Abstract
There are very few reports of spinal epidural lipomatosis (SEL) in association with scoliosis. A 49-year-old man presented with persistent back pain and right hip lump. The lumbar spine X-rays showed scoliosis (Lenke classification 5BN). Lumbar MRI demonstrated circumferential epidural fat deposit from L1 to lower S2 level. There was no obvious etiology of SEL except mild increased body mass index (BMI). The patient was managed with conservative treatment. After 6 months medication (limaprost and ginkgo), his symptoms were relieved.
Keywords: Epidural lipomatosis, scoliosis
Introduction
Spinal epidural lipomatosis (SEL) is a rare condition defined by un-encapsulated overgrowth of normal extra-dural fat, which can compress the spinal canal or cord (1-3). SEL has been regarded as a consequence of long-term administration of exogenous excess steroids, local corticosteroid injections and endocrinopathy associated with a variety of glucocorticoid-producing systemic diseases that included Cushing’s syndrome, obesity, carcinoid tumor, and hypothyroidism (1,2,4,5). Quite rarely, SEL occurs as an idiopathic condition that means in the absence of recognized predisposing factors (5).
SEL is often an incidental finding and the majority of patients remain asymptomatic (1). However, SEL has been related to a variety of neurologic impairments, which included back pain, radiculopathy, claudication, or myelopathy (4). There are very few reports of SEL in association with scoliosis (3). We present a case of scoliosis caused by idiopathic SEL.
Case presentation
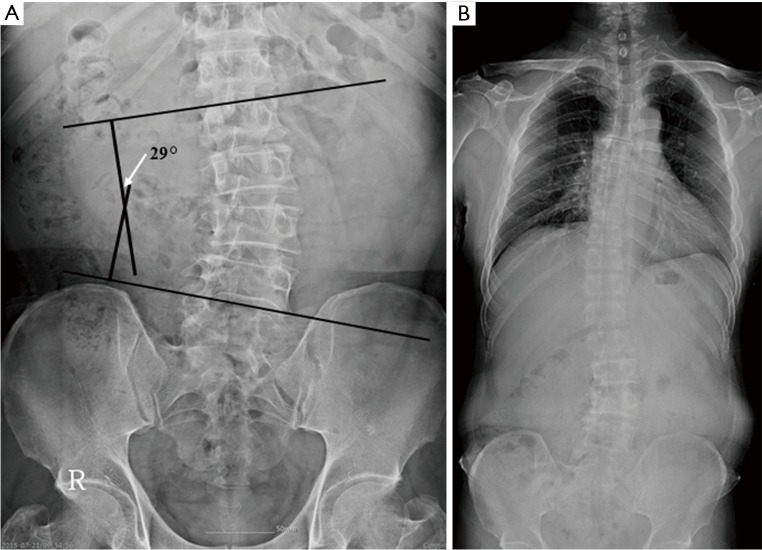
A 49-year-old man presented with persistent back pain and right hip lump. The physical examination revealed a lumbar scoliosis and asymmetric enlargement of right gluteus muscle. Neurological examination showed no motor and sensory deficits. The lumbar spine X-rays showed lumbar spine scoliosis without any significant vertebral abnormality. Cobb’s angle was measured at 29°. Scoliosis was classified as Lenke type 5BN (Figure 1). Right hip sonogram did not demonstrate any mass-like lesions.
Figure 1.
Lumbar spine (A) and whole spine (B) anterior-posterior X-rays show lumbar spine scoliosis (Lenke classification; 5BN) without any significant vertebral abnormality. Cobb’s angle was measured at 29°.
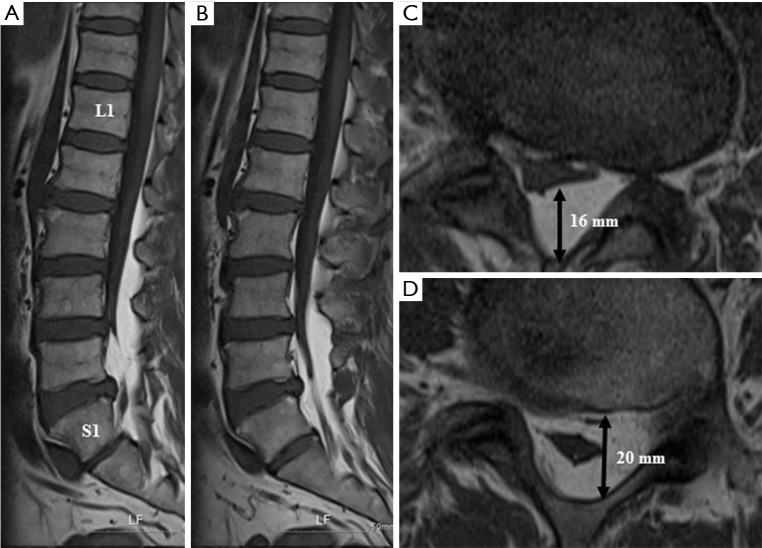
Lumbar magnetic resonance imaging (MRI) with enhancement demonstrated circumferential epidural fat deposit with co-existent spinal stenosis from L1 to lower S2 level and no evidence of enhancing lesion (Figure 2A,B). Epidural lipomatoses were worst at the L4/5 and L5/S1 levels (Figure 2C,D). We performed bilateral leg electromyography which showed no evidence of radiculopathy.
