Abstract
Aim:
The aim of this study was to compare the metabolic profiles of subjects with normal glucose tolerance (NGT) with and without elevated 1-h postglucose (1HrPG) values during an oral glucose tolerance test (OGTT).
Methodology:
The study group comprised 996 subjects without known diabetes seen at tertiary diabetes center between 2010 and 2014. NGT was defined as fasting plasma glucose <100 mg/dl (5.5 mmol/L) and 2-h plasma glucose <140 mg/dl (7.8 mmol/L) after an 82.5 g oral glucose (equivalent to 75 g of anhydrous glucose) OGTT. Anthropometric measurements and biochemical investigations were done using standardized methods. The prevalence rate of generalized and central obesity, hypertension, dyslipidemia, and metabolic syndrome (MS) was determined among the NGT subjects stratified based on their 1HrPG values as <143 mg/dl, ≥143–<155 mg/dl, and ≥155 mg/dl, after adjusting for age, sex, body mass index (BMI), waist circumference, alcohol consumption, smoking, and family history of diabetes.
Results:
The mean age of the 996 NGT subjects was 48 ± 12 years and 53.5% were male. The mean glycated hemoglobin for subjects with 1HrPG <143 mg/dl was 5.5%, for those with 1HrPG ≥143–<155 mg/dl, 5.6% and for those with 1HrPG ≥155 mg/dl, 5.7%. NGT subjects with 1HrPG ≥143–<155 mg/dl and ≥155 mg/dl had significantly higher BMI, waist circumference, systolic and diastolic blood pressure, triglyceride, total cholesterol/high-density lipoprotein (HDL) ratio, triglyceride/HDL ratio, leukocyte count, and gamma glutamyl aminotransferase (P < 0.05) compared to subjects with 1HrPG <143 mg/dl. The odds ratio for MS for subjects with 1HrPG ≥143 mg/dl was 1.84 times higher compared to subjects with 1HrPG <143 mg/dl taken as the reference.
Conclusion:
NGT subjects with elevated 1HrPG values have a worse metabolic profile than those with normal 1HrPG during an OGTT.
Keywords: Asian Indians, elevated 1-h plasma glucose, metabolic syndrome, normal glucose tolerance, South Asians, type 2 diabetes
INTRODUCTION
Recent studies have shown that subjects with normal glucose tolerance (NGT) who have elevated 1-h postglucose values (1HrPG ≥143–<155 mg/dl and ≥155 mg/dl) in a 3-sample oral glucose tolerance test (OGTT) are at increased risk of progression to prediabetes and type 2 diabetes mellitus (T2DM), respectively.[1] NGT subjects with elevated 1HrPG values have also been shown to have subclinical inflammation, lipid disorders, and insulin resistance (IR).[2] Another study found that subjects with elevated 1HrPG had elevated liver enzymes, aspartate aminotransferase (AST), and alanine aminotransferase (ALT).[3] This places them at increased risk of not only incident type 2 diabetes but also nonalcoholic fatty liver disease (NAFLD) and cardiovascular disease (CVD).[4,5]
We have shown earlier that NGT subjects who have a 1HrPG value ≥155 mg/dl and 1HrPG ≥143–<155 mg/dl had an increased risk of progression to diabetes and prediabetes, respectively.[1] Defects in insulin secretion and IR have also been demonstrated in individuals with these increased 1HrPG values.[6] The aim of the present study was to look at the cardiometabolic risk profile of NGT subjects with elevated 1HrPG values and compare them with NGT subjects who had normal 1HrPG values to see whether their metabolic profile is already worse at the very early stage of glucose intolerance.
METHODOLOGY
The study subjects for this cross-sectional study spanning 3 years included all subjects without known diabetes aged ≥20 years, who came to our center to rule out diabetes. All underwent an OGTT for the first time at a tertiary diabetes center in Chennai. Subjects were classified as NGT if the fasting plasma glucose (FPG) was <100 mg/dl and the 2-h postglucose value was <140 mg/dl.[7] In total, 996 subjects of the 5364 individuals who had undergone an OGTT between 2011 and 2014 had NGT and they were included in the study. Individuals with kidney dysfunction, CVD, or history of any known infectious or inflammatory disease, based on medical history, were excluded from the study. Written informed consent was obtained from all subjects included in the study and the study was approved by the Institutional Ethics Committee.
