Abstract
Coronal limb malalignment is a significant contributor to asymmetric joint wear, gait abnormalities, and the development and progression of degenerative joint disease. Osteotomies about the knee were developed to realign the mechanical axis of the limb to unload the affected compartment. Valgus malalignment is less common than varus malalignment, but can contribute to a variety of clinical conditions, including lateral compartment cartilage defects and arthritis, lateral patellofemoral instability, and medial collateral ligament laxity. In this article, we describe our preferred operative technique for a lateral opening wedge varus-producing distal femoral osteotomy to correct mild to moderate valgus malalignment.
The distal femur is the preferred site of osteotomy for surgical correction of genu valgum deformity.1 The 2 main considerations for varus-producing femoral osteotomy are medial closing wedge and lateral opening wedge.2 Here we will focus on lateral opening wedge osteotomy (Video 1), its stated advantages and disadvantages, surgical indications, preoperative planning, surgical technique, and clinical outcomes (Table 1).
Table 1.
Indications and Contraindications
|
|
|
Surgical Technique
Preoperative Planning and Radiograph Templating
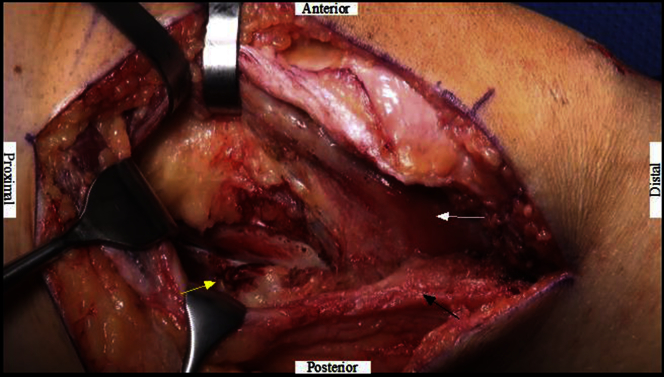
Examining both the mechanical and anatomic axes is an important consideration before surgery. The normal mechanical axis of the lower limb is defined as a line passing from the center of the femoral head, through the center of the knee, and continuing down to the center of the ankle. This differs from the anatomic axis of the lower limb, which follows a line from the center of the femoral head, down the femoral shaft through the center of the tibia at the knee joint, to the center of the ankle, as depicted in Figure 1. Abnormal lateral distal femoral angles are considered anything less than 84 degrees. Standard radiographic assessment includes a bilateral standing full-length alignment view, bilateral weight-bearing anteroposterior views in full extension, bilateral weight-bearing posteroanterior tunnel views at 30 degrees of flexion (Rosenberg view), lateral, and sunrise or Merchant views. Although not routine, if articular or meniscal pathology is suspected following preoperative evaluation, magnetic resonance imaging may be considered.
Fig 1.
Depiction of both the normal mechanical and anatomic axis of the lower limb in a bilateral standing full-length anteroposterior radiograph. The mechanical axis follows a line from the femoral head through the center of the talus. The anatomic axis follows a line through the center of the femoral shaft through the center of the tibia to the center of the ankle.
