Abstract
Objective: To assess results of the finger-to-floor distance (FFD) and the Schober test performed during the DOLOR study, and to verify correlation between Visual Analog Pain Scale scores (VAS) with these measures. Research design and methods: Previously tabulated data from the Clinical Research Forms of the DOLOR study were analyzed (statistical significance defined with a two-tailed p value < 0.05 and confidence interval of 95%). For continuous variables, the Student’s T- test or analysis of variance (ANOVA) was used, and differences between pre-treatment and Visits 2, 3, and 4 in the absolute number and percentage of patients with no change, improvement, or worsening of the Schober test and the FFD test scores were calculated, and the results were analyzed with the Chi-squared test. Spearman non-parametric correlation was used for correlating VAS scores with FFD and Schober test scores at each study visit. Main outcome measures: FFD, measured in centimeters; Schober test scores. Results: Throughout the treatment period, there was a statistically significant correlation between the VAS scores and the FFD in the total patient population and within treatment groups. This was not observed for the correlation between the Schober’s test scores and the VAS scores. FFD scores within treatment groups improved progressively at each study visit, as did the Schober Test scores. Conclusions: The results of this post-hoc analysis show that combination therapy with diclofenac plus vitamins B1, B6, and B12 had additional positive effects on mobility restoration among the patients of the DOLOR study and serve to highlight the correlation between mobility and pain intensity among patients presenting with low back pain. The two fundamental goals of low back pain therapy are to provide improvements in pain and function. In this sense, the combination of diclofenac with the B vitamins was particularly effective in achieving both of these goals.
Keywords: Low back pain, mobility, diclofenac, thiamine, pyridoxine, cyanocobalamin
Introduction
Diclofenac is among the most widely used non-steroidal anti-inflammatory agents (NSAIDs) and has been the subject of numerous clinical investigations in the treatment of a wide variety of mild-to-moderate painful conditions, including low back pain. The action of the combination of diclofenac (50 mg) and vitamins B1 (thiamine mononitrate, 50 mg), B6 (pyridoxine hydrochloride, 50 mg) and B12 (cyanocobalamin, 1 mg) vs diclofenac (50 mg) monotherapy was evaluated in a previous clinical trial (DOLOR study) among patients presenting with acute lumbago. Primary outcome measures including Visual Analog Pain Scale results were reported in the previously published paper entitled ‘Diclofenac plus B vitamins versus diclofenac monotherapy in lumbago: the DOLOR study’ 1 . However, in addition to the outcomes reported in the DOLOR publication, other data that may also be relevant in terms of patient mobility were also recorded during the treatment period. These measures included the finger-to-floor distance and the Schober test, and are the subject of this paper.
Patients and methods
In the DOLOR study, finger-to-floor distance (FFD) was recorded after having instructed the patient to plant both feet firmly on the floor and incline frontward with arms extended to the front. The distance between the patient’s middle finger and the floor was measured and recorded in centimeters (cm). The Schober test results were recorded in the following manner: with the patient standing erect, the investigator was asked to place a mark over the spinous process of the 5th lumbar vertebra, and another mark 10 cm above the previous mark, in the midline. The subject was asked to bend maximally forward and the distance between the two points (cm) was recorded.
Patients randomized to treatment in the DOLOR study were divided into two treatment groups: Group DB (n = 187) received the combination of diclofenac + B vitamins and Group D (n = 185) received diclofenac alone. A total of Enrolled subjects were scheduled to participate in study visits occurring at pre-treatment, Visit 2 (following 3 days of treatment), Visit 3 (following 5 days of treatment), and Visit 4 at the end of the 7-day treatment period. At study Visits 2 and 3, patients presenting with significant clinical improvement were allowed to prematurely terminate treatment and exit the study. Improvement was defined as Visual Analog Pain Scale (VAS) scores equal to or less than 20 mm on a 100 mm scale, and patient satisfaction with pain reduction. Accordingly, at Visit 2, 87 patients exited the study due to treatment success in the DB group and 55 patients exited the study in the D group, leaving 87 patients continuing treatment in group DB and 120 patients in Group D. At Visit 3, a further 71 patients exited the study in group DB and 52 in group D, leaving 16 subjects continuing treatment in group DB and 68 subjects in group D.
