analyses being older than 35 years (OR 1.7; 95% CI 1.1–2.6) and transgender (OR 4.9; 95% CI 2.1–11.7) was associated with a positive questionnaire (Table 3).
Table 2.
Frequency of reported clinical signs among 3588 migrants assessed with a TB questionnaire in four immigration centres in Italy
| Clinical signs | n (%) |
|---|---|
| History of TB | 42 (1.2) |
| History of previous TB contact | 27 (0.8) |
| Cough for more than 3 weeks | 30 (0.8) |
| Fever for at least 7 days | 11 (0.3) |
| Night sweats in the last 3 months | 13 (0.4) |
| Weight loss >10% in the last 3 months | 14 (0.4) |
| One episode of haemoptysis in the last 3 months | 11 (0.3) |
| Chest pain | 5 (0.1) |
| Total number of migrants with at least one positive clinical sign | 87 (2.4) |
Table 3.
Factors associated with a positive TB questionnaire among 3588 migrants in four immigration centres in Italy
| Variable | Negative clinical questionnaires n=3501 n (%) |
Positive clinical questionnaires n=87 n (%) |
Crude OR (95% CI) | p-value | Adjusted OR (95% CI)a | p-valuea |
|---|---|---|---|---|---|---|
| Age (years) | ||||||
| 15–35 | 2248 (64.2) | 45 (52) | 1 | 1 | ||
| ≥36 | 1103 (31.5) | 37 (43) | 1.7 (1.1–2.6) | 0.02 | 1.7 (1.1–2.6) | 0.02 |
| Missing data | 150 (4.3) | 5 (6) | ||||
| Gender | ||||||
| Female | 417 (11.9) | 10 (11) | 1 | 1 | ||
| Male | 2874 (82.1) | 60 (69) | 0.9 (0.4–1.7) | NS | 0.9 (0.5–1.8) | NS |
| Transgender | 105 (3.0) | 12 (14) | 4.8 (2.0–11.3) | <0.001 | 4.9 (2.1–11.7) | <0.001 |
| Missing data | 105 (3.0) | 5 (6) | ||||
| Geographical regions | ||||||
| North Africa | 1524 (43.5) | 26 (30) | 1 | |||
| Sub Saharan Africa | 532 (15.2) | 15 (17) | 1.7 (0.9–3.1) | NS | NA | NA |
| Americas | 309 (8.8) | 18 (21) | 3.4 (1.8–6.3) | <0.001 | NA | NA |
| Middle East & Asia | 257 (7.3) | 7 (8) | 1.6 (0.7–3.7) | NS | NA | NA |
| Europe | 706 (20.2) | 15 (17) | 1.2 (0.7–2.4) | NS | NA | NA |
| Missing data | 173 (4.9) | 6 (7) | NA | NA | NA | NA |
| TB burden in country of origin | ||||||
| High burden | 696 (19.9) | 18 (21) | 1.1 (0.6–1.8) | NS | NA | NA |
| Non-high burden | 2632 (75.2) | 63 (72) | 1 | |||
| Missing data | 173 (4.9) | 6 (7) | ||||
| Centres | ||||||
| Trapani | 695 (19.9) | 18 (20) | 1 | |||
| Caltanissetta | 448 (12.8) | 0 | NA | NA | NA | NA |
| Milan | 923 (26.4) | 35 (40) | 1.5 (0.8–2.6) | NS | NA | NA |
| Rome | 1435 (41.0) | 34 (39) | 0.9 (0.5–1.6) | NS | NA | NA |
NA: not applicable; NS: not significant.
a The constructed multivariate model was simplified by stepwise backwards elimination until the final model included variables with a p-value <0.05.
The 87 migrants with a positive TB questionnaire were consulted by a medical doctor in the CIE, to decide on indication for referral to the NHS. Thirty (34%) patients were referred by the doctor to the NHS for further investigations, which consisted of a chest X-ray and a specialist referral consultation. Three male adult migrants were diagnosed with pulmonary TB; they represented 0.1% of the 3588 screened for TB, 2.6% of those with positive questionnaire and 10% of the 30 individuals evaluated for TB (Figure 1). During the screening at arrival in the CIE all three reported a history of TB. None had completed the previous TB treatment. All three were asymptomatic. Sputum smears were positive for one patient, negative for another, and not reported for the third. Mycobacterial culture was only performed in one case and was negative.
Figure 1.