Goals
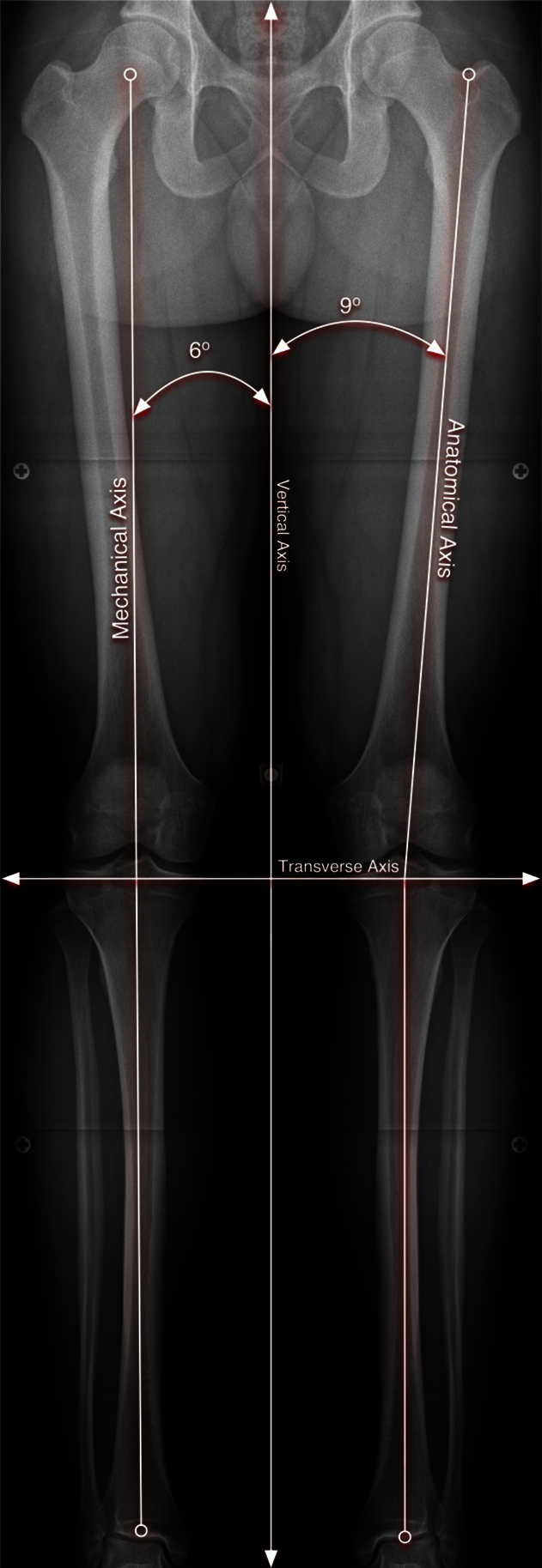
The goal of surgery is to re-create neutral alignment, such that the mechanical axis line passes through the center of the knee.3 The amount of correction is calculated based on the angle formed between the mechanical axis of the femur and tibia (Fig 2). Practically, 5 degrees of malalignment is the threshold to consider osteotomy. The calculated angle of correction in degrees determines the amount of wedge opening. The geometric triangle method is commonly used, measuring the distance on a size-calibrated radiograph.4 This is used as the initial intraoperative measurement and confirmed intraoperatively with radiographic and visual inspection of long leg alignment.
Fig 2.
Calculation of the correction using the angle formed between the mechanical axis of the femur and tibia, respectively. This figure depicts a cropped view at the knee as a means to demonstrate how the deformity correction is determined. Lines drawn are as follows: Line A represents the desired mechanical axis of the limb from the center of the femoral head, passing through the center of the knee, which is the goal of correction in this case. Line B represents mechanical axis of the tibia passing from the center of the knee to the center of the tibiotalar joint at the ankle. In this case, the angle of correction measures 6 degrees. Line C represents the orientation at which the lateral opening wedge osteotomy will be made. Six degrees will be used to calculate the distance of opening required to achieve this correction.
Distal Femoral Lateral Opening-Wedge Osteotomy
The authors' preferred technique for a distal femoral opening-wedge osteotomy is described below with an accompanying video demonstration (Video 1).
Patient Positioning
The patient is placed in the supine position with the sterile field exposing the entire limb including the iliac crest so that the axis of the limb can be assessed intraoperatively. Patient position must facilitate adequate intraoperative imaging studies; thus, the operative limb may be raised on a bump or the contralateral limb may be lowered. This position is also ideal for the surgical exposure to the medial femur. Fluoroscopy is assessed prior to draping to ensure that the hip, knee, and ankle can all be adequately imaged intraoperatively to assess overall alignment correction. The operative limb is also raised on a foam bump to allow for adequate lateral intraoperative imaging with less manipulation of the unstable osteotomy prior to fixation.