Anthropometric and clinical measurements
Demographic information obtained included age, sex, family history of diabetes, and alcohol consumption. Anthropometric measurements including weight, height, and waist circumference were measured using the standard techniques. Height (in cm) was measured using a stadiometer (SECA Model 214, Seca GmbH Co, Hamburg, Germany). Individuals were asked to stand upright without shoes with his/her back against the vertical backboard, heels together, and eyes directed forward. Weight (in kg) was measured with an electronic weighing scale (SECA Model 807, Seca GmbH Co, Hamburg, Germany) that was kept on a firm horizontal flat surface. Individuals were asked to wear light clothing, and weight was recorded to the nearest 0.5 kg. Waist circumference was measured using a nonstretchable measuring tape and individuals were asked to stand erect with both feet together. Waist circumference was measured at the smallest horizontal girth between the costal margins and the iliac crest at the end of expiration. Blood pressure was recorded in the sitting position in the right arm to the nearest 1 mmHg using a mercury sphygmomanometer (Diamond Deluxe, Pune, Maharashtra, India). Two readings were taken 5 min apart and their mean was taken as the blood pressure.
Biochemical investigations
Biochemical analysis was done at our laboratory which is certified by the College of American Pathologist and the National Accreditation Board for Testing and Calibration Laboratories.
A fasting blood sample was obtained from the subjects after an overnight fast of at least 8 h. Subjects were requested to consume oral glucose 82.5 g (Glucon D, Heinz, Mumbai, Maharashtra, India, equivalent to 75 g of anhydrous glucose) dissolved in 300 ml of water. Blood sampling was done at fasting and at 1 h and 2 h after the glucose load was ingested. Plasma glucose levels were analyzed by the hexokinase method, serum cholesterol by cholesterol oxidase-peroxidase-amidopyrine method, serum triglyceride by the glycerolphosphate oxidase-peroxidase-amidopyrine method, high-density lipoprotein cholesterol (HDL-C) by direct method-immunoinhibition method, and serum creatinine by Jaffe's method using the Beckman Coulter AU2700 (Fullerton, CA, USA) and Beckman kits. Low-density lipoprotein cholesterol (LDL-C) was calculated using the Friedewald formula.[8] Glycated hemoglobin (HbA1C) was measured by high-pressure liquid chromatography using the Variant II Turbo (Bio-Rad, Hercules, California, USA). Liver enzymes, namely, AST, ALT, and gamma-glutamyl transferase (GGT) were estimated using the Beckman Coulter AU2700 (Fullerton, CA, USA), Beckman kits, and following the International Federation of Clinical Chemistry standardized methods. The intra- and inter-assay coefficients of variation for the biochemical assays were <5%. Leukocyte count was measured by flow cytometry using the Sysmex XT-1800i, using kits supplied by TransAsia (Japan). The intra- and inter-assay coefficients of variation of leukocyte count were <10%.
Body mass index (BMI) was calculated using the formula: weight (in kg) divided by height (in m) squared.