Figure 2.
Mid-sagittal (A) and para-sagittal (B) T1-weighted MR images reveal high-intensity adipose tissue mass in the spinal canal and circumferential epidural fat deposit from L1 lower level to S2. Axial T1-weighted MR images at L4/5 (C) and L5/S1 (D) level show the stellate sign. Each L4/5 and L5/S1 level adipose tissue measured 16 and 20 mm.
We searched for etiologies of SEL. The patient had no history of steroid use, epidural steroid injections, no medical co-morbidities and taking no regular medication. A body mass index (BMI) of the patient was 29.5 kg/m2 which meant a slightly obese condition. The patient didn’t have neurological deficits except back pain and scoliosis. Therefore, we decided that the patient was treated with regular medications (limaprost and ginkgo) and closely observed.
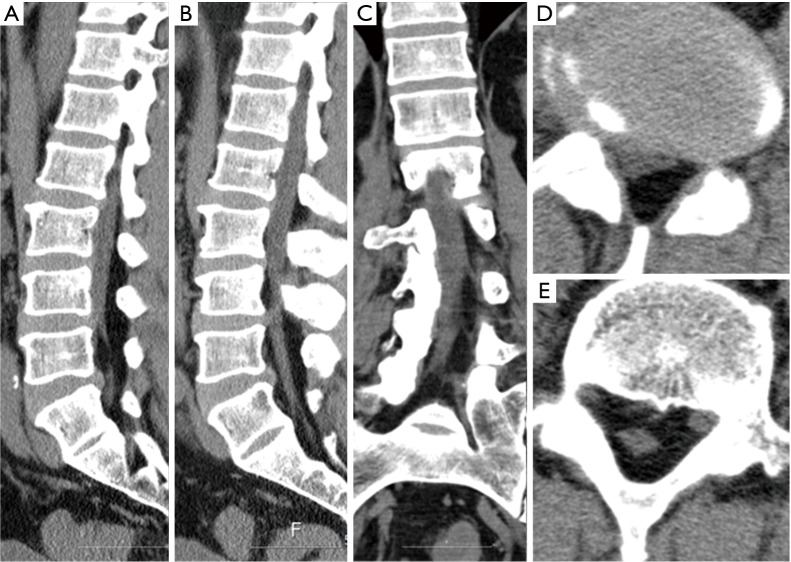
During the follow-up period, his symptoms were much improved. Six months after initiation of medications, follow-up lumbar computed tomography (CT) showed no interval change of prominent epidural fat deposit and scoliosis (Figure 3).
Figure 3.
Six months after treatment, follow-up lumbar CT images demonstrate no change of prominent epidural fat deposit and scoliosis. Mid sagittal (A), para-sagittal (B), Coronal (C), L4/5 Axial (D), L5/S1 axial (E).
Discussion
Mechanisms of SEL are still unclear (5). Increase of SEL incidence has been attributed to exogenous steroid use, endocrine disease, growing prevalence of obesity, and improvement in diagnostic techniques (4-6).
The typical MRI findings of SEL are the presence of a mass lesion on T1-weighted high-intensity and T2-weighted low-or immediate-intensity imaging (4,6). Advanced SEL can appear as a small oval or letter Y-shaped compression in the axial slice of the MRI that is commonly referred to as the stellate sign, or the “Y” sign (4,6). There must be greater than 7 or 8 mm thickness of adipose tissue to have a diagnosis of SEL (3,6). In this case, thickness of adipose tissue, L4/5 level is 16mm and L5/S1 level is 20 mm.