Surgical Technique
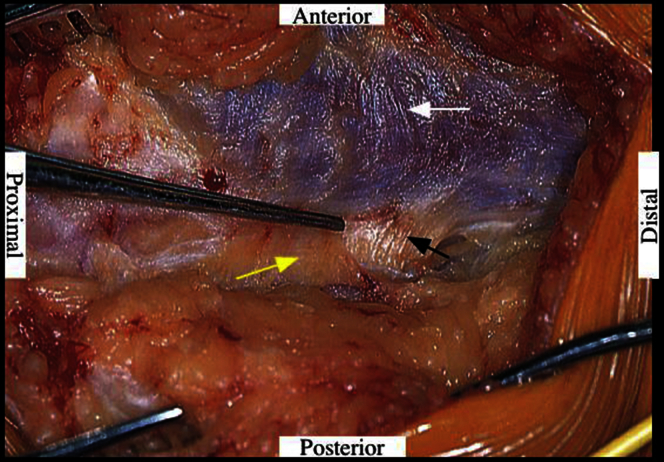
Two surgical approach options can be considered for a lateral, distal femoral osteotomy. The first is a true extra-articular approach in which a 12- to 15-cm lateral incision is made over the midline lateral femur and angulated anterior 2 cm distal to lateral epicondyle. The iliotibial band is split and the intermuscular septum is identified (Fig 3). The vastus lateralis is elevated from intermuscular septum, being careful to coagulate arterial branches of the profunda femoris.
Fig 3.
The intermuscular septum (white arrow) between vastus lateralis (black arrow) and biceps femoris, posterior aspect of vastus medialis (yellow arrow) is identified and elevated. Meticulous dissection in the correct plane is critical here as this will determine the exposure for the duration of the procedure.
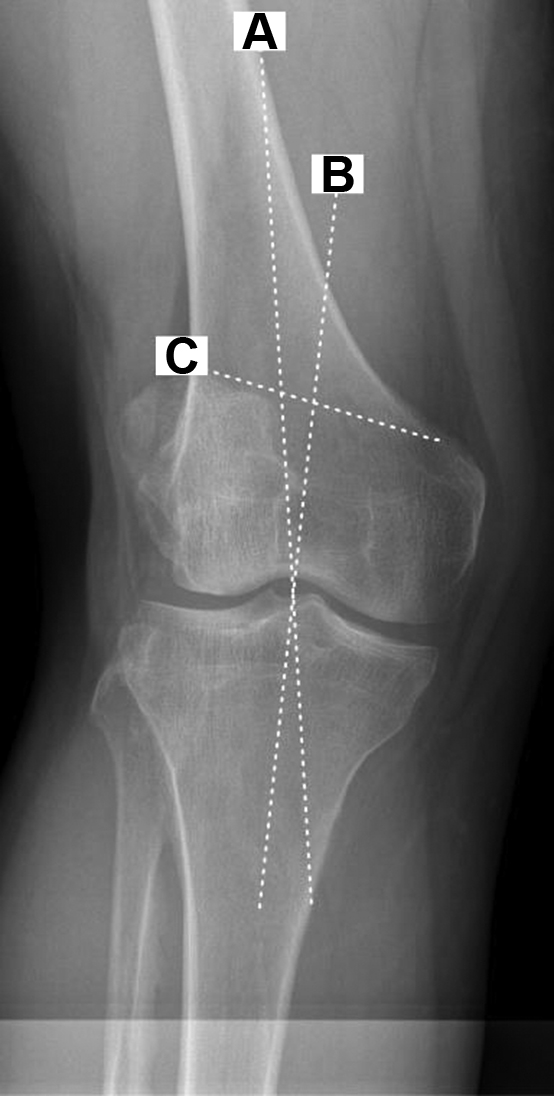
If a concomitant intra-articular procedure, such as a lateral femoral condyle cartilage procedure is to be performed, then an extended lateral peripatellar approach is recommended. Typically, we prefer to finish concomitant procedures prior to the osteotomy; arthroscopy may be used for diagnostic purposes as needed before proceeding (Fig 4). In cases of concomitant procedures, for example, lateral femoral condyle osteochondral allograft transplantation is completed first to avoid hyperflexing the knee that could cause intraoperative loss of fixation. The arthrotomy should be made as far proximal as possible to facilitate proximal hardware placement and lessen tension on the medially subluxed patella during access to the intra-articular lateral femoral condyle. The intermuscular septum is released and a radiolucent retractor in order placed to protect the tibial nerve and popliteal artery (Fig 5).