Generalized obesity was defined as BMI ≥25 kg/m2.[9]
Central obesity was defined as waist circumference ≥80 cm for women and ≥90 cm for men.[10]
Lipid abnormalities were classified based on the National Cholesterol Education Program guidelines.[11]
Hypercholesterolemia: serum cholesterol ≥200 mg/dl or drug treatment for hypercholesterolemia
Hypertriglyceridemia: serum triglyceride levels ≥150 mg/dl or drug treatment for hypertriglyceridemia
Low HDL-C: HDL-C levels <40 mg/dl for men and <50 mg/dl for women
High LDL-C: LDL-C levels ≥130 mg/dl calculated using the Friedewald equation
High total cholesterol ratio: total cholesterol to HDL ratio ≥4.5
Triglyceride to HDL ratio ≥3.5.[12]
Metabolic syndrome (MS) was defined based on the current harmonizing criteria, developed jointly by the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity, wherein any three of the following five components constitute MS:[13]
Abdominal obesity, i.e., increased waist circumference – ethnic specific cutoff points of ≥90 cm and ≥80 cm for men and women were used[10]
Elevated serum triglyceride levels ≥1.7 mmol/L (150 mg/dl) or on treatment for hypertriglyceridemia
Reduced serum HDL-C levels <40 mg/dl (1.0 mmol/L) in men and <50 mg/dl (1.3 mmol/L) in women
Elevated blood pressure ≥130/85 mmHg or on antihypertensive medication
Elevated FPG ≥100 mg/dl (5.6 mmol/L). These criteria were not applicable as by definition all subjects had NGT and therefore normal FPG.
Statistical analysis
Data analyses were performed with SPSS statistical software (version 22.0; SPSS, Chicago, IL, USA). Continuous data were reported as mean ± standard deviation values and categorical data as percentages. Subjects were stratified based on the 1HrPG cutoffs (1HrPG <143 mg/dl, 1HrPG ≥143–<155 mg/dl, and 1HrPG ≥155 mg/dl) which were determined and validated in the previous studies[1,6,14,15,16,17] and comparisons of their metabolic profiles were carried out. For continuous variables, one-way ANOVA was used to compare means between groups and Chi-square test was used to compare proportions between groups.
All variables were adjusted for confounding factors for CVD, diabetes, and MS, namely, age, sex, alcohol consumption, smoking, and family history for T2DM. The metabolic and glycemic variables were additionally adjusted for generalized and central obesity. Since the cutoffs for abdominal obesity (waist circumference) and elevated HDL are gender-specific, both waist circumference and HDL were adjusted only for age, alcohol consumption, smoking, and family history for T2DM. However, HDL was further adjusted for BMI. GGT was adjusted for age, sex, alcohol consumption, smoking, BMI, family history for T2DM, and in addition, HbA1c as it values are influenced by glycemic control.
The triglyceride/HDL-C ratio was computed as a surrogate marker for IR as it correlates strongly with homeostasis model assessment-IR.[18] Leukocyte counts were used as a surrogate marker for chronic subclinical inflammation.
Binary logistic regression was carried out using Group II + Group III (i.e., 1HrPG ≥143 mg/dl values) as dependent variable and Group I (1HrPG <143 mg/dl) as the reference. The anthropometric, biochemical, and metabolic markers pertinent to the study were taken as independent variables and the odds ratio (OR) (with 95% confidence interval [95% CI]) was determined. P < 0.05 was considered statistically significant.
RESULTS
The 996 NGT subjects had a mean age of 48 ± 12 years, 53.5% were male and 56.6% had one or both parents with diabetes. 16.2% were smokers and 19.9% consumed alcohol. 29.4% were on treatment for dyslipidemia and 15.1% for hypertension. For the purpose of analysis based on earlier studies,[1,6,14,15,16,17] all subjects were classified based on their 1HrPG cutoffs as 1HrPG <143 mg/dl designated as Group I (n = 525, 36.3%), those with 1HrPG ≥143–<155 mg/dl as Group II (n = 109, 10.9%), and those with 1HrPG ≥155 mg/dl as Group III (n = 362, 36.3%).
Table 1 describes the clinical and biochemical characteristics of subjects stratified based on 1HrPG levels. Groups II and III were older (P < 0.001) and had significantly higher BMI (P = 0.041), waist circumference (P = 0.012), systolic blood pressure (P < 0.001), diastolic blood pressure (P < 0.001), fasting glucose, 2HrPG (P < 0.001), HbA1c (P < 0.001), triglyceride (P < 0.004), leukocyte counts (P < 0.003), total cholesterol/HDL-C ratio (P = 0.001), triglyceride/HDL-C ratio (P < 0.001), creatinine (P = 0.003), and GGT (P = 0.020) compared to Group I. HDL-C was significantly lower (P = 0.019) in Groups II and III compared to Group I.