Flow diagram of TB screening among 3588 migrants in four immigration centres in Italy. CIE: identification and expulsion centres (centri di identificazione ed espulsione); NHS: National Health Service.
Twenty-five (29%; 25/87) migrants with positive questionnaires were not referred by the CIE to the NHS, following the doctors' decision, and thus not further investigated for TB. Eleven out of 25 had been recently investigated for TB during their permanence in either prison or another CIE. Fourteen out of 25 were diagnosed with an alternative condition by the doctors of the CIE. Alternative diagnoses included chronic cough secondary to smoking or asthma, chronic pharyngitis, and reduced food intake as an explanation for weight loss.
Finally, for 32 (37% of 87) migrants the diagnostic work-out was not completed: 15 had been either expelled to their countries of origin or were released from the CIE into the Italian territory; one could not be referred for logistic reasons, one refused to be referred and for 15 no information was available, and were considered lost to follow-up.
Discussion
This study assessed the feasibility and outcomes of an active TB case-finding programme based on symptom screening implemented by MSF in four detention centres for migrants in Italy, in collaboration with the medical and socio-cultural teams of these centres. In three out of four centres the screening could be conducted in the vast majority of the admitted migrants. Overall, 3588 migrants were screened, among whom 87 (2.4%) had a positive questionnaire. However, no further investigations took place for 57 (65.5%) migrants with a positive questionnaire. Out of 30 migrants referred for further investigations, three were diagnosed as having TB, or 0.1% out of 3588 individuals that underwent screening.
Our study population was very heterogeneous, ranging from newly arrived migrants to people that had been living in Italy for decades. People older than 35 years were 1.7-fold more likely to have a positive questionnaire than younger people which is not surprising given that they are more likely to have health complaints unrelated to TB, and they are also more likely to have had contact with TB in the past.15 Transgender individuals were 4.9-fold more likely to have a positive questionnaire. Other studies showed they tend to be more exposed through high risk-occupations such as prostitution.16,17 Subsequently HIV prevalence is often much higher in this subgroup.16–18 Although HIV infection increases the risk to acquire or reactivate TB, only few studies report on the epidemiology of TB amongst transgenders.19
The coverage of screening could be evaluated in three of the four participating centres. In these three centres 84% of admitted migrants could be screened, with some differences among centres. This coverage compares well with the 63.9% coverage reported by another TB symptom screening programme conducted in Italian primary care centres for migrants.13 A systematic review of TB screening programs for persons migrating to European countries found a high variability in screening coverage ranging from below 20 to almost 100%, with higher figures on asylum seekers and in compulsory screening programmes.20
In our programme the number of people to be screened in order to find one case of TB was 1196. The yield of TB screening was 84 per 100 000 people. This is lower than the yield reported in a systematic review, showing 125 to 1036 TB diagnoses per 100 000 asylum seekers and refugees groups screened.21
A first possible reason for our low yield could be the large proportion of individuals (66%; 57/87) that reported symptoms but did not receive a complete diagnostic evaluation for TB. Almost half of them (44%; 25/57) were given alternative diagnoses and not referred for further investigation as per doctors' decision. Among them, eight individuals were coughing for more than 3 weeks. The appropriateness of these medical decisions could not be ascertained. In addition, logistic, administrative and management factors partially explain the poor follow-up of people with positive TB questionnaires. To benefit from a referral consultation a police escort had to be organised. Furthermore, migrants were often transferred from centre to centre without notice and without a proper medical information flow, which obviously makes it difficult to monitor provided care. Earlier reports confirm the challenges of keeping track of undocumented migrants, given the mobile nature of their lives.22,23
In addition, we hypothesize that the lack of sensitivity and specificity of the employed diagnostic tests explains partially the low diagnostic yield. Although a chest X-ray has a sensitivity of 90% (95% CI 81–96) and specificity of 89% (95% CI 87–92%) when performed after positive screening for symptoms,24 sensitivity and specificity of chest X-rays depend largely on the ability of the doctor who interprets them. In our study chest X-rays were interpreted mainly by radiologists working in emergency departments at the nearest NHS facilities to each CIE, who had no specific expertise in TB diagnosis. The only regional NHS facility TB treatment centre, with longstanding experience in migrant screening was in Milan.25,26 On the other hand, most of the described TB screening programmes considered in the review of Aldridge et al., applied a symptom enquiry followed by a chest radiogram, with or without a Mantoux test.21
Finally, the cultural acceptability of TB screening should be studied. This is a survey of self-reported clinical signs, thus reporting bias might have occurred, due to language barriers, cultural and behavioural differences, or misconceptions of the migrants.27 Suggestions for future screening programs include clear criteria to orient the CIE's doctor's decision to refer or not patients with a positive TB screening questionnaire. Follow-up of migrants with symptoms or signs suggesting TB should be implemented inside CIEs. When means are limited, screening of transgenders and migrants above 35 years old could be prioritised. Finally, community-based interventions involving migrants and cultural mediators may enhance a more effective communication between provider and client, and result in improved performance of health care services.28
A strength of our study was the large sample and the use of program data. Thus our findings are likely representative of the reality of the TB screening program in reception centres. However, our study has also some important limitations. First, not all migrants had a TB questionnaire. Therefore we cannot estimate the prevalence of TB symptoms among migrants in reception centres. Second, TB diagnosis could not be confirmed or excluded among all migrants with a positive TB questionnaire. This may have led to an underestimation of the number of migrants with TB. Finally, as discussed above, a negative TB questionnaire does not equal the absence of TB. These limitations show the challenges of scaling up TB screening using a questionnaire in reception centres.