Fig 4.
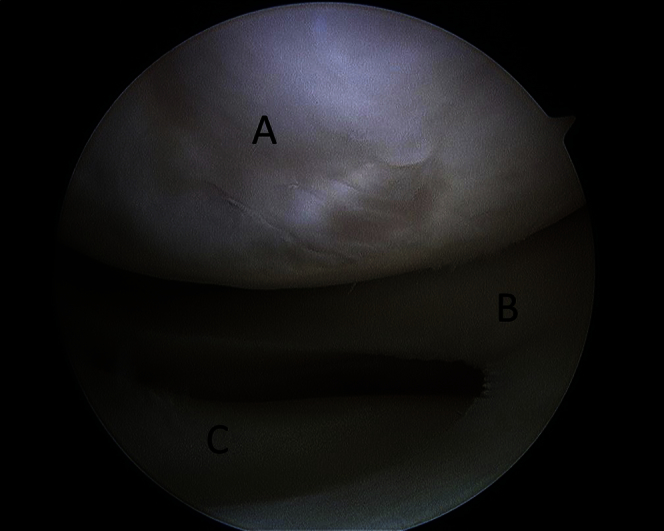
Depicted is an arthroscopic view of the lateral compartment of the knee from the anterolateral portal. Diagnostic arthroscopy can be used to assess for associated meniscoligamentous or cartilage injuries for concomitant procedures with the osteotomy. The denoted structures represent the lateral femoral condyle (A), the lateral meniscus (B), and the lateral tibial plateau (C).
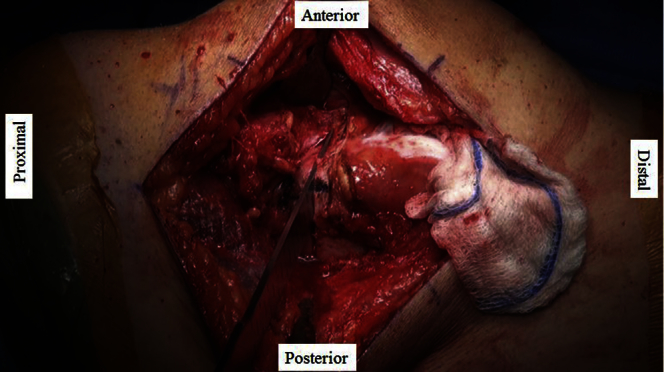
Fig 5.
The vastus lateralis (white arrow) is carefully lifted up from intermuscular septum (black arrow) and the distal medial aspect of the femoral shaft is identified. Care is taken to coagulate arterial branches of profunda femoris (yellow arrow). This is an essential step in the exposure as significant bleeding can be encountered if not appropriately coagulated, which can cause significant complications to the limb, as well as affect visualization during the procedure.
A metadiaphyseal guide pin (Stryker, Kalamazoo, MI) is placed approximately 2 to 3 fingerbreadths proximal to the lateral epicondyle and aimed just proximal to the medial epicondyle to establish the trajectory of the osteotomy (Fig 6). A mark on the cortex above and below the anticipated osteotomy helps assess any potential rotation of the femur (Fig 7). To minimize the risk of iatrogenic neurovascular injury, the knee is then flexed to decrease tension on the neurovascular bundle and increase their distance from the posterior cortex. An oscillating saw blade is used to start the osteotomy, while maintaining the trajectory of the guide pin. Thin osteotomes (Stryker) are used to complete the cut within 1 cm of the medial cortex (this distance is measured on a calibrated preoperative x-ray and the desired measurement marked on the osteotome). The jack opener (Stryker) is placed and opened, and the osteotomy is hinged carefully at the medial cortex slowly over time, to take advantage of the viscoelastic properties of bone. If performing a larger correction, it is helpful to perforate the medial cortex with a drill bit to allow a controlled opening. A locking plate is preferred in the setting of an unstable medial cortex. Corticocancellous wedges are harvested from the femoral neck portion of an allograft femoral head (Mayo Clinic Surgical Bone Bank) and placed into the osteotomy site according to the preoperative plan. These wedges stabilize the osteotomy while the final mechanical axis views are verified with fluoroscopy (Fig 8). The distal, lateral femoral locking plate (Synthes Tomofix, West Chester, PA) is then positioned on the lateral femoral cortex. Screw sequence involves placing the distal locking screws first, then a kickstand nonlocking screw in compression mode, followed by the proximal unicortical locking screws. It is important to maintain the cortical wedge allograft at the native cortex during placement of the nonlocking compression screw in order to avoid undercorrection of the opening osteotomy.