Table 1.
Clinical and biochemical characteristics of the study subjects
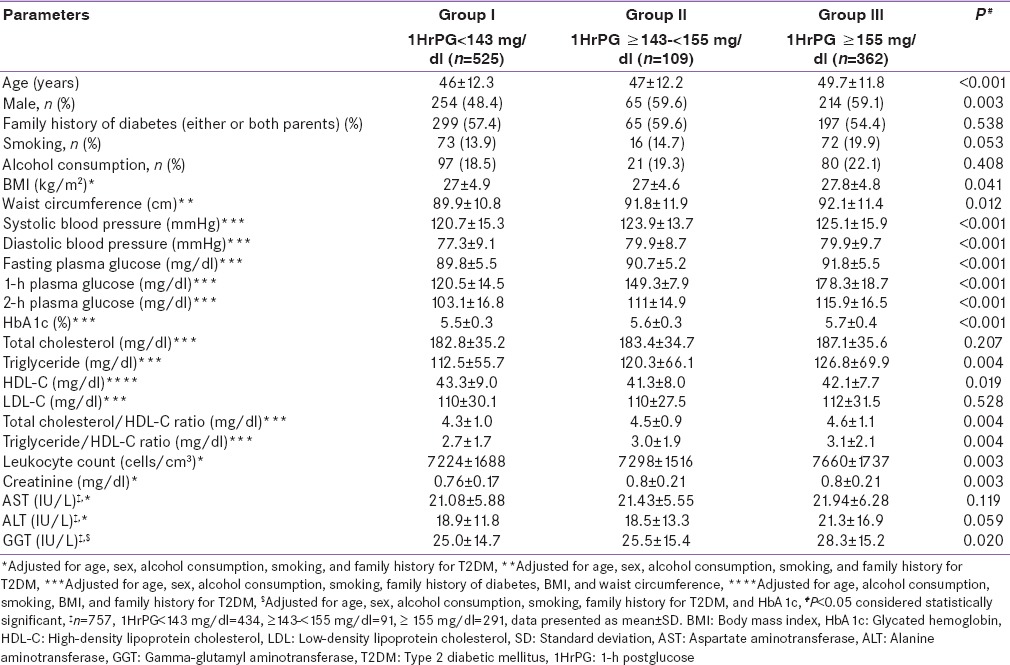
Table 2 shows the proportion of metabolic abnormalities among the NGT study subjects classified by their 1HrPG cutoffs as Groups I, II, and III after adjusting for age, sex, alcohol consumption smoking, family history of diabetes, BMI, and waist circumference. Hypertension (Group I 33.0% vs. Group II 45.9% vs. Group III 43.1%, P = 0.002), hypertriglyceridemia (39.3% vs. 49.1% vs. 48.1%, P = 0.018), high total cholesterol/HDL ratio (38.6% vs. 49.1% vs. 47.8%, P = 0.011), and high triglyceride/HDL ratio (23.9% vs. 31.5% vs. 31.8%, P = 0.023) were significantly higher in Groups II and III when compared to Group I. The proportion of NGT subjects with MS (≥3 risk factors), showed a significantly increasing trend in Groups II and III when compared to Group I (Group I 34.4% vs. Group II 50.0% vs. Group III 48.9%, P < 0.001).
Table 2.