Conclusions
In conclusion, TB screening with symptom screening questionnaires of migrants at admission in closed centres is feasible. However, to improve the yield, additional measures are required to improve the follow-up of clients with symptoms or signs suggestive for TB.
Acknowledgments
Authors' contributions: AC wrote the first draft of the paper. All co-authors contributed to the subsequent draft and the revised paper as a result of reviewers' comments and suggestions. All authors have read and approved the final paper. ER is the guarantor of the paper.
Funding: Funding to pay the Open Access publication charges for this article was provided by Médecins Sans Frontières, Operational Centre Brussels.
Competing interests: None declared.
Ethical approval: The study met the MSF Ethics Review Board approved criteria for studies of routinely collected data and was also approved by the London School of Hygiene & Tropical Medicine MSc Research Ethics Committee.
References
- 1.Ministry of Health. L'accesso alle cure della persona straniera: indicazioni operative. Istituto Superiore di Sanita. Rome: Ministry of Health; 2013. http://www.salute.gov.it/imgs/c_17_opuscoliposter_199_allegato.pdf [accessed 7 October 2015]. [Google Scholar]
- 2.Franzetti F, Codecasa L, Matteelli A et al. Genotyping analyses of tuberculosis transmission among immigrant residents in Italy. Clin Microbiol Infect 2010;16:1149–54. [DOI] [PubMed] [Google Scholar]
- 3.Kamper-Jørgensen Z, Andersen AB, Kok-Jensen A et al. Migrant tuberculosis: the extent of transmission in a low burden country. BMC Infect Dis 2012;12:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Manissero D, van der Werf MJ, Girardi E. Tuberculosis transmission between foreign- and native-born populations in the EU/EEA: a systematic review. Eur Respir J 2014;43:1159–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sulis G, Roggi A, Matteelli A, Raviglione MC. Tuberculosis: epidemiology and control. Mediterr J Hematol Infect Dis 2014;6:e2014070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zammarchi L, Bartalesi F, Bartoloni A. Tuberculosis in tropical areas and immigrants. Mediterr J Hematol Infect Dis 2014;6:e2014043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heldal E, Kuyvenhoven JV, Wares F et al. Diagnosis and treatment of tuberculosis in undocumented migrants in low- or intermediate-incidence countries. Int J Tuberc Lung Dis 2008;12:878–88. [PubMed] [Google Scholar]
- 8.Wickramage K, Mosca D. Can migration health assessments become a mechanism for global public health good? Int J Environ Res Public Health 2014;11:9954–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dara M, de Colombani P, Petrova-Benedict R et al. Minimum package for cross-border TB control and care in the WHO European region: a Wolfheze consensus statement. Eur Respir J 2012;40:1081–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lönnroth K, Migliori GB, Abubakar I et al. Towards tuberculosis elimination: an action framework for low-incidence countries. Eur Respir J 2015;45:928–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.European Centre for Disease Prevention and Control, WHO Regional Office for Europe. Tuberculosis surveillance and monitoring in Europe 2014. Stockholm: European Centre for Disease Prevention and Control; 2014. http://www.ecdc.europa.eu/en/publications/Publications/tuberculosis-surveillance-monitoring-Europe-2014.pdf [accessed 7 October 2015]. [Google Scholar]
- 12.Medici per I Diritti Umani. Italian Centres for Identification and Expulsion: National Data for 2013. Even more useless and distressing structures. Medici per I Diritti Umani 2013. http://www.mediciperidirittiumani.org/en/italian-centres-identification-expulsion/ [accessed 7 October 2015]. [Google Scholar]