The treatment of SEL includes conservative management and surgery (6). Weight loss or steroid reduction is recommended if SEL is associated with obesity or exogenous steroid use (6). In cases where neurological deficits are present, symptoms are rapidly progressive, or conservative therapies fail, surgical decompression has been shown to prevent further exacerbation and produce improvements in symptoms (4-6).
Limaprost (Prostaglandin E1 derivatives) improves symptoms in patients with lumbar spinal stenosis by improving the blood flow via its vasodilatory and anti-platelet aggregation effects (7). Ginkgo also inhibits platelet-activating factors and several studies showed that ginkgo increases the microcirculatory perfusion of blood vessels (8).
Spinal stenosis due to SEL was the main issue in this patient. Improving blood flow and increasing microcirculation in lumbar neural tissue are helpful in relieving the patient’s symptoms. Therefore, we decided that the patient be treated with a combination therapy (limaprost and ginkgo).
SEL with scoliosis is a very rare entity (3). A literature search revealed only two cases of SEL associated with scoliosis (3,9). They are summarized in Table 1. In this case, idiopathic SEL was incidentally found in the patient with back pain and lumbar scoliosis. We didn’t find any risk factors of SEL except mildly increased BMI.
Table 1. Summary of reported cases of scoliosis associated with spinal epidural lipomatosis.
| Author (Ref. No.) | Age/sex | Cause of SEL | Body mass index (kg/m2) | Scoliosis of Lenke classification | Range of SEL | Management of SEL |
|---|---|---|---|---|---|---|
| Sabharwal et al. (3) | 14/F | Idiopathic | – | 5CN | Entire thoracic spine | Posterior instrumentation(from T3 to L2) |
| Kurt et al. (9) | 52/M | Idiopathic | 29 | – | From L3 to S2 | Decompressive laminectomy (from L2 to S1) |
| This case | 49/M | Idiopathic | 29.5 | 5BN | From L1 to S2 | Conservative treatment |
Ref, reference; No, number; M, male; F, female; SEL, spinal epidural lipomatosis.
Conclusions
We report the case of a patient with scoliosis caused by idiopathic SEL. The patient was successfully managed with conservative treatment.
Acknowledgements
None.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Footnotes
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- 1.Dawes B, Lo J, Byrne ST, et al. Symptomatic concurrent spinal epidural lipomatosis and spinal pathology. ANZ J Surg 2015. [Epub ahead of print]. 10.1111/ans.13000 [DOI] [PubMed] [Google Scholar]
- 2.Yoo JC, Choi JJ, Lee DW, et al. Spinal epidural lipomatosis in korean. J Korean Neurosurg Soc 2014;55:365-9. 10.3340/jkns.2014.55.6.365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sabharwal S, Mahmood F. Thoracic spinal epidural lipomatosis associated with adolescent scoliosis. J Spinal Disord Tech 2006;19:217-21. 10.1097/01.bsd.0000179672.80229.0d [DOI] [PubMed] [Google Scholar]
- 4.Patel AJ, Sellin J, Ehni BL, et al. Spontaneous resolution of spinal epidural lipomatosis. J Clin Neurosci 2013;20:1595-7. 10.1016/j.jocn.2012.09.049 [DOI] [PubMed] [Google Scholar]
- 5.Mariotto S, Bianchi MR, Ferrari S, et al. Cauda equina syndrome caused by lumbosacral epidural lipomatosis. A case report. Clin Neurol Neurosurg 2013;115:1549-51. 10.1016/j.clineuro.2012.12.034 [DOI] [PubMed] [Google Scholar]
- 6.Sugaya H, Tanaka T, Ogawa T, et al. Spinal epidural lipomatosis in lumbar magnetic resonance imaging scans. Orthopedics 2014;37:e362-6. 10.3928/01477447-20140401-57 [DOI] [PubMed] [Google Scholar]
- 7.Yoshihara H. Prostaglandin E1 Treatment for Lumbar Spinal Canal Stenosis: Review of the Literature. Pain Pract 2016;16:245-56. 10.1111/papr.12272 [DOI] [PubMed] [Google Scholar]
- 8.Suter A, Niemer W, Klopp R. A new ginkgo fresh plant extract increases microcirculation and radical scavenging activity in elderly patients. Adv Ther 2011;28:1078-88. 10.1007/s12325-011-0083-4 [DOI] [PubMed] [Google Scholar]
- 9.Kurt E, Bakker-Niezen SH. Neurogenic claudication by epidural lipomatosis: a case report and review of literature. Clin Neurol Neurosurg 1995;97:354-7. 10.1016/0303-8467(95)00071-Q [DOI] [PubMed] [Google Scholar]