Prevalence of metabolic abnormalities among the normal glucose tolerance study subjects classified by their 1-h postglucose cutoffs
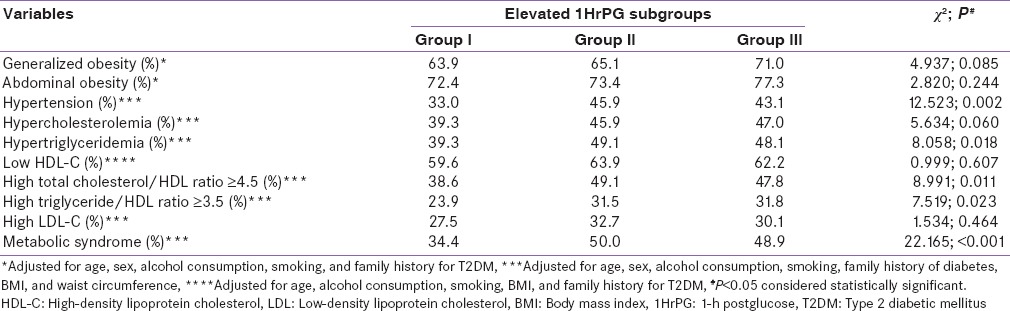
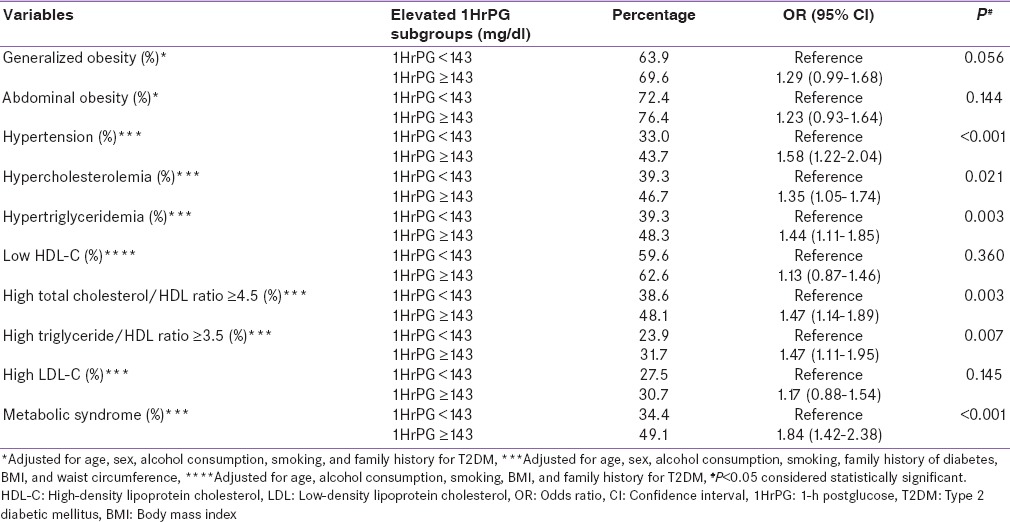
Table 3 presents the results of binary logistic regression to illustrate the discriminatory ability of the 1HrPG cutoffs (Groups I–III) in identifying adverse metabolic profiles. Due to small numbers, Groups II and III were combined and compared against Group I which was taken as the reference category (OR = 1). Individuals in Group II + Group III had significantly greater OR (95% CI) for hypertension 1.58 (1.22–2.04), hypercholesterolemia 1.35 (1.05–1.74), hypertriglyceridemia 1.44 (1.11–1.85), high total cholesterol/HDL ratio 1.47 (1.14–1.89), high triglyceride/HDL ratio 1.47 (1.11–1.959), and MS (≥3 risk factors) 1.84 (1.42–2.38) compared to Group I.
Table 3.
Binary logistic regression among the normal glucose tolerance study subjects classified by their 1-h postglucose cutoff to determine the odds ratio for prevalence of metabolic abnormalities
DISCUSSION
Asian Indians have an increased susceptibility to type 2 diabetes and CVD.[19,20,21] While there are several studies metabolically profiling Asian Indians with prediabetes (impaired fasting glucose and impaired glucose tolerance), there are little data on subjects particularly subclassifying NGT into different categories in the stage of NGT. Hence, we studied the metabolic profile of Asian-Indian NGT subjects with and without elevated 1HrPG values as an extension of our earlier studies in this field.[6]
The main findings of the study were that the (1) point prevalence of MS, FPG, 2HrPG, HbA1c, and leukocytes counts (as a marker of subclinical inflammation) were significantly higher in Groups II and III than their Group I counterparts. (2) While the mean liver enzymes levels (AST and ALT) were also significantly higher (P < 0.05) in Groups II and III than Group I, the significance was lost once they were adjusted for confounders such as age, sex, alcohol consumption, smoking, and family history for T2DM. (3) These findings suggest that Asian-Indian NGT subjects with elevated 1HrPG values have a worse metabolic profile than those with normal 1HrPG values. (4) It is possible that the worse metabolic profile contributes to a higher risk of progression to T2DM, CVD, and MS although longitudinal studies would be needed to prove this.