In this analysis, previously tabulated data from the Clinical Research Forms of the DOLOR study were analyzed using the software GraphPad Prism 5 for Windows, version 5.04 (GraphPad Software, San Diego CA). Statistical significance was defined with a two-tailed p-value of less than 0.05 with a confidence interval of 95%. For continuous variables, the Student’s T-test or analysis of variance (ANOVA) was used. Additionally, the differences between pre-treatment and Visits 2, 3, and 4 in the absolute number and percentage of patients with no change, improvement, or worsening of the Schober test and the FFD test scores were calculated, and the results were also arranged on contingency tables and analyzed with the Chi-squared test. In order to verify the presence of a correlation between decreased pain and improved mobility, we used the Spearman non-parametric correlation for total patient population and within treatment groups, correlating VAS scores with FFD and Schober test scores at each study visit.
Results
Throughout the treatment period, there was a statistically significant correlation between the VAS scores and the FFD in the total patient population and within treatment groups (Figure 1). This was not observed for the correlation between the Schober’s test scores and the VAS scores (Table 1).
Figure 1.
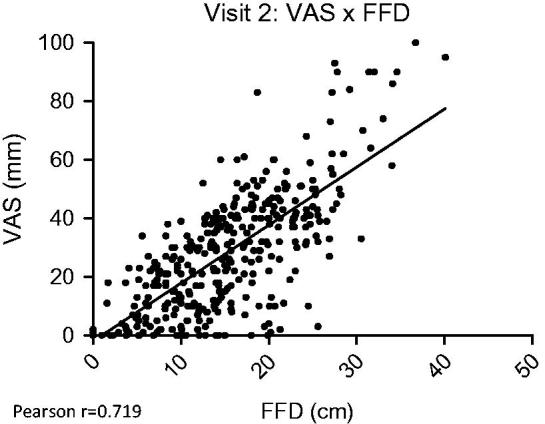
Total patients: Correlation between FFD and VAS scores at Visit 2.
Table 1.
Correlations between VAS scores with FFD and Schober test scores.
| VAS × FFD |
VAS × Schober Test |
|||
|---|---|---|---|---|
| Group DB | Group D | Group DB | Group D | |
| Pre-treatment | 0.36 | 0.355 | −0.151 | −0.057 |
| Visit 2 | 0.636 | 0.70 | −0.356 | −0.414 |
| Visit 3 | 0.527 | 0.527 | −0.30 | −0.326 |
| Visit 4 | 0.086 | 0.326 | −0.345 | −0.319 |
At pre-treatment, mean FFD in group DB was 19.57 cm (± 6.27), while that in group B was 21.19 cm (± 6.05). Following 3 days of treatment, the respective FFD scores were 13.72 cm (± 7.116) for group DB (statistically significant change from pre-treatment: p < 0.0001) and 16.64 cm (± 7.265) for Group D (statistically significant change from pretreatment: p < 0.0001). Mean FFD scores at Visit 2 were significantly lower among subjects of Group DB (p = 0.0001). Mean FFD scores following 5 days of treatment were: 9.899 cm (± 5.722) for Group DB and 12.86 cm (± 4.992) for Group D. Mean FFD scores at Visit 3 were significantly lower in group DB (p = 0.0001). At Visit 4, mean FFD in Group DB was 8.813 cm (± 3.559) and 10.49 cm (± 4.755) in Group D, with no statistically significant between-group difference (p = 0.1881).
Figure 2 summarizes the percentage of subjects presenting improvement, no change, or worsening of FFD at each study visit. No statistically significant between-group difference was detected at any study visit (Visit 2: p = 0.351; Visit 3: p = 0.465; Visit 4: p = 0.965).
Figure 2.
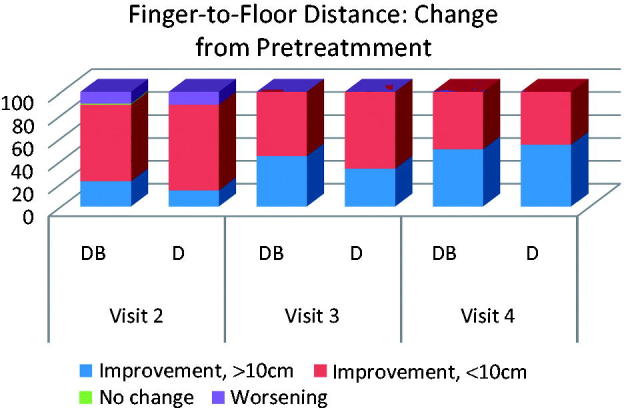
Percentage of subjects in Group DB (DB) and Group D (D) presenting improvement, no change, or worsening of FFD at each study visit.