Fig 6.

Using fluoroscopic guidance, a guide pin is placed approximately 2 to 3 fingerbreadths proximal to the lateral epicondyle and aimed just proximal to the medial epicondyle. This will determine the angle of the osteotomy made first with the oscillating saw, and followed by osteotomes.
Fig 7.
Osteotomes are used to complete the osteotomy in safe and effective manner. It is important not to violate the medial cortex during this step.
Fig 8.

Intraoperative fluoroscopic imaging is used to confirm adequate correction and plate-screw construct on the lateral femoral cortex. Only after the mechanical axis has been corrected will the plate be placed and secured on the lateral femoral cortex.
Postoperative Management
In the immediate postoperative period, all patients are placed on a chemical deep vein thrombosis prophylaxis agent, based on preoperative risk factors. Postprocedure, the operative extremity is kept in a sterile cotton dressing and ace wrap bandage. The leg is placed in a knee immobilizer and locked in full extension for mobilization/ambulation for the first 6 weeks. Knee range-of-motion exercises are allowed after surgery. Thromboembolic prophylaxis is provided based on preoperative risk factors. The patient is restricted to partial weight bearing for 6 weeks, followed by progressive weight bearing thereafter. Closed-chain strengthening and low-impact, aerobic exercises are permitted according to the patient's symptoms. Sport-specific training and progressive impact loading activities commence when deemed appropriate. Full-length standing radiographs are obtained to verify correction of deformity at 3 months postoperatively.
Discussion
There is consistency in the literature regarding patient outcomes and longevity utilizing modern osteotomy techniques and implants. Most authors agree this procedure is indicated for the young patient with isolated lateral compartment arthritis and valgus deformity. Kosashvili demonstrated that modified Knee Society scores significantly improved in 33 DFOs with minimum 10-year follow-up. One-half of these patients required conversion to total knee arthroplasty at 15 years following surgery.5 Backstein et al. reviewed a series of 40 DFOs with a mean follow-up of 10 years, demonstrating a 10-year survivorship of 82%, with a significant decline to 45% at 15 years.6 Sixty percent reported good to excellent results at most recent follow-up, with 15% reporting fair to poor; the majority of the latter group went on to total knee arthroplasty. In their systematic review in 2012, Saithna et al. reported similar results, with a cumulative survival ranging between 64% and 82% at 10 years, and 45% at 15 years, with conversion to arthroplasty serving as the end point.7 Drexler et al. showed encouraging results for DFOs in combination with osteochondral allograft transfer. Survivorship was reported as 89% at 10 years, 71% at 15 years, and 24% at 20 years.8
The advantages of a lateral opening wedge osteotomy include a familiar surgical approach, ability to fine-tune the intraoperative correction, and access to the lateral aspect of the knee.9, 10 The disadvantages include potential hardware irritation, a high rate of plate removal, malunion, or nonunion with the possible need for bone grafting, malcorrection, contracture, intra-articular fracture, breach of medial cortex, and neurovascular injury.3, 11, 12 See Table 2.
Table 2.