The significantly higher leukocyte count and worse lipid profiles seen among NGTs with elevated 1HrPG ≥155 mg/dl are similar to that reported by Bardini et al.[2] In the Chennai Urban Rural Epidemiology Study, we found a strong association between HbA1c and CVD in Asian-Indian subjects.[22] Longitudinal studies are needed to determine if a similar association with CVD exists in NGT subjects with elevated 1HrPG. Our earlier study revealed that NGT subjects with elevated 1HrPG levels had a 2-fold risk of developing diabetes.[1] Another study on NGTs with 1HrPG ≥155 mg/dl and MS found them to be at a 5-fold higher risk for type 2 diabetes.[14] A study on early glucose tolerance (early glucose intolerance [EGI] defined as 1HrPG ≥160 mg/dl and 2HrPG ≥140 and <200 mg/dl) in the Asian-Indian population revealed that the prevalence of MS was significantly higher in EGI individuals compared to NGT, 36.1% versus 27.9%.[23] Our study confirms these findings.
NGTs with elevated 1HrPG also had a higher prevalence of hypertension compared to NGT subjects with normal 1HrPG levels. There are studies that indicate that hypertension coupled with elevated 1HrPG levels is strongly associated with subclinical organ damage.[24] Hence, these findings are of great clinical significance.
One could speculate that hyperglycemia induces oxidative stress, formation of soluble advanced glycation end products, and lipid peroxidation which may, in turn, induce inflammatory gene expression.[25,26,27] Hyperglycemia is also toxic to endothelial cells and increases circulating cytokine concentrations, all of which implicated in IR causing plaque destabilization, and thereby future cardiovascular events.[25,26,27] These findings provide a likely explanation as to why some NGT subjects are at increased risk of CVD.
One of the limitations of the study is that being a cross-sectional one, no cause-effect relationship can be established. Further, although liver enzyme levels were estimated, we did not carry out ultrasonography; hence, we could not confirm the presence of NAFLD in these subjects. In the absence of direct markers, the triglyceride/HDL-C ratio was computed as a surrogate marker for IR[18] and elevated leukocyte counts were used as a surrogate marker for chronic subclinical inflammation,[2] both of which were significantly elevated in ≥143 mg/dl.
CONCLUSION
This study adds to a growing body of literature which supports the identification of NGT subjects with elevated 1HrPG values as they are prone to develop diabetes and CVD in the future. We suggest that Asian Indians with NGT but elevated 1HrPG value behave like prediabetes subjects with marked alterations in metabolic profile. There is thus clearly a need for instituting primary prevention of diabetes among these high-risk NGTs through lifestyle changes (physical activity and diet). Our study underscores the importance of reintroducing routine measurement of 1HrPG value during an OGTT as it can help to identify the subsets of NGT subjects who are at higher risk of type 2 diabetes and CVD. This used to be done years ago routinely as part of OGTT but was later given up as only the fasting and 2Hr values are included in the diagnostic criteria for diabetes with prediabetes. We suggest that those with NGT but elevated 1HrPG value in OGTT can be considered as a separate clinical entity, called EGI, which can be a still earlier stage in the natural history of T2DM.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank the participants and the staff of Dr. Mohan's Diabetes Specialities Centre and the Madras Diabetes Research Foundation, Chennai, for their help with this study.