Pre-treatment Schober test scores were 16.01cm (± 2.587) in Group DB and 16.1cm (± 2.343) in Group D. At Visit 2, Group DB scores increased in a statistically significant (p < 0.0001) manner to 17.23 cm (± 2.431) and Group D scores increased to 16.8 cm (± 2.26) (p < 0.001 in relation to pre-treatment values). While the mean Schober test scores in Group DB were higher than those of Group D at Visit 2, this difference did not attain statistical significance (p = 0.087). At Visit 3, mean Schober test scores in Group DB were 17.76 cm (± 2.214), while those in Group D were 17.22 cm (± 1.845). While the mean Schober test scores in Group DB were higher than those of Group D at Visit 3, this difference did not attain statistical significance (p = 0.0565). At Visit 4, mean Schober test scores among subjects of Group DB were 17.81 cm (± 2.073) and 17.56 cm (± 2.589) in Group D, with no statistically significant between-group difference (p = 0.7229).
Discussion
As the second most frequent symptom-related reason for physician visits after the common cold, low back pain represents one of the most common ailments in clinical practice, affecting up to 84% of adults at some point in time 2 . Low back pain carries a significant economic impact in terms of missed work, work-related disability, and medical expenses 3 . It is also important to note that patients with low back pain present both subjective and objective alterations in functional status, interfering with the ability to carry out daily activities and, thus, presenting a significant influence on quality-of-life 3 , 4 . Mobility is an important component of quality-of-life in patients with low back pain, and is associated with a profound effect on several aspects of the affected patients life including the ability to carry out essential daily activities 5 .
Significant improvement in pain and mobility were observed in both treatment groups. Mean FFD values did show superiority of the combination treatment over monotherapy after 3 and 5 days of treatment, but no between-group difference at treatment day 7. These results are in accordance with the overall findings previously reported in the DOLOR study of a faster time to treatment effect using combination therapy as compared to monotherapy 1 . While the scores of the Schober’s test were higher among Group DB subjects at both Visits 2 and 3, the scores did not attain statistical significant superiority over those observed in Group D.
The results of this post-hoc analysis serve to highlight the correlation between mobility and pain intensity among patients presenting with low back pain.
Conclusion
The results of this post-hoc analysis show that combination therapy with diclofenac plus vitamins B1, B6, and B12 had additional positive effects on mobility restoration among the patients of the DOLOR study and serve to highlight the correlation between mobility and pain intensity among patients presenting with low back pain. The two fundamental goals of low back pain therapy are to provide improvements in pain and function. In this sense, the combination of diclofenac with the B vitamins was particularly effective in achieving both of these goals.
Transparency
Declaration of funding
No funding was needed since this was a post-hoc analysis of data from a previously performed trial.
Declaration of financial/other relationships
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Mibielli MA, Geller M, Cohen JC. Diclofenac plus B vitamins versus diclofenac monotherapy in lumbago: the DOLOR study. CMRO. 2009;25:2589–99. doi: 10.3111/13696990903246911. [DOI] [PubMed] [Google Scholar]
- Manek N, MacGregor AJ. Epidemiology of low back disorders. Curr Opin Rheumatol. 2005;17:134–40. doi: 10.1097/01.bor.0000154215.08986.06. [DOI] [PubMed] [Google Scholar]
- Breivik H, Callett B, Ventafridda V. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10:287–333. doi: 10.1016/j.ejpain.2005.06.009. [DOI] [PubMed] [Google Scholar]
- Froud R, Patterson S, Eldridge S. A systematic review and meta-synthesis of the impact of low back pain on people’s lives. BMC Musculoskelet Disord. 2014;15:50. doi: 10.1186/1471-2474-15-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick N, Emanski E, Knaub MA. Acute and chronic low back pain. Med Clin North Am. 2014;98:777–89. doi: 10.1016/j.mcna.2014.03.005. [DOI] [PubMed] [Google Scholar]