Advantages and Risks
|
|
Distal femoral osteotomies have shown good survival for up to 10 years but also have some limitations and complications. This is a technically challenging procedure with reported complication rates ranging between 5% and 63%.1, 7, 13 Incomplete osteotomy or placement of the guidewire too close to the joint predisposes to intra-articular fracture. Failure of adequate plate fixation to the cortical bone can lead to screw or plate failure, collapse of the osteotomy, and malunion or nonunion.2 The risk of osteotomy nonunion is reported at 5% of cases in the literature and delayed union taking up to 6 months in some cases.13 Allowing weight bearing too early in the healing process may result in implant failure as well as collapse at the osteotomy site. Unintentional perforation of the posterior femoral cortex or poor retractor placement at the time of the osteotomy can result in injury to the neurovascular structures.14
Potential risks using this technique include malcorrection, intra-articular fracture, neurovascular injury, malunion or nonunion, and hardware irritation. Other general postoperative complications may include deep vein thrombosis, pulmonary embolism, infection, arthrofibrosis, and anterior knee pain.3, 11, 12 See Table 3.
Table 3.
Pearls and Pitfalls
|
|
The lateral opening wedge distal femoral osteotomy is a reproducible technique for limb alignment correction in patients with valgus malalignment. Backstein et al. reported the expected survivorship of this procedure to be greater than 80% after 10 years.6 More recent studies have shown similar results. In one study, the 5-year survival rate was 74% in patients with osteoarthritis and 92% in those with joint preservation procedures (such as cartilage and meniscus repair).9 Similarly, in another recent study, the survival rates were 89% at 10 years and 71% at 15 years.8 In conclusion, this procedure remains a versatile and reliable option for addressing limb malalignment in the young population that may want to preserve function and higher activity levels over a period of 10 or more years.
Footnotes
The authors report the following potential conflict of interest or source of funding: M.J.S. receives support from Arthrex and Stryker and is on the editorial or governing board for the American Journal of Sports Medicine. A.J.K. receives support from Arthrex, Arthritis Foundation, and Histogenics.
Supplementary Data
The video describes our preferred technique for lateral opening wedge distal femoral osteotomy. The patient is supine, with the operative extremity draped in a usual sterile fashion. Typically, a more lateral skin incision is made to gain access to the lateral femoral cortex. In this circumstance, a more anterior skin incision, followed by a formal arthrotomy, was performed, as a concomitant lateral femoral condyle osteochondral allograft transfer was performed. Once the lateral femoral cortex is adequately exposed, a meta-diaphyseal guidepin is inserted, starting on the lateral cortex, and placed at an angle toward the medial femoral epicondyle. This will serve as a guide for the osteotomy cut. After the osteotomy is made, the size of the allograft bone wedge insert is based on the amount of correction determined preoperatively. The allograft is placed temporarily in a press fit fashion, whereas the overall limb alignment is checked on intraoperative radiographs. Once the desired correction is obtained, the plate is then placed and secured on the lateral femoral cortex. Final anteroposterior and lateral intraoperative images of the distal femur are then obtained prior to formal wound closure.
References
- 1.Brinkman J.M., Freiling D., Lobenhoffer P., Staubli A.E., van Heerwaarden R.J. Supracondylar femur osteotomies around the knee: Patient selection, planning, operative techniques, stability of fixation, and bone healing. Orthopade. 2014;43(Suppl 1):S1–S10. doi: 10.1007/s00132-014-3007-6. [DOI] [PubMed] [Google Scholar]
- 2.Puddu G., Cipolla M., Cerullo G., Franco V., Gianni E. Osteotomies: The surgical treatment of the valgus knee. Sports Med Arthrosc. 2007;15:15–22. doi: 10.1097/JSA.0b013e3180305c76. [DOI] [PubMed] [Google Scholar]