REFERENCES
- 1.Priya M, Anjana RM, Chiwanga FS, Gokulakrishnan K, Deepa M, Mohan V. 1-hour venous plasma glucose and incident prediabetes and diabetes in Asian Indians. Diabetes Technol Ther. 2013;15:497–502. doi: 10.1089/dia.2013.0025. [DOI] [PubMed] [Google Scholar]
- 2.Bardini G, Dicembrini I, Cresci B, Rotella CM. Inflammation markers and metabolic characteristics of subjects with 1-h plasma glucose levels. Diabetes Care. 2010;33:411–3. doi: 10.2337/dc09-1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Succurro E, Arturi F, Grembiale A, Iorio F, Fiorentino TV, Andreozzi F, et al. One-hour post-load plasma glucose levels are associated with elevated liver enzymes. Nutr Metab Cardiovasc Dis. 2011;21:713–8. doi: 10.1016/j.numecd.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 4.Hanley AJ, Williams K, Festa A, Wagenknecht LE, D’Agostino RB, y, Kempf J, et al. Elevations in markers of liver injury and risk of type 2 diabetes: The insulin resistance atherosclerosis study. Diabetes. 2004;53:2623–32. doi: 10.2337/diabetes.53.10.2623. [DOI] [PubMed] [Google Scholar]
- 5.Kuppan G, Anjana RM, Deepa M, Paramasivam P, Chandrakumar S, Kaliyaperumal V, et al. Inflammatory markers in relation to nonalcoholic fatty liver disease in urban South Indians. Diabetes Technol Ther. 2012;14:152–8. doi: 10.1089/dia.2011.0213. [DOI] [PubMed] [Google Scholar]
- 6.Priya MM, Amutha A, Pramodkumar TA, Ranjani H, Jebarani S, Gokulakrishnan K, et al. ß-Cell function and insulin sensitivity in normal glucose-tolerant subjects stratified by 1-hour plasma glucose values. Diabetes Technol Ther. 2016;18:29–33. doi: 10.1089/dia.2015.0065. [DOI] [PubMed] [Google Scholar]
- 7.Standards of medical care in diabetes-2015: Summary of revisions. Diabetes Care. 2015;38:S4. doi: 10.2337/dc15-S003. [DOI] [PubMed] [Google Scholar]
- 8.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 9.World Health Organization. International Association for the Study of Obesity and International Obesity Task Force: The Asia Pacific Perspective: Redefining Obesity and Its Treatment. Sydney: Health Communications Australia Pty. Limited; 2000. pp. 17–21. [Google Scholar]
- 10.Enas EA, Mohan V, Deepa M, Farooq S, Pazhoor S, Chennikkara H. The metabolic syndrome and dyslipidemia among Asian Indians: A population with high rates of diabetes and premature coronary artery disease. J Cardiometab Syndr. 2007;2:267–75. doi: 10.1111/j.1559-4564.2007.07392.x. [DOI] [PubMed] [Google Scholar]
- 11.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 12.McLaughlin T, Reaven G, Abbasi F, Lamendola C, Saad M, Waters D, et al. Is there a simple way to identify insulin-resistant individuals at increased risk of cardiovascular disease? Am J Cardiol. 2005;96:399–404. doi: 10.1016/j.amjcard.2005.03.085. [DOI] [PubMed] [Google Scholar]
- 13.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: A joint interim statement of the International diabetes federation task force on epidemiology and prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–5. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 14.Abdul-Ghani MA, Abdul-Ghani T, Ali N, Defronzo RA. One-hour plasma glucose concentration and the metabolic syndrome identify subjects at high risk for future type 2 diabetes. Diabetes Care. 2008;31:1650–5. doi: 10.2337/dc08-0225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alyass A, Almgren P, Akerlund M, Dushoff J, Isomaa B, Nilsson P, et al. Modelling of OGTT curve identifies 1 h plasma glucose level as a strong predictor of incident type 2 diabetes: Results from two prospective cohorts. Diabetologia. 2015;58:87–97. doi: 10.1007/s00125-014-3390-x. [DOI] [PubMed] [Google Scholar]