- 13.Sañé Schepisi M, Gualano G, Fellus C et al. Tuberculosis case finding based on symptom screening among immigrants, refugees and asylum seekers in Rome. BMC Public Health 2013;13:872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.WHO. Global tuberculosis report 2015. Geneva: World Health Organization; 2015. http://www.who.int/tb/publications/global_report/en/ [accessed 7 October 2015]. [Google Scholar]
- 15.Schablon A, Nienhaus A, Ringshausen FC et al. Occupational screening for tuberculosis and the use of a borderline zone for interpretation of the IGRA in German healthcare workers. PLoS One 2014;9:e115322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dos Ramos Farías MS, Garcia MN, Reynaga E et al. First report on sexually transmitted infections among trans (male to female transvestites, transsexuals, or transgender) and male sex workers in Argentina: high HIV, HPV, HBV, and syphilis prevalence. Int J Infect Dis 2011;15:e635–40. [DOI] [PubMed] [Google Scholar]
- 17.Herbst JH, Jacobs ED, Finlayson TJ et al. HIV/AIDS Prevention Research Synthesis Team. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav 2008;12:1–17. [DOI] [PubMed] [Google Scholar]
- 18.Rovirola CH, Ortiz-Barreda G, Montemayor JCG et al. HIV and other sexually transmitted infections among migrant population in Spain: a scoping review. Rev Esp Salud Publica 2014;88:763–81. [DOI] [PubMed] [Google Scholar]
- 19.Centre of Disease Control 2000, HIV-ralated tuberculosis in a transgender network – Baltimore, Maryland and New York City area, 1998–2000. MMWR Morb Mortal Wkly Rep 2000;49:317–20. [PubMed] [Google Scholar]
- 20.Klinkenberg E, Manissero D, Semenza JC, Verver S. Migrant tuberculosis screening in the EU/EEA: yield, coverage and limitations. Eur Respir J 2009;34:1180–9. [DOI] [PubMed] [Google Scholar]
- 21.Aldridge RW, Yates TA, Zenner D et al. Pre-entry screening programmes for tuberculosis in migrants to low-incidence countries: a systematic review and meta-analysis. Lancet Infect Dis 2014;14:1240–9. [DOI] [PubMed] [Google Scholar]
- 22.Johnsen NL, Steen TW, Meyer H et al. Cohort analysis of asylum seekers in Oslo, Norway, 1987–1995: effectiveness of screening at entry and TB incidence in subsequent years. Int J Tuberc Lung Dis 2005;9:37–42. [PubMed] [Google Scholar]
- 23.Harling R, Pearce M, Chandrakumar M et al. Tuberculosis screening of asylum seekers: 1 years’ experience at the Dover Induction Centres. Public Health 2007;121:822–7. [DOI] [PubMed] [Google Scholar]
- 24.WHO. Systematic screening for active tuberculosis, principles and recommendations. Geneva: World Health Organization; 2013. http://www.who.int/tb/tbscreening/en/ [accessed 7 October 2015]. [PubMed] [Google Scholar]
- 25.Olivani P, Codecasa L, Colucci A et al. The tubercular disease in immigrants without documents: new diagnostic settings adopted in Milan, Italy. Ann Ig 2013;25:493–500. [DOI] [PubMed] [Google Scholar]
- 26.Codecasa AD, Porretta A, Gori F et al. Tuberculosis among immigrants from developing countries in the province of Milan - 1993–1996. Int J Tuberc Lung Dis 1999;3:589–95. [PubMed] [Google Scholar]
- 27.Tomás BA, Pell C, Cavanillas AB et al. Tuberculosis in migrant populations. A systematic review of the qualitative literature. PLoS One 2013;8:e82440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Seedat F, Hargreaves S, Friedland JS. Engaging new migrants in infectious disease screening: a qualitative semi-structured interview study of UK migrant community health-care leads. PLoS One 2014;9:e108261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.The Graduate Institute. Global Detention Project. Italy Detention Profile. Geneva: The Graduate Institute; Programme for the Study of Global Migration; 2012. http://www.refworld.org/pdfid/545b31704.pdf. [accessed 28 April 2016]. [Google Scholar]