- 3.Paccola C.A.J., Fogagnolo F. Open-wedge high tibial osteotomy: A technical trick to avoid loss of reduction of the opposite cortex. Knee Surg Sports Traumatol Arthrosc. 2005;13:19–22. doi: 10.1007/s00167-003-0480-6. [DOI] [PubMed] [Google Scholar]
- 4.Puddu G., Cipolla M., Cerullo G., Franco V., Giannì E. Which osteotomy for a valgus knee? Int Orthop. 2010;34:239–247. doi: 10.1007/s00264-009-0820-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kosashvili Y., Safir O., Gross A., Morag G., Lakstein D., Backstein D. Distal femoral varus osteotomy for lateral osteoarthritis of the knee: A minimum ten-year follow-up. Int Orthop. 2010;34:249–254. doi: 10.1007/s00264-009-0807-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Backstein D., Morag G., Hanna S., Safir O., Gross A. Long-term follow-up of distal femoral varus osteotomy of the knee. J Arthroplasty. 2007;22:2–6. doi: 10.1016/j.arth.2007.01.026. [DOI] [PubMed] [Google Scholar]
- 7.Saithna A., Kundra R., Getgood A., Spalding T. Opening wedge distal femoral varus osteotomy for lateral compartment osteoarthritis in the valgus knee. Knee. 2014;21:172–175. doi: 10.1016/j.knee.2013.08.014. [DOI] [PubMed] [Google Scholar]
- 8.Drexler M., Gross A., Dwyer T. Distal femoral varus osteotomy combined with tibial plateau fresh osteochondral allograft for post-traumatic osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc. 2015;23:1317–1323. doi: 10.1007/s00167-013-2828-x. [DOI] [PubMed] [Google Scholar]
- 9.Cameron J.I., McCauley J.C., Kermanshahi A.Y., Bugbee W.D. Lateral opening-wedge distal femoral osteotomy: Pain relief, functional improvement, and survivorship at 5 years. Clin Orthop Relat Res. 2015;473:2009–2015. doi: 10.1007/s11999-014-4106-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hetsroni I., Lyman S., Pearle A.D., Marx R.G. The effect of lateral opening wedge distal femoral osteotomy on medial knee opening: Clinical and biomechanical factors. Knee Surg Sports Traumatol Arthrosc. 2014;22:1659–1665. doi: 10.1007/s00167-013-2405-3. [DOI] [PubMed] [Google Scholar]
- 11.Hooper G., Leslie H., Burn J., Schouten R., Beci I. Oblique upper tibial opening wedge osteotomy for genu varum. Oper Orthop Traumatol. 2005;17:662–673. doi: 10.1007/s00064-005-1157-8. [DOI] [PubMed] [Google Scholar]
- 12.Dehoux E., Madi K., Fourati E., Mensa C., Segal P. High tibial open-wedge osteotomy using a tricalcium phosphate substitute: 70 cases with 18 months mean follow-up. Rev Chir Orthop Reparatrice Appar Mot. 2005;91:143–148. doi: 10.1016/s0035-1040(05)84292-8. [in French] [DOI] [PubMed] [Google Scholar]
- 13.Edgerton B.C., Mariani E.M., Morrey B.F. Distal femoral varus osteotomy for painful genu valgum. A five-to-11-year follow-up study. Clin Orthop Relat Res. 1993;288:263–269. [PubMed] [Google Scholar]
- 14.Koyonos L., Slenker N., Cohen S. Complications in brief: Osteotomy for lower extremity malalignment. Clin Orthop Relat Res. 2012;470:3630–3636. doi: 10.1007/s11999-012-2392-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The video describes our preferred technique for lateral opening wedge distal femoral osteotomy. The patient is supine, with the operative extremity draped in a usual sterile fashion. Typically, a more lateral skin incision is made to gain access to the lateral femoral cortex. In this circumstance, a more anterior skin incision, followed by a formal arthrotomy, was performed, as a concomitant lateral femoral condyle osteochondral allograft transfer was performed. Once the lateral femoral cortex is adequately exposed, a meta-diaphyseal guidepin is inserted, starting on the lateral cortex, and placed at an angle toward the medial femoral epicondyle. This will serve as a guide for the osteotomy cut. After the osteotomy is made, the size of the allograft bone wedge insert is based on the amount of correction determined preoperatively. The allograft is placed temporarily in a press fit fashion, whereas the overall limb alignment is checked on intraoperative radiographs. Once the desired correction is obtained, the plate is then placed and secured on the lateral femoral cortex. Final anteroposterior and lateral intraoperative images of the distal femur are then obtained prior to formal wound closure.