- 16.Oh TJ, Min SH, Ahn CH, Kim EK, Kwak SH, Jung HS, et al. Normal glucose tolerance with a high 1-hour postload plasma glucose level exhibits decreased β-cell function similar to impaired glucose tolerance. Diabetes Metab J. 2015;39:147–53. doi: 10.4093/dmj.2015.39.2.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Strandberg AY, Pienimäki T, Pitkälä KH, Tilvis RS, Salomaa VV, Strandberg TE. Comparison of normal fasting and one-hour glucose levels as predictors of future diabetes during a 34-year follow-up. Ann Med. 2013;45:336–40. doi: 10.3109/07853890.2013.785233. [DOI] [PubMed] [Google Scholar]
- 18.Ray S, Talukdar A, Sonthalia N, Saha M, Kundu S, Khanra D, et al. Serum lipoprotein ratios as markers of insulin resistance: A study among non-diabetic acute coronary syndrome patients with impaired fasting glucose. Indian J Med Res. 2015;141:62–7. doi: 10.4103/0971-5916.154504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Joshi SR, Anjana RM, Deepa M, Pradeepa R, Bhansali A, Dhandania VK, et al. Prevalence of dyslipidemia in Urban and Rural India: The ICMR-INDIAB study. PLoS One. 2014;9:e96808. doi: 10.1371/journal.pone.0096808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bhansali A, Dhandania VK, Deepa M, Anjana RM, Joshi SR, Joshi PP, et al. Prevalence of and risk factors for hypertension in Urban and Rural India: The ICMR-INDIAB study. J Hum Hypertens. 2015;29:204–9. doi: 10.1038/jhh.2014.57. [DOI] [PubMed] [Google Scholar]
- 21.Pradeepa R, Anjana RM, Joshi SR, Bhansali A, Deepa M, Joshi PP, et al. Prevalence of generalized & abdominal obesity in Urban & Rural India – The ICMR-INDIAB Study (Phase-I) [ICMR- NDIAB-3] Indian J Med Res. 2015;142:139–50. doi: 10.4103/0971-5916.164234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dilley J, Ganesan A, Deepa R, Deepa M, Sharada G, Williams OD, et al. Association of A1C with cardiovascular disease and metabolic syndrome in Asian Indians with normal glucose tolerance. Diabetes Care. 2007;30:1527–32. doi: 10.2337/dc06-2414. [DOI] [PubMed] [Google Scholar]
- 23.Viswanathan V, Kumpatla S, Michael C, Tilak P. Prevalence of metabolic syndrome among Asian Indian subjects with elevated intermediate glucose response during OGTT. Diabetes Res Clin Pract. 2009;83:e17–8. doi: 10.1016/j.diabres.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 24.Sciacqua A, Miceli S, Greco L, Arturi F, Naccarato P, Mazzaferro D, et al. One-hour postload plasma glucose levels and diastolic function in hypertensive patients. Diabetes Care. 2011;34:2291–6. doi: 10.2337/dc11-0879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Esposito K, Nappo F, Marfella R, Giugliano G, Giugliano F, Ciotola M, et al. Inflammatory cytokine concentrations are acutely increased by hyperglycemia in humans: Role of oxidative stress. Circulation. 2002;106:2067–72. doi: 10.1161/01.cir.0000034509.14906.ae. [DOI] [PubMed] [Google Scholar]
- 26.Gokulakrishnan K, Deepa R, Sampathkumar R, Balasubramanyam M, Mohan V. Association of leukocyte count with varying degrees of glucose intolerance in Asian Indians: The Chennai urban rural epidemiology study (CURES-26) Metab Syndr Relat Disord. 2009;7:205–10. doi: 10.1089/met.2008.0024. [DOI] [PubMed] [Google Scholar]
- 27.Gokulakrishnan K, Deepa R, Sampathkumar R, Balasubramanyam M, Mohan V. Association of leukocyte count and hsCRP with metabolic abnormalities in subjects with normal glucose tolerance (CURES-64) J Assoc Physicians India. 2009;57:27–32. [PubMed] [Google Scholar]


